?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
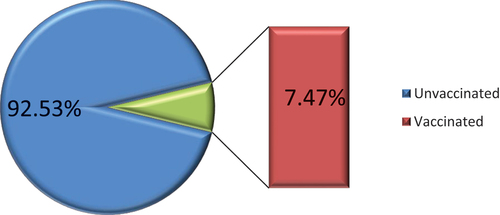
Cervical cancer is the fourth most common cancer, with 99% of cases linked to human papillomavirus (HPV) infection. It reflects global inequity as its burden is highest in low- and middle-income countries. The aim of this study was to determine the HPV vaccination coverage and its determinant factors among young women in the three sub-Saharan African countries. Data from the Demographic and Health Surveys among three sub-Saharan African countries were used for analysis. A total of 4,952 women were included in the study. Stata 14 was used to analyze the data. The determinants of the outcome variable were identified using a multilevel mixed-effects logistic regression model. Factors with p-values < 0.05 at 95% confidence interval were declared statistically significant. About 7.5% young women were vaccinated for HPV vaccine against cervical cancer in the current study. Younger age, use of internet, rich economic class, and individual-level media exposure were found to be favorable conditions, whereas being employed was negatively associated with HPV vaccination. Only few segments of young women in these three countries got HPV vaccination. The authors recommend that increasing internet use, media exposure, and economic level of young women will increase the HPV vaccination rates. Furthermore, creating awareness among employed women will also increase the possibility of HPV vaccination.
Background
Cervical cancer (CC) is the fourth most common cancer, with 99% of cases linked to human papillomavirus (HPV) infection.Citation1,Citation2 In the absence of HPV vaccination, the burden of CC is expected to reach 11.6 million by 2094.Citation1,Citation3 It reflects global inequity as its burden is highest in low- and middle-income countries, where access to community health facilities is limited and screening and treatments have not been broadly implemented.
Evidence shows a strong relationship between having multiple sexual partner, HPV infection, and CC development.Citation4 There are more than 100 types of HPV, of which at least 14 are cancer-causing. HPV is mainly transmitted through sexual contact, and most people are infected with shortly after the onset of sexual activity. Two HPV types (16 and 18) cause about 70% of CC and pre-cancerous cervical lesions.Citation5–7
Two effective prophylactic vaccines composed of HPV strains 16 and 18 are primary prevention strategiesCitation8 to reduce the disease burden. Strategies involving vaccinating girls aged 9–14 with two doses are predicted to be the most cost-effective in low- and middle-income countries. Evidence showed that routine immunization of girls at age 14 y and at age 9 y through a 5 y of extended interval between doses and a catch-up program at age 14 y are the most efficient to control CC.Citation9
World Health Organization (WHO) and other scholars recommend one- or two-dose schedule for girls aged 9–14 y, one- or two-dose schedule for girls and women aged 15–20 y, two doses with a 6-month interval for women older than 21 y, and more than two dose for immunosuppressed individuals.Citation10–12
Some barriers to HPV vaccination are low information about the vaccine, low awareness related to side-effects (syncope, pain, dizziness, nausea, headache), low involvement on decision-making, bad rumor, sex-related concerns, and infertility concerns. The price and low health insurance coverage in the low- and middle-income countries are also another cause that could limit access to the vaccine.Citation13–15
Initiatives to encourage later commencement of sexual intercourse and limiting the number of sexual partners would have a favorable impact on the risk of CC.Citation16 In addition, providing public education about safer sex practices, family planning, and eliminating cultural practices such as early marriage and polygamy are also the most important segments to reduce the disease morbidity and mortality.Citation17
Therefore, the current study aimed to determine HPV coverage against CC among young women and its associated factors in three sub-Saharan African (SSA) countries.
Methods and materials
Patient and public involvement statement
In this study, there was no public and patient involvement since the data were taken from Demographic and Health Surveys (DHS) dataset. The DHS is a community-based cross-sectional research carried out every 5 y in order to produce health and health-related indicators of low- and middle-income countries.
