?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
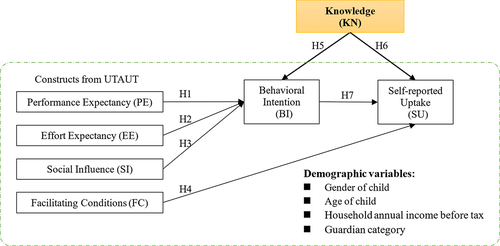
In China, the coverage rate of influenza vaccination among the general population is significantly lower than that of high-income countries, with only 2.46% of the population vaccinated. Preschool-aged children are particularly susceptible to influenza viruses, yet the factors that influence parents’ willingness to vaccinate their children are not well understood. To address this research gap, we developed a theoretical model grounded in the Unified Theory of Acceptance and Use of Technology (UTAUT), which explores six key factors influencing parental self-reported uptake of influenza vaccination in preschool children: performance expectancy, effort expectancy, social influence, facilitating conditions, knowledge, and behavioral intention. We collected data from 872 parents of children in five major cities in China and employed structural equation modeling to examine the significance of the theoretical model and explore the potential moderating effects of demographic variables on path relationships. Our analysis revealed that several positive factors influenced parents’ intention of influenza vaccination for preschool children, including effort expectancy (β = 0.38), social influence (β = 0.17), and knowledge (β = 0.52). Facilitating conditions (β = 0.34), knowledge (β = 0.40), and behavioral intention (β = 0.34) were found to be associated with self-reported uptake. Furthermore, we observed significant moderating effects of the child’s gender and age, as well as the guardian’s category and income, on the theoretical models. Parents’ willingness to vaccinate preschool children against influenza is influenced by both psychological and demographic variables. Further studies are needed to determine if these relationships persist over time and across different regions.
Introduction
The China Center for Disease Control and Prevention (CCDC) has released a national report on notifiable infectious disease epidemics. According to the report from October 1, 2021 to September 30, 2022, there were 2,660,868 reported cases of influenza in China, resulting in 21 fatalities.Citation1 Of those infected with influenza, children under the age of 5 accounted for 31.8% of cases, and they are at a higher risk of developing severe symptoms. Recently, the positive rate of influenza virus detection continued to rise in many Chinese cities, with A(H1N1) pdm09 predominant and A(H3N2) subtype influenza viruses circulating together.Citation2 The outbreak of influenza had a significant impact on public health in China, leading to a surge in demand for medical services and care, overwhelming the healthcare system and incurring substantial costs.Citation3,Citation4 A study on the disease burden of influenza in China spanning from 2006 to 2019 estimated that influenza-like illness (ILI) resulted in an annual average of 3.01 million cases (95%CI: 2.17–3.91) in China, with an average number of 2.35 million hospitalized cases of severe acute respiratory infection (SARI) (95%CI: 1.86–2.89), and an average of 92,000 excess deaths from respiratory diseases (95%CI: 75000–112,000).Citation5 Approximately 20%–30% of Chinese children are afflicted with influenza annually, they are susceptible to various severe complications, including pneumonia, myocarditis, otitis media, and meningitis.Citation6
Vaccination is a cost-effective prevention measure for high-risk groups.Citation3 The priority groups for influenza vaccination include medical professionals, individuals in gathering places, elderly persons aged 60 years and older, children aged 6 months to 5 years, patients with chronic illnesses, and family members of infants under 6 months.Citation7 The Chinese government has implemented various measures to reduce the cost of receiving influenza vaccinations. Many local governments in Beijing, Shenzhen, and Guangzhou provide free influenza vaccinations for elderly individuals aged 60 years and older, children in kindergartens, and primary and secondary school students. However, despite these efforts, the influenza vaccination rates in China remain low. The rates were 3.34% and 2.46% during the 2020–2021 and 2021–2022 influenza seasons, respectively.Citation6 In comparison, the United States reported an influenza vaccination rate of 52.1%, and Canada’s rate was approximately 40% during the 2020–2021 pandemic season.Citation8 Influenza vaccination hesitancy has been extensively studied, focusing on its determinants such as psychological perception and demographic factors.Citation9,Citation10 Psychological factors encompass knowledge, perceived effectiveness, perceived risk, affordability, accessibility, while sociodemographic variables include gender, age, education level, and family income.Citation9,Citation11,Citation17 Previous research conducted in Cyprus revealed that health care workers’ vaccine hesitancy stemmed from doubts about the vaccine’s effectiveness (21.5%) and safety concerns (29.3%).Citation2 Similarly, studies in Australia indicated that children from more affluent areas were more likely to be vaccinated, with funding playing a greater role in these regions compared to lower socio-economic backgrounds.Citation11 A survey of parents in mainland China shows that parental education and gender exert a moderating effect on parents’ decision on whether to consent to influenza vaccination for their children.Citation12 Policy measures such as promoting vaccination benefits, offering financial support, and ensuring safety guarantees have been shown to increase influenza vaccination rates.Citation11,Citation13–15 These prospective studies are valuable to encourage vulnerable populations to get vaccinated against influenza, ultimately reducing the incidence and impact of influenza.
While previous studies have explored the factors that influence flu vaccination intentions, the complex interplay between these factors remains poorly understood. Uncertain changes in individuals’ psychological motivations during the COVID-19 pandemic led to unpredictable health behavior decisions. To bridge this knowledge gap, our study focused specifically on influenza vaccination of preschool children during the COVID-19 pandemic. Over the past two years, we collected data on parental willingness to vaccinate preschoolers in China during the 2021–2022 and 2022–2023 influenza seasons. Our primary objective is to identify common influenza vaccination behaviors among parents of preschoolers and explore the associated factors. The current study uses structural equation modeling (SEM) to test and verify the complex relationship between observed and potential variables, including the construction of theoretical models and research hypotheses, measurement model testing, structural model testing, theoretical model and data fit, hypothesis testing, mediation effect and interference effect evaluation. This understanding is crucial for regulatory bodies, public health officials, and influenza vaccine manufacturers/operators, enabling them to optimize coverage levels in the preschool population and accurately predict future vaccine demand. By comprehensively grasping vaccination behaviors, we can work toward strategic goals for childhood influenza vaccination.
