Abstract
Objective: To evaluate the use of telehealth as part of specialized care for patients with amyotrophic lateral sclerosis (ALS) and the user experiences of patients and healthcare professionals. Methods: Fifty patients with ALS were recruited from a single specialist center and used telehealth, consisting of an ALS-app for self-monitoring and messaging, alerts for symptom-worsening, and nurse practitioner follow-up. Patients self-monitored their well-being (daily report), body weight (weekly) and functional status (monthly). The use of the telehealth service was evaluated through adoption rate, dropout rate and adherence to self-monitoring. User-experiences were collected through online surveys among 23 patients and nine healthcare professionals, and interviews with 12 patients. Results: The adoption rate was 80%, dropout rate 4% and median follow-up was 11 months. Good adherence was seen in 49% of patients for well-being, 83% for body weight and 87% for functional assessment. For patients who discontinued using telehealth due to the end-of-life phase, median time between last measurement and death was 19 days. The majority of patients experienced using telehealth as easy, helpful, not burdensome, and reported satisfaction with flexible clinic visits and the continuity of care. Healthcare professionals reported that telehealth was of added value in ALS-care. Conclusions: ALS-care supplemented by home-monitoring and nurse practitioner follow-up was shown to be suitable and widely accepted by patients and healthcare professionals in our ALS clinic. Success factors were low self-monitoring burden, a user-friendly platform and the provision of personalized feedback. Further research is needed to replicate these findings in other ALS clinics.
Introduction
A multidisciplinary specialist team approach in the management of amyotrophic lateral sclerosis (ALS) is the gold standard of care, aimed at improving quality of life and survival through symptom management (Citation1). Currently, however, patients experience considerable barriers and burden related to multidisciplinary clinic (MDC) attendance, every three to four months. Travel barriers, such as long distances and limited mobility, and long exhausting clinic days due to seeing multiple healthcare professionals, have been reported as disadvantages of MDC attendance (Citation2,Citation3).
A possible solution for these issues is the use of telehealth. Telehealth has the potential to supplement in-person specialist care by allowing patients with ALS to be monitored and receive personalized advice and information in the comfort of their own home through telecommunication technologies. In contrast to in-person specialist care, access to telehealth is independent of patients’ ability to travel or distance from a MDC. In addition, telehealth facilitates remote monitoring of patients between clinic visits, which is currently lacking in ALS care. The remote monitoring of disease progression could help the multidisciplinary care team to tailor care and information to the ever-changing needs of patients with ALS.
In co-creation with patients, caregivers, healthcare professionals, managers and information technologists, we developed the telehealth service ALS Home-monitoring and Coaching. A pilot study (N = 10) in 2016 confirmed its feasibility (Citation4). On 1st May 2017, the telehealth service was implemented in specialist care at the ALS clinic of the University Medical Center Utrecht, the Netherlands, where patients with motor neuron disease receive multidisciplinary care. The telehealth service has been used for over 18 months and patients with ALS were invited to use it as part of their care.
The aim of this study is to evaluate the use of ALS Home-monitoring and Coaching in specialist ALS care, and the user experiences from the perspectives of patients and healthcare professionals.
Materials and methods
Study design, setting and population
This prospective single center cohort study was performed at the specialized ALS clinic in Utrecht. The catchment area was the province of Utrecht, with a maximum travel distance of 50 km. All patients with ALS who received multidisciplinary care at the ALS clinic between May 2017 and November 2018 were eligible for inclusion. During a regular visit to the multidisciplinary clinic, a rehabilitation physician invited patients to use telehealth. Patients who participated were followed up until 28th November 2018.
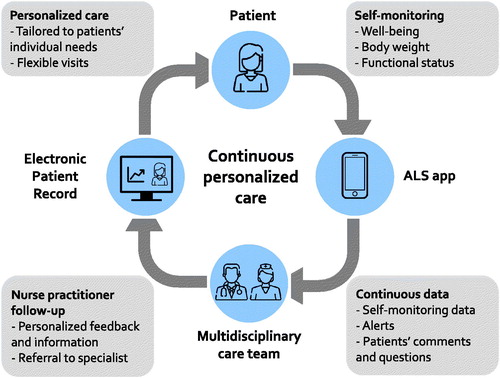
The telehealth service
The design process of ALS Home-monitoring and Coaching was inspired by the user-centered design approach which aims to truly meet the needs of end-users (patients and healthcare professionals) (Citation5). Involving patients in the development process resulted in the design of an appropriate self-monitoring protocol and a user-friendly telehealth service. In order to standardize remote monitoring, a protocol was developed based on ALS guidelines and expert opinion from members of the multidisciplinary care team. The protocol specified what information and feedback should be provided to the patient in response to changes in functioning. It also specified the timing of referral to the multidisciplinary care team and what topics the nurse practitioner should discuss with members of the team. The key features of ALS Home-monitoring and Coaching were: (1) App-based self-monitoring, (2) a message function, (3) alerts and (4) follow-up by a nurse practitioner. An overview of the key features can be found in .
