Abstract
Objectives: Attendance at a specialist multidisciplinary motor neurone disease (MND) clinic is associated with improved survival and may also improve quality of life and reduce hospital admissions. However, patients struggle to travel to clinic and may experience difficulties between clinic visits that may not be addressed in a timely manner. We wanted to explore how we could improve access to specialist MND care. Methods: We adopted an iterative, user-centered co-design approach, collaborating with those with experience of providing and receiving MND care including patients, carers, clinicians, and technology developers. We explored the unmet needs of those living with MND, how they might be met through service redesign and through the use of digital technologies. We developed a new digital solution and performed initial testing with potential users including clinicians, patients, and carers. Results: We used these findings to develop a telehealth system (TiM) using an Android app into which patients and carers answer a series of questions about their condition on a weekly basis. The questions aim to capture all the physical, emotional, and social difficulties associated with MND. This information is immediately uploaded to the internet for review by the MND team. The data undergoes analysis in order to alert clinicians to any changes in a patient or carer’s condition. Conclusions: We describe the benefits of developing a novel digitally enabled service underpinned by participatory design. Future trials must evaluate the feasibility and acceptability of the TiM system within a clinical environment.
Background
Motor neurone disease (MND) causes a range of complications including limb weakness, dysphagia, dysarthria, and respiratory failure (Citation1). Patients with MND (which includes those with amyotrophic lateral sclerosis, primary lateral sclerosis, and progressive muscular atrophy) require substantial help with their activities of daily living. This is usually provided by informal carers who, along with patients, also experience significant physical, emotional, and financial burden (Citation2). It is recommended that MND care is provided by a multidisciplinary team of specialists who can address the complex and changing biopsychosocial needs of patients and their carers in order to maximize survival and quality of life (Citation3). Attendance at a multidisciplinary clinic (MDC) is associated with increased survival and greater use of assistive aids and proven treatments (Citation4–6). It offers the convenience of a single visit rather than multiple appointments and may also improve quality of life and reduce hospital admissions (Citation4,Citation7,Citation8). MDCs are usually centralized in hospitals and as the patient becomes more disabled, traveling to often-lengthy appointments becomes difficult. Even in developed countries, attendance at MDCs is not universal (between 43 and 85%), and some patients may only be able to attend once (Citation9). Community clinicians who provide care between visits have limited exposure to this rare disease so lack specialist experience and this can result in patients and carers experiencing significant difficulties (Citation10–15). Lack of coordinated care and advanced planning makes access to services such as palliative and social care more difficult (Citation16).
We wanted to improve access to specialist care during and between clinic visits and maintain an efficient service and considered whether digital technology could help. Telehealth systems collect information about a patient and relay it to the healthcare provider enabling problems to be detected and treatments monitored remotely (Citation17). MND lends itself well to telehealth because monitoring relies mainly on assessing a patient’s function and identifying distressing symptoms (such as breathlessness), much of which can be self-reported. Technology-enabled care has been used in a limited number of MND centers to monitor respiratory parameters but no system has been developed to monitor the other features of the disease (Citation17).
Telehealth is a complex intervention as it consists of multiple interacting components (Citation18). Components might include the technology, the way it is used by patients and clinicians and the service in which it is embedded. Successful telehealth relies on each of those interacting processes (Citation18). Previous trials of telehealth have experienced difficulties with acceptability and staff and patient uptake, highlighting the importance of designing new services with the end-user in mind (Citation19–21). This reflects the wider experience of new services where too often, the user-experience is unsatisfactory and this is largely because the technology and the way we interact with it is designed and developed in isolation of the service and its users (Citation22). User-centered co-design is an approach used for developing new systems or services which involves end-users in every stage of the development process (Citation23). Those who are likely to be affected by a new intervention or service have the right to a have a say in what that outcome is and participatory design helps users influence the design by offering their experience and unique perspectives and preferences (Citation23). It also ensures that the focus remains on the end-user (Citation24). These approaches have been successfully used in health service redesign (Citation25–27), to promote self-management (for example the Intelligent Shoe in stroke rehabilitation (Citation28,Citation29)) and in MND (patient-education websites (Citation30), and the Head-Up collar (Citation31)).