Theoretical model and methods
Theoretical model and hypotheses development
Venkatesh et al.Citation16 proposed the Unified Theory of Acceptance and Use of Technology (UTAUT) by integrating eight psychological perception models concerning user acceptance of new technology or systems.Citation16 The UTAUT measures users’ willingness to accept technology as the dependent variable, with the independent variable comprising various psychological perception factors. The dependent variables encompass behavioral intention and usage behavior, while the independent variables include performance expectancy, effort expectancy, social influence, and facilitating conditions. Subsequently, the UTAUT framework has been extended to incorporate additional constructs such as hedonic motivation, price value, habit, trust, and perceived risk. Additionally, the measurement tools have been tailored to specific contextual requirements.Citation17–19 The UTAUT model, along with its extensions, has been applied to various user health behavior scenarios including telemedicine,Citation20 ambulatory care,Citation21 and pneumococcal vaccination.Citation22 Previous research has also investigated knowledge, attitudes, and practices (KAP) associated with seasonal influenza vaccination, including pandemic influenzaCitation4,Citation23 and human papillomavirus vaccine (HPV).Citation24,Citation25 These studies consistently find that healthcare provider recommendations are key predictors of vaccination compliance among users. Specifically, healthcare providers with up-to-date knowledge, good practices, and positive attitudes toward influenza vaccination promote greater acceptance of vaccination among children,Citation26 pregnant women,Citation27 and health care workers.Citation28 Based on these findings, our research model is grounded in UTAUT and knowledge, as visualized in .
The proposed theoretical model comprises six constructs with precise definitions.Citation16,Citation29 Performance expectancy is the degree to which an individual believes that using the system will enhance job performance. Effort expectancy is the degree of ease associated with using the system. Social influence is the degree to which an individual perceives that important others believe he or she should use the new system. Facilitating conditions refer to the degree to which an individual believes that there exists an organizational and technical infrastructure to support use of the system. Knowledge pertains to the degree to which users possess and comprehend relevant knowledge. Behavioral intention predicts the degree to which an individual intends to use the new system. Uptake Behavior predicts the degree to which an individual intends to use the new system. We adapted measurement items of these constructs in the context of parents’ willingness to vaccinate their children against influenza. Referring to the previous literature, we proposed the following research hypotheses in the context of parental acceptance of influenza vaccination for their children.
Aligned with the Unified Theory of Acceptance and Use of Technology (UTAUT), high performance expectancy regarding the effectiveness of the influenza vaccine directly influences parental behavioral intention to vaccinate their children. If parents believe that the influenza vaccine is effective in preventing flu and its complications, they are more likely to intend to vaccinate their children.Citation22 Therefore, H1 is proposed as follows:
H1.
Performance expectancy has a positive direct effect on parental behavioral intention to vaccinate their children against influenza.
Effort expectancy, under the UTAUT model, corresponds with the perceived ease of use concept in the Technology Acceptance Model (TAM), which suggests that individuals are more likely to adopt behaviors that are easy to perform or require minimal effort. Low effort expectancy regarding the vaccination process for their children would affect parental intention to vaccinate directly. Thus, if parents perceive the process of vaccinating their children against influenza as an easy and convenient task, they are more likely to have the intention to vaccinate.Citation9,Citation30 However, effort expectancy alone may not determine parental intention but can work alongside other influencing factors. Therefore, we propose the second research hypothesis as follows:
H2.
Effort expectancy has a positive direct effect on parental behavioral intention to vaccinate their children against influenza.
The concept of social influence aligns with the Theory of Planned Behavior and the Social Cognitive Theory, which highlight the role of social norms, subjective norms, and observational learning in shaping individual intentions and behaviors. Social influence is a critical factor in shaping health-related decisions and individual behaviors. Social circles can positively influence parental intention to vaccinate their children against influenza if they observe others, such as friends, family members, or healthcare professionals, who endorse and encourage vaccination. When parents perceive that vaccinating their children is socially expected and supported in their social circles, they are more likely to develop a stronger intention to vaccinate.Citation2,Citation31 However, it’s important to note that social influence can work both positively and negatively. Negative social influence or vaccine hesitancy within certain social networks may negatively impact parental intention.
H3.
Social influence has a positive direct effect on parental behavioral intention to vaccinate their children against influenza.
Facilitating conditions refer to external factors that enable individuals to engage in specific behaviors or take particular actions.Citation16 In this case, facilitating conditions are assumed to have a positive and direct impact on parental self-reported uptake of influenza vaccination for their children.Citation12 By providing a supportive environment, resources, and assistance, facilitating conditions can help parents overcome barriers and conveniently vaccinate their children against the flu. These conditions may include accessible vaccination clinics, reminders, educational materials, social support, and reduced costs of vaccination. Based on previous research and the current context, we propose the following hypothesis:
H4.
Facilitating conditions have a positive direct effect on parental self-reported uptake to vaccinate their children against influenza.
Knowledge plays a pivotal role in forming attitudes and beliefs related to vaccination.Citation25,Citation29 When parents comprehend the efficacy and safety of the flu vaccine, as well as the consequences of not vaccinating, they are more inclined to develop a positive attitude toward vaccination and intend to vaccinate their children. When parents are better informed about the benefits, risks, and recommended guidelines for influenza vaccination, they are more likely to take action and ensure their children receive the flu vaccine.Citation3,Citation4 The following two hypotheses are proposed regarding knowledge:H5. Knowledge has a positive direct effect on parental behavioral intention to vaccinate their children against influenza.
H6.
Knowledge has a positive direct effect on parental self-reported uptake to vaccinate their children against influenza.
