Abstract
This study assessed health-related quality of life (HRQoL) and musculoskeletal function in patients with musculoskeletal disorders after participation in group-based aqua-exercising, compared to before participation. Physiotherapists instructed group-based aqua-exercising for 30 min twice a week for 8 weeks in 39 patients (81% women, mean age 55 ± 12 years), with musculoskeletal disorders located in the back (28%), neck (17%), general myalgia (21%), lower extremities (9%), shoulder (7%) and multiple/other regions (18%). Before and after the aqua-exercising, physiotherapists assessed patients’ musculoskeletal function categorized using Goal Attainment Scaling, and HRQoL was measured using EuroQol 5 Dimensions (EQ-5D). The median EQ-5D score was 0.36 (25th–75th percentiles 0.09–0.69) at the start, and after the intervention improved to 0.62 (0.09–0.73) (p = 0.038). The EQ-5D score and musculoskeletal function improved in 49% (EQ-5D) and 34% (physiotherapist assessment), were stable in 33% and 63%, and worsened in 18% and 7% of patients, respectively. In conclusion, comparable with improvements previously seen after more time-consuming exercise periods, patients with musculoskeletal disorders had improved HRQoL after 8 weeks of aqua-exercising compared to before exercising. This uncontrolled feasibility study does not reveal whether this was the result of aqua-exercising. The effects and costs need to be evaluated in randomized controlled studies.
Introduction
Group-based aqua-exercising is a common treatment for a variety of musculoskeletal disorders[Citation1] in primary healthcare, but it is not known whether musculoskeletal function and quality of life will improve after participation in general group-based aqua-exercising led by physiotherapists. Previous studies have shown that aqua-exercising programmes developed for specific patient groups are effective, for example in back pain,[Citation2] knee and hip osteoarthritis,[Citation3] fibromyalgia,[Citation4] and neurological and musculoskeletal disorders.[Citation5] A variety of musculoskeletal disorders accounts for two-thirds of all pain disorders handled in Swedish primary healthcare clinics.[Citation6] Musculoskeletal disorders have increased over the past decade[Citation7] and produce the second highest rates of sickness absence in the UK.[Citation8] The most common regions for musculoskeletal disorders assessed and treated in general practices are back and neck pain, followed by knee and shoulder pain.[Citation9] Compared to the general population, individuals with musculoskeletal disorders rate their health-related quality of life (HRQoL) lower.[Citation10] Both in Sweden and in other countries, physiotherapists assess and treat patients with musculoskeletal disorders,[Citation11,Citation12] attempting to improve HRQoL limitations,[Citation10] which are often evaluated using generic HRQoL instruments, e.g. the EuroQol 5 Dimensions (EQ-5D).[Citation13]
A common physiotherapy intervention for musculoskeletal disorders is group-based aqua-exercising.[Citation1–5].The water environment provides a relevant tool for treatment of these patients. Beside the pain-relieving effects of the sensory stimulation induced by the water temperature, immersion in the water increases muscular blood flow. The immersion decreases the axial loading and allows performance of movement that may be impossible on land, through the effects of buoyancy and balance support. The water provides flow and turbulence, and the hydrostatic pressure induces resistance to exercising the extremities and trunk.[Citation14] Previous studies evaluated individual or group-based aqua-exercises developed for specific disorders, mostly performed for a duration of 1 h, two or three times a week, for 3 months or even longer.[Citation1–5] For example, aqua-exercising for arthritis of the knee focused on musculoskeletal function of the lower extremities, specifically knee function.[Citation3] Specific aqua-exercises were found to improve musculoskeletal function and HRQoL measured using multi-item instruments with satisfactory sensitivity to detect changes.[Citation1] However, in an ordinary clinical primary care setting, aqua-exercises are often performed in groups including mixed types of musculoskeletal disorders, exercising for shorter durations than in the previous studies. We do not know the feasibility and the benefit of this type of group exercise. Does the EQ-5D, with low sensitivity to detect changes,[Citation13] detect potential changes in HRQoL after compared to before short-term aqua-exercising performed in mixed groups?
Before conducting a controlled study of the benefits and costs of group-based aqua-exercising, we performed this feasibility study. The study aimed to assess HRQoL and musculoskeletal function in patients with musculoskeletal disorders after participation in group-based aqua-exercising, compared to before participation.
