ABSTRACT
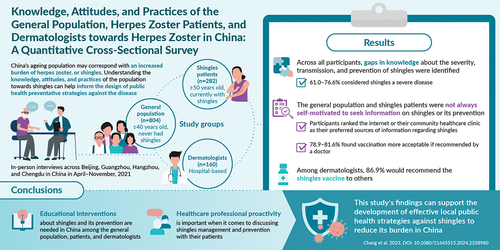
The burden of herpes zoster (HZ) is anticipated to increase among the aging population of China over time. The knowledge, attitudes, and practices (KAP) of the population toward HZ can help inform the design of public health strategies. As there is a paucity of KAP data in China, this cross-sectional survey therefore sought to assess KAP related to HZ from the general population, patients with HZ, and dermatologists in China. The total number of respondents from the general population, HZ patients, and dermatologists were 804, 282, and 160, respectively. Notably, some gaps in knowledge regarding the severity, transmission, and prevention of HZ were identified across all groups. For example, less than half of respondents from the general population and HZ patients understood that vaccination does not treat HZ. For dermatologists, not all were aware of adverse reactions following HZ vaccination and some had misconceptions regarding the mode of transmission of HZ. Given the link between an individual’s disease knowledge to their attitudes and practices, improved understanding of HZ could underlie positive attitudes and help reinforce healthcare professionals’ recommendations in the management and prevention of HZ. In particular, doctors may be well-positioned to support HZ prevention initiatives, as most of the general population and HZ patients found vaccination more acceptable if recommended by a doctor (78.9% and 81.6%, respectively). Therefore, consideration of these KAP attributes may support the development of targeted educational interventions and effective public health strategies against HZ in China.
Introduction
Herpes zoster (HZ) is a painful condition that is associated with a variety of distressing and potentially serious complications, all of which can be painful and debilitating.Citation1,Citation2 They often result in a substantial loss of quality of life (QoL) for patients,Citation3–5 and impose an economic burden on the individuals, their caregivers, and the healthcare system.Citation2,Citation6 HZ is caused by the reactivation of the varicella zoster virus.Citation1 Though the causes of reactivation can be multifactorial, older age has also been associated with an increased incidence of HZ.Citation1,Citation4 This may be due to immunosenescence, a natural, age-related decline in immunity, which can render older adults more susceptible to disease.Citation1,Citation2
According to international estimates, approximately 1 in 3 people will develop HZ in their lifetime.Citation7–9 However, this risk may increase in countries with aging populations, such as China, due to the growing composition of older age groups.Citation10–12 Consequently, the public health burden and associated costs of HZ are expected to increase over time. In China, incidence rates reported by studies on HZ among older adults (aged ≥50 years) range from 2.9 to 6.6 per 1,000 person-years.Citation13,Citation14 The economic burden of HZ has also been described in terms of costs and healthcare resource utilization associated with HZ and its complications, including outpatient visits, hospitalization, and duration of hospitalization.Citation13,Citation14 However, there is a lack of formal surveillance systems in China as HZ is not an officially notifiable disease,Citation15,Citation16 making it a challenge to accurately establish the local epidemiology of HZ and potentially leading to underestimation of HZ burden.
As studies have shown that conventional HZ treatments do not always achieve satisfactory results in patients, a proactive approach to managing HZ may alleviate its disease burden.Citation17 One such preventative strategy is vaccination; in 2019, a two-dose, adjuvanted recombinant zoster vaccine (RZV) was approved by the National Medicinal Products Administration in China and subsequently commercially launched in June 2020.Citation18,Citation19 In China, RZV is licensed for prevention of HZ among adults aged ≥50 years,Citation18 and eligible patients can voluntarily opt to receive the vaccination at their own expense.Citation18,Citation20 The Department of Aging Health in China also advocates for HZ vaccination for the elderly as a core strategy for disability prevention among this population.Citation16
There is a paucity of data on the knowledge, attitudes, and practices (KAP) related to HZ across the Asia-Pacific region, including China.Citation14,Citation17 In China and Hong Kong, studies describing KAP of the general population and HZ patients toward HZ highlighted an association between misconceptions and a lack of knowledge of HZ with under-recognition of disease burden and a low perceived need for vaccination.Citation20–22 Consequently, studying KAP from a range of respondents (e.g., general population, HZ patients, healthcare professionals) can elicit current perspectives on HZ from each population, and potentially elucidate differences in KAP between subpopulations. Stakeholders can thus leverage KAP findings to maximize outreach and efficacy of targeted public health interventions, such as health education, to uplift the standard of care for patients with HZ.