Methods
Aims
We aimed to:
Explore the current MND service, the unmet needs associated with access to specialist care, and how the service could be improved;
Identify opportunities by which technology-enabled service might be used to improve the service;
Use the results to develop the aims, scope, and content of technology that could be used in the MND service;
Perform initial testing with users;
Explore how the system might be evaluated.
The methods followed the Medical Research Council framework for development, evaluation, and implementation of complex interventions (Citation18). We used a range of iterative techniques occurring in parallel, using triangulation method to combine results. Investigator triangulation involved the three facilitators at the workshops providing written feedback all of which was reviewed by EH who then returned to the transcripts and audio-recordings to ensure all relevant themes identified were supported by the data. Data triangulation involved presenting results from each consultation process to trial management meetings to allow interpretation by the broader development team. Methods triangulation involved discussing themes identified from the early consultation work (informal presentations, the patient/carer interview, and discussions with clinicians) in the workshops to explore the range of ideas in more detail.
Service-user consultations
We consulted a range of people with experience of MND. Early ideas were presented at three meetings of a patient and public involvement group (the Sheffield MND Research Advisory Group (Citation32)) and two local MND Association charity meetings. Field notes were made and feedback was invited in person and by email. In addition, patient and one carer who lived at a distance from the MND center underwent a semi-structured interview using a topic guide which was audio-recorded, transcribed, and the themes identified using thematic analysis (Citation33). These meetings provided early feedback on the aims and scope of the project and informed the structure of the workshops that would explore the questions in more detail.
User-centered design workshops
Two workshops employing user-centered design techniques were conducted. Participants were recruited by word-of-mouth through the local MND Association charity, the MDC, and the Sheffield MND Research Advisory Group. Three males with MND, six carers or ex-carers (five female, one male), and an MND specialist nurse took part. Two patients attended with carers (both attended with their wives and one also brought his daughter) and one patient attended alone. Two patients used a wheelchair, one a scooter and all three had upper limb disabilities. One patient had speech difficulties but could communicate verbally with support from his wife.
INVOLVE patient and public involvement guidelines were followed (Citation34). Travel expenses, disabled parking, toilet facilities and refreshments were provided and carers were encouraged to participate to support those with MND. The workshops were facilitated by a clinician (EH), a specialist in user-centered design (RP) and a telehealth user experience designer. Time was allowed to ensure all participants could communicate using whichever means they preferred. A written feedback questionnaire was provided to participants at the end of the session. Written consent was obtained. Ethical approval was not required as the individuals were acting in an advisory role rather than as research participants (Citation34).
All workshops were audio-recorded. Field notes were made independently by the three facilitators and EH reviewed all the notes and recordings, transcribed relevant text and produced summary of each workshop describing the key themes, feedback, and comments.
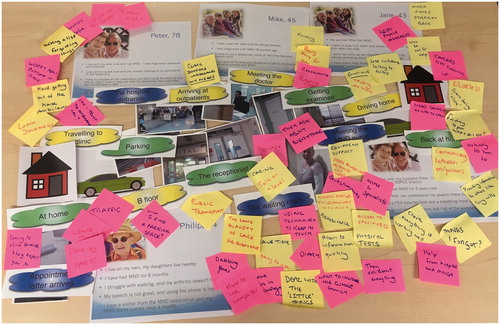
The two workshops were conducted as follows. An icebreaker session used puzzles and games to introduce the group and established aims and rules of the workshop. A patient journey mapping exercise explored participants’ experiences of attending an MDC appointment, their stories, emotions, and difficulties with services (). Participants arranged pictures and labels describing the stages of before, during, and after an MDC. By sharing their lived experience, this approach has proven successful as a prompt for further interrogation of the patient experience (Citation25). Personas (picture and descriptions of other examples of patients and carers (Citation35)) encouraged consideration for the experiences of others living with MND. Notes were made placed on the table to summarize the findings. A round-table activity involved individual participants explaining how they would use a tablet computer. This allowed participants to explain how MND affected them, their attitudes toward and barriers and enablers to using technology and telehealth, their experiences of clinical trials, and how these novel interventions could be used and tested. To encourage creativity and avoid constraining participants’ thinking, the proposed telehealth model was not shown to the participants at this stage. Instead, a cardboard square was used to represent a basic tablet computer and the participants were encouraged to explain how they would like to use or adapt the technology, however, impractical. This article prototyping uses the “good enough” model which allows an initial understanding of complex systems to be shared and experienced by users (Citation36). Participants tested a wire-frame HTML click-dummy mimicking an early version of a potential telehealth patient app. Facilitators could assess its ease of use and participants’ reactions to the system. Patients were videoed using the app. Concurrent think-aloud techniques encouraged participants to describe their thoughts as they interacted with the software and concurrent probing was used by facilitators to explore their ideas in more detail (Citation37).
