Abstract
Objectives: Learning from incident reporting systems is one core strategy to develop a culture of safety for healthcare workers and patients. The aim of this retrospective study was to explore patient injuries focussing on falls. Furthermore, on healthcare workers incidents, injuries and the situations they occurred.
Method: A total of 65,749 patient risks and incidents were registered in the incident reporting system between 2011 and 2014. Of these, 11,006 were classified as an injury to a patient. Risks and incidents were registered and analysed for 1702 healthcare workers.
Results: Fifteen percent of the patient injuries required treatment. Falls were reported in 17% of the cases. Patients fell mainly in unassisted situations. Healthcare workers’ incidents and injuries were registered mainly by nurses and assistant nurses. Sixteen percent of the injuries required treatment. Prevalence of incidents was on an average 3.5% each year. Common injuries were: needle stick, workplace violence, injuries during patient manual handling. The patient was present in 74% of all incidents.
Conclusion: Patient and healthcare workers injuries are still prevalent in Swedish healthcare and a substantial part of the incidents involved a patient situation. Collaboration between employers, employees and patient representatives is needed to increase awareness of safety in healthcare.
Introduction
Efforts have been made to increase the safety of patients; however, nearly one out of ten inpatients are still affected by harmful incidents each year [Citation1]. Accidental falls are among the most commonly reported incidents [Citation2]. There are also risk factors in the healthcare environment for healthcare workers (HCWs) leading to work-related injuries [Citation3,Citation4] as well as harmful incidents for patients. This indicates both insufficient patient safety and occupational safety for HCWs. Previous research has confirmed a relationship between working conditions and HCW injuries [Citation5,Citation6] and poor healthcare working conditions might also be associated with poor quality of care and patient injuries [Citation7–9]. A few studies have explored the relationship between working conditions and HCW and patient injuries together, primarily showing that a safety climate supports safe patient care and also ensures HCW safety [Citation10,Citation11]. Perceived staffing levels and managerial commitment are potential predictors for safety outcomes [Citation10]. In a Swedish interview study [Citation11], patient safety was promoted when HCWs had good access to their psychological and social capacities, but these functions were jeopardised by stress caused by prolonged high workload, excessive cognitive work tasks, and lack of social support and teamwork. This leads to mistakes and near misses [Citation11], i.e. patient safety incidents [Citation12]. Patient safety incidents are suggested to be reported in incident reporting systems (IRSs), which are integrated into healthcare systems worldwide as a key method to enable organisational learning and to improve patient safety [Citation13–15]. High patient incident reporting rates are associated with a positive culture of safety [Citation16]; nevertheless, an effective response system is required to enable change [Citation14,Citation15].
The way of reporting occupational incidents and injuries varies in different countries and the IRS might not be used as commonly for HCW incidents as it is for patient incidents, despite the prevalence of work-related injuries [Citation3,Citation4], and thus there is still a need for organisational learning and improved safety. There is a need to explore reported incidents based on a systems approach, including the perspectives of both patients and HCWs. A systems perspective has been emphasised in previous research in order to understand the complexity of incidents in healthcare [Citation17]. A human factor systems approach explains how the design of a work system can impact not only the safety of patients but also HCW safety and organisational outcomes [Citation17]. Data on the patient, HCW, and organisational outcomes as well as care processes can be used to identify problems and opportunities for re-designing the work system and the effect of the re-designed work system on care processes and outcomes can then be evaluated. These feedback loops are key factors when improving the culture of safety [Citation17].
Reporting rates are important, but they are probably inaccurate as an indicator of the safety of a hospital [Citation18]. Instead, there is a trend towards how IRSs can result in learning at the organisational and individual levels [Citation19]. Previous studies have used data from IRSs regarding mainly patients [Citation18–21]; a few have focussed on HCWs, but rarely have they explored IRS data including both patient and HCW incidents. Reported incidents among physiotherapists (PTs) are lacking. Further inquiry into reported incidents can provide a better understanding of how to develop successful measures to improve patient and HCW safety.
The aim of this retrospective study was to explore patient injuries and HCW incidents and injuries reported over a four-year period. A specific objective was to analyse the reports’ descriptions of the sequence of incidents regarding accidental patient falls. Another specific objective was to analyse the incidents of HCW injuries with a particular focus on the types of injuries, who suffers the injuries and the situations in which they occur.
