ABSTRACT
This study assessed three Ad26.RSV.preF/RSV preF protein combinations, combining different Ad26.RSV.preF doses and naturally aged preF protein, representing the expected critical vaccine quality attributes close to release, around intermediate shelf-life (ISL) and near-presumed end-of-shelf-life (EoSL), as a way to evaluate the vaccine immunogenicity and safety throughout its shelf-life. A single dose of Ad26.RSV.preF/RSV preF protein vaccine was administered to adults 60–75 years of age. Solicited adverse events (AEs), unsolicited AEs, and serious AEs (SAEs) were assessed for 7-day, 28-day, and 6-month periods after vaccination, respectively. RSV preF-binding antibody concentrations and RSV neutralizing titers were measured 14 days post-vaccination as primary and secondary endpoints, respectively; binding antibodies were also measured 6 months post-vaccination. The RSV preF-binding antibody responses induced by Ad26.RSV.preF/RSV preF protein vaccine lots representing the critical quality attributes around ISL and near presumed EoSL were noninferior to the responses induced by the vaccine lot representing the critical quality attributes near release. The RSV preF-binding and RSV neutralizing antibody levels measured 14 days post-vaccination were similar across the 3 groups. RSV preF-binding antibody concentrations were also similar 6 months post-vaccination. Solicited AEs were mostly mild to moderate in intensity, and a decreased reactogenicity was observed from the Release group to the ISL and EoSL group. None of the reported SAEs were considered related to study vaccination. The study provided evidence of sustained immunogenicity and safety over the intended shelf-life of the Ad26.RSV.pref/RSV preF protein vaccine. The three vaccine lots had acceptable safety profiles.
Introduction
Respiratory syncytial virus (RSV) is a cause of severe respiratory disease globally: primarily in infants, where it can cause severe bronchiolitis, and in older adults, where RSV infections lead to a substantial disease burden, especially in people with underlying respiratory or cardiac conditions.Citation1,Citation2 Globally, in 2015, in adults ≥65 years of age, there were an estimated 1.5 million episodes of RSV acute respiratory infection in industrialized countries, of which approximately 14% led to hospitalization.Citation3 In the EU during two successive RSV seasons over 2017–2019, the incidence of RSV illness in persons ≥65 years was 4.2% and 7.2%, respectively.Citation4
The search for a vaccine against RSV identified the F protein in its prefusion conformation (preF) as a key antigen candidate, since preF is a primary target for neutralizing antibodies naturally induced during RSV infection.Citation5 Vaccines recently approved for protecting older adults against RSV-related lower respiratory tract disease (LRTD) are based on the RSV preF protein.Citation6,Citation7
The adenovirus type 26 (Ad26) vector was selected to express the preF protein (Ad26.RSV.preF) for its capacity to elicit strong and durable humoral immune responses as well as cellular immune responses in the target population of older adults.Citation8 Ad26.RSV.preF was in addition shown to be able to confer protection against RSV infection in healthy adults in a human challenge study.Citation9 The combination of the preF protein with Ad26.RSV.preF leads to a high humoral response associated with a strong cellular response, including stimulation of CD8+ T cells, Th1 cytokine production, and durability.Citation10,Citation11 The Ad26.RSV.preF/RSV preF protein vaccine was demonstrated to be protective against RSV-related LRTD in adults 65 years of age or older in a phase 2b proof-of-concept trial, with efficacy ranging 70% to 80%, based on different case-definitions.Citation12
To account for a potential decrease in potency of the Ad26.RSV.preF/RSV preF protein vaccine over time after release, this clinical study was undertaken to assess humoral immune responses to the Ad26.RSV.preF/RSV preF protein vaccine during and at the end of the intended shelf-life. Naturally aged Ad26.RSV.preF representative of commercial material was not available at the time; consequently, in line with guidance on stability specification for live viral vaccines,Citation13 a dilution approach was adopted. Formulations were based on a mathematical shelf-life model and previously obtained clinical data with this Ad26.RSV.preF/RSV preF protein vaccine with down-dosed vaccine lots (NCT04453202). On the other hand, naturally aged preF protein was available and was used. The three formulations evaluated presented the critical quality attributes, i.e. the infectivity of Ad26.RSV.preF and the trimer content of the RSV preF protein component, representative of release, intermediate, and end-of-shelf life.