App-based self-monitoring
The ALS app (by Focuscura, the Netherlands) was operational on a smartphone, tablet and personal computer. Patients were offered a tablet when they had no electronic device compatible with the ALS app. When patients had upper limb impairment, (informal) caregivers assisted with operating the smartphone/tablet and self-monitoring. Patients were able to use eye-control when using a computer for self-monitoring. During an introductory interview, the nurse practitioner created an account for patients and helped them install the ALS app. Patients used the ALS app to self-monitor their health status, through the assessment of well-being, body weight and functional status. Well-being was assessed by answering the question “How are you today?” with a score from 1 to 10. Additionally, patients were invited to comment on their score and well-being in the ALS app through a free-text entry. Body weight was assessed with a regular or Bluetooth body weight scale. All patients were offered a Bluetooth scale, but patients were allowed to use their own scale. The Bluetooth scale transmitted the body weight data automatically to the ALS app, while patients with a regular scale had to enter the data manually. Functional status was assessed with a self-administration version of the revised ALS functional rating scale (ALSFRS-R) (Citation6). The default self-monitoring frequencies were daily for well-being, weekly for body weight and monthly for functional status. At the start of monitoring, frequencies were set at default, but could be adjusted to patients’ preference. To remind patients about self-monitoring, a notification was automatically sent by email at an agreed-upon time and day of the week. Patients had open access to their own data, which was accessible in the ALS app. Once a measurement had been completed, the data were transmitted automatically to a central server, also accessible to healthcare professionals. Additionally, the ALS app was integrated in the electronic health records, which facilitated data accessibility for the multidisciplinary care team.
Message function
The ALS app included a free-text message function, which allowed for patients to comment on or ask questions about any topic including: symptoms, treatments, aids, personal issues, technical issues or consultation planning. Depending on the question or comment, the nurse practitioner answered the questions and gave advice within three days, and if needed referred patients to the multidisciplinary care team. Patients were informed about a possible delay in the reply, and in case of urgency, they were told to contact their general practitioner.
Alerts
Alerts signaled the nurse practitioner when a significant change in health status occurred involving a drop to (or below) a pre-determined threshold. Alerts were generated when (1) body weight had decreased by 5% and 10% of premorbid weight, (2) the well-being question was answered with a score of two or lower and (3) any item score of the ALSFRS-R dropped one point or more relative to the last measurement. The nurse practitioner monitored the individual alerts and trends of all patients and discussed the changes in health status weekly with the multidisciplinary care team.
Monthly follow-up by nurse practitioner
In addition to the follow-up on patient’s messages, the nurse practitioner, who was engaged with all patients, evaluated their individual health status data and provided monthly personalized feedback and information via an e-consult or telephone consultation. Patients could access the e-consult in their electronic medical record, through a web portal login with two-factor authentication (digital identification: the online ID allowing access to services and government websites in the Netherlands, with username, password and short message service (SMS) verification). The nurse practitioner was supervised by a rehabilitation physician and used the standardized monitoring protocol to ensure adequate personalized feedback and information for all patients. If necessary, patients were referred by the nurse practitioner to members of the multidisciplinary care team for a face-to-face consultation.
Outcome measures for the use of the ALS app
The use of the ALS app was evaluated through the adoption rate, adherence, and dropout. Adoption rate was calculated as the proportion of patients who chose to adopt telehealth. Adherence was defined as the percentage of completed self-monitoring assessments agreed upon. Adherence was calculated for patients who had activated their account for ≥1 month for well-being and body weight, and for ≥2 months for functional status. The dropout was defined as the number of patients who discontinued telehealth due to reasons unrelated to the end-of-life phase or death.