Material and methods
The study was a pragmatically conducted uncontrolled clinical feasibility study. The study did not add any intervention or data collection other than those included in ordinary routine praxis, and the patients’ full integrity was secured. No ethical approval was therefore needed, according to Swedish ethical law. The patients received a code number which replaced their names during all data management.
Sample and setting
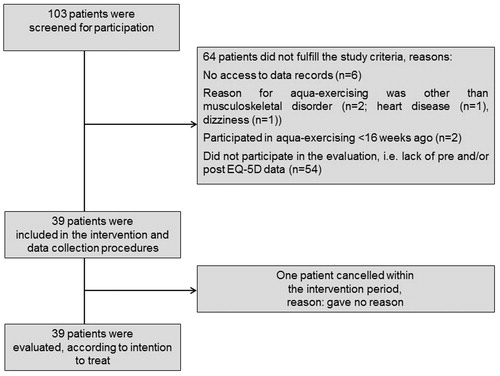
During a 20 month period in a primary healthcare district in a county council in central Sweden, all patients were included who complied with the inclusion criteria: had participated in group-based aqua-exercising for musculoskeletal disorders and had supplied HRQoL data before and after the aqua-exercising period. Patients were excluded if they had taken part in previous aqua-exercising in primary healthcare for musculoskeletal disorders less than 16 weeks before the start of the intervention. Of 103 patients screened for inclusion, 39 fulfilled the study criteria and 64 did not: 54 did not supply HRQoL data, i.e. did not deliver pre- or post-exercise data, and 10 for other reasons ().
Data collection
Physiotherapists collected the data and registered the data in the patients’ medical records, according to their normal routines. To minimize potential therapist bias, the physiotherapists were unaware both that the data would be used in a study and which patients would comply with study criteria until after data extraction, although they were aware that the patients participated in aqua-exercising.
Clinical and socio-demographic data
Following a standardized data collection scheme, the physiotherapists responsible for each patient provided clinical and socio-demographic data from the patient’s medical records to the evaluator (). Data regarding events in each patient’s situation during the time-frame of the aqua-exercising period were supplied, e.g. changes in personal or working situation, or in the patient’s mood, medical complications and the initiation of exercising other than the intervention. For each patient, the evaluator then categorized these events into three categories: events supposed to affect health positively, events supposed to affect health negatively and no known events. Data on compliance with the aqua-exercising sessions were collected.
Table 1. Characteristics of the patients.
Health-related quality of life
To measure HRQoL, the physiotherapists responsible for each patient delivered the generic EQ-5D form[Citation13] to the patients. The patients answered it in writing at the start of the period of aqua-exercising and immediately after the period, during an evaluation session with the physiotherapist. The EQ-5D[Citation13] is valid and reliable, with an intraclass correlation coefficient of 0.82–0.87,[Citation15] and is widely used.[Citation13] It has previously been used in other aqua-exercising studies.[Citation16] The form consists of five dimensions, each with three alternative answers (). The possible different combinations of answers on these dimensions result in a total score ranging from –0.59 (no health at all – equal to or worse than death) to 1 (best imaginable health). The form also includes the EQ-5D barometer, a vertical health barometer in which the patients grade their health from 0 (worst imaginable health state) to 100 (best imaginable health state).[Citation13]
Table 2. EuroQol 5 Dimensions (EQ-5D) measured before and after aqua-exercising.
Physiotherapy assessment of musculoskeletal function
The physiotherapists responsible for each patient performed a physiotherapy assessment of the patients’ musculoskeletal function[Citation17] at the start and the end of the aqua-exercising period according to ordinary clinical routines and depending on the location of the patient’s disorder: anamnesis, inspection in rest and in motion, functional fitness tests, active and passive range of motion and joint mobility in the affected body area, and musculoskeletal disorder-specific physical tests [e.g. Hawkin’s test during subacromial shoulder pain.[Citation18]] Goal Attainment Scaling[Citation19] was used by the physiotherapists to categorize potential changes in musculoskeletal function between pre- and post-assessment. The scale has been shown to be highly sensitive to changes over time.[Citation20] Goal Attainment Scaling in its original version utilizes five steps.[Citation19] In the present study, the evaluator categorized “much worse and worse” as “worse”, and “better” and “much better” as “better” owing to the very low numbers of patients in the first and last categories.