Study design, area, and period
Data from the 2015–2019/20 DHS available from the three SSA countries (Rwanda, Zambia, and Zimbabwe) were used to carry out the current study. Since the outcome variable is found only from these three countries, we could not include other countries in this region. The data were appended to figure out the coverage and contributing factors of HPV vaccination among young women (age group from 15 to 24 y). DHS uses two-stage stratified cluster design that includes enumeration areas as the first stage and generates a sample of households from each enumeration area as the second stage.Citation18 The variable “has card where HPV vaccination against CC are written” (s1110b) from the maternal record (IR) dataset was chosen and recoded to create the outcome variable. A total sample of 4,952 young women was included in this study ().
Table 1. Sample size for coverage and associated factors of HPV vaccine among young women in the three SSA countries.
Study variables
Dependent variables
In this study, the dependent variable was HPV vaccination against CC. It was coded as “Yes = 1” if the study participants had a card documenting HPV vaccinations against CC. On the other hand, it was coded as “No = 0” if the study participants did not have a card documenting HPV vaccinations against CC.
Independent variables
Since DHS data are hierarchical in nature, explanatory variables from two sources (at the individual and community levels) were considered. Individual-level variables were age (15–19, 20–4), education (no formal education, primary, secondary, and higher), partner education (no formal education, primary, secondary, and higher), occupation (unemployed, employed), marital status (never married, currently married, ever married), use of internet (yes, no), heard of family planning (yes, no), wealth index (poor, middle, rich), and media exposure (yes, no). At the community-level, place of residence (urban, rural), community illiteracy (low, high), level of poverty (low, high), and media exposure (low, high) were considered.
Data processing and statistical analysis
The data extracted from DHS datasets were recoded and analyzed using STATA version 14.0. Since DHS data are hierarchal in nature, other standard logistic regression models cannot account this hierarchal and intercluster variations. Therefore, the best fitted model was found to be multilevel mixed-effect logistic regression to determine the potential factors associated with HPV vaccination against CC. Multilevel mixed-effect logistic regression follows four models [(the null model (outcome variable only), mode I (individual level variables with the outcome variable), model II (community level variables with the outcome variable), and model III (both individual and community level variables with the outcome variable)]. The null model was used to check the variability of HPV vaccination across the clusters. In the final model (Model III), the association of both individual and community-level variables was fitted simultaneously with the outcome variable. Variables with p-values < 0.05 were considered statistically significant at 95% confidence interval. The results are presented using texts, tables, and figures.
Random effects
The proportional change in variance (PCV), intra-class correlation coefficient (ICC), and median odds ratio (MOR) were used to evaluate random effects. To quantify the difference across clusters, PCV and ICC were calculated. Taking clusters as a random variable, the ICC reflects the variation of HPV vaccination between clusters, and it is calculated as . The MOR describes the median value of the odds ratio between the highest risk and the lowest risk areas of HPV vaccination when two clusters are randomly selected and computed as MOR =
.
Furthermore, the PCV shows variation in the coverage of HPV vaccination explained through independent covariates, and it is obtained as, where Vnull = variance of the null model and VC is cluster-level variance. The fixed effects were used to estimate the association between the likelihood of HPV vaccination and individual- and community-level independent variables. Its strength was measured using adjusted odds ratio (AOR) and 95% confidence intervals with a p-value of < .05. Because of the nested nature of the model, deviation = −2(log likelihood ratio) was used to compare models, and the model with the lowest deviance was selected as the best-fit model.Citation18 The variables used in the models were verified for multi-collinearity using variance inflation factor (VIF) with mean VIF of 1.95.
Result
Sociodemographic characteristics of young women in the three SSA countries
Out of the total study participants, more than half (55.44%) are in 15–19 age groups. The majority (59.48%) of the participants completed secondary education or above, about two-thirds (67.74%) were employed, and nearly three-fourths (69.74) were unmarried. Only 18.67% were internet users, 35.61% were in poor economic class, and about 46% of the households had media exposure.