Methods
Study design and setting
This study, the Patient and Workers Safety Study (PAWSS), has a retrospective design using data from an IRS. The studied county is located in Sweden and has approximately 450,000 inhabitants. The county has three hospitals and 41 primary healthcare centres, with a total of 13,000 employees. In total, there were 72,311 numbers of admissions in 2011, 74,006 in 2012, 73,624 in 2013, and 74,031 in 2014.
The incident reporting system
The web-based IRS Synergi is used at all units in the studied county and similar to other IRSs operated in Sweden, it is confidential and non-punitive. The IRS includes all types of risks and incidents of patients and workers reported by individual staff members and heads of departments in two separate systems. A ‘patient safety incident’ is defined as an event or circumstance that could have resulted, or did result, in unnecessary harm to a patient [Citation12]. According to the Swedish Patient Safety Act, it is mandatory for HCWs to report the patient safety incidents that they observe (SFS 2010:659, ch. 6 §4). An injury is defined as a harmful incident [Citation12]. All employees in Sweden, including HCWs, are covered by the occupational injury insurance. An HCW incident is defined as an undesired event or situation that could lead or did lead, to health problems, illness, or accidents. All HCW incidents are to be reported to the employer in addition to the IRS.
Data collection
A total of 65,749 patient risks and incidents and 1702 HCW risks and incidents in the County’s three hospitals, primary healthcare, home care, psychiatric care, and dental care were registered in the IRS between 2011 and 2014. Of these patient reports, 11,006 were classified by the county’s IRS coordinator as an injury to a patient and categorised into the following injury severity levels: [Citation1] injuries resulting in death; [Citation2] injuries requiring treatment and resulting in permanent harm; [Citation3] injuries requiring treatment but not resulting in permanent harm; [Citation4] injuries that did not require treatment; and [Citation5] no harm. In this study, the reports of the 11,006 patient injuries and 1702 HCW total reported incidents and injuries during the years 2011–2014 were included. HCW injury severity levels were categorised according to the same levels.
Data analysis
In the IRS, the reporter enters the date of the identified incident and provides a description of the incident. Each report requires the age and sex of the patient or HCW, the date of the incident, and the incident location. In a free-text section, the reporter is obliged to describe the sequence of the incident. The IRS coordinator determines the process of care, type of injury, severity, and number of injuries based on information provided in the IRS patient report. Data regarding the process of care and severity are entered using pre-fixed multiple-choice responses. In this study, data with pre-fixed multiple-choice responses (severity and care process), sex of the patient or HCW, the HCW occupation, and the date and location of the incident constituted the categorical variables. Age of the patient and the HCW were the continuous variables. The incident location, i.e. the reporting unit/ward, was categorised by the authors according to the region’s current organisation. The reports also provide free-text descriptions of the sequence of the incident, which were analysed in all HCW reports (N = 1702) and in those patient reports including accidental falls (N = 1855). The text was analysed using manifest content analysis with an inductive category development [Citation22]. The focus of interest was the specific text’s substantial content regarding the incident and for HCWs also the type of work situation, type of injury, and the consequences of the injury. Examples of this categorisation are provided in . Two researchers were mainly responsible for categorising this text (CW, ENS), and discussions were continuously held until consensus was reached among the categories. The findings are presented by providing descriptions of the frequencies of the different categories [Citation23]. Descriptive statistics were used to analyse the frequencies of all categorical variables and the mean age. SPSS Statistics version 22 was used for all statistical analyses.
Table 1. Example of categorisation of free text describing the sequence of fall injury and healthcare workers (HCW) incident and injury in the incident reporting system.
Ethics approval
The study was approved by the Regional Ethical Board at Linköping University, Sweden (Dnr: 2015/330-31). All data were de-identified by the County before being assessed by the research team and informed consent for use of the data was not required. All data were handled confidentially.
