Abstract
Background
Physical exercises targeting proprioception are part of conservative therapy for Subacromial Pain Syndrome (SAPS). However, the effect of such exercises on proprioception itself has not been orderly established, hampering the advancement of treatment protocols and implementation. We summarised the evidence for a loss of proprioception in SAPS and defined the type of interventions that target and improve proprioception in SAPS.
Methods
Two reviewers independently analysed 12/761 articles that evaluated joint position, kinaesthetic or force sense in patients with SAPS.
Results
Patients with SAPS had reduced joint position sense during abduction. There was no evidence for a loss of kinaesthetic sense or force sense. Stretching, strengthening and stabilisation exercises improved joint position and kinaesthetic sense in SAPS. Microcurrent electrical stimulation and kinesiotaping did not improve proprioception in SAPS.
Conclusions
The lack of evidence on proprioception in SAPS is striking. We found limited evidence for a loss of joint position sense in the higher ranges of abduction in SAPS. Active training programmes including strengthening and stabilisation exercises showed superiority in terms of enhancing proprioception relative to passive methods like kinesiotaping. The results of this narrative synthesis should be used as a base for providing value-based and data-driven treatment solutions to SAPS.
PROSPERO::
Introduction
Chronic shoulder pain is the second most common musculoskeletal disorder in the general population, with prevalence rates ranging between 15% and 22% [Citation1–3]. In approximately 29–34% of all patients with chronic shoulder pain a specific anatomical explanation (e.g. acromioclavicular osteoarthritis, calcific tendinitis, or full-thickness rotator cuff tears) is not present, and the condition of these patients is described as Subacromial Pain Syndrome (SAPS) [Citation4,Citation5]. This prevalent condition becomes chronic frequently and the associated pain, sleep disturbance and restrictions in activities of daily living have a substantial impact on an individual’s quality of life [Citation6]. Recent studies suggest that surgical treatment provides no significant benefit over non-surgical intervention and while conservative management is effective, more targeted approaches are warranted [Citation4,Citation5,Citation7–9].
A systematic review dating from 2015 showed evidence for a loss of proprioception in SAPS and studies have demonstrated a clinical benefit of exercises targeting proprioception in SAPS [Citation10–12]. Hence, conservative management aimed at improving shoulder proprioception and active joint stabilisation is suggested as a viable targeted treatment approach in SAPS [Citation13–15]. The effect of exercises on proprioception itself has however not been orderly established, which hampers the advancement of treatment protocols and clinical implementation.
We were interested in defining the type of interventions that target proprioception in patients with SAPS and assessing whether these interventions improve proprioception. Because there has been an expansion of research on the loss of proprioception in SAPS since a systematic review in 2015 [Citation10], we first re-evaluated the evidence for a loss of proprioception in SAPS [Citation16–19]. Then, we summarised the effectiveness of different types of intervention on proprioception and symptoms in SAPS.
Material and methods
Protocol and registration
We conducted this review following the published guidelines by the International Committee of Medical Journal Editors (ICMJE) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [Citation20,Citation21]. The protocol was published (PROSPERO: No. CRD42017055520, registered 10/02/2017) prior to conducting the search [Citation22].
Information sources and search strategy
We performed the search with support from an expert librarian using PubMed, Embase, CINAHL, Web of Science, Cochrane Library, CENTRAL, Academic Search Premier, Emcare and ScienceDirect from inception to 27 February 2019. Search terms included text words and controlled vocabulary i.e. Medical Subheadings (MeSH) and equivalents related to (1) subacromial pain syndrome and (2) proprioception [Citation23]. These components were combined with the operator, ‘AND’ and the search was performed without any limits (Supplementary material). We also included relevant articles from the reference lists of included articles and reference lists of systematic reviews on similar topics.