Aqua-exercising intervention
Physiotherapists instructed standard aqua-exercising programmes based on the scientific literature[Citation1,Citation14,Citation21] and clinical experience: 30 min twice a week for 8 weeks (16 sessions), including the sections described in . The training sessions were of moderate intensity. During aerobic training sections, the patients, according to international exercise guidelines,[Citation21] trained at approximately 65% of their aerobic maximum [maximal oxygen consumption (VO2max)]. They were thus instructed to experience the signs of moderate-level exertion: feeling warm, increased frequency of heart rate and breathing, but still being able to converse. Thus, patients with higher VO2max trained at a higher speed than patients with lower VO2max to experience the same signs, i.e. to achieve a similar level of aerobic training (percentage of VO2max). During endurance strength sections, the speed of the endurance strength exercises was enough for the water to provide a resistance of approximately 65% of one repetition maximum (RM). Each endurance strength exercise was repeated 15–20 times, for three to five sets. Patients with higher RM performed a larger range of motion, or performed the exercise with a larger body area against the water resistance, than patients with lower RM, to achieve a similar percentage of RM (). To meet the patients’ improvements, the sessions thus became progressively harder with time to provide a moderate level of intensity. The temperature in the pool was 34 °C and the water level was approximately breast or shoulder deep (140 cm water depth).
Table 3. Description of the studied standard aqua-exercise programme.
Statistical analyses
The evaluator, who was not involved with assessing or treating the patients, calculated descriptive statistics regarding the collected variables: number (n), proportion (%), mean ± SD for continuous variables, and median (25th–75th percentiles) for ordinal or non-normally distributed variables. Pre- and post-exercise EQ-5D total scores, dimension scores and EQ-5D barometer were compared using Wilcoxon’s test (paired analyses, ordinal variables). For pedagogical reasons when presenting data (not when analysing), the differences in EQ-5D scores between pre- and post-exercising were categorized into worse, similar and better.
To distinguish whether the 39 patients included in the study were representative of the whole population of 93 patients with musculoskeletal disorders participating in aqua-exercising in the studied primary healthcare region during the study period (), we compared the 39 included patients with the 54 not included patients regarding the variables shown in . The unpaired Student’s t test was used for the continuous variable age, the Mann–Whitney U test for the continuous but non-normally distributed variable compliance rate, and Fisher’s exact test for category variables (gender, location of musculoskeletal disorder, parallel physiotherapy, events, other diagnoses). To distinguish whether the variables were normally distributed or not, we visually observed histograms of the distribution of the values and used the Kolmogorov–Smirnoff test. The significance level was set at 5%.
Results
A “typical” study patient (n = 39) was a 55-year-old (mean value) woman, participating in the aqua-exercises for a musculoskeletal disorder located in the vertebral column (41% of the patients), having at least one other diagnosis (85%) and not receiving any parallel physiotherapy during the intervention period (54%) (see for characteristics of the patients).
The only statistically significant differences between the study patients (n = 39) and the aqua-exercising patients who were not included in the study owing to a lack of EQ-5D pre/post data (n = 54) were that the study patients had higher rates of compliance (p = 0.009) and fewer cancelled therapy periods (p = 0.012). The study patients attended a median of 13 out of 16 offered sessions, and 72% of them participated in 13 to all 16 sessions ().
Health-related quality of life and musculoskeletal function after compared to before aqua-exercising
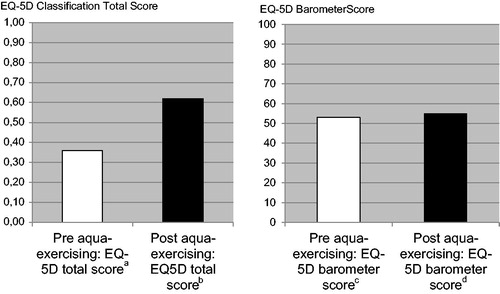
The total EQ-5D score was improved after compared to before the aqua-exercising (p = 0.038). The size of the improvement in EQ-5D score seen after 8 weeks (one-sixth of a year) was 0.26 (post-score 0.62 – pre-score 0.36). This equates to 0.043 quality-adjusted life-years (QALYs): 0.26/6.[Citation21] The EQ-5D barometer did not change significantly (p = 0.378) ().