Results
Patient injuries
A quality assessment of the patient and HCW incident reports is presented in . Information regarding patient sex, a description of the incident, care process, and reporting unit/ward was provided in almost 100% of the reports (86–100%). An exception was the type of patient injury, which was described in fewer than 7% of the total reports, and therefore, not further analysed. There was a decline in the frequency of reported patient injuries over the four years from 3010 in 2011 to 2201 in 2014. During the study period, 3% of the patient injuries were reported to require treatment and resulted in permanent harm, 12% required treatment but did not result in permanent harm, 22% resulted in harm but did not require treatment and in 62%, no harm was reported. Two percent of the incidents caused death (n = 204). The injuries were related to different care processes, primarily medication (23.5%) and nursing (22%). The majority of the patient injuries were reported from primary and homecare (26.8%), medical clinics (18%), emergency wards, including ambulance travel (18%), and surgical clinics (13%) (). The patients in the reports had a mean age of 65 years (SD 24.04) and 55% were women.
Figure 1. Reporting clinic, percentage based on N = 1702 healthcare workers incident reports and N = 11,006 patient incident reports. Missing information on reporting clinic in 45 patient incident reports.
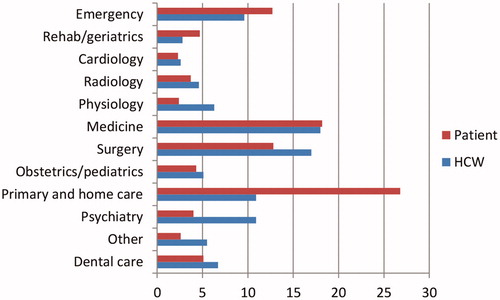
Table 2. Data quality assessment of patient (N = 11,006) and HCW incident reports (N = 1,702) during the years 2011–2014. The numbers are the percentages of reports containing the indicated data.
Accidental patient falls
Patient falls were reported in 17% (n = 1860) of all incident reports and almost all occurred in nursing care (99%). The mean age of the patients who fell was 78 years (SD 15.18), and about half were male (52%). During the study period, 2% of the falls were reported to require treatment and resulted in permanent harm, 13% required treatment but did not result in permanent harm, 32% resulted in harm but did not require treatment and in 52%, no harm was reported. One percent of the falls caused death (n = 15). Patient falls were most frequently reported from primary and homecare (37%), medical clinics (29%), emergency wards (16%), and rehabilitation/geriatric clinics (9%). The analysis of the free text describing the sequence of the incident resulted in the following 8 subcategories: fall when transfer was assisted by an HCW (patient manual handling), fall out of bed, fall with mobility aids, fall when walking/standing/rising, fall when going to the toilet, fall at night, found on the floor, and fall not specified in the text. According to the reports, most patients fell in unassisted situations (94%), primarily when going to the toilet (27%) or they were just found on the floor (20%). In approximately 6% of the fall incidents, an HCW was assisting the patient ().
Table 3. Classification of the sequence of all fall incidents and those assisted by HCWs.
Healthcare workers’ incidents and injuries
The majority of the 1702 HCW incidents and injuries were registered from medical clinics (18%), surgical clinics (17%), primary and home care (11%), and emergency wards, including ambulance travel (10%) (). The following professions reported incidents and injuries: nurses (41.6%), assistant nurses (22.5%), dental personnel (6.6%), mental health personnel (6%), physicians (5.9%), biomedical analysts (4.5%), administrative personnel (3.5%), midwives (2.1%), PTs (1.5%), occupational therapists (1.2%), students (1.5%), and social therapy staff, medical technical staff, and those registered as other occupations (7.6%). The mean age of the HCWs was 42 years (SD 12.7) and the majority were women (86.8%). In total, 2436 injuries were reported among the HCWs. The prevalence of reported incidents during the years 2011 to 2014 varied between 3.1 and 3.8%. The incidents were categorised in the IRS into five injury severity levels – 0.1% resulted in death, 3% required treatment and resulted in permanent harm, 13% required treatment but did not result in permanent harm, 59% did not require treatment and 25% resulted in no harm. The vast majority of the incidents happened at work (85%), with the rest occurring while commuting to and from work. The type of injury and the situations at work where the incidents and injuries occurred are presented in . In total, the most common injury was sharp object or needle stick injury (44.1%), followed by threats and workplace violence (18.6%) and patient manual handling (10.2%). The patient was present in 74% of all reported incidents (). The most frequent injuries for nurses were a sharp object or needle stick injury, threat and workplace violence, falls followed by patient manual handling. For nurses, the incidents happened mainly at work (89%) and the rest while commuting to and from work (11%). For assistant nurses, the most frequent injuries were a sharp object or needle stick injury, patient manual handling, threat and workplace violence followed by falls. For assistant nurses, the incidents happened mainly at work (88%) and the rest while commuting to and from work (12%). The most frequent injuries for PTs were falls followed by needle stick injury and patient manual handling. For PTs, the incidents happened both at work (60%) and while commuting to and from work (40%).