Regarding the community status, about two-thirds (64.41%) were living in the countryside, more than half (55.6%) were literate, nearly 53% were in low poverty level, and about 46% had high media exposure ().
Table 2. Sociodemographic characteristics of young women in the three SSA countries.
Prevalence of HPV vaccination coverage
The prevalence of HPV vaccination against CC in the current study is found to be 7.47% (95% CI: 6.77–8.24) ().
Random effect and model fitness
Findings from the null model showed that there were significant variations in HPV vaccination between communities, with a variance of 0.8591735 and a p value of 0.000. The variance within clusters contributed 85.22% of the variation in HPV vaccination, while the variance across clusters was responsible for 14.78% of the variation.
In the null model, the odds of HPV vaccination varied between higher- and lower-risk clusters by 2.41 times. The interclass correlation value for Model I revealed that 15.3% of the variation in HPV vaccination accounts for communities differences. Cluster variations were the basis for 17.1% of the differences in HPV vaccination based on the ICC value from Model II. The chance of HPV vaccination differed by 2.04 times between low and high clusters in the final model, which attributed roughly 33.34% of the variation in HPV vaccination likelihood to both individual- and community-level variables ().
Table 3. Model comparison and random effect analysis for HPV vaccination coverage among three SSA countries.
Association of individual- and community-level factors with HPV vaccination coverage against CC
Multilevel mixed-effect logistic regression model was used to identify the potential covariates that could affect the outcome variable. In the final model, the association of both individual- and community-level variables was fitted simultaneously with the outcome variable. In this model, variables with p-value less than < 0.05 with respected AOR were declared statistically significant.
In the final fitted model of multivariable, multilevel logistic regression analysis, age, use of internet, employment status, wealth index, and individual-level media exposure were significantly associated with HPV vaccination against CC ().
Table 4. Multivariable, multilevel logistic regression analysis of individual- and community-level factors associated with HPV vaccination among young women in sub-Saharan Africa.
The odds of HPV vaccination were about two times higher among women aged 15 to 19 y compared 20 to 24 y (AOR = 2.12, 95% CI (1.62–2.77)). HPV vaccination against CC was about 2.4 times more likely among women who used internet than those who did not (AOR = 2.38, 95% CI (1.80–3.15))
Women from the rich economic class were vaccinated with the HPV vaccine nearly 2.3 times more than those from poor economic level (AOR = 2.26, 95% CI (1.50–3.4)). Furthermore, the odds of HPV vaccination were found to be 1.4 times ((AOR = 1.39, 95% CI (1.07–1.81)) more likely for the women who had media exposure than their counterparts.
Another paradoxical finding of this study is that only 33% of employed women were vaccinated for HPV vaccine against CC (AOR = 0.67, 95% CI (0.51–.89)) ().
Discussion
The current study aimed to determine the HPV vaccination coverage against CC and its determinant factors in the three SSA countries using the DHS data.
The HPV vaccination coverage in this study was found to be about 7.5%, which is much lower than the expected coverage to reduce CC in this region and globally. The current finding was lower than studies conducted in different regions of the world where vaccination rates were 12.2%,Citation19 33.6% of high economic class countries,Citation20 but higher than the 2016 study results in low-income countries, which was 2.7%.Citation20
The possible reasons for these disparities could be that in high-income counties, there could be enough accessibility of the vaccine, good awareness about the disease and the vaccine, and good governmental support as compared to the low- and middle-income countries with low coverage of health insurance, minority status, mistrust of the healthcare system, and cultural influences on health-seeking behaviors and health-related decision-making.Citation21,Citation22
In the current study, younger age, using internet, household media exposure, high economic class, and employment status were significantly associated with HPV vaccination.
The probability of vaccination against CC was higher among young women under 20 y old. This finding is supported by different studies conducted in different settings.Citation23–25 The possible reason could be the perception of the community that the HPV vaccine is given only to individuals under 20 y old, especially those under 15.