User-experience assessment
Surveys
Patients. Patients whose account was activated for over four months were invited to fill in a one-time online survey designed for the purpose of the study. Patients received an email with a link to the survey that was accessible on a secure survey website (Collector 2015.Q2). Data were stored on the web-server of the website. The survey evaluated user experiences, such as ease of use, perceived burden, and perceived benefits. Patients were asked to respond to a number of statements and questions on a 5-point Likert scale. Scores of 4 or higher were coded as being in agreement.
Healthcare professionals. A one-time online survey was administered to all members of the multidisciplinary care team at the UMCU. Healthcare professionals received an email with a link to the survey that was accessible on a secure survey website (Collector 2015.Q2). The survey evaluated the extent to which the self-monitoring data were used by the healthcare professionals and whether the use of telehealth led to changes in care.
Semi-structured interviews
Semi-structured interviews were conducted by two of the investigators (JH, RvE) to further explore opinions and experiences of patients regarding the use of telehealth. Consecutive patients who completed the survey were selected. The interviews were discontinued when data saturation was reached.
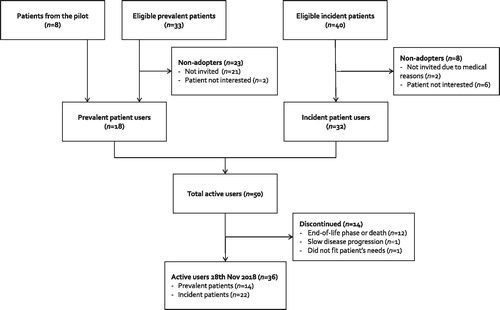
Analysis
Two groups of patients were distinguished: prevalent and incident patients. Prevalent patients included those who were diagnosed and received multidisciplinary care at the ALS clinic before the implementation of telehealth on 1st May 2017 (including patients who participated in the pilot). The prevalent group was a convenience sample, as these patients were selected by the rehabilitation physician based on health status, disease progression and potential benefits of telehealth use. Incident patients included all consecutive patients who were diagnosed and started to receive multidisciplinary care at the ALS clinic after the implementation of telehealth. In order to avoid selection bias, the adoption rate was only calculated for the sub-group of incident patients.
Self-monitoring adherence was calculated for all patients and reported as the percentage of patients that showed good adherence. The adherence of an assessment was judged as good when patients completed ≥50% of agreed-upon measurements for well-being and body weight and ≥75% for functional status. A minimal adherence of 50% was considered to be sufficient for patients to reflect on their well-being and for healthcare professionals to observe a trend in body weight between clinic visits. Body weight adherence was calculated until patients were unable to weigh themselves due to the inability to stand (ALSFRS-R item 8 score = 0). A minimal adherence of 75% for the assessment of functional status was required, as the ALSFRS-R was only measured once per month and the provision of tailored feedback and information was mainly based on ALSFRS-R scores.
The survey results were reported as the number and percentage of subjects who (totally) agreed to a statement. Data from the structured interviews were digitally recorded and transcribed verbatim. The interviews were coded by two independent researchers. Thematic analysis was performed until data saturation was reached and no more themes emerged (Citation7).
Results
In the period 1st May 2017 to 28th November 2018, a total of 50 patients used ALS Home-monitoring and Coaching, consisting of 18 prevalent and 32 incident patients. The inclusion flowchart can be found in . A total of 41 prevalent patients received care before the implementation of the telehealth service, 8 of which were already enrolled in the pilot, 21 of which were not invited (reasons not documented), 12 were invited of which 10 adopted telehealth. 40 newly diagnosed incident patients were referred to the multidisciplinary care team and were invited to use telehealth between May 2017 and November 2018; of these 32 (80%) adopted telehealth. A total of 14 patients discontinued using telehealth in the follow-up period. The most frequently reported reason for discontinuing telehealth was no added benefit from telehealth due to the end-of-life phase or death (n = 12). For patients who discontinued telehealth in the end-of-life phase, median time between the final measurement and death was 19.0 days (IQR = 7.8–49.0). There were two dropouts in this study. Reasons for dropping out were no perceived use due to slow disease progression (n = 1) and telehealth did not fit patient’s needs (n = 1).
Patients were, on average, 61 years old at diagnosis, mostly male (64%), diagnosed with ALS (76%), and had spinal onset (72%). provides an overview of all patient characteristics. four patients had an electronic device that was not compatible with the ALS app and therefore received a tablet for self-monitoring, all other patients had compatible devices. Six patients received a Bluetooth scale, all other patients preferred using their own scale. Patients were followed-up for a median of 10.8 months (IQR = 5.9–13.2) ().