Behavioral intention refers to an individual’s readiness and willingness to engage in a specific behavior,Citation16 in this case, vaccinating their children against influenza. When parents have a positive attitude toward vaccination, perceive it as important, and express a clear intention to vaccinate their children, it increases the likelihood that they will vaccinate their children. Thus, we propose the following hypothesis:
H7.
Behavioral intention has a positive direct effect on parental self-reported uptake to vaccinate their children against influenza.
Questionnaire design
The second part of our study focused on the measurement of each factor in the theoretical model. In China, legal guardianship for over 99% of minors is with their parents, with the remaining 1% primarily being raised by grandparents or relatives, and only a small number under the care of social welfare agencies. For our research, data was collected only from cases where the parent served as the guardian. We adapted measurement items for six constructs from the UTAUT model (such as performance expectancy, effort expectancy, social influence, facilitating conditions, behavioral intention, and self-reported uptake) and drew from the KAP model for additional knowledge based on previous research. We then customized the measurement questions to align with the research scenario at hand, which concerned the behavioral intentions of parents with regards to influenza vaccination for their children. All measurement items were rated on a 7-point Likert scale, with responses ranging from 1 (strongly disagree) to 7 (strongly agree), and are presented in .
Table 1. Measurement items.
Data collection and statistical analysis
Parents of children seeking medical treatment or vaccination were randomly selected from child health centers or pediatric clinics across 21 medical institutions located in five Chinese cities: Beijing, Shanghai, Guangzhou, Chengdu, and Changsha. These cities are situated in various regions of China, all with populations exceeding 10 million. Children aged between six months and six years were chosen randomly based on their medical card numbers, and their parents were identified as potential respondents. Prior to completing the questionnaire, participants were required to sign an informed consent form and were given a detailed briefing about the survey’s content by the survey team.
In previous studies of structural equation models, the covariation between predictor and criterion variables may arise due to various factors such as data collection methods, measurement conditions, and project contexts. To mitigate the potential impact of common method bias (CMB) on statistical results, we took four measures in this investigation. Firstly, we employed multi-wave surveys that spanned two consecutive six-month periods during the 2021–2022 and 2022–2023 flu seasons. The fluctuating prevalence of flu across different months ensured survey results are generalizable to the overall level of flu season. Secondly, we conducted subregional surveys across five major cities – Beijing, Shanghai, Guangzhou, Chengdu, and Changsha – located in different regions of China. Given China’s vast territory and diverse population, various regions have differing levels of economic development and unique cultural practices. Thus, selecting multiple cities enhances sample representativeness and mitigates common bias. Thirdly, we utilized the randomization technique for questionnaire items to ensure that participants responded to items with inconsistent serial numbers, thereby reducing the likelihood of common method biases. Lastly, we utilized the Harman single-factor test to evaluate any potential common method biases in the collected data. All variables underwent exploratory factor analysis to test the outcomes of the unrotated factor analysis and identify the minimum number of factors required to explain the variation in variables. If only one factor emerged or if a given factor exhibited exceptional explanatory power (over 50%), we concluded that unacceptable common method bias was present.Citation32
The collected data underwent thorough cleansing, coding, and validation, before being analyzed using structural equation models in Amos 24.0 and SPSS 22.0 software, in order to test the research hypotheses. The first step involved testing the reliability of the data. Internal consistency of each construct was gauged using Cronbach’s alpha and confirmatory factor analysis, with acceptable criteria being Cronbach’s alpha exceeding 0.7 and standard loading of over 0.6.Citation33,Citation34 The second step involved testing the validity of the data. The convergence effectiveness of structural variables was measured by extracting the mean variance, with an average variance extracted (AVE) > 0.5 used as the acceptable criterion.Citation34,Citation35 Finally, a structural equation model was established to measure path loadings between variables and to determine the significance of the influence between different constructs. Moreover, it is presumed that behavioral intention acts as a mediator in the correlation between self-reported uptake and performance expectancy, effort expectancy, knowledge, and social influence. As per the PRODCLIN2 approach recommended by MacKinnon (2007), mediating effects were assessed through bootstrap samples (N = 6,000).Citation36,Citation37 Initially, the coefficient (a) and corresponding standard error of the influence of the independent variable (X) on mediator (M) is derived through regression analysis. Next, in case of controlling X, the coefficient (b) indicating the effect of M on the dependent variable (Y) and corresponding standard error are evaluated. Subsequently, these parameters were input into Prodclin2 to compute the confidence interval for the mediation effect. When zero is not included in the confidence interval, the mediating effect is deemed significant. Finally, the coefficient (c) and corresponding standard error of the direct influence of X on Y is derived through regression analysis, and the direct effect interval is estimated as . If the estimation range for indirect effects does not include zero, the direct effect is considered significant and classified as a “partial mediator;” otherwise, it is labeled as a “complete mediator.” Finally, in the fourth step, the moderating effects of control variables (i.e., sociodemographic variables) were tested based on a non-normalized coefficient.Citation38 Each sociodemographic variable was divided into two groups: child gender (male vs. female), child age (6 months to 3 years old vs. greater than 3 years old), household annual income (less than or equal to $10,000 vs. exceeding $10,000), guardian category (father versus mother). Group 1 consisted of participants with children aged between 6 months and 3 years, a household annual income before tax less than or equal to $10,000, and fathers. Group 2 comprised participants with children over 3 years old, a household annual income before tax exceeding $10,000, and mothers. Group 1 was coded as 0, while Group 2 was coded as 1. We examined the moderating effect of demographic variables by Z-test of the difference between regression coefficients.Citation38
, and
represents the unstandardized (not betas) regression coefficient and SE represents the standard error. If the absolute Z-value is greater than 1.96, it indicates that the demographic variable exerted a significant moderating effect at the confidence level of 0.05.