Study selection
We managed search data using a reference manager (EndNote X7.7.1. 2016; Thomson Reuters). Duplicates were removed and titles and abstracts were individually screened for eligibility by two researchers (CLO, HG). SAPS was defined as shoulder pain that exacerbated by abduction, with at least one positive clinical test for SAPS (e.g. Neer test, Hawkins test, Jobe test) [Citation24]. Articles had to furthermore measure aspects of proprioception, including Joint Position Sense, Kinaesthetic Sense and Force Sense. These aspects of proprioception can be measured with good reliability using Joint Position Reproduction (JPR), measurement of the Threshold To Detection of Passive Movement (TTDPM) and force steadiness testing, repsectively [Citation14–16,Citation22,Citation23]. Exclusion criteria included signs of other shoulder pathology (e.g. acromioclavicular osteoarthritis, massive tears, isolated subscapularis tears, frozen shoulder), primary or secondary glenohumeral osteoarthritis, glenohumeral instability disorder, neuromuscular disorder (e.g. cerebral ischaemic attack, muscular dystrophy), no measurement of proprioception, surgical intervention, inappropriate study design (e.g. systematic review, letters to the editor), non-peer reviewed articles in languages other than Dutch, German or English language. We accessed the full-text in cases of uncertainty regarding the eligibility of an article and disagreements were solved by means of discussion with a third reviewer (JN) until consensus was reached.
Assessment of methodological quality
The full-text of all included articles were assessed for methodological quality for each study question separately. We used the validated Effective Public Health Practice Project (EPHPP) instrument, which scores six components (i.e. selection bias, study design, confounders, blinding, data collection method and withdrawals/drop-outs) on an ordinal scale, i.e. (1) strong, (2) moderate and (3) weak [Citation25,Citation26]. This grading system allows for the assessment of both observational, non-randomised studies as well as interventional, randomised or clinical controlled trials [Citation25]. An additional quality assessment of two components (intervention integrity and assessment of analyses) was performed for studies related to our second study question i.e. interventions targeting proprioception, using the same ordinal scale [Citation25]. We then assigned a rating for overall methodological quality for each study; i.e. (1) strong, (2) moderate or (3) weak global rating [Citation25]. A strong rating was given if there were no weak ratings in any components, moderate if there was one weak rating, and weak if there are two or more weak ratings [Citation25]. Two researchers (CLO, HG) assessed the quality of the articles independently and disagreements were solved via discussion with a third reviewer (JN) and reaching consensus.
Data collection and abstraction
We extracted the following data using a standardised data-abstraction sheet: (1) author, year of publication and country; (2) study design, study populations, demographics (age/gender); (3) intervention, if applicable; (4) duration of follow-up, if applicable; (5) measurement method of Joint Position Sense, Kinaesthetic Sense and Force Sense and; (6) other reported outcome measures: e.g. clinical symptoms, patient reported outcome measures, if applicable. Due to the heterogeneity of studies in terms of the outcome measures and measurement methods, statistical pooling was not considered feasible or appropriate and thus, our conclusions were based on a narrative synthesis of study results and methodological quality.
Results
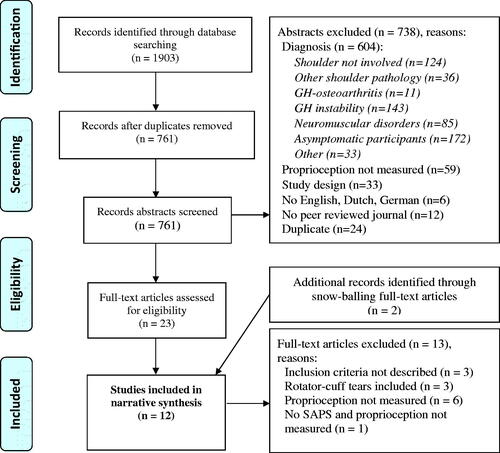
The search yielded 761 unique articles. After screening for eligibility, 738 studies were excluded, leaving 23 articles of which the full-text articles were screened for eligibility (flow diagram, ). Two additional articles were retrieved from the reference lists of included studies. Thirteen full-text articles were excluded, resulting in 12 articles for the final analysis () [Citation16–18,Citation27–35]. One study performed both a comparison of proprioception between patients with SAPS and controls and assessed the efficacy of an intervention in SAPS, and was therefore used for both study questions () [Citation32].
Table 1. Study characteristics.