Figure 3 Months of follow-up per patient. *Started July 2016 (pilot), E: End-of-life phase, D: Dropout.
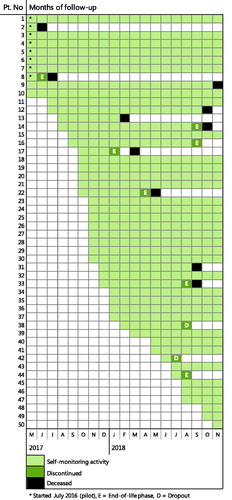
Table 1 Patient characteristics.
Adherence and user data
Good adherence was seen in 49% of patients for the assessment of well-being, in 83% for the assessment of body weight and in 87% for the assessment of functional status.
A total of 2003 messages were sent to the nurse practitioner via the ALS app by 47 patients (M = 42.6, range = 3–268). Most of the messages were comments explaining the given well-being score. 241 well-being alerts were generated in 17 patients (M = 14.2, range = 1–44), 395 body weight alerts were generated in 31 patients (M = 12.7, range = 1–39) and 263 functional status alerts were generated in 47 patients (M = 5.6, range = 1–14).
User experiences
Patient survey
In total, 23 out of 34 patients who were invited, completed the survey (response rate 68%); 17 of whom were men and with an average age of 63.2 years. Patients completed the survey after using telehealth for a median duration of 5.8 months (IQR = 4.7–10.9). The majority of patients were positive about receiving personalized feedback and information, and perceived the use of telehealth as helpful, easy and not burdensome. All but one patient would recommend the use of ALS Home-monitoring and Coaching to others. Patients had mixed opinions on the ease of logging onto their electronic medical record with their digital ID to access the monthly feedback through the e-consult. All patient survey results can be found in .
Table 2 Patient survey results.
Healthcare professional survey
The healthcare professional survey was administered 18 months after the implementation of telehealth and was completed by 9 of 11 (82%) healthcare professionals of the multidisciplinary care team (two rehabilitation physicians, two occupational therapists, two physical therapists, a speech therapist, a dietician and a social worker). The survey showed that the majority of healthcare professionals used the monitored data to prepare for consultations (). Healthcare professionals reported that they had consultations as a result of referral by the nurse practitioner. Workload was similar compared to care without telehealth for most healthcare professionals, but in-person consultations were used more effectively, as the available monitoring data helped them in preparing the consultation. Furthermore, all healthcare professionals reported that the use of telehealth was of added value in ALS care and that they would recommend it to other healthcare professionals.
Table 3 Healthcare professional survey results.
Structured patient interviews
The interviews showed negative as well as positive experiences. Themes related to negative experiences were log on issues and being confronted by decreasing ALSFRS-R scores. Themes related to positive experiences were the user-friendliness of the ALS app, the low burden of the self-monitoring protocol, better understanding of the disease, increased perceived control over care, greater continuity of care and reassurance, more flexible consultations and moments for self-reflection. Identified themes are presented in .
Table 4 Overview of themes regarding patients’ experiences with telehealth, supported by quotes.
Discussion
This study showed that the use of home-monitoring and nurse practitioner follow-up was suitable for the provision of multidisciplinary ALS care, with a high adoption rate, good adherence, few dropouts and positive experiences from patients and healthcare professionals. This is the first study to report on the use of an implemented app-based telehealth service with self-monitoring in specialized ALS care.
The majority of newly diagnosed patients in the current study adopted telehealth, showing that patients with ALS were willing to use technology in their care. Previous research has shown that patients with ALS are generally familiar with using technology (Citation8–11). Patients who did not adopt telehealth were, on average, older and the majority were female.
Patients showed good overall adherence to the self-monitoring protocol. Facilitators of self-monitoring adherence in the current study were a user-friendly app, low burden of self-monitoring and use of notifications. These factors have also been identified as facilitators of self-monitoring in previous literature (Citation12). Another facilitator of adherence was the provision of monthly personalized feedback on the self-monitoring data (Citation12). This likely motivated patients to adhere to the self-monitoring protocol. Furthermore, most healthcare professionals used the monitored data during regular in-clinic consultations. Other factors that motivated patients were a feeling of control they gained through self-monitoring, as well as more flexible clinic visits tailored to their needs. A barrier to telehealth use was difficulty accessing the e-consult. Providing personalized feedback in the ALS app could facilitate accessibility in the future.