This study therefore sought to assess the knowledge and attitudes toward HZ, as well as practices related to its management and prevention, among the general population, patients with HZ, and dermatologists in China.
Materials and methods
Study population
There were three categories of study participants: the HZ-naïve general population of China aged ≥40 years (“general population;” served to represent the region of interest in terms of age, sex, education, and socio-economic status), patients aged ≥50 years who were diagnosed with a current episode of HZ at the time of the study (acute phase HZ) as confirmed by a doctor’s diagnosis (“HZ patients”), and dermatologists across primary, secondary, and tertiary hospitals with experience in the diagnosis, treatment, and management of HZ patients (“dermatologists”).
Study design
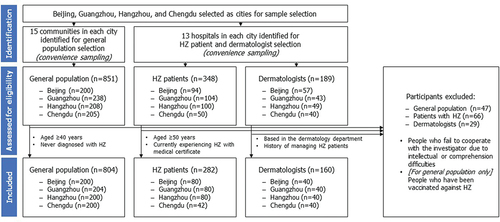
A cross-sectional survey was conducted among participants from 15 communities and 13 hospitals in Beijing, Guangzhou, Hangzhou, and Chengdu in April 2, 2021–November 8, 2021. Communities were selected randomly. Hospitals within the selected communities were then selected via convenience sampling. The survey used electronic questionnaires, which were facilitated by trained staff via in-person interviews (informed consent form shown in Appendix S1).
Multi-stage stratified sampling was used for selection of study sites and convenience sampling was used to recruit study participants. Members of the general population were recruited from selected local communities. Dermatologists were recruited from selected hospitals, and HZ patients were recruited from the same hospitals with assistance from healthcare professionals (HCPs).
Questionnaire design
The survey design was first tested among a sample population (n = 19). These data informed subsequent adjustments to the study design for a larger cohort survey among the target study population groups.
All surveys collected information on participant baseline demographics and their KAP toward HZ and its prevention. Survey questions were tailored to the cohort, resulting in three distinct questionnaires for each cohort (Appendix S2). The knowledge section of the questionnaire was divided into five subsections, including basic information regarding HZ, clinical characteristics of HZ, complications of HZ, risk factors for HZ, and vaccine immunity. The attitude section of the questionnaire had four subsections, including susceptibility to HZ, severity of HZ, benefits of the HZ vaccine, and barriers of vaccination. The practice section had two subsections on the prevention and treatment of HZ.
Ethics approval and consent
The study was conducted in accordance with the guiding principles of the Declaration of Helsinki (2008) and approved by the Ethics Committee of Peking University Health Science Center (IRB 00001052–21007; January 31, 2021). Informed consent was obtained from all individual participants included in the study. Written, informed consent to publish de-identified study results was also obtained from all individual participants included in the study.
Statistical analysis
The reliability and validity of the questionnaires were assessed using Cronbach’s alpha statistic and factor analysis, respectively. Cronbach’s alpha was used to assess reliability in the pilot phase of the study. Multivariable logistic regression was also used to identify factors that influenced the status of KAP. Data were analyzed using descriptive statistics. Missing data were not imputed at the first step of normality testing, and items with more than 50% missing responses were discarded. A p value of < .05 was considered as being statistically significant. Statistical analyzes were conducted using the statistical software SAS V.9.4 (SAS Institute Inc., Cary, North Carolina, United States [US]).