Internet users among the participants had vaccinated more than non-users. The current finding is in line with other different studies.Citation26–28 The possible explanation for these findings could be that women who use internet can access more information about the advantage of the vaccine and the relationship between HPV and CC that might facilitate decision-making regarding vaccination.
Young women who are exposed to various forms of media such as television and radio were vaccinated for HPV against CC than their counterparts. Different studies also report similar findings.Citation29–31 This could be because those who watch television and listen to radio are more likely to be informed about the advantages of the vaccine and the devastating nature of CC, leading them to make the decision to get vaccinated compared to non-exposed women.
In the current study, women from higher economic class were vaccinated more than those from lower economic class. This is also supported by different literature sources.Citation32–34 This could be attributed to the fact that women from higher economic levels may have access to smartphones, television, radio, and other media platforms that provide information about the advantages of the vaccine over its disadvantages.
Conclusion and recommendations
In the current study, only about 7.5% of young women in SSA countries were vaccinated with the HPV vaccine against CC. Young age, internet use, media exposure, and higher economic level were found to be favorable factors, whereas being employed was a discouraging factor for HPV vaccination against CC.
The authors recommend that increasing internet usage, media exposure, and economic level of young women will increase the HPV vaccination rates. Creating awareness among employed young women will also increase the possibility of HPV vaccination. Furthermore, the governments of these countries could promote vaccination by providing accurate information about the vaccine using easily accessible meads, community campaign, and focal persons like community leaders and religious figures. It will be also important to increase health insurance coverage, waive the cost of the vaccine, and address harmful traditional practices like early marriage in order to increase vaccine uptake.
Limitations of the study
In the current study, only three countries were included, and this could not represent the vast categories of the SSA countries’ HPV vaccination status. Another limitation of this study is using 2015–2019/20 DHS data that would not represent the current vaccination status. This limitation could be addressed by considering the most recent data of each country using a qualitative study design/approach.
Author’s contributions
MW: involved in designing the study, data extraction, data analysis, interpretation, report and manuscript writing AFZ: involved in designing the study, data extraction, data analysis, interpretation, report and manuscript writing, TTT: involved in designing the study, interpretation, analysis, report and manuscript writing. EGM: involved in data analysis, interpretation, and manuscript writing, BT: involved in data extraction, and manuscript writing, GA: involved in data extraction and result interpretation, MSA: involved in data curation, formal analysis, methodology, ATG: involved in software, supervision, data validation, ATK: involved in conceptualization, validation, writing original draft, BSW: involved in review and editing, validation, visualization.
Availability of data and materials
The recent data from the Demographic and Health Surveys were used in this study, and it is publicly available online at (https://www.dhsprogram.com).
Ethical approval and consent to participate
After obtaining consent, the manuscript was submitted to the DHS Program/ICF to download the dataset for this investigation, and the International Review Board of Demographic and Health Surveys (DHS) program data archivists waived informed consent. Furthermore, the study’s dataset is from a publicly accessible source. All the methods were conducted according to the Helsinki Declarations. More details regarding DHS data and ethical standards are available online at http://www.dhsprogram.com.
Acknowledgments
We are grateful to the DHS program for letting us use the relevant DHS data in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bonjour M, Charvat H, Franco EL, Piñeros M, Clifford GM, Bray F, Baussano I. Global estimates of expected and preventable cervical cancers among girls born between 2005 and 2014: a birth cohort analysis. The Lancet Public Health. 2021;6(7):510–6. doi:10.1016/S2468-2667(21)00046-3.
- Vu M, Yu J, Awolude OA, Chuang L. Cervical cancer worldwide. Curr Probl Cancer. 2018;42(5):457–65. doi:10.1016/j.currproblcancer.2018.06.003.
- Abbas KM, van Zandvoort K, Brisson M, Jit M. Effects of updated demography, disability weights, and cervical cancer burden on estimates of human papillomavirus vaccination impact at the global, regional, and national levels: a PRIME modelling study. Lancet Glob Health. 2020;8(4):536–44. doi:10.1016/S2214-109X(20)30022-X.