Healthcare professional consultations
EH (specialist registrar in neurology) and CM (consultant neurologist with over 10-year experience in MND) led the development and consulted a wider group of clinicians (another MND specialist neurologist, a specialist neurology registrar, and four Sheffield MDC nurses/therapists). Results from the consultations were presented and discussed at regular meetings which helped refine the aims, scope, and feasibility of an improved service. Clinicians later reviewed telehealth content and the software. To obtain the views of those outside the MDC, a community specialist MND occupational therapist underwent an audio-recorded semi-structured interview. Two home visitors who volunteered for the Motor Neurone Disease Association reviewed the Patient App and provided written feedback. In parallel, reviews of the literature were conducted to identify existing best practice, the unmet needs of those living with MND, the potential uses of digital technology and the barriers and enablers to a successful service (Citation17,Citation38).
Developing the TiM software
Regular meetings enabled project leads to understand the abilities and limitations of telehealth. Meanwhile, the telehealth developers learned about the needs of the service and its users particularly in the unique context of MND. Specifications of the telehealth service were defined including:
The information a clinician gains from a patient and carer in MDC assessment and how this could be captured;
The frequency of monitoring;
The clinical algorithms which would analyze the data and alert clinicians to problems;
The way in which the patient, carer and MND clinicians would interact with system.
A click dummy was tested during the user consultations. This meant modification could be made in response to feedback prior to coding. The Clinical Portal displaying the patient/carer answers was then developed and beta-tested by clinicians who used the software and entered different answers several times into the app to detect faults in the software or clinical algorithms.
Results
The main themes identified in the consultations with patients, carers, clinicians, and volunteers were:
The importance of coordinated, accessible MND care;
The desire for information to help people cope with MND;
The acceptability of telehealth and remote monitoring;
The value of patient-reported information in remote monitoring;
The potential impact of telehealth.
1) The importance of coordinated, accessible MND care
All those consulted felt that there was a need to improve access to MDC. They identified valuable aspects of the MDC including access to evidence-based treatments and trials, monitoring of the clinical progress (through questions and physical examination) and the provision of specialist information.
Without coming to clinic you are left in the dark. Patient, user-centered design workshop.
The interpersonal aspect of MDC was also important: participants valued the ability to be able to talk to experts who could understand and solve their (often complex) problems as well as provide empathy and reassurance.
It’s nice to be told you’re doing well. Patient, user-centered design workshop.
Difficulty accessing care outside the MDC were also identified. Patients and carers reporting having to deal with multiple different community healthcare professionals who often lacked the specialist knowledge and coordination required to manage MND, particularly for issues unique to neurological disease, such as wheelchairs, gastrostomy tubes, and ventilation equipment.
Everything seems to take at least three months to sort out, which is frustrating… There’s nobody that seems to take control of the situation. Patient, interview.
Carers had to become experts themselves in order to assume the responsibility for managing these problems, particularly out-of-hours.
A lot of time you were left on your own. Ex-carer, user-centered design workshop.
2) The desire for information to help people cope with MND
Whilst participants relied heavily on healthcare professionals, all stakeholders felt more information and signposting should be available to help them self-manage their condition. Difficulties posed by the nature of the hospital-based service model including traveling to MDC (described as stressful and tiring), the inflexible nature of MDC appointments, and rapidly changing nature of the disease. This meant patients suffered delays in identification and treatment of new problems and worried that a deterioration in their condition could lead to avoidable emergency hospital admissions.
I waited so long for this special chair that by the time it arrived I had got worse and couldn’t use it.
Patient, user-centered design workshop.