Results
Participant characteristics
A total of 851, 348, and 189 participants from the general population, HZ patients, and dermatologist groups were assessed for eligibility, respectively. Of these, 804 (94.5%), 282 (81.0%), and 160 (84.7%) members of the general population, HZ patients, and dermatologists were included in the final study, respectively (). Among the general population, HZ patients, and dermatologists, 60.6%, 59.9%, and 68.1% were female, respectively. The mean (standard deviation [SD]) age of the study groups was 56.2 (9.6), 63.6 (9.1), and 36.7 (9.8) years, respectively ().
Table 1. Baseline participant demographics and characteristics.
Among the general population and HZ patients, less than half reported a monthly household income greater than CNY ¥9,999 (equivalent to approximately US dollar [USD] $1,599; general population: 46.8%, HZ patients: 42.6%), and a similar proportion reported having a family size of ≥ 4 members (general population: 43.2%, HZ patients: 41.8%). Junior high school was the highest level of educational attainment among 40.6% and 50.0% of participants from the general population and HZ patients, respectively.
Among dermatologists, most had a master’s degree (57.5%), with a median of seven years of medical practice. The majority of dermatologists (73.8%) had treated >30 HZ patients in the past six months. Additionally, 11.9% of dermatologists reported that more than half of their HZ patients had HZ-related complications (e.g., PHN or ophthalmic involvement) in the past six months.
Knowledge regarding HZ
In terms of knowledge on HZ disease, most respondents across all study groups identified HZ as a skin disease caused by viral infection and over half considered HZ to be a severe disease (). Specifically, among the general population, 66.2% identified HZ as a skin disease, 71.6% identified that HZ was caused by a virus, and 61.0% thought of HZ as being severe in nature. A similar proportion of HZ patient respondents identified HZ as a skin disease (62.1%), and a slightly larger proportion thought of HZ as being a severe disease (76.6%). Notably, a lower proportion of all respondents were aware that the virus could be transmitted through contact with blister fluid (general population: 37.8%, HZ patients: 27.3%, dermatologists: 50.0%).
Table 2. Knowledge of HZ among the general population, HZ patients, and dermatologists.
Regarding HZ prevention, the majority of respondents across all study groups acknowledged that vaccination could prevent HZ, although less than half of the general population and HZ patients understood that vaccination does not treat HZ (43.5% and 40.8%, respectively). Similar proportions of respondents from the general population and HZ patients knew of an existing vaccine to prevent HZ (31.2% and 47.5%, respectively) and were aware of adverse reactions following vaccination in general (42.5% and 31.2%, respectively). Among dermatologists, 90.0% understood that vaccination does not treat HZ, 98.8% were aware of an existing vaccine to prevent HZ, and 66.9% knew of adverse reactions following vaccination in general.
Factors associated with knowledge regarding HZ
Significant predictors of knowledge about HZ for the general population included education level (p < .001), monthly family income (p = .0061), and awareness of chickenpox (p < .0001) (Table S1). For HZ patients, history of chicken pox (p = .0087) and city (p < .0001) were significant predictors of knowledge.
Attitudes towards HZ
Most respondents across all study groups agreed that HZ had a great effect on affected patients’ QoL; overall, most were also worried that they or their family members may contract HZ ().
Table 3. Attitudes regarding HZ among each cohort.
Regarding vaccination against HZ, approximately half to more than half of respondents among the general population and HZ patients agreed that vaccine effectiveness, its side effects, the number of doses required, and its cost would affect their willingness to be vaccinated. Most dermatologists also reported similar factors affecting vaccination willingness for patients; in particular, most dermatologists believed vaccine effectiveness and cost to be motivating factors for patients. Notably, most of the general population and HZ patients indicated that they found vaccination more acceptable if recommended by a doctor (78.9% and 81.6%, respectively).
In terms of the financial implications of HZ, more than half of respondents across all study groups believed that HZ significantly increased the family economic costs of patients with HZ, and that vaccination would decrease disease-associated expenditures.