Participants and methods
Participants and study design
This randomized, double-blind Phase 3 study was conducted from November 2021 to September 2022 at 12 sites in the United States. Adults 60–75 years of age, in stable health, were randomly assigned to one of three groups to receive Ad26.RSV.preF/RSV preF protein lots, either representative of release or intermediate shelf-life or end-of-shelf life. Participants were vaccinated over a period of 4 months, between 2 November 2021 and 4 March 2022.
Participants provided written informed consent before participation in the study and before any study procedure was performed. Clinical procedures were approved by the ethical committees of the study centers and complied with good clinical practice principles, in accordance with the Declaration of Helsinki.Citation14 The trial was registered at ClinicalTrials.gov (NCT05101486).
The co-primary objectives of the trial were to demonstrate the non-inferiority, in terms of the induced binding immune response 14 days after vaccination, of 2 Ad26.RSV.preF/RSV preF protein vaccine lots, representative of intermediate-shelf-life and of intended end-of-shelf-life, to a vaccine lot representative of near release. Secondary objectives were to assess neutralizing antibody responses to vaccination and the reactogenicity and safety of the vaccine lots administered.
Study vaccine
The study vaccine was made of two components: Ad26.RSV.preF, a recombinant, replication-incompetent, Ad26 vector encoding the RSV preF protein, and recombinant RSV preF protein. These were mixed prior to administration as a single injection (1.0 mL) in the deltoid muscle.
The potency of the Ad26.RSV.preF vaccine component was assessed as the infectivity of the viral vector, tested by a quantitative potency assay on HEK293 cells, and measured in infectious units (IU). The presumed shelf-life of Ad26.RSV.preF was 2 years stored at −20°C, followed by 2 years stored at 2–8°C. The Ad26.RSV.preF content was 1.0 × 1011 viral particles (vp) (corresponding approximately to 9.57 log10 infectious units [IU]) per dose for the “Release” vaccine lot, 2.5 × 1010 vp (corresponding approximately to 9.06 log10 IU) per dose for the “Intermediate shelf-life (ISL)” vaccine lot and 1.0 × 1010 vp (corresponding approximately to 8.66 log10 IU) per dose for the “End-of-shelf-life (EoSL)” vaccine lot.
The amount of RSV preF protein was 150 μg in all vaccine lots. Trimer content, assessed using SE-HPLC size exclusion high performance liquid chromatography, was expected to be ≥90% at release and ≥80% at end-of-shelf-life. The presumed shelf life of the preF protein was 4 years stored at 2–8°C. Three different lots of preF protein were used: a release lot, a lot naturally aged at 2–8°C representing the intermediate shelf-life (kept 33 months at 2–8°C before study start), and a naturally aged lot representing the presumed end of shelf-life (kept 42 months at 2–8°C before study start). Both vaccine components were stored at 4°C during the study vaccination phase, adding 4 months of storage at 2–8°C for participants vaccinated last.
Safety assessment
Adverse events (AEs), vital signs, and any abnormal physical examination findings were documented. Solicited and unsolicited AEs were recorded for 7 and 28 days after vaccination, respectively. The use of analgesic/antipyretic medication was recorded for 7 days post-vaccination. Data on SAEs were collected for 6 months after study vaccination. AEs were graded with an adapted FDA Toxicity Grading Scale for Healthy Adult and Adolescent Volunteers Enrolled in Preventive Vaccine Clinical Trials.Citation15
Thrombosis and thrombocytopenia syndrome (TTS), also known as vaccine-induced immune thrombotic thrombocytopenia (VITT), has been observed following vaccination with Janssen COVID-19 vaccine (Ad26.COV2.S). Ad26.RSV.preF utilizes the same non-replicative Ad26 vector as the Ad26.COV2.S vaccine but with a different transgene insert encoding the RSV preF protein. To capture any potential safety signal with the Ad26.RSV.preF/RSV preF protein vaccine in this study, any thrombotic event and/or thrombocytopenia were considered as Adverse Events of Specific Interest (AESIs). Cases with concurrent thrombocytopenia and thrombosis, and cases of thrombosis were considered as “qualified for assessment” and were to be further classified by level of certainty for TTS by an adjudication committee, composed of internal and external experts, according to case definitions from the Brighton Collaboration,Citation16 the Centers for Disease Control (CDC),Citation17 and the Pharmacovigilance Risk Assessment Committee, which is based on the proposal from NICE.Citation18 The adjudication committee also assessed the cases for relatedness to the vaccine.