3) The acceptability of telehealth and remote monitoring
The principle of telehealth: that is, using patient/carer questionnaires to enable the MND specialist team to remotely monitor them was felt to be acceptable to patients and their carers. Patients thought that telehealth could reduce the need for patients to attend the clinic if they were stable and currently needed no MDC input and could allow the MDC to remain in contact with those unable to attend clinic.
4) The value of patient-reported information
We identified problems that could be monitored and once identified could be addressed by the MDT by treatment, signposting or education such as:
Disease progression;
Complications of MND that might impact on survival, quality of life, or result in a hospital admission;
Problems with specialist equipment;
Carer difficulties.
5) The potential impact of telehealth
Potential benefits of telehealth identified were identified. These included earlier management of problems which might lead to improved clinical outcomes (quality of life and survival) and reduced unnecessary health encounters. Better coordination might mean patients can access the clinician best placed to address the problem, rather than having to first consult non-specialist clinicians.
The TiM system
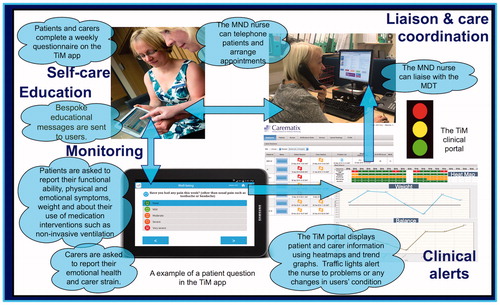
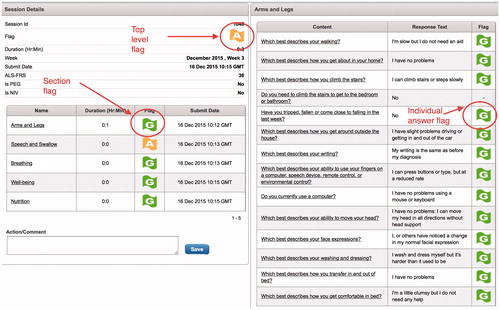
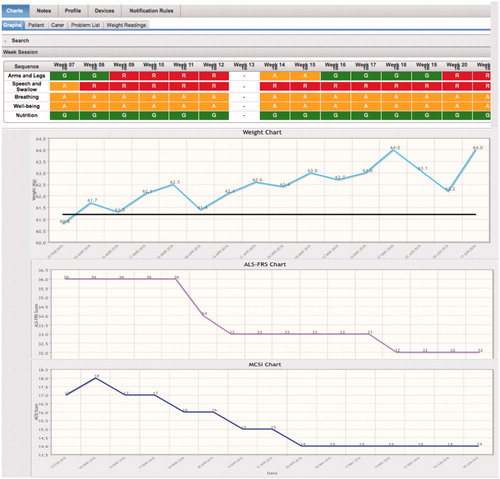
The Telehealth in Motor neurone disease (TiM) system was developed. A Patient App sends information to a Clinical Portal (a website accessible to the MDC team) (). Pre-defined clinical algorithms assign the information a flag (green, amber, and red). Clinicians can review the answers and initiate interventions as required. Information is transferred anonymously using only the device IMEI identifier and stored on a secure server using two-factor identification access. The TiM system was not designed to manage emergency situations: a message at the end of the TiM session reminds the user to contact a healthcare professional in these circumstances.
The Patient App
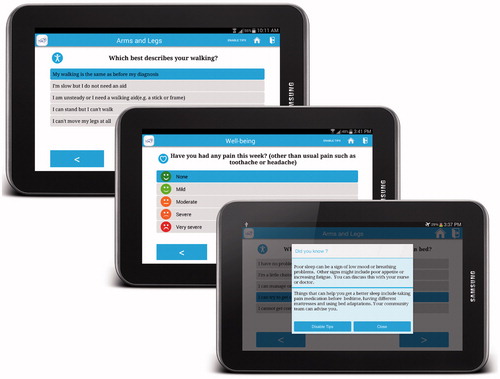
The Patient App is an Android software application designed to be used on a 7-inch tablet computer (). It asks patients and their carer a series of weekly questions. Additional questions appear if patients use non-invasive ventilation, a gastrostomy or report complications. The questions cover all aspects of MND: “Arms and Legs”, “Speech and swallow”, “Breathing”, “Wellbeing” and “Nutrition”. Some questions closely match validated scoring scales (for example the depression and anxiety short screening tool PHQ-4 or the ALS functional rating scale (Citation39,Citation40)). Other questions were designed for the TiM using direct questions or symptom severity scales (). Carers have separate questions which are accessed through a separate login assessing carer strain, depression, and anxiety. The TiM also receives data from Wi-Fi-enabled scales collecting weight and a measure of standing balance. Additional physical biomarkers (such as blood pressure or pulse oximeter) were not included because the team concluded that their value to routine MND care was limited.