Practices towards HZ
Regarding self-education on HZ, most of the general population and HZ patients would look to obtain information regarding these subjects through the internet or from their community healthcare clinic (). However, less than half of these respondents would proactively seek more information about HZ or its vaccination (47.0% and 46.5%, respectively). In terms of self-management of HZ, 80.6% of the general population and 36.9% of HZ patients would self-quarantine if they experienced HZ or HZ-associated complications. The majority of respondents in both groups also indicated that they would go to the hospital immediately if they experienced HZ or HZ-associated complications (99.0% and 91.1%, respectively).
Table 4. Practices toward HZ among each cohort.
Regarding the clinical management of HZ, all dermatologists recommended antiviral medication and 86.9% recommended an analgesic. It was also noted that 91.9% of dermatologists recommended acupuncture as a traditional Chinese medicine to treat HZ.
Discussion
Given China’s rapidly aging population, the burden of HZ is only expected to grow over time, highlighting the need for proactive, preventative measures against the disease.Citation23
This study highlighted several gaps in knowledge among the general population and HZ patients regarding the severity, transmission, and prevention of HZ. The majority of respondents from the general population and HZ patient groups had an educational level of high school or less, and all dermatologists had a bachelor’s degree at the minimum. Differences in knowledge of HZ and its prevention between these groups could therefore be partially attributed to level of educational attainment and profession, as evidenced by other studies reporting correlations between knowledge of HZ and educational attainment in the region.Citation21,Citation22 Furthermore, education level was a significant predictor of knowledge about HZ for the general population in this survey, suggesting a link between level of educational attainment and awareness of HZ in the general population of China.
Notably, the current study observed that while the majority of respondents would consider HZ vaccination, they were paradoxically not necessarily self-motivated to seek further information on HZ or its prevention. In comparison, other national and international surveys have reported HZ vaccine hesitancy or unwillingness among the public, which was associated with an incomplete understanding of HZ or misconceptions regarding their own HZ risk.Citation24–26 In a survey of HZ-vaccinated and unvaccinated respondents from the United Kingdom, unvaccinated individuals were also more likely to perceive that they were able to control HZ without vaccination, compared with vaccinated respondents.Citation26 National and international data alongside results from this study suggest that educational interventions could be tailored to fulfill specific gaps in knowledge regarding HZ disease and its prevention. This may be helpful to improve the public’s understanding of their own risk of HZ and potentially allay concerns regarding HZ vaccination. Specifically in China, study data highlight the need to adopt a proactive approach to raising HZ awareness among the public.
HZ vaccine-specific factors in influencing vaccination willingness were also identified in this study, such as effectiveness, side effects, cost, and number of doses. KAP surveys on HZ vaccination conducted within the Asia-Pacific region have reported similar vaccine-specific barriers against a willingness to vaccinate, including uncertainty about effectiveness, adverse reactions, and high cost.Citation24,Citation25 Of note, a survey of the general population of South Korea reported that, among participants who initially refused vaccination due to cost, subsequent physician recommendation to vaccinate reversed over half of these participants’ decisions.Citation25 Similar trends were also observed in international KAP survey results on HZ, whereby recommendation to vaccinate from a healthcare provider was an important influencing factor toward uptake of HZ vaccination.Citation24–27 Most respondents from the current study also indicated that they trusted their doctors to recommend vaccination. In the context of China, these data may therefore suggest that doctors are likely to be well-positioned to support HZ prevention initiatives, which could include recommending vaccination in line with local guidelines.