In contrast to the current study, Paneroni et al. (Citation13) reported low adherence to a self-monitoring protocol. This was likely a result of the complexity of reporting and the high number of daily assessments in this study. In two other studies, good adherence with (bi-)weekly home-based self-monitoring was observed (Citation14,Citation15). Accordingly, patients reported that technology was user-friendly and self-monitoring was easy (Citation15,Citation16).
Although we found good overall adherence in the current study, it was noticeable that adherence to the well-being assessment was low compared to the adherence to the bodyweight and functional status assessments. Low adherence was likely due to the fact that the default frequency with daily assessments was too high for some of the patients. For this reason, self-monitoring frequencies were lowered at individual patients’ request. The requested changes in frequency were, however, not taken into account in the calculation of adherence as these were not documented in the ALS app. The missing information resulted in an underestimation of adherence. Despite the lower adherence of the well-being assessment, 85% of patients completed the well-being assessment at least once per week. This was found to be sufficient for the provision of psychological support and for patients to self-reflect on their well-being.
A remarkable finding was that patients continued to use the ALS app to contact the ALS clinic and read the personal feedback from the nurse practitioner until shortly before their death. These findings suggest that patients valued communication with the nurse practitioner in the end-of-life phase, despite the fact that care in the end-of-life phase is on the whole provided by a general practitioner. Accordingly, the interviews showed that patients experienced more continuity of care and a feeling of reassurance as a result of remote monitoring by the nurse practitioner.
An important aspect of remote monitoring was alerts for disease worsening, which were found to be appropriate for the provision of feedback and information in most cases. However, for the well-being assessment, repetitive alerts were seen in two patients who gave low scores consecutively. These patients were called by the nurse practitioner and received psychological support. Repetitive alerts were also generated in some patients for the body weight assessment, as these patients remained stable in body weight below the cutoff value. The nurse practitioner did not perceive these repetitive alerts as a burden. The alerts that were generated for every drop of the ALSFRS-R score were found to be abundant, as the nurse practitioner would provide monthly feedback three days after patients completed the ALSFRS-R, regardless of any changes in score. For this reason, we have removed all alerts for the functional status assessment.
So far, previous research on the use of telehealth in ALS has reported on home-based self-monitoring, videoconferencing, the store and forward method, and remote monitoring of noninvasive ventilation (Citation17). A parallel publication reported on the use of a telehealth system similar to ALS Home-monitoring and Coaching, which also included a patient app for self-monitoring, a clinical portal, alerts and a telehealth nurse (Citation15,Citation18). In this trial, patients and caregivers reported that telehealth was easy to use, self-monitoring did not cost a lot of time and they would recommend telehealth to others. These findings are similar to the results of the current study, and support that app-based self-monitoring is a suitable method for providing remote care to patients with ALS.
Currently, the platform costs associated with the telehealth service are funded by the University Medical Center Utrecht as there is no reimbursement for this type of telehealth. The lack of reimbursement is the main barrier to widespread implementation and use of telehealth. In order to facilitate the future implementation and use of telehealth, healthcare insurance companies should include telehealth in their reimbursement options.
Limitations
The current study was conducted in a single specialized center, which limits the generalizability of the results and the transferability to other settings. We are, however, working on the nationwide implementation of ALS Home-monitoring and Coaching, which will allow us to evaluate its feasibility in other healthcare settings and generalize future findings. The results obtained from the prevalent patients may suffer from selection bias, as this was a convenience sample. Furthermore, the response rate of the patient survey was relatively low, which could mean the results of the survey may have a risk of bias. A methodological and technical limitation was that requested changes in self-monitoring frequency were not documented in the ALS app software. As a result, the missing data lead to an underestimation of adherence. In the current study, we chose to exclude the assessment of caregiver user experiences. However, caregivers play an important role in assisting patients with the use of telehealth; for this reason, this is an interesting topic for future research. Future studies should also investigate the cost-effectiveness of ALS Home-monitoring and Coaching, its feasibility in other healthcare settings, and the effect of personalized care on the timing of therapies and assistive devices.
Conclusion
In conclusion, we have shown that ALS care supplemented by app-based self-monitoring and nurse practitioner follow-up was suitable and widely accepted by patients and healthcare professionals. Success factors of the telehealth service were low self-monitoring burden, a user-friendly platform and the provision of personalized feedback. A potential barrier for widespread implementation of this telehealth service, is the lack of reimbursement. Future research should investigate the cost-effectiveness and the feasibility of this telehealth service in other healthcare settings.
