Abstract
Objectives
Research into work-related factors that positively influence Oral Health Providers (OHPs) health is scarce. This study aimed to analyse which OHPs in dental services remain healthy over time in relation to work- and health-related factors.
Methods
OHPs took part in this prospective cohort study (n = 168). In 2012 and 2014 they answered a questionnaire featuring questions about demographics, health indicators, work and organisational factors.
Results
OHPs were classified into three subgroups; healthy group (n = 66), semi-healthy group (n = 45) and unhealthy group (n = 57). The healthy group reported no sick leave or sickness presence in 2012 or 2014. Factors that explained a greater likelihood of belonging to the healthy group were: good work ability, not having neck pain, perceived low exertion at the end of the working day, not having sleeping problems. They scored higher on health indicators than OHPs in the unhealthy group.
Conclusions
OHPs with no sick leave or sickness presence report much better salutogenic health, better physical work ability and lower perceived exertion at the end of their workday compared with unhealthy group of OHPs. Understanding the relationship between working conditions and well-being is crucial to target interventions for OHPs which improve work conditions and health.
Introduction
Studies of dental workplace environments have mainly focussed on pathogenic factors, i.e. risk factors such as high perceived physical and mental workload especially among dentists and dental hygienists [Citation1–3]. The most common sites for musculoskeletal problems among Oral Health Providers (OHPs) are the neck, shoulders, lower back and wrist [Citation2,Citation4,Citation5]. OHPs includes the professions dentist, dental nurses and dental hygienists. There is consistent evidence that occupational health-related problems are prevalent among employees in dental organisations, and the risk of work related injuries is still a major concern [Citation2,Citation5]. A recent study reported the prevalence of injuries for both patients and employees in healthcare and dentistry indicating the need for prevention, assessments of risks, and tailored interventions at the workplace [Citation6]. Work-related stress is reported to be prevalent also [Citation2,Citation7]. Previous research shows that some of the factors associated with burnout in dental personnel are younger age, high job-strain/working hours, certain personality types, and having a high proportion of challenging patients [Citation8,Citation9]. Overall, OHPs are at an increased risk of musculoskeletal disorders because the work is often monotonous and repetitive and involves static postures [Citation10]. Both physical and psychosocial problems in the work environment are reported to contribute to sickness absence. Workplace health promotion often involves strategies to maintain and improve the health and wellbeing of employees. This is line with the salutogenic theory, which focuses on health promoting factors rather than risk factors [Citation11]. For a salutogenic approach at the workplace, it must be comprehensible, manageable and meaningful for employees, where job-related resources are important for coherent work experiences [Citation12]. In a study by Lindberg and Vingård, several factors were found to be important for a workplace to be perceived as healthy [Citation13]. Some of the most important were good collaboration and teamwork; opportunities to develop as an individual; having a fair, accessible and supportive leader; and appropriate staffing. It was also important to give appreciation, have a culture of employee involvement and for work to be physically safe. Based on previous research it is therefore reasonable to assume that both individual and organisational work-environment factors influence perceived health. So far, few studies of factors that contribute to good work-related health in dentistry have focussed on OHPs who stay healthy and the factors which are associated with well-being and a healthy and meaningful working life. Recent work by our team has shown that, from a salutogenic perspective, many OHPs reported a positive experience of working life [Citation14]. Previous research shows that better mental well-being is related to a high perception of personal mastery and high management support [Citation15]. Organisational factors also seem to be important for job satisfaction among dentists [Citation16]. The dental workplace is an arena with potential for health promotion since many OHPs spend 30–40 h or more per week at work. Thus, work is also significant for their general circumstances and their health [Citation12]. Hitherto, little research has been carried out into work-related factors that positively influence the health of dentists, dental hygienists and dental nurses. The overall aim of this study is to analyse, from a salutogenic perspective, which OHPs in the public dental service remain healthy at work and which organisational, work- and health-related factors contribute to this. The main aim is to analyse the extent to which health and work-related factors influence the ability to stay healthy at work over time. The research questions are, I) to explore how OHPs with no sick leave or sickness presenteeism perceive leadership, support at work, working conditions, job control and demands, health, and work ability and, II) to compared this with OHPs with reported sickness absence and/or sickness presenteeism.