Figure 2. Health-related quality of life measured before and after aqua-exercising: median EuroQol 5 Dimensions (EQ-5D) total score and barometer score. 25th–75th percentiles: a0.09–0.69, b0.09–0.73, c35–70, d40–75.
After the aqua-exercising period, the patients reported improvements in the EQ-5D dimension anxiety/depression. Before aqua-exercising, 27% reported no problems with anxious or depressed mood, whereas after aqua-exercising, 46% reported no problems. There was a tendency, although not statistically significant, for daily activities to have improved after aqua-exercising: 36% reported no problems after compared to 23% before exercising. No significant differences were seen for the other dimensions ().
The EQ-5D total score and the musculoskeletal function improved in 49% (EQ-5D) and 34% (physiotherapist assessment), were stable in 33% and 63%, and worsened in 18% and 7% of the patients, respectively. In 12 out of a total of 32 patients, the results of the physiotherapy assessment and the EQ-5D total score were consistent regarding the direction of change, if any ().
Table 4. Health-related quality of life (HRQoL) and musculoskeletal function after compared to before aqua-exercising.
Discussion
In this uncontrolled feasibility study, we found that patients with musculoskeletal disorders had improved HRQoL and less anxious or depressed mood after 8 weeks of aqua-exercising compared to before exercising, and in one-third of the patients the musculoskeletal function had improved. Since our study had no control group, we do not know whether the improvements seen after the aqua-exercising period were the result of the aqua-exercising or of other uncontrolled factors.
That HRQoL had improved after compared to before only 8 weeks of 30 min sessions of group-based aqua-exercising for patients with mixed musculoskeletal disorders is a new observation but is consistent with previous studies using more time-consuming aqua-exercising interventions, specifically developed for the evaluated disorder. These studies showed improvements in HRQoL, measured with a variety of instruments.[Citation16,Citation23–26] In one of the studies using HRQoL instruments other than EQ-5D, patients with hip or knee arthritis, similarly to our study, performed only 18 group-based aqua-exercise sessions (three times per week for 6 weeks). However, they performed pure strength training specifically for the lower extremity.[Citation24] In other studies, the aqua-exercising had longer durations; patients with osteoarthritis performed group-based aqua-exercising for 60 min three times a week during 20 weeks[Citation25] or during 52 weeks.[Citation26] In our study, the improvement in EQ-5D score was 0.26 between before and after 480 min (16 sessions at 30 min) of group-based aqua-exercise sessions. This is a similar size of improvement in EQ-5D score to that seen by Gusi and co-workers,[Citation16] with a change of 0.27 after 2160 min (36 sessions at 60 min) group-based aqua-exercising in patients with fibromyalgia.[Citation16]
When comparing pre- and post-scores for the separate EQ-5D dimensions in our study, we revealed statistically significant improvement only in the anxiety/depression dimension and a tendency for the dimension of usual activities. Our intervention continued for less than a quarter of the duration of the previously mentioned study;[Citation16] that study observed improvements in all EQ-5D dimensions, except for self-care. Improvements in anxious and depressed mood, measured with a variety of instruments, are in agreement with previous studies of patients with fibromyalgia, receiving a higher dose of aqua-exercise.[Citation16,Citation27] Saltskår Jentoft and co-workers[Citation27] evaluated patients after 3600 min of aqua-exercising (60 sessions at 60 min). In previous studies, one-quarter of individuals with musculoskeletal disorders in general and approximately half of individuals with back, neck or shoulder pain reported some or extreme problems with anxiety/depression in the EQ-5D,[Citation10] compared to 15% among individuals from the general population.[Citation28] In our study sample, 73% of patients reported some or extreme problems with anxiety/depression before aqua-exercising. Thus, the improvement in this dimension seen after aqua-exercising seems to be clinically significant. In a qualitative focus group study, older patients with osteoarthritis stated that they experienced positive effects on health and fitness from their aqua-exercising.[Citation29]
In our study, one-third of the patients had improved their musculoskeletal function after compared to before the intervention according to the physiotherapy assessment, while half of the patients had improved HRQoL. In 12 out of a total of 32 patients, the results of the physiotherapy assessment and the EQ-5D total score were consistent regarding the direction of change, if any. The EQ-5D and physiotherapy assessment complement each other, appearing to partly measure different aspects of the patients’ status. Hypothetically, the patients had gained a larger improvement in HRQoL than in musculoskeletal function since the aqua-exercising was designed for groups including mixed musculoskeletal disorders and thus did not completely comply with the training principle “specificity”, discussed below. Despite the fact that the EQ-5D score had improved after compared to before aqua-exercising, the EQ-5D barometer did not change significantly. Hypothetically, the patients may have incorporated other health issues (e.g. health issues related to economic/social aspects) in this general barometer than those covered by the explicit questions in the EQ-5D score.