Loss of proprioception in SAPS
Joint position sense
Three studies compared Joint Position Sense between a total of 73 patients with SAPS and 92 controls () [Citation16,Citation18,Citation34]. Joint Position Sense was tested using Joint Position Reproduction tasks (JPR) in scapular plane abduction (scaption) [Citation16] and axial humerus rotation [Citation18,Citation34]. Active JPR testing in scaption showed that patients with SAPS have a higher Degree of Mismatch (MMdegree) compared to controls at 100°, indicating reduced Joint Position Sense, which was not present during testing in 40° scaption () [Citation16]. During the testing in 100° scaption, patients experienced significantly more pain (3.4 cm on 10 cm Visual Analogue Scale) compared to testing in 40° scaption (1.8 cm on 10 cm Visual Analogue Scale), which may be associated with the observed reduction in Joint Position Sense [Citation16]. The risk of bias in this study was low, and a reliability assessment showed that measurements were performed with good reliability during testing in 40° and moderate reliability during testing in 100° () [Citation16]. During both passive and active axial humerus rotation testing neither of the two studies found a difference in MMdegree between patients with SAPS and controls [Citation18,Citation34]. Thus, Joint Position Sense in patients with SAPS may be affected during high scaption [Citation16], but seems to be preserved during axial humerus rotation [Citation18,Citation34]. It is yet unclear whether declined Joint Position Sense during high scaption is influenced by associated pain (or vice versa) [Citation16].
Table 2. Quality assessment of included full-text articles.
Table 3. Summary of results – loss of proprioception in SAPS.
Kinaesthetic sense
Using the Threshold to Detection of Passive Motion (TTDPM) testing method, the two case-control comparisons, which were of moderate [Citation34] and strong [Citation32] methodological quality (), showed no differences in MMdegree between patients with SAPS and controls in adduction and 60° scaption, thus Kinaesthetic Sense seems preserved in patients with SAPS ().
Force sense
Only one of four studies found a deficit in Force Sense [Citation28], and this was only in one of three tasks (concentric contraction, ), which suggests that Force Sense is not affected in patients with SAPS [Citation17,Citation28,Citation30,Citation31].
The effect of conservative interventions on proprioception in SAPS
There were five studies that assessed the effect of an active (e.g. strengthening exercises) [Citation29,Citation33] or passive (e.g. kinesiotape or microcurrent electrical stimulation) [Citation27,Citation32,Citation35] training programme on proprioception in a total of 103 patients with SAPS (10–32 patients study) [Citation27,Citation29,Citation32,Citation35,Citation36].
Active training programmes
The 6-weeks training programme of Baskurt et al. consisted of standardised flexibility exercises, strengthening, Codman exercises and scapular stabilisation exercises [Citation29]. Flexibility exercises focussed on anterior, posterior and inferior capsule stretching, next to forward flexion, abduction and internal rotation stretching. The subscapularis, infraspinatus, supraspinatus, and anterior part of deltoid and posterior part of deltoid were strengthened. Scapular stabilisation exercises consisted of scapular proprioceptive neuromuscular facilitation (PNF) exercises, scapular clock exercise, standing weight shift, double arm balancing, scapular depression, wall push up, wall slide exercises [Citation29].
The 4-weeks training programme of Jerosch and Wüstner consisted of standardised sensorimotor training for the glenohumeral joint, using proprioceptive exercise tools (body-blade, BOING), next to Tai Chi and aquatic gymnastic [Citation33].
Both studies showed that the active training programmes improved Joint Position Sense (and Kinaesthetic Sense [Citation33]) with a moderate [Citation33] and large [Citation29] risk of bias (). These studies also showed significant reduced pain (assessed with the Visual Analogue Scale [Citation29], Constant Score [Citation33] and University of California Los Angeles score [Citation33]) and reduced impairment or disability (assessed with the Constant Score [Citation33], Western Ontario Rotator Cuff index [Citation29] and University of California Los Angeles score [Citation33]) after intervention.
Table 4. Summary of results – effect of intervention.