Method
This prospective cohort study is part of the Dental Organisation in Transition in Sweden survey (DOiT). It is a follow up of previous studies of the public dental service in a Swedish county. The dental staffs from each dental clinic were first informed about the study and also that participation was voluntary. All 486 employees including dentists, dental hygienist and dental nurses, in the dental organisation were given the opportunity to complete a web survey, both part time and fulltime employees. All participants should be able to understand Swedish to be able to answer the web survey.
The questionnaire was developed as a web survey using the EsMaker NX3 software, with the link emailed to the recipients. The response rate in 2012 was 66%. A follow-up questionnaire was administered in 2014 to all 510 employees in the dental organisation (response rate 65%). EsMaker NX3 was used for the web survey that was sent to the study population. This study uses data from the dentists, dental hygienists and dental nurses who completed the questionnaire in both 2012 and 2014 (n = 168). The total dropout was just over 67%. A review of the databases in 2012 and 2014 indicates a random drop out. A participant could be either healthy or unhealthy or both at baseline and during the entire study period. In order to identify these variations, the web survey variables sickness presenteeism (remaining at work when unwell) and sickness absence were used to classify the study population of OHPs into three health subgroups; a) the healthy group, b) the semi-healthy group, and c) the unhealthy group. The classification into subgroups was made by the research group. The healthy group was defined as having reported no sickness absence or sickness presenteeism in either 2012 or 2014. The semi-healthy group had sickness absence and/or sickness presenteeism in 2012 or 2014. The unhealthy group had sickness absence and sickness presenteeism in both 2012 and 2014 (). The theoretical reasoning was that we wanted to compare self-reported health patterns among OHPs to increase knowledge about health promoting factors. The survey included demographic items such as sex, age, profession, years in the profession, working hours per week and size of dental clinic. The survey also included work-related factors concerning, health, pain, work ability, sickness presenteeism, and sick leave. Further items were work-related organisational factors like leadership, support at work, working conditions, job control and demands, and work experience. All measurements are described below and in detail elsewhere [Citation1,Citation14,Citation17]. The results in and are presented from a salutogenic perspective in percent and, is based on responses from all OHPs (n = 168).
Figure 1. Conditions for sickness presence and sickness absence for (A) Healthy group, (B) Semi healthy group and (C) Unhealthy group.
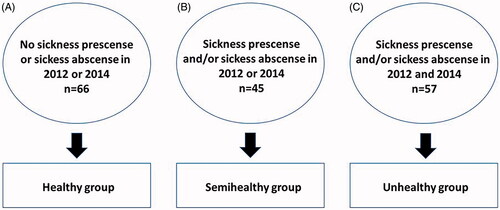
Table 2. Comparison between subgroups; (A) Healthy Group (Healthy) (n = 66), (B) Semi Healthy group (Semi healthy) (n = 45), (C) Unhealthy Group (Unhealthy) (n = 57) concerning work ability and musculoskeletal pain in percent (%).
Table 3. Physical and psychosocial work place conditions work posture, precision demands, perceived exertion psychosocial demands, work control, social support, good leadership, WEMS, SHIS in percent (%).
Sickness presenteeism and sickness absence
In this study, sickness presenteeism due to physical or mental problems was evaluated by two separate questions; ‘Have you worked during the last 6 months even though you had mental problems/problems with the musculoskeletal system?' and 'should have been on sick leave?'
Each question with four possible response options: ‘Not at all’, ‘Sometimes’, ‘Often’, and ‘Always’, as previously used by Ekberg et al. [Citation18]. Responses were combined to form the dichotomous variable ‘Not at all’, which was renamed ‘No presenteeism’. The options ‘Sometimes’, ‘Often’, and ‘Always’ were combined to form the category ‘Presenteeism’.
To evaluate sickness absence resulting from physical or psychosocial problems, we used two separate questions; have you ever been on sick leave during the last 6 months due to a poor psychosocial/physical work environment?, both with five possible response options: ‘No’, ‘Yes, less than a week’, ‘Yes, one to four weeks’, ‘Yes, four weeks to two months’, and ‘Yes, more than two months’. Responses were regrouped for both items to form the dichotomous variables ‘No’ and ‘Yes’ for sickness absence caused by physical and psychosocial workload [Citation18].