Results
Demographic data
We enrolled a cohort of 1,000 parents who had children with at least one outpatient visit during the influenza seasons of 2021–2022 and 2022–2023, which spanned from November to March. A total of 895 questionnaires were collected, and 872 questionnaires were effectively completed (questionnaires were completely filled in without any missing or incomplete answers). To ensure the adequacy of our sample size for structural equation model analysis, we followed Bollen’s (1991) recommendation that the sample size should be more than 15 times the number of variables.Citation39 The first common factor’s variance, as determined through exploratory factor analysis, explained 37.2% of the total variance, which is below the threshold of 50%. This indicates acceptable levels of common method biases. Further information on the characteristics of the sample can be found in .
Table 2. Sample characteristics (N = 872).
Measurement model
To assess the reliability of the measurements, we compared the standardized loadings of the latent variables with the threshold value of 0.6.Citation32,Citation39 The smallest standardized load, observed for SU1 (“My child was vaccinated against the flu”), was 0.747, indicating that all measurements were deemed acceptable. Moreover, a bootstrap sampling procedure (N = 6,000) was employed to test the stability of the estimates, and significance levels corresponded to p < .001 in each case. To evaluate the convergent validity at the construct level, we computed the composite reliability (CR), average variance extracted (AVE), and Cronbach’s alpha values. The minimum acceptable thresholds for these indicators were 0.7, 0.5, and 0.7, respectively. The calculated values for each construct were no less than 0.820, 0.822, and 0.598, respectively, demonstrating acceptable levels of convergence validity. The results of the reliability and convergence validity tests can be found in .
Table 3. The results of reliability and convergence validity tests.
Secondly, in accordance with Fornell and Larcker’s (1981) suggestion,Citation35 a discriminant validity test was conducted by comparing the square root of each construct’s average variance extracted (AVE) with the correlation coefficients related to other constructs. A construct is considered to have acceptable discriminant validity if its square root of AVE is greater than the correlation coefficients. The distinct items measure their respective constructs, indicating the discriminant validity of the analysis. The discriminant validity test outcomes for the constructs can be found in .
Table 4. The results of the constructs’ discriminative validity tests.
Structural model analysis
The initial step is to examine the overall fit of the theoretical model and data through structural equation modeling. We utilized the following indicators and thresholds as standards for verification: chi-square/freedom (NC value < 5), root mean square error of approximation (RMSEA) (<0.08), normed fit index (NFI) (>0.9), relative fit index (RFI) (>0.9), comparative fit index (CFI) (>0.9), Tucker-Lewis index (TLI) (>0.9), and adjusted goodness-of-fit index (AGFI) (>0.9). The above indexes analyzed via structural equation modeling produced the following results: chi-square/freedom = 1.646, RMSEA = 0.027, NFI = 0.968, RFI = 0.963, CFI = 0.987, AGFI = 0.953. These coefficients indicated that the fit between data and the theoretical model is acceptable. With regard to R2 values, our theoretical model effectively explained parents’ intention to vaccinate their children against influenza and their self-reported vaccinations, accounting for 85.6% and 84.5% of the variance in behavioral intention and self-reported uptake, respectively. This finding confirms that the current theoretical model possesses strong explanatory power.
Subsequently, standardized path coefficients and levels of significance were utilized to verify seven research hypotheses. The hypothesis testing results are listed in . Analysis reveals that, with the exception of the path coefficient from performance expectancy to behavioral intention, the significance of the remaining relational paths was confirmed. Three factors were identified as significant antecedents of behavioral intention, with knowledge (β = 0.519) being the most influential factor, followed by effort expectancy (β = 0.384) and social influence (β = 0.166), thereby supporting H2, H3, and H5. It was determined that knowledge (β = 0.400), facilitating conditions (β = 0.340) and behavioral intention (β = 0.337) were significant antecedents of self-reported uptake, thus supporting H4, H6, and H7.
Table 5. The results of hypotheses tests.
The mediation analysis results are presented in , uncovering a noteworthy correlation between the independent variable (X), mediating variable (M), and dependent variable (Y). Behavioral intention serves as a significant partial mediator in three paths, where the dependent variable is denoted as “self-reported uptake,” and the independent variables are performance expectancy, effort expectancy, and knowledge. However, it does not play a significant mediating role in the relationship between social influence and self-reported uptake. Our analysis outcomes display a significant association between independent variables and the dependent variable, where the mediator (behavioral intention) partially moderates the strength of their relationship. These findings unveil the underlying mechanisms of the independent and dependent variables’ relationship, emphasizing the significance of considering the mediating role of behavioral intent when comprehending their interaction.
Table 6. Mediation effects of behavioral intention.
The questionnaire measured four demographic variables, gender of child, age of child, household annual income before tax, and guardian category, and the results of moderating effects were tested with Z-values and the results are listed in . The gender of child had a significant moderating effect on two pathways, from performance expectancy to behavioral intention (Z = 2.32) and from social influence to behavioral intention (Z = −3.33). The age of child released a significant moderating effect on three paths, i.e., from effort expectancy to behavioral intention (Z = −6.57), from social influence to behavioral intention (Z = 2.80), and from knowledge to behavioral intention (Z = 3.07). Income was the demographic variable with the most significant moderating effects, releasing significant moderating effects on four paths associate with behavioral intention, the independent variables include effort expectancy (Z = −6.21), effort expectancy (Z = −43.13), social influence (Z = −7.76), knowledge (Z = −3.58). Income also released significant moderating effects in the following two paths, from facilitating conditions to self-reported uptake (Z = −2.22), and from knowledge to self-reported uptake (Z = 5.69). In particular, the significance of different pathways between the lowest income group and the highest income group changed substantially. For example, on the path from effort expectancy to behavioral intention, the lowest income group was not significant (β = 0.08), while the highest income group showed a strong correlation (β = 0.81). The guardian category showed a significant moderating effect only on the path from social influence to behavioral intention (Z = 3.139). The analysis of the moderating effect of demographic variables will provide practical reference for the targeted vaccination promotion policies of population subgroups.