Passive training programmes
No improvement in proprioception was observed using micro-current electrical stimulation, while symptoms did improve (weak methodological quality) [Citation27]. Both studies assessing the effect of kinesiotaping on proprioception, used the taping methods suggested by Kase et al. with slight differences [Citation37]. Next to a Y-strip covering the deltoid and a I-strip behind crossing the glenohumeral joint, De Oliveira applied a I-strip crossing the glenohumeral joint vertically [Citation35], while Keenan et al. [Citation32] applied a Y-strip from the insertion to the origin of the supraspinatus. Both studies showed no effect of kinesiotaping on proprioception (both strong methodological quality) [Citation32,Citation35]. The effect of these taping methods on symptoms was not assessed [Citation32,Citation35]. Altogether, passive methods including micro-current electrical stimulation [Citation27] or kinesiotaping [Citation32,Citation35] had no effect on proprioception.
Discussion
We included twelve studies in a narrative analysis on the loss of proprioception in SAPS and the effect of conservative interventions on proprioception in SAPS. Although two components of proprioception (Kinaesthetic Sense and Force Sense) seem to remain intact in SAPS, Joint Position Sense in higher angles of scapular plane elevation may be compromised. Passive therapeutic strategies, such as kinesiotape, did not yield an improvement in proprioception, whereas active training with strengthening and stabilisation exercises improved proprioception in SAPS.
Loss of proprioception in SAPS
We found no evidence for a loss of Kinaesthetic Sense or Force Sense in patients with SAPS [Citation17,Citation28,Citation30–32]. The well-powered, strong methodological quality study by Anderson and Wee [Citation16] suggests that patients with SAPS do have a loss of Joint Position Sense manifesting at higher scapular plane elevation angles, but not during axial humerus rotation.
It has been suggested that impaired Joint Position Sense present in patients with SAPS during abduction, but not during axial humerus rotation, means that glenohumeral proprioception is preserved and pain is the explanation for observed deficits during abduction [Citation34]. This explanation is contradicted by two experimental studies that showed reduced Joint Position Sense and increased asymmetry of scapular kinematics in response to pain relief with subacromial anaesthetics in patients with SAPS [Citation38,Citation39]. We therefore suggest an alternative line of reasoning. Electromyography studies have shown that patients with SAPS exhibit reduced co-contraction of shoulder girdle muscles during abduction, which is also related to excessive upward migration of the humerus during this movement [Citation40–42]. Subsequent reduced muscle tonus of antagonists (e.g. infraspinatus and teres major) results in reduced excitability of muscle spindles and this may explain impaired Joint Position Sense in patients with SAPS during abduction [Citation43].
Effect of interventions targeting proprioception
Based on consistent findings in two studies of moderate and weak methodological quality, it may be suggested that proprioception (Joint Position Sense [Citation29,Citation33] and Kinaesthetic Sense [Citation33]) in SAPS can be improved with exercise therapy aimed at enhancing shoulder stability [Citation29,Citation33] and strength [Citation29], either or not also aimed at enhancing range of motion [Citation29]. Additional well designed studies are warranted to confirm these findings.
Previous studies have suggested impaired active joint stabilisation as a causal factor in SAPS [Citation40–42] and the goal of exercises targeting proprioception would be to enhance joint stability [Citation40–42,Citation44,Citation45]. We suggest that effective exercises may accomplish enhanced joint stability in two ways. First, exercises may result in increased co-contraction of agonists and antagonists at the glenohumeral and scapulothoracal joint, which directly results in increased active stabilisation [Citation40–42]. Second, consequent increased tonus of antagonistic muscles may lower the excitation threshold of muscle spindles, enhancing Joint Position Sense, and thus active joint stabilisation [Citation43]. Considering also that muscle spindle information is the main source of input for Joint Position Sense, this would explain why passive strategies such as kinesiotape are less effective in improving Joint Position Sense in patients with SAPS [Citation27,Citation32,Citation35,Citation46].