Musculoskeletal pain
The presence of pain and symptoms in the neck, shoulders, elbows, wrists/hands, upper back, lower back, one or both hips, one or both knees, and one or both ankles was identified by means of nine items [Citation19]. The possible responses were ‘no pain’ and ‘yes, having pain’. Only OHPs who reported ‘no pain’ are presented in the study.
Work ability
Work ability in this study was evaluated by three questions. The first two (work ability in relation to the physical demands of the job and the mental demands of the job) were measured by five possible response options. They were dichotomised into ‘good’ and ‘poor’ work ability in relation to the physical and mental demands of the job. This measurement is well known and has been used in previous research [Citation17]. The response options of ‘very good’, ‘fairly good’, and ‘reasonably good’ were grouped together as ‘good’, while the options of ‘not so good’ and ‘poor’ were grouped together as ‘poor’. The participants’ own estimation of their work ability during the two-year period was measured by three options. The option ‘hardly’ (poor) remained as one option, while the options ‘maybe’ and ‘yes’ formed the second option (good) [Citation20].
Physical and psychosocial workplace conditions
The questions about physical working conditions were created using the same items used in an exploratory factor analysis in previously conducted studies [Citation3,Citation21]. Physical working conditions were evaluated by six items scored on a scale of 1 = ‘not at all’ to 10 = ‘to a very high degree’. The same item was used to assess precision demands (three items) and work posture (three items). A lower score reflects better physical conditions. All items were dichotomised (1–5 and 6–10). An example of a question is ‘Does your work usually involve many repetitive movements?’
Psychosocial conditions were evaluated by 15 items and grouped into three factors with conceptually related items: high psychosocial demands (six items), poor work control (four items), and poor social support (five items); For example, one question asks: ‘Does your work often demand maximum concentration for considerable periods of time?’ Each item was scored on a scale from 1 = ‘not at all’ to 10 ‘to a great deal’. A higher score reflects poorer psychosocial conditions; Three items evaluated good leadership and were scored on a similar scale, with a lower value indicating good leadership. All items were dichotomised (1–5 and 6–10). For example, one question asks: ‘Does your immediate superior show appreciation when you do a good job?’ Questions about physical and psychosocial conditions were largely adapted from a questionnaire by Ekberg [Citation22] which was theoretically based on the dose response and demand-control working perspective.
The question about perceived sleep quality was scored on a 10-point scale [Citation1–10], with a lower score reflecting better sleep. The factors demand for precision, work posture, psychosocial demands, social support, and items for leadership and perceived sleep were then dichotomised (1–5 and 6–10), with the values 1–5 indicating the positive aspects of exposure at work and presented as percentages.
Perceived exertion at the end of the working day
We evaluated strain in the neck and shoulders, upper and lower back, and left and right upper arm, elbows, wrists, hands/fingers and eyes. An example of one such question is: ‘Over the past month, how much strain would you say your work has put on your neck by the end of a normal working day?’ Each location was scored from 1 = extremely little to 15 = extremely strenuous. All items were combined using the median and this perceived exertion factor was dichotomised on the middle value (1–7 and 8–15). A lower score reflects lower perceived exertion and means that work is not strenuous.
The work experience measurement scale (WEMS)
The Work Experience Measurement Scale (WEMS) was used to evaluate dimensions of workplace health promotion as used in previous studies [Citation23]. WEMS includes 32 statements divided into six dimensions: 1) supportive work conditions, which includes encouragement and support, workplace culture, routine, feedback, job satisfaction, health promotion, advice and help when needed; 2) internal work experience, which includes meaningfulness, development, variation, satisfaction with work content, happiness, and challenges; 3) autonomy, which captures dimensions of how, when, what to do and time control; 4) experience of time, which includes low time pressure, enough time to complete work tasks, and overtime; 5) management, which includes aspects of availability, engagement, fairness, participation in decisions, ability to make decisions, workplace goals and visions; and 6) reorganisation, which covers dialogue, responsiveness, meaningfulness, participation, safety, communication. Each statement is rated on a six-point Likert scale ranging from ‘agree completely’ (score of 1) to ‘disagree completely’ (score of 6), with a range of 32–192. Higher scores indicate a positive work experience. The summed score on the WEMS was dichotomised at the median value for 2012, with scores of 148 or more being positive.