However, data from the current study suggest that not all dermatologists have a thorough understanding of HZ disease or vaccination. For example, only half of dermatologists were aware that blister fluid can transmit HZ. In terms of general vaccine knowledge, approximately one in three were not aware that adverse reactions could occur following vaccination (survey questions referred to vaccines in general and were not specific to HZ vaccination). As gaps in knowledge among the treating physicians may hinder discussions with patients, these data emphasize the importance of ensuring doctors have an accurate understanding of vaccination to effectively educate patients. Furthermore, some differences in practice between dermatologists in China and international guidance were noted; for example, a majority of dermatologists from the current survey reported recommending acupuncture as treatment for HZ, which differs from guidelines in the US and UK,Citation28,Citation29 which may reflect a greater use of traditional medicine for HZ in China compared with other parts of the world.Citation30
Overall, given the link between an individual’s disease knowledge to their attitudes and practices, improved knowledge of HZ could underlie positive attitudes and help to reinforce HCPs’ recommendations in the management and prevention of HZ. Specifically, data from this study can be used by local HCPs to understand what aspects impact patients’ willingness to vaccinate, enabling dermatologists to confidently discuss and weigh the benefits of vaccination against potential risks with their patients. The study also highlighted potential channels for communicating and delivering educational interventions and healthcare strategies. Notably, the internet (e.g., social media) and community healthcare clinics may be appropriate avenues to deliver key messages to members of the public and raise awareness on HZ, as these were ranked highly as sources for information on HZ by the general population and HZ patient respondents. In the US, the potential benefits of delivering HZ educational interventions in locations beyond a hospital or urgent-care setting have been highlighted.Citation31 Additionally, given that the high cost of HZ vaccines has been established as a barrier to vaccination both internationally and in China,Citation25,Citation32,Citation33 data from the current study highlight the potential value of increasing access to HZ vaccination by providing financial support to patients who would need vaccination the most.
To the authors’ knowledge, most KAP surveys on HZ in China to date do not capture the perspectives of local HCPs. A key strength of this study lies in its insight into responses from both laypeople (general population and HZ patients) and dermatologists, thereby providing a more holistic understanding of current beliefs and practices of these key participants in the healthcare system. These data therefore provide basis for development of effective, targeted public health interventions with considerations from both non-HCP and HCP parties.
In terms of limitations, firstly, medical jargon used in the general population survey may have hindered understanding by laypersons. However, this was mitigated by translation into simpler terms when the survey was conducted in Mandarin. A guidance document was also provided to investigators to ensure consistency of these translations. Future research could consider designing forms in accessible, simple language to ensure that informed consent can be sought in a consistent manner. Furthermore, participants were only informed to the extent compatible with the participants’ understanding.
Secondly, due to practical limitations arising from the COVID-19 pandemic, convenience sampling was used to identify the study population. Here, differences in economy and public education between the sampled cities were not mitigated, however baseline characteristics were collected to demonstrate the representativeness of the sample population (e.g., socioeconomic data on family income). Therefore, a randomized sampling approach could be used in future research.
In addition, this study included HZ patients on the basis of a doctor’s diagnosis, although this was not formally validated in the study. HZ patients were also sampled from a dermatology outpatient setting only, which may differ from actual practice where patients may receive treatment in various medical settings (e.g., neurology for PHN or ophthalmology for ophthalmic involvement). Moreover, only the responses of acute cases identified from outpatient settings were captured based on the study’s definition of HZ patients. In China, patients with HZ are initially managed in an outpatient setting, whereas those with chronic pain or symptoms persisting >1 month, suggesting a more complicated case,Citation34 would be referred for inpatient care. Given the above, findings may not be representative of chronic disease or patients with serious cases of HZ.
For dermatologists, results are limited to the perspectives of hospital-based dermatologists and may not be representative of the wider multidisciplinary care team. In reality, other HCPs (e.g., community doctors, pharmacists, nurses) may be involved in the care of a HZ patient. Future research to elicit the KAP of other HCPs may therefore be helpful to provide a more holistic overview of HCPs’ KAP toward HZ in China.
Finally, the questionnaire design could be further optimized for data collection in future research. For example, a variety of subjective versus forced choice format questions could be used to elicit clear responses. Moreover, implementation of a benchmark could be helpful for comparing and interpreting study results, thus helping to increase the robustness of findings.
Conclusions
This KAP study highlights areas for education and intervention among the general population, HZ patients, and dermatologists in China. These data also emphasize the importance of proactivity among HCPs in discussing HZ management and prevention with their patients. Furthermore, results from this study illuminate potential opportunities for collaboration between policymakers, key stakeholders, and the general body of HCPs to improve public awareness of HZ for disease prevention. Overall, findings can be used to support the development of effective local public health and education strategies against HZ, so as to reduce the burden of HZ in China.