This study had a number of limitations. First, we found only few relevant articles on the topic and therefore our conclusions should only serve as guidance for future studies and not for direct clinical interpretation. Second, due to inconsistency in diagnostic criteria for SAPS, variability in population characteristics may have occurred [Citation47]. In order to enhance the generalizability of our findings, we handled strict inclusion criteria. Third, sample sizes were low in five studies (≤20 participants per group). Four of these studies had negative results, and it cannot be made sure that there indeed was no effect, or that negative results may be explained by underpowering. Nevertheless, the findings of studies with low power were consistent with other higher powered studies and therefore we do not think that underpowering affected our conclusions. Fourth, regarding our second study question, the studies that showed a positive effect of active training programmes on proprioception did not include control groups without therapy and thereby did not account for a bias of time or natural regression to the mean [Citation29,Citation33]. In one of these, the follow-up duration was 4 weeks, while the pre-existent duration of complaints was minimal 3 months (mean 6.2 months) [Citation36]. Considering this pre-existent duration of complaints it seems unlikely that the observed improvement in proprioception would have also occurred without the intervention.
In patients with SAPS, it has been shown that surgical treatment provides no significant benefit over non-surgical intervention and physical therapy is preferable [Citation7–9]. We believe that physical therapy programmes can be improved with targeted approaches [Citation7]. Generally, the goal of these programmes is to enhance proprioception and active joint stabilisation [Citation40–42] through stability [Citation29,Citation33] and strength exercises [Citation29]. It has been suggested that increasing co-contraction of the arm adductors (teres major and latissimus dorsi) is a viable treatment option for patients with SAPS to enhance stability [Citation41,Citation42,Citation48,Citation49]. In future clinical assessments, it may be assessed whether enhancing proprioception and stability in patients with SAPS, for instance by training adductor co-contraction is effective. To gain insight into causal relationships, EMG monitoring, kinematic assessments to monitor excessive upward migration of the humerus during abduction and clinical evaluations may be used [Citation50–52].
Conclusion
For the prevalent condition SAPS, physical treatment is the treatment of choice, with exercise therapy focussing on proprioception and stability being cornerstone [Citation4,Citation5,Citation7–9]. In this narrative review we found a striking lack of evidence on proprioception in patients with SAPS. There was limited evidence for a reduction of Joint Position Sense during arm elevation (not during axial humerus rotation) in patients with SAPS [Citation16]. No evidence was found for a loss of Kinaesthetic Sense or Force Sense in patients with SAPS [Citation17,Citation28,Citation30–33]. It showed that active treatment programmes targeting proprioception, such as stability [Citation29,Citation33] and strength exercises [Citation29], enhance Joint Position Sense and Kinaesthetic Sense, while passive strategies, such as kinesiotaping, do not improve proprioception in patients with SAPS [Citation27,Citation32,Citation35]. Providing value-based and data driven solutions to common shoulder problems such as SAPS should be the goal of practicing orthopaedic surgeons, general practitioners and physical therapists. The findings of this review may serve as a base for further studies into the development of targeted conservative treatment approaches in SAPS.
Supplementary_material__search_strategy.docx
Download MS Word (21.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS). 3rd ed. Rosemont (IL); 2014. [cited 2019 Feb 12]. Available from: http://www.boneandjointburden.org
- Picavet HS, Schouten JS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain. 2003;102(1–2):167–178.
- Andersson HI, Ejlertsson G, Leden I, et al. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9(3):174–182.
- de Witte PB, Overbeek CL, Navas A, et al. Heterogeneous MR arthrography findings in patients with subacromial impingement syndrome - diagnostic subgroups? J Electromyogr Kinesiol. 2016;29:64–73.
- Vecchio P, Kavanagh R, Hazleman BL, et al. Shoulder pain in a community-based rheumatology clinic. Br J Rheumatol. 1995;34(5):440–442.
- van der Windt DA, Koes BW, de Jong BA, et al. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54(12):959–964.
- Hanratty CE, McVeigh JG, Kerr DP, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum. 2012;42(3):297–316.
- Beard DJ, Rees JL, Cook JA, et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet. 2018;391(10118):329–338.
- Kolk A, Thomassen BJW, Hund H, et al. Does acromioplasty result in favorable clinical and radiologic outcomes in the management of chronic subacromial pain syndrome? A double-blinded randomized clinical trial with 9 to 14 years' follow-up. J Shoulder Elbow Surg. 2017;26(8):1407–1415.