Table 7. The moderating effects testing of demographic variables.
Discussion
The purpose of this study was to investigate the various factors that impact parental intention to vaccinate their preschool-age children against influenza, using data collected from the 2021–2022 and 2022–2023 influenza seasons. By applying an extended UTAUT theoretical framework, structural equation analysis helped to identify the intricate mechanisms underlying parental decision-making processes regarding influenza vaccination for their preschool children. The research provides an analytical framework that touches upon a range of multidimensional mechanisms in the context of childhood influenza vaccination, encompassing a variety of psychological factors and demographic variables. The empirical analysis, which considers the cross-association of multiple factors, offers novel perspectives and intriguing conclusions.
Performance expectancy does not appear to be a significant factor influencing parental intention to vaccinate preschool children against influenza, which differs from most previous studies in alternative contexts. While performance expectancy (perceived usefulness) has been identified as a contributing factor in HPV vaccination among sexual and gender minority patients,Citation30,Citation40 as well as in the acceptance behavior of elderly individuals utilizing home telehealth services,Citation41 there remains a lack of clear consensus among parents regarding the perceived usefulness of influenza vaccination against influenza viruses. This lack of agreement may be attributed to the dynamic variability of influenza viruses, which creates uncertainty concerning the protective benefits offered by influenza vaccines. The World Health Organization (WHO) has announced the dominant strains for the 2021–2022 flu season based on global influenza virus surveillance, namely A/Victoria/2570/2019 (H1N1) pdm09-like virus, Cambodia/e0826360/2020 (H3N2)-like virus, and B/Washington/02/2019-like (B/Victoria lineage) virus.Citation7 However, even if individuals receive the influenza vaccine, there is no guarantee of complete protection against the flu during the current influenza season. Respondents in the questionnaire survey frequently queried the efficacy of the influenza vaccine in protecting preschoolers from the influenza virus. The absence of a definitive answer is a primary reason why many parents are uncertain about vaccinating their preschool children. Another potential explanation for negative parental attitudes toward influenza vaccination is pervasive skepticism in China regarding the effectiveness of domestically produced vaccines. The 2018 vaccine scandal shed light on the inadequate quality of vaccines produced by Changsheng Bio-technology and Wuhan Biological Products Research Institute. These manufacturers distributed 250,000 and 400,000 doses of a faulty “adsorbed acellular DTP combined vaccine” to children in China, eroding public trust in vaccines. This lack of confidence, stemming from the actions of both manufacturers and government officials,Citation31 persists despite China’s extensive COVID-19 vaccination campaign. This campaign successfully administered a total of 3.32 billion doses to fully vaccinate 1.24 billion individuals between 2019–2022. However, mainland China still grapples with the ongoing COVID-19 pandemic. Additionally, doubts among the public regarding the effectiveness of domestically produced vaccines extend to influenza vaccination. These concerns significantly contribute to parents’ negative inclinations toward vaccinating their preschool-aged children.
Effort expectancy, referring to the perceived ease of use, is a critical factor in determining the behavioral intention of parents to vaccinate their preschoolers. This finding aligns with previous studies on various topics such as young adult male sexual minorities (MSM) and their willingness to initiate human papillomavirus (HPV) vaccination, as well as the impact physicians’ behavioral intentions have on the adoption of e-health apps.Citation30 Regarding influenza vaccination, the concept of effort expectancy mainly presents itself in the convenience of the process, including vaccination time, location, and cost.Citation9 In view of these findings, public health policymakers should consider implementing the following policies. First, they should prioritize improving information transparency by providing families with accurate, clear, and easily understandable information about the significance of influenza vaccination for preschool children, thereby increasing their confidence and willingness to vaccinate.Citation42 Second, improving the vaccination process could help combat low vaccination rates. These could include offering more convenient inoculation methods, such as implementing a reservation system or a quick inoculation channel, to streamline wait times and increase efficiency.Citation9 Finally, financial incentives such as coupons, discounts, or other benefits, could also encourage vaccination rates.Citation11 For instance, implementing the policy of free influenza vaccination for primary and secondary school students led to a significant increase in vaccination rates of approximately 85% in Beijing. However, few cities in China have enacted similar policies for preschool children.
Social influence refers to the impact that social factors, such as family, friends, colleagues, and media, have on individuals’ decision-making processes. In regards to influenza vaccination, significant research demonstrates that social influence plays a positive role in shaping parents’ attitudes toward vaccinating their preschool-aged children. These findings are consistent with observations made in other vaccination contexts.Citation2,Citation15,Citation25 Public policymakers should prioritize two areas of policy: social support and social responsibility. The first path involves increasing social support through channels such as social networks, family, and friends, to effectively communicate the importance of influenza vaccination for preschoolers and boost parents’ willingness to vaccinate.Citation11 The second path entails highlighting the social responsibility of influenza vaccination.Citation15 Public health advocates are encouraged to implement positive and effective health education campaigns that remind people that vaccination not only protects themselves, but also the wider community. This emphasis can help individuals realize that vaccination is an essential public responsibility.
Facilitating conditions encompass the resources, tools, and support available to assist individuals in accomplishing a specific behavior or task.Citation19,Citation20,Citation41 These conditions significantly influence people’s vaccination behavior, and can include access to vaccines, accurate information regarding vaccine safety and efficacy, convenient vaccination locations, and transportation options. When such services are readily available, vaccination becomes more feasible for individuals. For instance, if vaccines are widely accessible in a community and there are ample convenient locations offering vaccinations, the likelihood of vaccination uptake increases. Similarly, providing parents with accurate information on the safety and efficacy of flu vaccinations for children helps gain their trust and encourages them to vaccinate their children. With an eye to curbing the spread of infectious diseases, governments are advised to ensure that individuals receive the necessary resources, tools, and support to increase the probability of vaccination.