The Clinical Portal
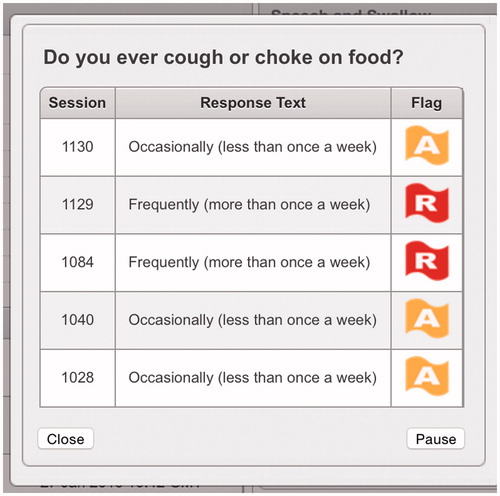
Information from the Patient App is immediately uploaded to the internet and displayed on a web-based Clinical Portal for MDC clinicians (). A flag (red, amber, and green) is generated for each question based on predefined clinical algorithms. Flags highlight significant or sustained changes in the patient/carer condition or the presence of serious complications (such as choking). The portal displays a summary for each patient and carer, all flags raised, and individual answers from each question. Additions were added later: a “Heatmap” page which provides a visual display of historical flags and trends in scores (ALS-FRS-R, weight, balance, and carer strain) () and a facility to review the previous six answers and pause flags ().
The impact of user-centered design on the TiM
The user-centered design workshop participants all agreed that they could make their opinions heard and that they would attend another event. One liked “the interactive element, stimulated lots of discussion”, another thought the session was “very informative and good to be involved in research”. The participatory design process influenced TiM development. Participants reported a strong desire to learn more about the disease to help people cope so we added screens in the app providing signposting and information about self-management () and a section to enable patients to record problems they wish to discuss. Developers observed patients with upper limb weakness and fatigue using the software and understood how this impacted on the use of the app. As a result, the touch-screen layout was redesigned to reduce the amount of hand movement that was required to complete the questionnaire. The usability testing later demonstrated that the Patient App could be completed quickly, even by those with moderate arm weakness or fatigue.
The consultations explored whether using telehealth to assess sensitive topics was likely to be acceptable. Clinicians were concerned that patients would be distressed if presented with answers that described the most severe stages of MND (such as being unable to swallow). However, patients and carers welcomed the thorough assessment of the impact of MND on their lives and confirmed that they were happy to answer questions on sensitive topics. They explained they were already aware of the implications of MND and that they were not distressed by seeing the full range of answers. Furthermore, they preferred to see all the possible answers because they thought that presenting only a limited number of options might make them give incorrect answers. In response, we changed the question structure to include all possible answers (see for an example). This had the added benefit of reducing the total number of questions thus shortening the time taken to complete the TiM system.
Discussion
There is clear evidence that specialist MND care brings benefits to patients but all participants in this project felt that access to this care needs to be improved. This early work has established ways in which technology could be used to improve MND care by facilitating monitoring, communication and care coordination, and this could offer improved outcomes. Despite their frailty, our participants highlighted their desire to learn about and self-manage their disease and telehealth offers the opportunity to improve health literacy, shared decision making, and self-management (which might be associated with improved self-efficacy (Citation41)). Self-management programs are being promoted as a cost-effective response to the challenges imposed by a population with increasing age and co-morbidities (Citation22). This is particularly relevant to MND given the prospect of new therapies that prolong survival meaning pressure on the already limited MND services will increase. Telehealth may be even more vital in countries with more highly dispersed populations or in resource-poor areas where patients do not have the means to travel to regional centers. These services may also compliment other forms of technology-enabled care, such as video consultations which are already used in some MDCs (Citation17,Citation42,Citation43).