Table 4. Reported situation when occupational incidents and injury occurred at work.
Several occupational injuries were reported by the HCWs, primarily occurring when reaching, bending, and lifting and mostly related to patient manual handling. The most commonly reported body locations for injury were ‘trunk, shoulder, arm, hand’ (11.2%) and ‘lower back’ (8.4%). The lower back pain was most frequently reported by nurses and nurse assistants (7.4%). Other reported body locations of injuries were ‘hip, knee, ankle’ (4.8%) and ‘neck and head’ (3.4%). Mental illness due to workplace violence or high work demands was reported in 6%. Other reported occupational injuries were ‘crushes, dislocations, fractures’ (5.8%). In several incidents, both the patients and the HCW were injured, which to some extent, were reported in the IRS for HCW.
Discussion
We explored both patient injuries and HCW incidents and injuries reported in an IRS. Because accidental falls are still among the most commonly reported patient incidents, the reports’ descriptions of the incidents regarding falls were analysed. The incidents and injuries of HCWs were also analysed with a particular focus on the types of injuries, who was injured, and the situations in which they occurred. The majority of the patient and HCW incidents and injuries were reported from primary and homecare followed by medical clinics and emergency wards.
This study showed that severe patient injuries are still prevalent in Swedish healthcare, with 15% of the injuries requiring treatment and 2% resulting in death. Seventeen percent of the injuries were falls, mostly in homecare, medical clinics, and emergency wards. Consistent with previous research [Citation18], older patients were more likely to be included in an incident report and to suffer a fall. Falls were also more frequently reported as harmful and patients mostly fell when going to the toilet or they were just found on the floor.
Patients were present in 75% of the incidents and injuries involving HCWs, suggesting that risk assessments for patients and HCWs should be combined in order to prevent risks and to promote a healthy and sustainable healthcare environment. In a study by McCaughey et al. [Citation24], injuries and illnesses in the workplace were found to be associated with poor perceptions of the workplace safety climate.
The annual prevalence of HCW incidents and injuries was about 3%. The highest rate of injuries was found among nurses and nurse assistants and the most commonly reported injuries were from sharp instruments or needle sticks. These injuries are frequent and costly [Citation25,Citation26]. Factors associated with injuries from needles and sharp objects are age, level of education, number of shifts per month, and history of related training [Citation26]. Other frequent incidents reported by HCWs were threats and violence. This is a problem, especially in psychiatric care and emergency wards and has been reported by various health professionals [Citation27]. Other frequent injury situations were patient manual handling, including positioning, transferring, and lifting. The most commonly reported pain locations were the trunk, shoulder, arm, hand and lower back. Andersen et al. [Citation28] found an association with daily patient transfer and increased risk for back injury among HCWs and the use of assistive devices reduced the risk.
In this study, PTs reported a low incidence of work-related injuries, where the most frequent injuries for PTs were falls. The incidents caused conditions affecting mostly parts of the upper body and back. It is known that underreporting of injuries among healthcare workers is a problem, which might be the case for PTs in the present study. Previous research including PTs has mainly focussed on work-related musculoskeletal disorders (WMSD) among PTs. In one review, Vieira et al. [Citation29] summarises that up to 50–90% have WMSD during their careers where low back pain is the body part most commonly affected. Another study by Darragh et al. [Citation30] analysed injury incidents among PTs and occupational therapists. They found that among 248 injury incidents, manual therapy and transfers/lifts were associated with 54% of all injuries.