It would be of interest in future randomized controlled studies to compare group-based aqua-exercising with other treatment alternatives for musculoskeletal disorders, regarding benefits and costs. A crude calculation of the cost for providing 16 aqua-exercise group sessions (12 patients) at 30 min each (480 min), with a pre- (60 min) and post- (30 min) physiotherapy assessment, results in a mean cost per patient of 1170 Swedish crowns (sek) or 94 euro (eur), i.e. 477 sek/51 eur for the therapist and 400 sek/43 eur for the pool (www.valuta.se, 13 November 2015).1,2,3 Accordingly, if it was the intervention that caused the major part of the improvement of 0.043 QALYs, the cost may be considered as low. In a previous study, a variety of more resource-consuming physiotherapy interventions for musculoskeletal disorders resulted in 0.039 QALYs.[Citation30] The improvement is comparable with, for example, a change from “having problems with anxiety or depression to some extent” to “having no problems with anxiety or depression”. Thus, the improvement in HRQoL between pre- and post-aqua-exercising was probably valuable for the studied patients, whether the improvement was caused by the intervention or by other uncontrolled factors.
Discussing methodological aspects of our study, the largest threat to internal validity is the uncontrolled design. The study was pragmatic, evaluating ordinary clinical routines for intervention and data collection procedures, and thus lacked a control group. The improvements in EQ-5D and musculoskeletal function may be related to the aqua-exercising as well as to uncontrolled factors, e.g. non-specific effects including “placebo” effects, the natural history or confounding factors. We made efforts to register changes during the intervention period. Events supposed to affect health positively occurred in only four patients. However, medical records do not cover all potentially affecting events. We used established methods for data collection.[Citation11,Citation13,Citation15,Citation17,Citation19] The middle three of the original five categories on the Goal Attainment Scaling[Citation19] were used to maximize the number of patients per category before statistical analyses, owing to the low number of patients in the first and the last categories. The physiotherapists assessed musculoskeletal function according to ordinary clinical routines, including a large variety of physical tests depending on the individual patient.[Citation17] Each musculoskeletal disorder required its own combination of physical tests, e.g. Hawkin’s test during subacromial shoulder pain.[Citation18] In future studies, more standardized physiotherapy assessments would be welcomed.
The aqua-exercise intervention followed principles regarding the water environment as a tool for exercise[Citation14] and the well-known principles of training, essential to provide effects of exercises:[Citation21] “individualization”, i.e. the patients modified the speed, range of motion and size of the body surface to the water resistance depending on their individual fitness; “progressive overload”, i.e. the sessions became progressively harder with time to increase training stress; and “rest/recovery”, i.e. the sections within the sessions altered between cardiorespiratory and endurance strength, and there were at least 2 days between the sessions.
The patients had varying musculoskeletal disorders. Thus, it was hard to completely follow the principle of specificity. The exercises were designed to induce general functional and health improvements, potentially affecting HRQoL, rather than to induce improvements in the specific physical tests for each different musculoskeletal disorder performed during the physiotherapy assessment.[Citation17,Citation18] Future aqua-exercising sessions may include a section specifically designed for each individual patient, to potentially induce larger improvements in musculoskeletal function and in the EQ-5D dimensions other than the anxiety/depression dimension. The study patients participated in median of 13 out of 16 offered sessions, and 72% of them participated in 13 to all 16 sessions. When screening patients for inclusion, 54 patients did not fulfil the inclusion criteria owing to a lack of pre- and/or post-exercise EQ-5D data, indicating the need for more efforts to obtain patient data in future studies and in daily clinical work.