Immunogenicity analyses
Venous blood samples were collected for assessment of humoral immune responses on Day 1, Day 15, and Day 183. Vaccine elicited RSV A preF-specific IgG concentrations constituted the trial primary endpoint and were measured at the 3 time points using a validated enzyme-linked immunosorbent assay (ELISA). The lower limit of quantification for this assay was 3.4 EU/L. Titers of RSV A2-specific neutralizing antibodies were analyzed as secondary endpoint and were measured at Day 1 and Day 15. These assays were performed as described earlier.Citation12
Statistical analyses
Sample size calculation was based on a 95% power to demonstrate non-inferiority for each primary endpoint comparison separately. This required a total of 236 evaluable participants per group. With this sample size, the overall power to demonstrate non-inferiority of the EoSL Group versus the Release Group as the second comparison in the hierarchy was at least 90%.
The primary population for the immunogenicity analyses was the Per Protocol Immunogenicity Set, which consisted of vaccinated participants with post-vaccination immunogenicity data available, excluding participants with major protocol deviations expected to impact the immunogenicity outcomes and samples collected out of window.
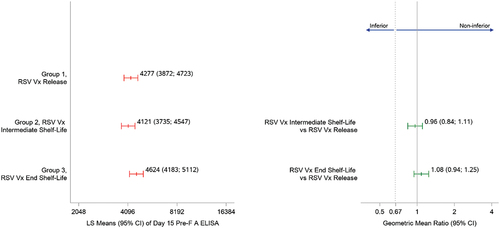
Geometric mean concentration (GMCs) of preF-binding antibodies and geometric mean titers (GMTs) of RSV-specific neutralizing antibodies were calculated per group with 95% confidence intervals (CIs). The primary immunogenicity objective was assessed by calculating the 2-sided 95% CIs for the difference in log2-transformed Day 15 RSV preF-binding antibody concentrations for each comparison to the Release group. The CIs were calculated via an ANOVA including all groups with log2-transformed Day 15 RSV preF-binding antibody concentrations as dependent variable and group as independent variable. The CIs around the difference were back-transformed to CIs around a geometric mean ratio (geometric mean concentration [GMC] ISL or EoSL group/GMC Release group). Non-inferiority was demonstrated if the 2-sided 95% CI for the GMR lied entirely above 0.67. The significance level (α) was 5% (2-sided). If the non-inferiority of the ISL Group versus the Release group was demonstrated, then non-inferiority of the EoSL group versus the Release group was tested. Secondary immunogenicity endpoints were analyzed descriptively.
The primary population for the safety analyses consisted of all vaccinated participants (Full Analysis Set) with safety data available after vaccine administration. Safety analyses were descriptive; the number and percentage of participants with at least one particular AE were tabulated.
Results
Demographics
A total of 752 adults 60–75 years of age were recruited and vaccinated (). The demographic and baseline characteristics were generally balanced across the groups (). Most participants were white and 55.3% were female. The mean age was 65.0 years (ranging from 60 to 75 years), and the mean body mass index was 30.34 kg/m2. Overall, 147 (20.3%) participants had an underlying medical condition (chronic heart and/or lung disease), placing them at increased risk for severe RSV disease.
Table 1. Summary of demographics and baseline characteristics.
Immunogenicity results
The co-primary objectives of the trial were met as the non-inferiority of the immune response induced by the lots representative of intermediate- and end-of-shelf-life to that induced by a lot at release was demonstrated. Indeed, the 95% CI around the GMR of RSV preF-binding antibody concentrations is above the non-inferiority limit of 0.67 for the ISL and for the EoSL groups as compared to the Release lot ().