- Fyhr C, Gustavsson L, Wassinger C, et al. The effects of shoulder injury on kinaesthesia: a systematic review and meta-analysis. Man Ther. 2015;20(1):28–37.
- Nakra N, Quddus N, Khan S, et al. Efficacy of proprioceptive neuromuscular facilitation on shoulder function in secondary shoulder impingement. Int J Ther Rehabil. 2013;20(9):450–459.
- Marzetti E, Rabini A, Piccinini G, et al. Neurocognitive therapeutic exercise improves pain and function in patients with shoulder impingement syndrome: a single-blind randomized controlled clinical trial. Eur J Phys Rehabil Med. 2014;50(3):255–264.
- Myers JB, Lephart SM. The role of the sensorimotor system in the athletic shoulder. J Athl Train. 2000;35(3):351–363.
- Pedersen J, Lonn J, Hellstrom F, et al. Localized muscle fatigue decreases the acuity of the movement sense in the human shoulder. Med Sci Sports Exerc. 1999;31(7):1047–1052.
- Riemann BL, Lephart SM. The sensorimotor system, part I: the physiologic basis of functional joint stability. J Athl Train. 2002;37(1):71–79.
- Anderson VB, Wee E. Impaired joint proprioception at higher shoulder elevations in chronic rotator cuff pathology. Arch Phys Med Rehabil. 2011;92(7):1146–1151.
- Maenhout AG, Palmans T, De Muynck M, et al. The impact of rotator cuff tendinopathy on proprioception, measuring force sensation. J Shoulder Elbow Surg. 2012;21(8):1080–1086.
- Haik MN, Camargo PR, Zanca GG, et al. Joint position sense is not altered during shoulder medial and lateral rotations in female assembly line workers with shoulder impingement syndrome. Physiother Theory Pract. 2013;29(1):41–50.
- Machner A, Merk H, Becker R, et al. Kinesthetic sense of the shoulder in patients with impingement syndrome. Acta Orthop Scand. 2003;74(1):85–88.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341.
- International Committee of Medical Journal Editors. Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals. 2013.
- PROSPERO. Centre for reviews and dissemination. http://wwwcrdyorkacuk/PROSPERO. 2016.
- PubMed Help [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2005. PubMed Help. [updated 2018 Mar 28; cited 2018 April 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK3827/
- Diercks R, Bron C, Dorrestijn O, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 2014;85(3):314–322.
- Thomas BH, Ciliska D, Dobbins M, et al. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–184.
- Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003;7(27):iii–ii1, x, 173.
- Atya AM. Efficacy of microcurrent electrical stimulation on pain, proprioception accuracy and functional disability in subacromial impingement. RCT. Indian J Physiother Occup Ther. 2012;6(1):15–18.
- Bandholm T, Rasmussen L, Aagaard P, et al. Force steadiness, muscle activity, and maximal muscle strength in subjects with subacromial impingement syndrome. Muscle Nerve. 2006;34(5):631–639.
- Başkurt Z, Başkurt F, Gelecek N, et al. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. BMR. 2011;24(3):173–179.
- Zanca GG, Camargo PR, Oliveira AB, et al. Isometric medial and lateral rotations torque steadiness in female workers with shoulder impingement. IES. 2010;18(3):115–114.
- Camargo PR, Avila MA, de Oliveira AB, et al. Shoulder abduction torque steadiness is preserved in subacromial impingement syndrome. Eur J Appl Physiol. 2009;106(3):381–387.
- Keenan KA, Akins JS, Varnell M, et al. Kinesiology taping does not alter shoulder strength, shoulder proprioception, or scapular kinematics in healthy, physically active subjects and subjects with Subacromial Impingement Syndrome. Phys Ther Sport. 2017;24:60–66.
- Jerosch J, Wustner P. [Effect of a sensorimotor training program on patients with subacromial pain syndrome]. Unfallchirurg. 2002;105(1):36–43.
- Gomes BSQ, Coelho VK, Terra BS, et al. Patients with subacromial pain syndrome present no reduction of shoulder proprioception: a matched case-control study. Pm R. 2019;11(9):972–978.