Authors’ contributions
Substantial contributions to study conception and design: CC, HT, XZ, CZ, YF, CY; substantial contributions to analysis and interpretation of the data: CC, HT, XZ, CZ, YF, CY; drafting the article or revising it critically for important intellectual content: CC, HT, XZ, CZ, YF, CY; final approval of the version of the article to be published: CC, HT, XZ, CZ, YF, CY.
Ethics approval and consent
The study was conducted in accordance with the guiding principles of the Declaration of Helsinki (2008) and approved by the Ethics Committee of Peking University Health Science Center (IRB 00001052–21007; January 31, 2021). Informed consent was obtained from all individual participants included in the study. Written, informed consent to publish de-identified study results was also obtained from all individual participants included in the study.
China KAP_Supplementary Material_26Mar24_clean.docx
Download MS Word (91.9 KB)Acknowledgments
The authors acknowledge Professor Hang Li, First Hospital, Peking University, Beijing, China, for contributions to questionnaire design and site coordination, Jiaoting Ye, Xiamen Chazen Biomedical Technology Co. Ltd, Xiamen, China, for contributions to study site coordination, Ning Jiang, Everest Medicines, Beijing, China, and Yanfei Yuan, Everest Medicines, Beijing, China, for contributions to the design of the work, Yunkun He, GSK, Beijing, China, Sumitra Shantakumar, GSK, Singapore, Singapore, and Jing Chen, GSK, Singapore, Singapore, for contributions to the collection, generation, analyses, and interpretation of the work, and Roeland Van Kerckhoven, GSK, Wavre, Belgium for publication management. The authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Paige Foo Jia-Qi, Costello Medical, Singapore for medical writing and editorial assistance based on authors’ input and direction.
Disclosure statement
CC: Nothing to disclose; HT: Former employee of the GSK group of companies; XZ: Nothing to disclose; CZ: Former employee of Xiamen Chazen Biomedical Technology Co. Ltd, which received funding from the GSK group of companies to conduct the study disclosed in this publication; YF: Employee of Xiamen Chazen Biomedical Technology Co. Ltd, which received funding from the GSK group of companies to conduct the study disclosed in this publication; CY: Employee of the GSK group of companies.
Data availability statement
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2338980.
Additional information
Funding
References
- Centers for Disease Control and Prevention. The Pink Book: Zoster. 2021 Aug 18 [accessed 2022 Mar]. https://www.cdc.gov/vaccines/pubs/pinkbook/herpes-zoster.html.
- Johnson RW, Alvarez-Pasquin MJ, Bijl M, Franco E, Gaillat J, Clara JG, Labetoulle M, Michel JP, Naldi L, Sanmarti LS, Weinke T. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vaccines. 2015;3:109–13. doi:10.1177/2051013615599151.
- Johnson RW, Bouhassira D, Kassianos G, Leplège A, Schmader KE, Weinke T. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med. 2010;8:37. doi:10.1186/1741-7015-8-37.
- Katz J, Cooper EM, Walther RR, Sweeney EW, Dworkin RH. Acute pain in herpes zoster and its impact on health-related quality of life. Clin Infect Dis. 2004;39:342–8. doi:10.1086/421942.
- Schmader KE, Sloane R, Pieper C, Coplan PM, Nikas A, Saddier P, Chan IS, Choo P, Levin MJ, Johnson G, Williams HM, Oxman MN. The impact of acute herpes zoster pain and discomfort on functional status and quality of life in older adults. Clin J Pain. 2007;23(6):490–6. doi:10.1097/AJP.0b013e318065b6c9.
- Yu SY, Fan BF, Yang F, DiBonaventura M, Chen YX, Li RY, King-Concialdi K, Kudel I, Hlavacek P, Hopps M, Udall M, Sadosky A, Cappelleri JC. Patient and economic burdens of postherpetic neuralgia in China. Clin Outcomes Res. 2019;11:539–50. doi:10.2147/CEOR.S203920.