Our experience demonstrates the benefits of user-centered co-design. The use of creative visual methods enabled rich conversations between diverse groups (Citation44). Capturing the current and desired experiences of users helped us understand what is important to an MND service and what could be improved. Involving clinicians meant the system retained focus on delivering evidence-based best-practice within the constraints of the real-world setting. Enabling developers to work with patients and carers meant they had a better understanding of the difficulties faced by those with MND and could work together to modify and test solutions. An unexpected benefit of this collaboration was that participants were also able to allay clinicians’ concerns about using technology to assess sensitive problems. Finally, as was previously observed when developing the Head-Up collar (Citation31), we hope that co-design participants will become advocates of the product, increasing the likelihood of wider “buy-in”.
Limitations
This project involved a small number of those with experience of MND, most of whom only had experience of the Sheffield MDC. However, it did include other participants who had not attended an MDC or who faced barriers to access. Crucially, it involved participants with years of experience visiting families living with MND. They provided insights into the views of less-heard groups, such as those who could no longer attend clinic. This project has stimulated further research that suggested that the positive attitudes to technology are shared with a larger sample of patients and carers (Citation45). The major limitation of designing of a digital product is the need to for multiple changes. There are time and financial constraints to development, particularly when involving users in the way we did. Whilst our iterative design process did allow changes to be made to the scope and content of the service before the technology was coded, after that time, changes become more difficult to implement. The rapid improvement in technology and changes in the health service itself mean improved and upgrades must be planned at each stage of the design process.
The TiM system now needs to be evaluated in a real-life setting. This project helped identify some of the uncertainties that need addressing including how the TiM system will be used in real-life, the use by those facing barriers, such as severe disability or a lack of digital literacy and the impact TiM has on users and the service itself. This project identified some aspects of MND care that are important to patients and clinicians but are difficult to recreate using digital technology (such as interpersonal relationships and physical examinations) and future evaluations should address whether telehealth can deliver a good standard of care despite these constraints. Evaluations should not only aim to measure the impact of the TiM but should also help establish how a successful telehealth service could be widely implemented by exploring the processes that occur during service change and identifying the barriers and facilitators to service improvement (Citation46,Citation47).
Conclusion
We used user-centered design to develop a novel system which could facilitate access to specialist care. It is strongly recommended that this approach involving all those involved in the receipt and delivery of care are used whenever a new intervention or service is developed in order to increase the chances of success.
Declaration of interest
The authors declare no individual conflict of interest. The TiM system intellectual property is jointly owned by Mylan and the University of Sheffield.
The development of the TiM was supported and funded by Cogent Healthcare Systems, Abbott Healthcare Limited, and Mylan. The project was funded by the National Institute for Health Research (Academic Clinical Fellowship and DRF-2013-06-076 to EH) and an NIHR Research Design Service for Yorkshire and the Humber (RDS YH) Patient and Public Involvement grant. Support was received from the NIHR CLAHRC Yorkshire and Humber, Sheffield Hallam University, Lab4Living, Sheffield Teaching Hospitals, NHS Foundation Trust Motor Neurone Disease Care, and Research Centre and Devices4Dignity. EH is also funded by an NIHR Clinical Lecturer award. PJS is supported by NIHR Senior Investigator award NF-SI-0512-10082 and PJS and CMD by the NIHR Sheffield Biomedical Research Centre (Translational Neuroscience IS-BRC-1215-20017). SM is funded and supported by NIHR CLAHRC Yorkshire and Humber (IS-CLA-0113-10020) and the RfPB Grant PB-PG-0214-33067. WB is funded and supported by NIHR RDS YH PR-RD-0312-10004 and the PGfAR RP-PG-0514-20013. This article presents independent research funded by the National Institute for Health Research (NIHR) and Research Trainees Coordinating Centre. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Additional information
Funding
References
- McDermott CJ, Shaw PJ. Diagnosis and management of motor neurone disease. BMJ. 2008;336:658–62.
- Mockford C, Jenkinson C, Fitzpatrick R. A review: carers, MND and service provision. Amyotroph Lateral Scler. 2006;7:132–41.
- National Institute for Clinical Excellence (UK). Motor neurone disease: assessment and management. London: National Institute for Clinical Excellence; 2016:1–47.