- Huang Y, Wu X, Lin Y, Li W, Liu J, Song B. Multiple sexual partners and vaginal microecological disorder are associated with HPV infection and cervical carcinoma development. Oncol Lett. 2020;20(2):1915–21. doi:10.3892/ol.2020.11738.
- Organization WH. Human papillomavirus vaccines: WHO position paper, May 2017–Recommendations. Vaccine. 2017;35(43):5753–5.
- Okunade KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol. 2020;40(5):602–8. doi:10.1080/01443615.2019.1634030.
- Ma L, Lei J, Ma L, Cong X, Wang N, Yang H, Liu Q, Yu Y, Cao Y. Characteristics of women infected with human papillomavirus in a tertiary hospital in Beijing China, 2014–2018. BMC Infect Dis. 2019;19(1):1–8. doi:10.1186/s12879-019-4313-8.
- Berman TA, Schiller JT. Human papillomavirus in cervical cancer and oropharyngeal cancer: one cause, two diseases. Cancer. 2017;123(12):2219–29. doi:10.1002/cncr.30588.
- Drolet M, Laprise J-F, Martin D, Jit M, Bénard É, Gingras G, Boily M-C, Alary M, Baussano I, Hutubessy R, et al. Optimal human papillomavirus vaccination strategies to prevent cervical cancer in low-income and middle-income countries in the context of limited resources: a mathematical modelling analysis. Lancet Infect Dis. 2021;21(11):1598–610. doi:10.1016/S1473-3099(20)30860-4.
- Schwarz TF, Huang L-M, Valencia A, Panzer F, Chiu C-H, Decreux A, Poncelet S, Karkada N, Folschweiller N, Lin L, et al. A ten-year study of immunogenicity and safety of the AS04-HPV-16/18 vaccine in adolescent girls aged 10-14 years. Hum Vaccines Immunother. 2019;15(7–8):1970–9. doi:10.1080/21645515.2019.1625644.
- Mavundza EJ, Jaca A, Ndwandwe D, Cooper S. Facebook users’ attitudes towards human papillomavirus vaccination in South Africa. 2023.
- Whitworth HS, Gallagher KE, Howard N, Mounier-Jack S, Mbwanji G, Kreimer AR, Basu P, Kelly H, Drolet M, Brisson M, et al. Efficacy and immunogenicity of a single dose of human papillomavirus vaccine compared to no vaccination or standard three and two-dose vaccination regimens: a systematic review of evidence from clinical trials. Vaccine. 2020;38(6):1302–14. doi:10.1016/j.vaccine.2019.12.017.
- White MD. Pros, cons, and ethics of HPV vaccine in teens-Why such controversy? Transl Androl Urol. 2014;3(4):429–34. doi:10.3978/j.issn.2223-4683.2014.11.02.
- Brown B, Folayan M. Barriers to uptake of human papilloma virus vaccine in Nigeria: a population in need. Niger Med J. 2015;56(4):301. doi:10.4103/0300-1652.165033.
- Leidner AJ, Chesson HW, Talih M. HPV vaccine status and sexual behavior among young sexually-active women in the US: evidence from the national health and nutrition examination survey, 2007–2014. Health Econ Policy Law. 2020;15(4):477–95. doi:10.1017/S1744133119000136.
- Mekonnen AG, Mittiku YM, Linde DS. Early-onset of sexual activity as a potential risk of cervical cancer in Africa: a review of literature. PLOS Glob Public Health. 2023;3(3):e0000941. doi:10.1371/journal.pgph.0000941.
- Tadesse SK. Socio-economic and cultural vulnerabilities to cervical cancer and challenges faced by patients attending care at Tikur Anbessa hospital: a cross sectional and qualitative study. BMC Women’s Health. 2015;15(1):75. doi:10.1186/s12905-015-0231-0.