- Brisson M, Edmunds WJ, Law B, Gay NJ, Walld R, Brownell M, Roos LL, DE Serres G. Epidemiology of varicella zoster virus infection in Canada and the United Kingdom. Epidemiol Infect. 2001;127:305–14. doi:10.1017/S0950268801005921.
- Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep. 2008;57 quiz CE2–4:1–30.
- Lin YH, Huang LM, Chang IS, Tsai F-Y, Lu C-Y, Shao P-L, Chang L-Y. Disease burden and epidemiology of herpes zoster in pre-vaccine Taiwan. Vaccine. 2010;28:1217–20. doi:10.1016/j.vaccine.2009.11.029.
- National Bureau of Statistics. Bulletin for the 7th census of China (5th Edition). 2021 May 11 [accessed 2022 Mar]. http://www.stats.gov.cn/sj/tjgb/rkpcgb/qgrkpcgb/202302/t20230206_1902005.html.
- Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, Zhu X, Preedy V, Lu H, Bohr VA, Chan WY, Liu Y, Ng TB. A research agenda for aging in China in the 21st century. Ageing Res Rev. 2015;24:197–205. doi:10.1016/j.arr.2015.08.003.
- Li Y, An Z, Yin D, Liu Y, Huang Z, Xu J, Ma Y, Tu Q, Li Q, Wang H. Disease burden due to herpes zoster among population aged ≥50 years old in China: a community based retrospective survey. PLoS One. 2016;11(4):e0152660. doi:10.1371/journal.pone.0152660.
- Sun X, Wei Z, Lin H, Jit M, Li Z, Fu C. Incidence and disease burden of herpes zoster in the population aged ≥50 years in China: data from an integrated health care network. J Infect. 2021;82:253–60. doi:10.1016/j.jinf.2020.12.013.
- Yin D, Van Oorschot D, Jiang N, Marijam A, Saha D, Wu Z, Tang H, Diaz-Decaro J, Watson P, Xie X, Ren Y, He Y, Feng Y. A systematic literature review to assess the burden of herpes zoster disease in China. Expert Rev Anti Infect Ther. 2021;19(2):165–79. doi:10.1080/14787210.2020.1792290.
- Zhu Q, Zheng H, Qu H, Deng H, Zhang J, Ma W, Lin Y, Xie X, Qiu Q, Huang Z. Epidemiology of herpes zoster among adults aged 50 and above in Guangdong, China. Hum Vaccin Immunother. 2015;11:2113–8. doi:10.1080/21645515.2015.1016672.
- Shi J, Gao C, Yu P. Interpretation of core information on disability prevention in the elderly. Chinese J Geriatr. 2019;38:1077–8.
- Chen L-K, Arai H, Chen L-Y, Chou M-Y, Djauzi S, Dong B, Kojima T, Kwon KT, Leong HN, Leung EMF, Liang C-K, Liu X, Mathai D, Pan JY, Peng L-N, Poblete ERS, Poi PJH, Reid S, Tantawichien T, Won CW. Looking back to move forward: a twenty-year audit of herpes zoster in Asia-Pacific. BMC Infect Dis. 2017;17(1):213. doi:10.1186/s12879-017-2198-y.
- National Medical Products Administration of the People’s Republic of China. Herpes zoster vaccine (recombinant, adjuvanted). 2019 May 22 [accessed 2022 Mar]. https://www.nmpa.gov.cn/directory/web/nmpa/zhuanti/ypqxgg/gggzjzh/20190522150701437.html.
- Wang F, Zhang W, Tang F, Lu H, Sun L, Qi Q, Hao F, Wang H, Yin Z. Interpretation of shingles vaccination guidelines of the advisory committee on immunization practices in the United States and Canada. Chin Med J. 2021;101:363–8. doi:10.3760/cma.j.cn112137-20201030-02968.
- Wang M, Hu M, Wang Y, Long C, Xia Y, Zhu D, Zhao W, Yuan B, He P. Willingness to vaccinate against herpes zoster in Chinese urban population: a mixed-methods study. BMJ Open. 2023;13:e079115. doi:10.1136/bmjopen-2023-079115.