The physiotherapists assessing the patients were, for most patients, not the same as those who instructed the aqua-exercising, and were not involved in the statistical evaluation. In future controlled studies, it would be important for the assessors to be entirely blinded to whether the patients were participating in aqua-exercising or not (i.e. control patients). However, the physiotherapists in our study were aware neither of the study nor of which patients complied with study criteria until after extraction of the data, to minimize potential therapist-induced bias. Since the study did not add any routines to the ordinary clinical routines, we could not remind the patients to answer the EQ-5D.
The study sample was rather small (n = 39). However, data were collected during almost 2 years and prolonging the period did not seem relevant since this is a feasibility study, carried out before conducting a larger controlled study.
The low number of study patients per se limits the external validity. However, it is a strength that the study covered a wide range of musculoskeletal disorders and the included patient sample still seemed to be representative of the population of patients who actually participate in group-based aqua-exercises within the primary healthcare district. The study patients did not differ from aqua-exercise participants who were not included, except from that the former had higher compliance with the intervention. Furthermore, the location of musculoskeletal disorders in our study seemed to be distributed similarly to populations who in general seek primary care for musculoskeletal disorders; the locations in a previous study[Citation9] versus those in our study were: the back 25% versus 28%, neck 18% versus 13%, lower extremity 17% versus 13%, and shoulder 17% versus 8% (plus multiple locations 10% in our study).
Using the EQ-5D[Citation13] in future studies, potential benefits of aqua-exercise interventions in terms of improved quality of life may be quantified in QALYs, and costs for the benefit may be calculated.[Citation31,Citation32] When giving priority to one health-care method over others, it is of growing interest and importance to perform health-economic analyses.[Citation33] The findings of our study were that patients with musculoskeletal disorders had improved HRQoL after 8 weeks of aqua-exercising compared to before exercising, comparable with improvements seen after more time-consuming exercise periods; and one-third of the patients seemed to have improved musculoskeletal function. This feasibility study thus indicates that group-based aqua-exercising for a heterogeneous group of patients with musculoskeletal disorders feasibly may be conducted twice per week for 8 weeks. Since this uncontrolled study cannot reveal whether the indicated improvements in HRQoL were the result of the aqua-exercising or of uncontrolled factors, the effects and costs need to be evaluated in randomized controlled studies including sufficient sample sizes.
Acknowledgements
We thank the participating patients, the physiotherapists leading the aqua-exercising groups and the physiotherapists assessing the functional status of the patients.
Disclosure statement
The authors declare no competing interests.
Funding information
The study was funded by Linköping University and the Region of Östergötland.
Notes
Notes
1 Each patient consumed 130 therapist minutes (480 min/12 patients (= 40 min) + 90 min at 220 sek/60 min2 = 770 sek, and 53 min in the pool (16 sessions ×40 min, including entering/leaving =640 min/12 patients) at 450 sek/60 min3 = 400 sek.
2 A public primary healthcare physiotherapist earns a mean of 36,671 sek/month (23,968 sek exclusive of indirect costs of 53%), or 220 sek/h.
3 According to prices in the evaluated county council.
References
- Kamioka H, Tsutani K, Okuizumi H, et al. Effectiveness of aquatic exercise and balneotherapy: a summary of systematic reviews based on randomized controlled trials of water immersion therapies. J Epidemiol. 2010;20:2–12.
- Pittler MH, Karagülle MZ, Karagülle M, et al. Spa therapy and balneotherapy for treating low back pain: meta-analysis of randomized trials. Rheumatology (Oxford). 2006;45:880–884.
- Bartels EM, Lund H, Hagen KB, et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2007;4:CD005523.
- McVeigh JG, McGaughey H, Hall M, et al. The effectiveness of hydrotherapy in the management of fibromyalgia syndrome: a systematic review. Rheumatol Int. 2008;29:119–130.
- Hall J, Swinkels A, Briddon J, et al. Does aquatic exercise relieve pain in adults with neurologic or musculoskeletal disease? A systematic review and metaanalysis of randomized controlled trials. Arch Phys Med Rehabil. 2008;89:873–883.