Previous research has consistently shown that parental knowledge is a significant predictor of their intention to vaccinate preschoolers against influenza. With the emergence of COVID-19, there has been an increasing awareness among Chinese citizens about the importance of virus protection and public health, leading to the widespread adoption of non-pharmaceutical interventions such as wearing masks and reducing social interaction.Citation43 While these interventions have significantly reduced the transmission of influenza, they have also potentially increased susceptibility to the virus and may lead to future outbreaks. Improved knowledge can help alleviate parental concerns and dispel misconceptions related to influenza vaccination for preschoolers, including fears of adverse reactions.Citation23,Citation29 Educational campaigns aimed at debunking such myths are necessary to increase public confidence in vaccination.Citation13 Public health practitioners should play an active role in disseminating accurate information to correct misconceptions and concerns, thereby enhancing people’s willingness to get vaccinated.Citation14,Citation26 Furthermore, accurate knowledge can also facilitate timely and appropriate immunization of preschoolers, such as ensuring they receive vaccines by the end of October,, which is before the peak of flu season.Citation44
The empirical findings confirm the mediating function of behavioral intentions in the correlation between diverse independent variables and self-reported influenza vaccination uptake among children. The dependent variable was “self-reported uptake,” referring to parents’ report on their children’s reception of flu immunization. The independent variables included performance expectancy, effort expectancy, knowledge, and social influence. The results indicated that behavioral intention partially mediated the relationship between performance expectancy, effort expectancy, and knowledge with self-reported vaccine uptake. This implies that the influence of these three independent variables on vaccination uptake was in part accounted for by behavioral intention. Intriguingly, behavioral intention didn’t play a significant mediating function in the relationship between social influence and self-reported vaccine uptake. This indicates that other factors beyond behavioral intention might contribute to the influence of peers, family members, or healthcare professionals on parents’ vaccination decisions. These findings hold substantial implications for promoting influenza vaccination in children, emphasizing the importance of factors such as perceived benefits, vaccination convenience, and vaccination awareness in shaping parental conduct. Future studies should explore other potential mediators or moderators that might account for the correlation among social influence and influenza vaccination among children. Demographic analysis provides a novel perspective on parental attitudes toward influenza vaccination for preschoolers. By exploring factors such as child’s gender and age, household income, and guardian role, we can gain a more comprehensive understanding of which demographics are more likely to decline or hesitate vaccination and take appropriate measures to alter their views.Citation45–47 Concerning the child’s gender, it influences two pathways: from performance expectancy to behavioral intention and from social influence to behavioral intention. Parents of male children have a greater tendency to accept the flu vaccine based on its perceived effectiveness, while parents of female children are more inclined to vaccinate due to its social impact. Child age is an interesting demographic variable that moderates all four pathways concerning behavioral intention, including performance expectancy, effort expectancy, social influence, and knowledge. Parents of younger children (ages 6 months to 3 years) are more likely to have an active intention to vaccinate preschoolers against influenza due to performance expectancy, effort expectancy, and knowledge, while parents of older children have positive intentions mainly due to effort expectancy. Income is a significant moderating factor that affects six paths as follows: the high-income group (over $50,000) significantly produces behavioral intention from effort expectancy and self-reported uptake from facilitating conditions, while the low-income group (below $10,000) reports vaccination behavior that is more influenced by knowledge. The difference in paternal or maternal guardian roles does not make a significant difference, except that fathers are more likely to be motivated by social influences to vaccinate preschoolers.
Despite some recent findings, the current study has several limitations. Firstly, the study only considered cases where the guardian was a biological parent, and the respondent was a parent of a child who had outpatient visit in hospitals. However, it may be of theoretical value to explore the link between guardian type and influenza vaccination in future studies to gain a more comprehensive understanding of the factors affecting vaccination behavior in children. Secondly, the use of cross-sectional data limits the ability to conduct longitudinal research over time. In China, a unified national vaccination information system is lacking, making it increasingly difficult to track previous vaccinations. The government is working to integrate and unify immunization information to alleviate this issue. It is recommended that future studies undertake temporal research to identify long-term factors that impact parents’ vaccination willingness throughout the preschool years. Finally, given China’s vast land area and uneven levels of development, the survey conducted in large cities may not be representative of the entire country. Regional variations may play a critical role in preschoolers’ interest in influenza vaccination. Additional research is necessary to understand the reasons for the lack of interest in influenza vaccination among preschoolers in small and medium-sized cities and rural areas and to investigate the link between vaccine provider and vaccination rates.
Conclusions
A multi-factorial crossover study has established a correlation between influenza immunization among preschool-aged children and parental readiness during the COVID-19 pandemic. The study identified various factors that impact parental willingness to vaccinate their children, including psychological and demographic variables. The study found that significant factors influencing parents’ intention to vaccinate preschool children against influenza are effort expectancy, social influence, and knowledge. Facilitating conditions, knowledge, and behavioral intention are positive factors that increase self-reported uptake. The child’s gender and age, guardian status, and income level demonstrated considerable moderating effects in theoretical models. These findings could lead to targeted initiatives by the government to encourage parental uptake of influenza vaccination among preschoolers. Future research should focus on the underlying reasons for the low vaccination rates among preschoolers.
Author contributions
SQ, MZ, and MY were responsible for the study conception and contributed to the elaboration of the questionnaire. MZ, HX, and WH contributed to data collection and conducted the statistical analyses. MZ, SQ, XT, and KC revised the manuscript and submitted it. All authors were implicated in the final manuscript preparation and approved the final manuscript. Each author agrees to be personally accountable for the author’s own contributions. All authors attest that they meet the ICMJE criteria for authorship.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- China-Center-for-Disease-Control-and-Prevention. Summary of influenza prevalence in China; 2023 [accessed 2023 Apr 12]. https://ivdc.chinacdc.cn/cnic/zyzx/lgzb/202304/t20230413_265257.htm.