- de Oliveira FCL, Pairot de Fontenay B, Bouyer LJ, et al. Immediate effects of kinesiotaping on acromiohumeral distance and shoulder proprioception in individuals with symptomatic rotator cuff tendinopathy. Clin Biomech (Bristol, Avon). 2019;61:16–21.
- Jerosch J, Brinkmann T, Schneppenheim M. The angle velocity reproduction test (AVRT) as sensorimotor function of the glenohumeral complex. Arch Orthop Trauma Surg. 2003;123(4):151–157.
- Kase T, Kase K, Wallis J. Clinical therapeutic applications of the Kinesio taping method. Tokyo (Japan): Ken Ikai Co; 2003.
- Ettinger LR, Shapiro M, Karduna A. Subacromial anesthetics increase proprioceptive deficit in the shoulder and elbow in patients with subacromial impingement syndrome. Clin Med Insights Arthritis Musculoskelet Disord. 2017;10:1179544117713196.
- Kolk A, Henseler JF, de Witte PB, et al. Subacromial anaesthetics increase asymmetry of scapular kinematics in patients with subacromial pain syndrome. Man Ther. 2016;26:31–37.
- Keramat KU, Creesh MK, Kropmans T. Voluntary co-contraction exercise effective in early stage of subacromial impingement syndrome management. IJRS. 2015;4(2):7–13.
- Graichen H, Hinterwimmer S, von Eisenhart-Rothe R, et al. Effect of abducting and adducting muscle activity on glenohumeral translation, scapular kinematics and subacromial space width in vivo. J Biomech. 2005;38(4):755–760.
- Overbeek CL, Kolk A, de Groot JH, et al. Altered cocontraction patterns of humeral head depressors in patients with subacromial pain syndrome: a cross-sectional electromyography analysis. Clin Orthop Relat Res. 2019;477(8):1862–1868.
- Burke D, Eklund G. Muscle spindle activity in man during standing. Acta Physiol Scand. 1977;100(2):187–199.
- Graichen H, Bonel H, Stammberger T, et al. Three-dimensional analysis of the width of the subacromial space in healthy subjects and patients with impingement syndrome. AJR Am J Roentgenol. 1999;172(4):1081–1086..
- Deutsch A, Altchek DW, Schwartz E, et al. Radiologic measurement of superior displacement of the humeral head in the impingement syndrome. J Shoulder Elbow Surg. 1996;5(3):186–193.
- Gilman S. Joint position sense and vibration sense: anatomical organisation and assessment. J Neurol Neurosurg Psychiatry. 2002;73(5):473–477.
- de Witte PB, de Groot JH, van Zwet EW, et al. Communication breakdown: clinicians disagree on subacromial impingement. Med Biol Eng Comput. 2014;52(3):221–231.
- Beaudreuil J, Lasbleiz S, Aout M, et al. Effect of dynamic humeral centring (DHC) treatment on painful active elevation of the arm in subacromial impingement syndrome. Secondary analysis of data from an RCT. Br J Sports Med. 2015;49(5):343–346.
- Overbeek CL, Kolk A, Nagels J, et al. Increased co-contraction of arm adductors is associated with a favorable course in subacromial pain syndrome. J Shoulder Elbow Surg. 2018;27(11):1925–1931.
- Holtermann A, Mork PJ, Andersen LL, et al. The use of EMG biofeedback for learning of selective activation of intra-muscular parts within the serratus anterior muscle: a novel approach for rehabilitation of scapular muscle imbalance. J Electromyogr Kinesiol. 2010;20(2):359–365.
- Huang HY, Lin JJ, Guo YL, Wang WT, et al. EMG biofeedback effectiveness to alter muscle activity pattern and scapular kinematics in subjects with and without shoulder impingement. J Electromyogr Kinesiol. 2013;23(1):267–274.
- Larsen CM, Juul-Kristensen B, Olsen HB, et al. Selective activation of intra-muscular compartments within the trapezius muscle in subjects with Subacromial Impingement Syndrome. A case-control study. J Electromyogr Kinesiol. 2014;24(1):58–64.