Declaration of interest
The authors declare no conflicts of interest and that the current study is their own work.
Acknowledgements
We would like to thank Nicole Tiemessen and Melanie Groothuis from the Department of Information Technology, University Medical Center Utrecht for their support during the development and implementation of ALS Home-monitoring and Coaching.
Additional information
Funding
References
- van Es MA, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp RJ, Veldink JH, et al. Amyotrophic lateral sclerosis. Lancet. 2017;390:2084–98. [Internet]. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0140673617312874
- Schellenberg KL, Hansen G. Patient perspectives on transitioning to amyotrophic lateral sclerosis multidisciplinary clinics. Jmdh. 2018;11:519–24.
- Stephens HE, Young J, Felgoise SH, Simmons Z. A qualitative study of multidisciplinary ALS clinic use in the United States. Amyotroph Lateral Scler Front Degener. 2016;17:55–61.
- Willems M, Reiff E, Kruitwagen E, van den Berg L, Visser-Meily J, Schröder C. Pilot thuismonitoren bij ALS. Nederlands Tijdschrift Voor Revalidatiegeneeskunde. 2017;39:51–4. Available from: www.dehoogstraatorthopedietechniek.nl
- De Vito Dabbs A, Myers BA, Mc Curry KR, Dunbar-Jacob J, Hawkins RP, Begey A, et al. User-centered design and interactive health technologies for patientsi. CIN - Comput Informatics Nurs. 2009; 27:175–83.
- Bakker L, Schröder C, Tan H, Vugts S, van Eijk R, van Es M, et al. Development and assessment of the inter- and intra-rater reproducability of a self-administration version of the ALSFRS-R. 2020;91:75–81.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
- Geronimo A, Wright C, Morris A, Walsh S, Snyder B, Simmons Z. Incorporation of telehealth into a multidisciplinary ALS Clinic: feasibility and acceptability. Amyotroph Lateral Scler Front Degener. 2017;18:555–61. Oct 2
- Hobson EV, Fazal S, Shaw PJ, McDermott CJ. “Anything that makes life’s journey better.” Exploring the use of digital technology by people living with motor neurone disease. Amyotroph Lateral Scler Front Degener. 2017;18:378–87.
- James N, Power E, Hogden A, Vucic S. Patients’ perspectives of multidisciplinary home-based e-Health service delivery for motor neurone disease. Disabil Rehabil Assist Technol. 2018;
- Mackenzie L, Bhuta P, Rusten K, Devine J, Love A, Waterson P. Communications technology and motor neuron disease: an Australian survey of people with motor neuron disease. JMIR Rehabil Assist Technol. 2016;3:e2.
- Simblett S, Greer B, Matcham F, Curtis H, Polhemus A, Ferrão J, et al. Barriers to and facilitators of engagement with remote measurement technology for managing health: Systematic review and content analysis of findings. J Med Internet Res. 2018;20:e10480.
- Paneroni M, Trainini D, Winck JC, Vitacca M. Pilot study for home monitoring of cough capacity in amyotrophic lateral sclerosis: a case series. Rev Port Pneumol. 2014;20:181–7.
- Ando H, Ashcroft-Kelso H, Halhead R, Young CA, Chakrabarti B, Levene P, et al. Incorporating self-reported questions for telemonitoring to optimize care of patients with MND on noninvasive ventilation (MND OptNIVent). Amyotroph Lateral Scler Front Degener. 2019; 20:336–47.
- Hobson E, Baird W, Bradburn M, Cooper C, Mawson S, Quinn A, et al. Process evaluation and exploration of telehealth in motor neuron disease in a UK specialist centre. BMJ Open. 2019;9:e028526.
- Ando H, Ashcroft-Kelso H, Halhead R, Chakrabarti B, Young CA, Cousins R, et al. Experience of telehealth in people with motor neurone disease using noninvasive ventilation. Disabil Rehabil Assist Technol. 2019;1–7.
- Helleman J, Kruitwagen E, van den Berg L, Visser-Meily J, Beelen A. The current use of telehealth in ALS care and the barriers to and facilitators of implementation: a systematic review. Amyotroph Lateral Scler Front Degener. 2019:1–16.
- Hobson EV, Baird WO, Bradburn M, Cooper C, Mawson S, Quinn A, et al. Using telehealth in motor neuron disease to increase access to specialist multidisciplinary care: a UK-based pilot and feasibility study. BMJ Open. 2019;9:e028525.