- Papageorgiou C, Mazeri S, Karaiskakis M, Constantinou D, Nikolaides C, Katsouris S, Patsalou M, Kourouzidou D, Pantelas G, Koliou M, et al. Exploring vaccination coverage and attitudes of health care workers towards influenza vaccine in Cyprus. Vaccine. 2022;40(12):1775–11. doi:10.1016/j.vaccine.2022.02.020.
- Ye C, Zhu W, Yu J, Li Z, Hu W, Hao L, Wang Y, Xu H, Sun Q, Zhao G. Low coverage rate and awareness of influenza vaccine among older people in Shanghai, China: a cross-sectional study. Hum Vaccin Immunother. 2018;1–7. doi:10.1080/21645515.2018.1491246.
- Wendlandt R, Cowling BJ, Chen Y, Havers F, Shifflett P, Song Y, Zhang R, Iuliano D, Xu C, Yu H, et al. Knowledge, attitudes and practices related to the influenza virus and vaccine among older adults in Eastern China. Vaccine. 2018:36(19):2673–82. doi:10.1016/j.vaccine.2018.03.052.
- Gong H, Shen X, Yan H, Lu WY, Zhong GJ, Dong KG, Yang J, Yu HJ. Estimating the disease burden of seasonal influenza in China, 2006–2019. Zhonghua yi xue za zhi. 2021;101(8):560–7. doi:10.3760/cma.j.cn112137-20201210-03323.
- Zhao H, Peng, ZB, Ni, ZL, Yang, XK, Guo, QY, Zheng, JD, Qin, Y, Zhang, YP. Investigation on influenza vaccination policy and vaccination situation during the influenza seasons of 2020–2021 and 2021–2022 in China. Chin J Prev Med. 2022;56(11):1560–4.
- CCDC. China’s influenza vaccination technical guidelines 2022–2023. 2022 Aug 26 [accessed 2023 Apr 16].
- Sokale I, Alvarez J, Rosales O, Bakota E, Amos CI, Badr H, Oluyomi AO. COVID-19 vaccine uptake among US adults according to standard occupational groups. Vaccines (Basel). 2022;10(7):1000. doi:10.3390/vaccines10071000.
- Briggs L, Fronek P, Quinn V, Wilde T. Perceptions of influenza and pneumococcal vaccine uptake by older persons in Australia. Vaccine. 2019;37(32):4454–9. doi:10.1016/j.vaccine.2019.06.079.
- Zhou M, Zhao L, Campy KS, Wang S. Changing of China׳s health policy and doctor–patient relationship: 1949–2016. Health Policy Technol. 2017;6(3):358–67. doi:10.1016/j.hlpt.2017.05.002.
- De Oliveira Bernardo C, González-Chica DA, Stocks N. Impact of funding influenza vaccination on coverage among Australian children: a national study using MedicineInsight, a large general practice database. Hum Vaccin Immunother. 2019;16(3):1–6. doi:10.1080/21645515.2019.1664866.
- Zhao M, Liu H, Qu S, He L, Campy KS. Factors associated with parental acceptance of influenza vaccination for their children: the evidence from four cities of China. Hum Vaccin Immunother. 2021;17(2):457–64. doi:10.1080/21645515.2020.1771988.
- Wilson R, Scronias D, Zaytseva A, Ferry M-A, Chamboredon P, Dubé E, Verger P. Seasonal influenza self-vaccination behaviours and attitudes among nurses in Southeastern France. Hum Vaccin Immunother. 2019;15(10):2423–33. doi:10.1080/21645515.2019.1587274.
- Battistella C, Quattrin R, Celotto D, d’Angelo M, Fabbro E, Brusaferro S, Agodi A, Astengo M, Baldo V, Baldovin T, et al. Factors predicting influenza vaccination adherence among patients in dialysis: an Italian survey. Hum Vaccin Immunother. 2019;15(10):2434–9. doi:10.1080/21645515.2019.1588005.
- Seo J, Lim J. Trends in influenza vaccination coverage rates in South Korea from 2005 to 2014: effect of public health policies on vaccination behavior. Vaccine. 2018;36(25):3666–73. doi:10.1016/j.vaccine.2018.05.024.
- Venkatesh V, Morris, MG, Davis, GB, Davis, FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–78. doi:10.2307/30036540.
- Or CK, Karsh BT. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc. 2009;16(4):550–60. doi:10.1197/jamia.M2888.
- Venkatesh V, Thong T, Xu X. Consumer acceptance and use of information technology: extending the Unified theory of acceptance and use of technology. MIS Q. 2012;36(1):157–78. doi:10.2307/41410412.
- Oliveira T, Faria M, Thomas MA, Popovič A. Extending the understanding of mobile banking adoption: when UTAUT meets TTF and ITM. Int J Inf Manag. 2014;34(5):689–703. doi:10.1016/j.ijinfomgt.2014.06.004.
- Dwivedi YK, Rana NP, Jeyaraj A, Clement M, Williams MD. Re-examining the unified Theory of acceptance and use of technology (UTAUT): towards a revised theoretical model. Inf Syst Front. 2017;21(3):719–34. doi:10.1007/s10796-017-9774-y.
- Dunnebeil S, Sunyaev A, Blohm I, Leimeister JM, Krcmar H. Determinants of physicians’ technology acceptance for e-health in ambulatory care. Int J Med Inf. 2012;81(11):746–60. doi:10.1016/j.ijmedinf.2012.02.002.
- Zhou M, Zhan J, Kong N, Campy KS, Chen Y. Factors associated with intention to uptake pneumococcal vaccines among Chinese elderly aged 60 years and older during the early stage of COVID-19 pandemic. Psychol Health Med. 2021;27(1):91–105. doi:10.1080/13548506.2021.1905862.