Concentrations of RSV preF-binding antibodies were similar in the three groups at Day 15 (). Concentrations 6 months after vaccination were still 2.5-fold higher than those measured at baseline, with 1588 (95% CI: 1445; 1744) in the Release group, 1516 (95% CI: 1375; 1672) in the ISL group and 1562 (95% CI: 1428; 1709) in the EoSL group (Supplementary Table S1).
RSV neutralizing antibody GMTs at baseline were similar in the three groups, and increases at Day 15 were of comparable magnitude, ranging 6.5 to 7.3-fold (). Of note, RSV neutralizing antibody GMRs for the ISL group versus the Release group and for the EoSL group versus the Release group were 0.85 (95% CI: 0.72; 1.00) and 1.05 (95% CI: 0.89; 1.24), respectively (Supplementary Table S2). These ratios are comparable to those obtained for RSV preF IgG GMRs at Day 15.
Table 2. Titers of neutralizing antibodies to RSV A2 strain and fold increase from baseline.
Safety results
There was a trend toward decreased reactogenicity with increasing clinical trial material age (). In view of the similar trend observed with down-dosed Ad26.RSV.preF combined with non-aged preF protein,Citation11 this is likely due to the lower vp content of the Ad26.RSV.preF component in vaccine lots mimicking aged lots. In all groups, the most frequently reported solicited local AE was pain/tenderness (reported by up to 49.0% of participants) and the most frequently reported solicited systemic AEs were fatigue, headache, and myalgia (reported by up to 34.2% of participants for fatigue). The majority of solicited AEs were Grade 1 to 2 in severity, and all were transient in nature, with a median duration of 2 days at most. There was a trend toward a decreased use of analgesic/antipyretic medication from the Release group to the ISL and EoSL groups, likely attributable to the observed decreasing reactogenicity with decreasing Ad26.RSV.preF content.
Table 3. Frequency of solicited adverse events after vaccination.
Unsolicited AEs were reported by 6% to 9% of participants across the three study groups. Unsolicited AEs considered related to study vaccine by the investigator were reported by eight participants. These were chills, reported by three participants (1.2%) in the Release group; gastrointestinal disorders, reported by one participant in the Release group and one participant in the EoSL group; limb discomfort (1 participant in the ISL group), dizziness postural (1 participant in the Release group), and pruritus (1 participant in the EoSL group).
Overall, two deaths were reported during the study period. One (0.4%) due to unknown causes, occurred on Day 98 in the Release group and 1 (0.4%) cardiac arrest occurred on Day 88 in the EoSL group. Both deaths were considered not related to study vaccine by the investigator. A total of 16 SAEs were reported during the study: none was considered related to the study vaccine by the investigator. No participants discontinued the study due to an unsolicited AE. During the study, three AESIs were identified, including the two deaths described above and a myocardial infarction 152 days post vaccination which resolved timely; none was considered related to the study vaccine by investigators, and none qualified for further assessment by the TTS adjudication committee as there was no evidence of thrombocytopenia nor of thrombosis. There were no cases of vaccine-induced TTS in this study.
Discussion
This study was conducted to provide a clinical immunogenicity and safety assessment of the Ad26.RSV.preF/RSV preF protein vaccine administered during and at the end of its intended shelf-life. Naturally aged Ad26.RSV.preF representative of commercial material was not available at this time due to a process change and, in line with WHO guidance,Citation13 aging of the Ad26.RSV.preF vaccine component after release was mimicked by dilution of the vaccine to reproduce a decrease in potency (i.e. the infectivity of the viral vector measured in infectious units, IU) observed in real-time stability studies for storage at 2°C to 8°C, the foreseen storage conditions of commercial lots. Specific approaches were used to mimic the aging of the two vaccine components: i) dilution of Ad26.RSV.preF to reflect potency variation, estimated to be from 9.96 to 8.96 IU/mL throughout the shelf-life, which reflects the classical 0.5–1.0 Log loss reported for live viral vaccines; ii) use of naturally aged RSV preF protein, reflecting the expected decrease in trimer content over shelf-life. This approach allows to make inferences regarding immunogenicity and safety over the intended shelf-life of a vaccine and is a way to support the setting of the vaccine stability specifications.Citation13,Citation19
The primary objective of the trial was met, demonstrating the noninferiority of the vaccine-induced immune response during and at the end of the intended vaccine shelf-life to the response induced by the vaccine at release. There were no differences between groups in terms of RSV preF IgG serum antibody concentrations at Day 15 and no differences were observed either at Day 183. Neutralizing antibody titers against RSV, as measured at Day 15, were also similar in the three study groups. Collectively, these results provide evidence of a sustained immune response within the limits of the predicted Ad26.RSV.preF/RSV preF protein vaccine critical attributes throughout the intended shelf-life of the vaccine.