- Chio A, Buffa C, Mutani R, Bora G., PARALS. Positive effects of tertiary centres for amyotrophic lateral sclerosis on outcome and use of hospital facilities. J Neurol Neurosurg Psychiatry. 2006;77:948–50.
- Aridegbe T, Kandler R, Walters SJ, Walsh T, Shaw PJ, McDermott CJ. The natural history of motor neuron disease: assessing the impact of specialist care. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:13–9.
- Rooney J, Byrne S, Heverin M, Tobin K, Dick A, Donaghy C, et al. A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry. 2015;86:496–501.
- Van den Berg JP, Kalmijn S, Lindeman E, Veldink JH, de Visser M, Van der Graaff MM, et al. Multidisciplinary ALS care improves quality of life in patients with ALS. Neurology. 2005;65:1264–7.
- Stephens HE, Young J, Felgoise SH, Simmons Z. A qualitative study of multidisciplinary ALS clinic use in the United States. Amyotroph Lateral Scler Frontotemporal Degener. 2015;17:55–61.
- Hogden A, Foley G, Henderson R, James N, Aoun S. Amyotrophic lateral sclerosis: improving care with a multidisciplinary approach. J Multidiscip Healthc. 2017;10:205–15.
- Whitehead B, O’Brien MR, Jack BA, Mitchell D. Experiences of dying, death and bereavement in motor neurone disease: a qualitative study. Palliat Med. 2012;26:368–78.
- O’Brien MR, Whitehead B, Murphy PN, Mitchell JD, Jack BA. Social services homecare for people with motor neurone disease/amyotrophic lateral sclerosis: why are such services used or refused? Palliat Med. 2012;26:123–31.
- Foley G, O’Mahony P, Hardiman O. Perceptions of quality of life in people with ALS: effects of coping and health care. Amyotroph Lateral Scler. 2007;8:164–9.
- Baxter SK, Baird WO, Thompson S, Bianchi SM, Walters SJ, Lee E, et al. The use of non-invasive ventilation at end of life in patients with motor neurone disease: a qualitative exploration of family carer and health professional experiences. Palliat Med. 2013;27:516–23.
- Peters M, Jenkinson C, Doll H, Playford ED, Fitzpatrick R. Carer quality of life and experiences of health services: a cross-sectional survey across three neurological conditions. Health Qual Life Outcomes. 2013;11:1.
- van Teijlingen ER, Friend E, Kamal AD. Service use and needs of people with motor neurone disease and their carers in Scotland. Health Soc Care Community. 2001;9:397–403.
- O’Brien M, Whitehead B. Optimisation of service for people with Motor Neurone Disease (MND) in Lancashire and South Cumbria. 2010. [Internet] Available at https://www.edgehill.ac.uk/eprc/files/2011/08/Optimisation-of-services-for-people-with-MND.-Executive-summary-July-2010.pdf]
- Hobson EV, Baird WO, Cooper CL, Mawson S, Shaw PJ, McDermott CJ. Using technology to improve access to specialist care in amyotrophic lateral sclerosis: a systematic review. Amyotroph Lateral Scler Frontotemporal Degener. 2016;17:313–24.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new medical research council guidance. BMJ. 2008;337:a1655.
- Sanders C, Rogers A, Bowen R, Bower P, Hirani S, Cartwright M, et al. Exploring barriers to participation and adoption of telehealth and telecare within the whole system demonstrator trial: a qualitative study. BMC Health Serv Res. 2012;12:1–12.
- Bentley CL, Mountain GA, Thompson J, Fitzsimmons DA, Lowrie K, Parker SG, et al. A pilot randomised controlled trial of a Telehealth intervention in patients with chronic obstructive pulmonary disease: challenges of clinician-led data collection. Trials. 2014;15:313.
- MacNeill V, Sanders C, Fitzpatrick R, Hendy J, Barlow J, Knapp M, et al. Experiences of front-line health professionals in the delivery of telehealth: a qualitative study. Br J Gen Pract. 2014;64:e401–7.
- Chamberlain P, Mawson S, Wolstenholme D. Services: service design in chronic health. In: Tsekleves E, Cooper R, eds. Design for health. Design for social responsibility. Abingdon: Routledge; 2017:216–40.