- Ghandora H, Halperin DM, Isenor JE, Taylor BA, Fullsack P, Di Castri AM, Halperin SA. Knowledge, attitudes, behaviours, and beliefs of healthcare provider students regarding mandatory influenza vaccination. Hum Vaccin Immunother. 2019;15(3):700–9. doi:10.1080/21645515.2018.1543523.
- Wang MC, Chou C-Y, Ma M-C, Hsu YYA. Parental intention regarding the administration of the HPV vaccine for adolescent daughters in Taiwan. Women Health. 2016;56(4):361–75. doi:10.1080/03630242.2015.1101740.
- Krawczyk A, Knäuper B, Gilca V, Dubé E, Perez S, Joyal-Desmarais K, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccin Immunother. 2015;11(2):322–9. doi:10.1080/21645515.2014.1004030.
- Awad S, Abdo N, Yusef D, Jawarneh A, Babaa A, Alwady D, Al-Bawayeh H, Kasrawi I, Amaireh M, Obeidat M, et al. Knowledge, attitudes and practices related to influenza illness and vaccination in children: role of awareness campaigns in changing parents’ attitudes toward influenza vaccination in Jordan. Vaccine. 2019;37(25):3303–9. doi:10.1016/j.vaccine.2019.04.083.
- Arriola CS, Vasconez N, Bresee J, Ropero AM. Knowledge, attitudes and practices about influenza vaccination among pregnant women and healthcare providers serving pregnant women in Managua, Nicaragua. Vaccine. 2018;36(25):3686–93. doi:10.1016/j.vaccine.2018.05.013.
- Tognetto A, Zorzoli E, Franco E, Gervasi G, Paglione L, Di Ninno F, De Soccio P, Barbara A, Orsi GB, De Vito C, et al. Seasonal influenza vaccination among health-care workers: the impact of different tailored programs in four university hospitals in Rome. Hum Vaccin Immunother. 2020;16(1):81–5. doi:10.1080/21645515.2019.1632684.
- Leung JTC, Law CK. Revisiting knowledge, attitudes and practice (KAP) on human papillomavirus (HPV) vaccination among female university students in Hong Kong. Hum Vaccin Immunother. 2018;14(4):924–30. doi:10.1080/21645515.2017.1415685.
- Wheldon CW, Daley EM, Walsh-Buhi ER, Baldwin JA, Nyitray AG, Giuliano AR. An integrative theoretical framework for HPV vaccine promotion among male sexual minorities. Am J Mens Health. 2018;12(5):1409–20. doi:10.1177/1557988316652937.
- Zhou M, Qu S, Zhao L, Kong N, Campy KS, Wang S. Trust collapse caused by the Changsheng vaccine crisis in China. Vaccine. 2019;37(26):3419–25. doi:10.1016/j.vaccine.2019.05.020.
- Podsakoff PM, MacKenzie SB, Lee J-Y, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. doi:10.1037/0021-9010.88.5.879.
- Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor-analysis – the effect of sample-size. Psychol Bull. 1988;103(3):391–410. doi:10.1037/0033-2909.103.3.391.
- Cronin JJ, Brady MK, Hult GTM. Assessing the effects of quality, value, and customer satisfaction on consumer behavioral intentions in service environments. J Retail. 2000;76(2):193–218. doi:10.1016/S0022-4359(00)00028-2.
- Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. doi:10.1177/002224378101800104.
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58(1):593–614. doi:10.1146/annurev.psych.58.110405.085542.
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: program PRODCLIN. Behav Res Method. 2007;39(3):384–9. doi:10.3758/BF03193007.
- Duncan OD. Introduction to structural equation models. In: Duncan OD, editor. Introduction to structural equation models. San Diego: Academic Press; 1975. p. 1–173.
- Bollen K, Lennox R. Conventional wisdom on measurement – a structural equation perspective. Psychol Bull. 1991;110(2):305–14. doi:10.1037/0033-2909.110.2.305.
- Santhanes D, Wong CP, Yap YY, San SP, Chaiyakunapruk N, Khan TM. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): a scoping review. Hum Vaccin Immunother. 2018;14(1):124–33. doi:10.1080/21645515.2017.1381811.
- Cimperman M, Makovec Brencic M, Trkman P. Analyzing older users’ home telehealth services acceptance behavior-applying an extended UTAUT model. Int J Med Inform. 2016;90:22–31. doi:10.1016/j.ijmedinf.2016.03.002.
- Fireman B, Lee J, Lewis N, Bembom O, van der Laan M, Baxter R. Influenza vaccination and mortality: differentiating vaccine effects from bias. Am J Epidemiol. 2009;170(5):650–6. doi:10.1093/aje/kwp173.
- Zhou M, Long P, Kong N, Campy KS. Characterizing Wuhan residents’ mask-wearing intention at early stages of the COVID-19 pandemic. Patient Educ Couns. 2021;104(8):1868–77. doi:10.1016/j.pec.2020.12.020.
- Kaufmann J, DeVoe JE, Angier H, Moreno L, Cahen V, Marino M. Association of parent influenza vaccination and early childhood vaccinations using linked electronic health record data. Vaccine. 2022;40(49):7097–107. doi:10.1016/j.vaccine.2022.09.040.
- Hughes MM, Saiyed NS, Chen TS. Local-level adult influenza and pneumococcal vaccination disparities: Chicago, Illinois, 2015–2016. Am J Public Health. 2018;108(4):517–23. doi:10.2105/AJPH.2017.304257.
- Rolfes MA, Flannery B, Chung JR, O’Halloran A, Garg S, Belongia EA, Gaglani M, Zimmerman RK, Jackson ML, Monto AS, et al. Effects of influenza vaccination in the United States during the 2017–2018 influenza season. Clin Infect Dis. 2019;69(11):1845–53. doi:10.1093/cid/ciz075.
- Gates DM, Cohen SA, Orr K, Caffrey AR. Pediatric influenza vaccination rates lower than previous estimates in the United States. Vaccine. 2022;40(44):6337–43. doi:10.1016/j.vaccine.2022.09.053.