Reactogenicity in the Release Group was in line with previous reports with the Ad26.RSV.preF/RSV preF protein vaccine,Citation11,Citation12 displaying mainly mild-to-moderate intensity of both local and systemic solicited AEs. There was a trend toward a decreasing reactogenicity from the Release group to the Intermediate and End of Shelf-Life groups. In view of the similar trend observed with varying doses of Ad26.RSV.preF combined with non-aged preF protein,Citation11 this can likely be attributed to the decreasing titer in viral particles of the Ad26.RSV.preF vector. Of note, since no decrease in viral particle content is expected throughout shelf-life for the naturally aged vaccine, stable safety throughout shelf-life would be expected.
No SAEs were considered related to study vaccination, and no cases of vaccine-induced TTS were identified or reported during this study. VITT/TTS was considered as an AESI in this study since it has been very rarely observed among persons receiving Janssen’s Ad26.COV2.S COVID-19 vaccine (JCOVDEN®), the vaccine that shares the same platform technology with the Ad26.RSV.preF/RSV preF protein vaccine.Citation12 None of the study participants developed VITT/TTS post vaccination. To date, no cases of VITT have been identified in clinical trials using the Ad26.RSV.preF/RSV preF protein vaccine or any other Ad26-based vaccines besides JCOVDEN®. Collectively, these data demonstrated that the Ad26.RSV.preF/RSV preF protein vaccine was generally well tolerated and did not show any safety concern.
The three vaccine lots showed acceptable safety profiles throughout the 6-month post-vaccination follow-up, leading to infer a stable safety profile of the vaccine during its intended shelf-life.
Conclusions
This study provided evidence of an unimpaired, sustained immunogenicity of the Ad26.RSV.preF/RSV preF protein vaccine during its intended shelf-life in the older adult population targeted for vaccination against RSV, including persons at a higher risk of severe RSV disease due to underlying chronic conditions. There were no safety concerns in the study.
Data sharing statement
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
RSV3003 Supplementary Tables April 2024.docx
Download MS Word (15.4 KB)Acknowledgments
We thank all the study participants and their families, the study investigators and site personnel. Thanks also go to the Janssen study team (Annekatrien Menten, Mary Sweeney, Eric Shannon, Annette Cheeseman, Cristina Garbovan). We thank Jeanne-Marie Jacquet for medical writing support and Yvonne Salzgeber for publication coordination.
Disclosure statement
B.V.M. and R.H. are full-time employees of the study sponsor. W.H. is an employee of Cytel and works full time for the study sponsor. A.R.B., B.C., C.C., E.H., N.L., and T.H. were employees of the sponsor at the time of the trial.
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2344970.
Additional information
Funding
References
- WHO. Respiratory syncytial virus (RSV) disease. https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/respiratory-syncytial-virus-disease.
- Glezen WP, Taber LH, Frank AL, Kasel JA. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140:543–7. doi:10.1001/archpedi.1986.02140200053026.
- Shi T, Denouel A, Tietjen AK, Campbell I, Moran E, Li X, Campbell H, Demont, Nyawanda BO, Chu HY, et al. Global disease burden estimates of respiratory syncytial virus–associated acute respiratory infection in older adults in 2015: a systematic review and meta-analysis. J Infect Dis. 2020;222(S7):S577–83. doi:10.1093/infdis/jiz059.