Methodological considerations
A strength of this retrospective study is that it included the total number of a County’s reported HCW incidents and patient injuries during the years 2011–2014, providing two perspectives. The information is provided by the individual staff member, giving their view of the incident. As shown in , the incident reports provided the required information indicating good quality of the data and thus strengthening the validity of the analysis. Furthermore, data from IRSs can yield learning at the organisational and individual levels as previously suggested [Citation19]. The main analysis focussed on the free-text section, which might capture the true value of the reports [Citation18]. This free-text section from all HCW reports was considered the unit of analysis. Due to the large amount of data and the fact that accidental patient falls are not declining similarly to other harmful incidents [Citation2], we selected patient falls in as the unit of analysis.
In this study, the overall reporting rates of patient injuries decreased slightly during 2011–2014. Previous research has found that the overall reporting rate is low for both patient and HCW injuries [Citation31] and this might indicate a further need for improved safety culture. Incident reporting is encouraged due to its potential to enable organisational learning and thereby improve safety [Citation13,Citation15] and open environments and reduced fear of punitive responses might increase incident reporting [Citation22].
We have no information about the quantity of missing data, i.e. incidents that were not reported or the quality of incidents not being classified as injuries. Thus, a limitation of this study is the lack of complementary data sources that might have enriched the analysis regarding the sequences of the incidents. Further inquiry into how to enhance HCW and patient safety would need not only medical record reviews and prospective studies, but also qualitative studies combining observations and interviews with HCWs and patients.
Practical implications
Employers in healthcare are recommended to use incident reports every time there is an incident for HCWs and/or patients. Incident reports capture information that provides a learning opportunity by identifying injury risk factors. In clinical practice, risk assessment for patients and for HCWs should be combined in order to prevent risks and to promote healthy and sustainable healthcare environments. In line with previous research, our findings further emphasise that patient and HCW safety are connected [Citation9,Citation11]. The results from this study highlight that patient falls are frequent in many wards, indicating the need for assessments of functioning, risks, and tailored interventions. We suggest that employers in collaboration with PTs and other HCWs and the occupational health services discuss how risks are assessed at the workplace using a human factor system approach. By providing assessments of functioning, risks and tailored interventions, PTs at different healthcare settings, wards and teams may play an important role in safe patient manual handling for both patients and HCW.
Conclusions
Patient and HCW injuries are still prevalent in Swedish healthcare and a substantial part of the HCW incidents involved a patient situation. Frequent injuries among HCWs were due to sharp-object injuries, violence, and patient manual handling. As many as 15% of the patient injuries were so severe that they required treatment and patient falls were reported in 17% of the incidences. Patients are more likely to fall when unassisted and impaired balance and muscle strength are major contributing factors to patient falls. These are known risk factors, which can be assessed and targeted in a fall prevention programme of which PTs can play an important role. The majority of both patient and HCW incidents were reported from primary/homecare, medical clinics, and emergency wards. These findings indicate the need to create a safer healthcare environment for patients and HCW at many units. It may be suggested that PTs and other HCW in collaboration with employers and union can increase their awareness of patient and HCW safety in daily practice where incident reports can be used to gain deeper knowledge on incidents.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- de Vries EN, Ramrattan MA, Smorenburg SM, et al. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17:216–223.
- Socialstyrelsen. Lägesrapport inom patientsäkerhetsområdet, 2016;4:21.
- Bernal D, Campos-Serna J, Tobias A, et al. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: a systematic review and meta-analysis. Int J Nurs Stud. 2015;52:635–648.
- Davis KG, Kotowski SE. Prevalence of musculoskeletal disorders for nurses in hospitals, long-term care facilities, and home health care: a comprehensive review. Hum Factors. 2015;57:754–792.
- Holtermann A, Clausen T, Aust B, et al. Risk for low back pain from different frequencies, load mass and trunk postures of lifting and carrying among female healthcare workers. Int Arch Occup Environ Health. 2013;86:463–470.
- Reme SE, Shaw WS, Boden LI, et al. Worker assessments of organizational practices and psychosocial work environment are associated with musculoskeletal injuries in hospital patient care workers. Am J Ind Med. 2014;57:810–818.
- Bae SH. Assessing the relationships between nurse working conditions and patient outcomes: systematic literature review. J Nurs Manag. 2011;19:700–713.
- Tvedt C, Sjetne IS, Helgeland J, et al. An observational study: associations between nurse-reported hospital characteristics and estimated 30-day survival probabilities. BMJ Qual Saf. 2014;23:757–764.