- Zegeye AF, Negash WD, Kassie AT, Wassie LA, Tamir TT, Gebrekidan K. Home delivery among women who had optimal ANC follow-up in sub-Saharan Africa: a multilevel analysis. PLOS ONE. 2023;18(11):e0295289. doi:10.1371/journal.pone.0295289.
- Spayne J, Hesketh T. Estimate of global human papillomavirus vaccination coverage: analysis of country-level indicators. BMJ Open. 2021;11(9):e052016. doi:10.1136/bmjopen-2021-052016.
- Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, de Sanjosé S, Castellsagué X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4(7):453–63. doi:10.1016/S2214-109X(16)30099-7.
- Thomas TL, Strickland OL, Higgins M. Mothers, fathers, sons, and human papillomavirus immunization practices. Fam Community Health. 2017;40(3):278–87. doi:10.1097/FCH.0000000000000104.
- Nolan J, Renderos TB, Hynson J, Dai X, Chow W, Christie A, et al. Barriers to cervical cancer screening and follow‐up care among black women in Massachusetts. J Obstetric, Gynecologic & Neonatal Nurs. 2014;43(5):580–8. doi:10.1111/1552-6909.12488.
- Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14(1):700. doi:10.1186/1471-2458-14-700.
- White MD. Pros, cons, and ethics of HPV vaccine in teens—Why such controversy? Transl Androl Urol. 2014;3(4):429–34. doi:10.3978/j.issn.2223-4683.2014.11.02.
- Cunningham MS, Davison C, Aronson KJ. HPV vaccine acceptability in Africa: a systematic review. Prev Med. 2014;69:274–9. doi:10.1016/j.ypmed.2014.08.035.
- Llavona-Ortiz JY, Spanos KE. Associations between human papillomavirus vaccine decisions and exposure to vaccine information in social media. Cancer Control. 2022;29:10732748221138404. doi:10.1177/10732748221138404.
- Dib F, Mayaud P, Longfier L, Chauvin P, Launay O. Effect of internet use for searching information on vaccination on the uptake of human papillomavirus vaccine in France: a path-analysis approach. Prev Med. 2021;149:106615. doi:10.1016/j.ypmed.2021.106615.
- Ortiz RR, Smith A, Coyne-Beasley T. A systematic literature review to examine the potential for social media to impact HPV vaccine uptake and awareness, knowledge, and attitudes about HPV and HPV vaccination. Hum Vaccines Immunother. 2019;15(7–8):1465–75. doi:10.1080/21645515.2019.1581543.
- Wubu A, Balta B, Cherie A, Bizuwork K. Perception about human papillomavirus vaccination among middle adolescent school girls in Addis Ababa, Ethiopia 2023: qualitative study. BMC Women’s Health. 2023;23(1):520. doi:10.1186/s12905-023-02660-1.
- Galvin AM, Garg A, Moore JD, Litt DM, Thompson EL. Quality over quantity: human papillomavirus vaccine information on social media and associations with adult and child vaccination. Hum Vaccines Immunother. 2021;17(10):3587–94. doi:10.1080/21645515.2021.1932219.
- Pan S, Zhang D, Zhang J. Caught in the crossfire: how contradictory information and norms on social media influence young women’s intentions to receive HPV vaccination in the United States and China. Front Psychol. 2020;11:548365. doi:10.3389/fpsyg.2020.548365.
- Zewdie A, Kasahun AW, Adane HA, Mose A. Willingness to vaccinate their daughters against human papillomavirus among parents of Ethiopian adolescent girls: a systematic review and meta-analysis. J Pharm Policy Pract. 2023;16(1):126. doi:10.1186/s40545-023-00639-9.
- Frianto D, Setiawan D, Diantini A, Suwantika AA. Economic evaluations of HPV vaccination in targeted regions of low- and middle-income countries: a systematic review of modelling studies. Int J Womens Health. 2022;14:1315–22. doi:10.2147/IJWH.S367953.
- Kim JJ, Goldie SJ. Health and economic implications of HPV vaccination in the United States. N Engl J Med. 2008;359(8):821–32. doi:10.1056/NEJMsa0707052.