- De Vitto Dabbs A, Myers BA, Mc Curry KR, Dunbar-Jacob J, Hawkins RP, Begey A, et al. User-centered design and interactive health technologies for patients. CIN. 2009;27:175–83.
- Carroll JM, Rosson MB. Participatory design in community informatics. Design Studies. 2007;28:243–61.
- Wolstenholme D, Cobb M, Bowen S, Wright P, Dearden A. Design-led service improvement for older people. Australas Med J. 2010;3:465–70.
- Wolstenholme D, Ross H, Cobb M, Bowen S. Participatory design facilitates person centred nursing in service improvement with older people: a secondary directed content analysis. J Clin Nurs. 2017;26:1217–1225.
- Bowen S, Sustar H, Wolstenholme D, Dearden A. Engaging teenagers productively in service design. Int J Child Comput Interact. 2013;1:71–81.
- Mawson S, Nasr N, Parker J, Zheng H, Davies R, Mountain G. Developing a personalised self-management system for post stroke rehabilitation; utilising a user-centred design methodology. Disabil Rehabil Assist Technol. 2014;9:521–8.
- Mawson S, Nasr N, Parker J, Davies R, Zheng H, Mountain G. A personalized self-management rehabilitation system with an intelligent shoe for stroke survivors: a realist evaluation. JMIR Rehabil Assist Technol. 2016;3:e1–12.
- White S, Hobson EV, Soreny C. The development of the myTube website. CN Focus. 2017;9:47–50.
- Reed H, Langley J, Stanton A, Heron N, Clarke Z, Judge S, et al. Head-Up; an interdisciplinary, participatory and co-design process informing the development of a novel head and neck support for people living with progressive neck muscle weakness. J Med Eng Technol. 2014;39:404–10.
- Sheffield Motor Neurone Disease Research Advisory Group [Internet]. 2017. [cited 2017 Dec 6]; Available at: http://smndrag.group.shef.ac.uk
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
- Health Research Authority. INVOLVE. Public involvement in research and research ethics committee review. London: Health Research Authority; 2016:1–4.
- Stickdorn M, Schneider J. This is service design thinking. Amsterdam: Bis Publishers; 2012.
- Ehn P. Work-oriented design of computer artifacts. Stockholm: Arbetslivscentrum; 1989.
- Ericsson KA, Simon HA. Protocol analysis. Cambridge, MA: MIT Press; 1993.
- Hobson EV, McDermott CJ. Supportive and symptomatic management of amyotrophic lateral sclerosis. Nat Rev Neurol. 2016;12:526–38.
- Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–21.
- Montes J, Levy G, Albert S, Kaufmann P, Buchsbaum R, Gordon PH, et al. Development and evaluation of a self-administered version of the ALSFRS-R. Neurology. 2006;67:1294–6.
- Jones F, Mandy A, Partridge C. Changing self-efficacy in individuals following a first time stroke: preliminary study of a novel self-management intervention. Clin Rehabil. 2009;23:522–33.
- Selkirk SM, Washington MO, McClellan F, Flynn B, Seton JM, Strozewski R. Delivering tertiary centre specialty care to ALS patients via telemedicine: a retrospective cohort analysis. Amyotroph Lateral Scler Frontotemporal Degener. 2017;18:324–32.
- Andrew G, Courtney W, Anne M, Susan W, Bethany S, Zachary S. Incorporation of telehealth into a multidisciplinary ALS Clinic: feasibility and acceptability. Amyotroph Lateral Scler Frontotemporal Degener. 2017;0:555–61.
- Cooke J, Langley J, Wolstenholme D, Hampshaw S. “Seeing” the difference: the importance of visibility and action as a mark of “Authenticity” in co-production comment on “Collaboration and co-production of knowledge in healthcare: opportunities and challenges”. Int J Health Policy Manag. 2016;6:345–8.
- Hobson EV, Fazal S, Shaw PJ, McDermott CJ. “Anything that makes life’s journey better.” Exploring the use of digital technology by people living with motor neurone disease. Amyotroph Lateral Scler Frontotemporal Degener. 2017;34:1–10.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350:h1258.
- Pawson R, Tilley N. Realist evaluation. Thousand Oaks, CA: Sage; 2004.