- Hasselstrom J, Liu-Palmgren J, Rasjo-Wraak G. Prevalence of pain in general practice. Eur J Pain. 2002;6:375–385.
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008 13;299:656–664.
- Wynne-Jones G, Mallen CD, Mottram S, et al. Identification of UK sickness certification rates, standardised for age and sex. Br J Gen Pract. 2009;59:510–516.
- Parsons S, Breen A, Foster NE, et al. Prevalence and comparative troublesomeness by age of musculoskeletal pain in different body locations. Fam Pract. 2007;24:308–316.
- Picavet H, Hoeymans N. Health related quality of life in multiple musculoskeletal diseases: SF-36 and EQ-5D in the DMC3 study. Ann Rheum Dis. 2004;63:723–729.
- Ludvigsson ML, Enthoven P. Evaluation of physiotherapists as primary assessors of patients with musculoskeletal disorders seeking primary health care. Physiotherapy. 2012;98:131–137.
- Holdsworth L, Webster V, McFadyen A, Scottish Physiotherapy Self Referral Study Group. Physiotherapists’ and general practitioners’ views of self-referral and physiotherapy scope of practice: results from a national trial. Physiotherapy. 2008;94:236–243.
- Brooks R, EuroQol Group. EuroQol: the current state of play. Health Policy. 1996;37:53–72.
- Becker BE. Aquatic therapy: scientific foundations and clinical rehabilitation applications. PMR. 2009;1:859–872.
- Solberg T, Olsen J-A, Ingebrigtsen T, et al. Health-related quality of life assessment by the EuroQol-5D can provide cost-utility data in the field of low back surgery. Eur Spine J. 2005;14:1000–1007.
- Gusi N, Tomas-Carus P, Häkkinen A, et al. Exercise in waist-high warm water decreases pain and improves health-related quality of life and strength in lower extremities in women with fibromyalgia. Arthritis Rheum. 2006;15;55:66–73.
- Thonnard J, Penta M. Functional assessment in physiotherapy: a literature review. Eura Medicophys. 2007;43:525–541.
- Hanchard NC, Lenza M, Handoll HH, et al. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;4:CD007427.
- Ottenbacker K, Cusik A. Discriminative versus evaluative assessment: some observations on goal attainment scaling. Am J Occup Ther. 1993;47:349–354.
- Gordon J, Powel C, Rockwood K. Goal attainment scaling as a measure of clinically important change in nursing-home patients. Age Ageing 1999;28:275–281.
- Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359.
- O’Riordan C, Clifford A, Van De Ven P, et al. Chronic neck pain and exercise interventions: frequency, intensity, time, and type principle. Arch Phys Med Rehabil. 2014;95:770–783.
- De Melo Vitorino D, Bizari Coin De Carvalho L, Do Prado G. Hydrotherapy and conventional physiotherapy improve total sleep time and quality of life of fibromyalgia patients: randomized clinical trial. Sleep Med. 2006;7:293–296.
- Foley A, Halbert J, Hewitt T, et al. Does hydrotherapy improve strength and physical function in patients with osteoarthritis – a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62:1162–1167.
- Patrick D, Ramsey S, Spencer A, et al. Economic evaluation of aquatic exercise for persons with osteoarthritis. Med Care. 2001;39:413–424.
- Cochrane T, Davey RC, Matthes Edwards SM. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess. 2005;9:iii–iv, ix–xi, 1–114.
- Saltskår Jentoft E, Grimstvedt Kvalvik A, Mengshoel A. Effects of pool based and land based aerobic exercise on women with fibromyalgia/chronic widespread muscle pain. Arthritis Rheum. 2001;45:42–47.
- Burström K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001;10:621–635.
- Fisken A, Keogh JW, Waters DL, et al. Perceived benefits, motives, and barriers to aqua-based exercise among older adults with and without osteoarthritis. J Appl Gerontol. 2015;34:377–396.
- Hill JC, Whitehurst DG, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;29;378:1560–1571.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–496.
- Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
- Nielsen CP, Funch TM, Kristensen FB. Health technology assessment: research trends and future priorities in Europe. J Health Serv Res Policy. 2011;16(Suppl. 2):6–15.