- Korsten K, Adriaenssens N, Coenen S, Butler C, Ravanfar B, Rutter H, Allen J, Falsey A, Pirçon J-Y, Gruselle O, et al. Burden of respiratory syncytial virus infection in community-dwelling older adults in Europe (Resceu): an international prospective cohort study. Eur Respir J. 2021;57(4):2002688. doi:10.1183/13993003.02688-2020.
- Mazur NI, Higgins D, Nunes MC, Melero JA, Langedijk AC, Horsley N, Buchholz UJ, Openshaw PJ, McLellan JS, Englund JA, et al. The respiratory syncytial virus vaccine landscape: lessons from the graveyard and promising candidates. Lancet Infect Dis. 2018 Oct;18(10):295–311. doi:10.1016/S1473-3099(18)30292-5. Epub 2018 Jun 18.
- FDA. Abrysvo® package insert. https://www.fda.gov/vaccines-blood-biologics/abrysvo.
- FDA. Arexvy® package insert. https://www.fda.gov/vaccines-blood-biologics/arexvy.
- Williams K, Bastian AR, Feldman RA, Omoruyi E, De Paepe E, Hendriks J, van Zeeburg H, Godeaux O, Langedijk JPM, Schuitemaker H, et al. Phase 1 safety and immunogenicity study of a respiratory syncytial virus vaccine with an adenovirus 26 vector encoding prefusion F (Ad26.RSV.preF) in adults aged ≥60years. J Infect Dis. 2020;222(6):979–88. doi:10.1093/infdis/jiaa193.
- Sadoff J, De Paepe E, DeVincenzo J, Gymnopoulou E, Menten J, Murray B, Bastian AR, Vandebosch A, Haazen W, Noulin N, et al. Prevention of respiratory syncytial virus infection in healthy adults by a single immunization of Ad26.RSV.preF in a human challenge study. J Infect Dis. 2021 Jan 5;226:396–406. doi:10.1093/infdis/jiab003. Epub ahead of print. PMID: 33400792.
- Saeland E, Van der Fits L, Bolder R, Heemskerk-van der Meer M, Drijver J, Van Polanen Y, Vaneman C, Tettero L, Serroyen J, Schuitemaker H, et al. Combination Ad26.RSV.preF/preF protein vaccine induces superior protective immunity compared with individual vaccine components in preclinical models. NPJ Vaccines. 2023;8:45. doi:10.1038/s41541-023-00637-7.
- Comeaux C, Bart S, Bastian AR, Klyashtornyy V, De Paepe E, Omoruyi E, Van der Fits L, Van Heesbeen R, Heijnen E, Callendret B, et al. Safety, immunogenicity, and regimen selection of Ad26.RSV.preF–based vaccine combinations: a randomized, double-blind, placebo-controlled, phase 1/2a study. J Infect Dis. 2023;229:19–29. doi:10.1093/infdis/jiad220.
- Falsey AR, Williams K, Gymnopoulou E, Bart S, Ervin J, Bastian AR, Menten J, De Paepe E, Vandenberghe S, Chan EKH, et al. Efficacy and safety of an Ad26.RSV.preF-RSV preF protein vaccine in older adults. N Engl J Med. 2023;388:609–20. doi:10.1056/NEJMoa2207566.
- WHO. Guidelines on clinical evaluation of vaccines: regulatory expectations; 2017. WHO technical report series 1004, annex 9. https://www.who.int/publications/m/item/WHO-TRS-1004-web-annex-9.
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. doi:10.1001/jama.2013.281053.
- US Food and Drug Administration. Guidance for industry: toxicity grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials; 2007. https://www.fda.gov/media/73679/download.
- Brighton Collaboration. Interim case definition of thrombosis with thrombocytopenia syndrome (TTS); 2021. https://brightoncollaboration.us/thrombosis-with-thrombocytopenia-syndrome-interim-case-definition/.
- ACIP. Update: Thrombosis with thrombocytopenia syndrome (TTS) following COVID-19 vaccination 2021; updated 2021 May 12. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-05-12/07-COVID-Shimabukuro-508.pdf.
- NICE. Overview | COVID-19 rapid guideline: managing the long-term effects of COVID-19; 2020. https://www.nice.org.uk/guidance/NG188.
- ICH Q6B. Guidelines. https://www.ich.org/page/quality-guidelines.