- Lam AC, Chan MY, Chou HY, Ho SY, Li HL, Lo CY, Shek KF, To SY, Yam KK, Yeung I. A cross-sectional study of the knowledge, attitude, and practice of patients aged 50 years or above towards herpes zoster in an out-patient setting. Hong Kong Med J. 2017;23:365–73. doi:10.12809/hkmj165043.
- Wang M, Long C, Hu MZ, Wang YS, Xia YQ, Yuan BB, Zhu DW, He P. A study on knowledge, attitude, and vaccination behavior of herpes zoster vaccine among urban residents in selected areas of China. Zhonghua Liu Xing Bing Xue Za Zhi. 2023;44:899–904. doi:10.3760/cma.j.cn112338-20221125-00998.
- Lee C, Giannelos N, Curran D, Dong H, Tang H, Jiang N, Ye C, Yuan Y, Ng C. Lifetime risk of herpes zoster in the population of Beijing, China. Public Health Pract. 2023;5:100356. doi:10.1016/j.puhip.2023.100356.
- Cheng L-Y. A pilot study to assess the awareness of herpes zoster and the attitudes towards herpes zoster vaccination among Chinese patients attending a government general out-patient clinic in Hong Kong. HK Pract. 2019;41:60–5.
- Yang TU, Cheong HJ, Song JY, Noh JY, Kim WJ. Survey on public awareness, attitudes, and barriers for herpes zoster vaccination in South Korea. Hum Vaccin Immunother. 2015;11:719–26. doi:10.1080/21645515.2015.1008885.
- Bricout H, Torcel-Pagnon L, Lecomte C, Almas MF, Matthews I, Lu X, Wheelock A, Sevdalis N. Determinants of shingles vaccine acceptance in the United Kingdom. PLoS One. 2019;14:e0220230. doi:10.1371/journal.pone.0220230.
- Baalbaki NA, Fava JP, Ng M, Okorafor E, Nawaz A, Chiu W, Salim A, Cha R, Kilgore PE. A community-based survey to assess knowledge, attitudes, beliefs and practices regarding herpes zoster in an urban setting. Infect Dis Ther. 2019;8:687–94. doi:10.1007/s40121-019-00269-2.
- Centers for Disease Control and Prevention. Shingles (Herpes Zoster). 2023 May 10 [accessed 2023 Jul]. https://www.cdc.gov/shingles/about/treatment.html.
- British Association of Dermatologists: Shingles (herpes zoster) PIL. 2020 May [accessed 2023 Jul]. https://www.bad.org.uk/pils/shingles-herpes-zoster/.
- Jiang Y, Zheng RX, Yu ZY, Zhang XW, Li J, Lan HD, Qiao SY, Han M, Cao HJ, Robinson N, Liu JP. Traditional Chinese medicine for HIV-associated acute herpes zoster: a systematic review and meta-analysis of randomized trials. Evid Based Complementary Altern Med. 2022;2022:1–12. doi:10.1155/2022/8674648.
- Forsberg IN, Comrie RW, Jenkins D, Jezuit D. Educational strategies to improve herpes zoster vaccination in older adults. J Health Commun. 2018;3:35. doi:10.4172/2472-1654.100145.
- Hurley LP, Lindley MC, Harpaz R, Stokley S, Daley MF, Crane LA, Dong F, Beaty BL, Tan L, Babbel C, Dickinson LM, Kempe A. Barriers to the use of herpes zoster vaccine. Ann Intern Med. 2010;152:555–60. doi:10.7326/0003-4819-152-9-201005040-00005.
- Lu X, Lu J, Zhang F, Wagner AL, Zhang L, Mei K, Guan B, Lu Y. Low willingness to vaccinate against herpes zoster in a Chinese metropolis. Hum Vaccin Immunother. 2021;17:4163–70. doi:10.1080/21645515.2021.1960137.
- Herpes Zoster Expert Consensus Working Group of Chinese Dermatologist Association. Consensus of Chinese experts on herpes zoster. Chin J Dermatol. 2018;51:403–8. doi:10.3760/cma.j.issn.0412-4030.2018.06.001.