- Kramer T, Schneider A, Spiess E, et al. Associations between job demands, work-related strain and perceived quality of care: a longitudinal study among hospital physicians. Int J Qual Health Care. 2016;28:824–829.
- Agnew C, Flin R, Mearns K. Patient safety climate and worker safety behaviours in acute hospitals in Scotland. J Safety Res. 2013;45:95–101.
- Eklöf M, Törner M, Pousette A. Organizational and social-psychological conditions in healthcare and their importance for patient and staff safety. A critical incident study among doctors and nurses. Safety Sci. 2014;70:211–221.
- Runciman W, Hibbert P, Thomson R, et al. Towards an International Classification for Patient Safety: key concepts and terms. Int J Qual Health Care. 2009;21:18–26.
- Hudson P. Applying the lessons of high risk industries to health care. Qual Saf Health Care. 2003;12 Suppl 1:i7–12.
- European Commission, Patient Safety and Quality of Care working group. Key findings and recommendations on Reporting and learning systems for patient safety incidents across Europe.
- World Health Organization. World alliance for patient safety: WHO draft guidelines for adverse event reporting and learning systems: from information to action. Geneva, Switzerland, World Health Organization, 2005.
- Hutchinson A, Young TA, Cooper KL, et al. Trends in healthcare incident reporting and relationship to safety and quality data in acute hospitals: results from the National Reporting and Learning System. Qual Saf Health Care. 2009;18:5–10.
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, et al. Human factors systems approach to healthcare quality and patient safety. Appl Ergon. 2014;45:14–25.
- Howell AM, Burns EM, Bouras G, et al. Can patient safety incident reports be used to compare hospital safety? Results from a quantitative analysis of the English national reporting and learning system data. PLoS One. 2015;10:e0144107.
- Ahlberg E-L, Elfström J, Risberg Borgstedt M, et al. Learning from incident reporting? Analysis of incidents resulting in patient injuries in a web-based system in Swedish health care. J Patient Safety.2017;1. (Nov 4.) doi: 10.1097/PTS.0000000000000343. [Epub ahead of print].
- Westbrook JI, Li L, Lehnbom EC, et al. What are incident reports telling us? A comparative study at two Australian hospitals of medication errors identified at audit, detected by staff and reported to an incident system. Int J Qual Health Care. 2015;27:1–9.
- Hignett S, Sands G, Griffiths P. In-patient falls: what can we learn from incident reports? Age Ageing. 2013;42:527–531.
- Krippendorff K. Content analysis. An introduction to its methodology. 3rd ed. Thousands Oaks: Sage Publications, Inc.; 2013.
- Downe-Wamboldt B. Content analysis: method, applications, and issues. Health Care Women Int. 1992;13:313–321.
- McCaughey D, DelliFraine JL, McGhan G, et al. The negative effects of workplace injury and illness on workplace safety climate perceptions and health care worker outcomes. Safety Sci. 2013;51:138–147.
- Elseviers MM, Arias-Guillen M, Gorke A, et al. Sharps injuries amongst healthcare workers: review of incidence, transmissions and costs. J Ren Care. 2014;40:150–156.
- Motaarefi H, Mahmoudi H, Mohammadi E, et al. Factors associated with needlestick injuries in health care occupations: a systematic review. J Clin Diagn Res. 2016;10:IE01–IIE4.
- Groenewold MR, Sarmiento RFR, Vanoli K, et al. Workplace violence injury in 106 US hospitals participating in the Occupational Health Safety Network (OHSN), 2012–2015. Am J Ind Med 2017;61(2):157–166.
- Andersen LL, Burdorf A, Fallentin N, et al. Patient transfers and assistive devices: prospective cohort study on the risk for occupational back injury among healthcare workers. Scand J Work Environ Health. 2014;40:74–81.
- Vieira ER, Schneider P, Guidera C, et al. Work-related musculoskeletal disorders among physical therapists: a systematic review. BMR. 2016;29:417–428.
- Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists. Work. 2012;42:373–384.
- Tricarico P, Castriotta L, Battistella C, et al. Professional attitudes toward incident reporting: can we measure and compare improvements in patient safety culture? Int J Qual Health Care. 2017;29:243–249.