The salutogenic health indicator scale (SHIS)
SHIS includes health indicators with twelve items covering 1) cognitive, 2) physical and 3) psychosomatic dimensions of health. The items are estimated as one index. The SHIS has one overall question: ‘How have you felt in the past 4 weeks? In the last 4 weeks I have…’. The response format has one positive end (healthy) and one negative end (unhealthy), with a range from 1 to 6 for each item. Higher scores indicate better health. Scores are summed to give a range of 12–72. The validity and reliability of the SHIS have been shown to be high [Citation24]. The SHIS score was dichotomised at the median value for 2012. A score of 53 or more was considered good and are presented in percent in the analysis.
Statistics
A power analysis shows that a two-sided chi2 test requires a total sample size of 52 people to find a 25 percent difference at p < 0.05 and an effect size (Cohens’d) of 0.40 with 80 percent power. Descriptive statistics are presented as percent, frequencies (n), and 95% confidence intervals, medians and quartiles (Q1 and Q3). Bootstrapping was used to calculate the 95% confidence interval. Chi-square analysis (the likelihood ratio) was used for comparisons between the three groups in 2012 and in 2014 respectively and McNemar test was used for comparisons within groups over time, from 2012 to 2014. Number of years in the dental service and working hours per week between the three subgroups in 2012 were calculated with Kruskal–Wallis test since none of the variables were normally distributed according to Shapiro Wilk and Kolmogorov Smirnoff tests. The limit for significance for these tests was set at α = .01 due to the large number of tests to reduce the risk of mass significance. The three health subgroups (healthy group, semi-healthy group and unhealthy group) were included as a dependent variable in a multinomial logistic regression analysis for 2012, in which the ‘unhealthy group’ was set as the reference. Eighteen independent variables were included. These were: musculoskeletal pain (5 items), physical and mental work ability (2 items), physical and psychosocial working conditions (4 items), perceived exertion after work (1 item), WEMS and SHIS (2 items), sickness presenteeism (1 item), work satisfaction, leadership and sleep problems (3 items). These items were selected on the basis of an overall assessment of their significant relevance to the aim of the study. The limit for significance was set at α = .05 for the multinomial logistic regression. Data processing was performed using SPSS version 25.
Ethical considerations
The OHPs from each dental clinic were informed about the study by their clinic manager and an information letter was added to the e-mail in conjunction with the link to the web-based questionnaire. Completion of the questionnaire was seen as consent. The ethical rules for research described in the Helsinki Declarations were followed in this study. The study was approved by the Regional Ethical Board, Linköping University, Sweden (Dnr:2012/186-31).
Results
The demographic data for the study population (N = 168) are presented for each of the three health subgroups in : A) the healthy group (n = 66), B) the semi-healthy group (n = 45) and C) the unhealthy group (n = 57). There were no statistically significant differences between the three groups in terms of sex, age, professional category, clinic size, number of years in the dental service or working hours per week.
Table 1. Characteristics of participants (n = 168) in frequencies (n), percentages (%), and 95% confidence intervals (95%CI) and median and Quartiles (Q1, Q3) for each group; (A) Healthy Group, (B) Semi Healthy Group and (C) Unhealthy Group.
Comparisons of work ability, prognosis of staying in work, sleep problems and musculoskeletal symptoms between groups in 2012 and 2014
Work ability and musculoskeletal pain for the three subgroups (healthy group, semi-healthy group and unhealthy group for 2012 and 2014) are shown in . In 2012, the healthy group (n = 66) and the semi-healthy group (n = 45) reported significantly (p < 0.001 and p < 0.01) better physical work ability (59% and 47% respectively) and mental work ability (56% and 64% respectively) than the unhealthy group (n = 57) (19% and 32%). Significantly (p < 0.001) more participants in the healthy group (49%) than in the semi-healthy group (29%) and the unhealthy group (14%) experienced no neck pain during the previous 12 months. Significantly (p < 0.01 and p < 0.001) more participants in the healthy group (59%) than in the semi-healthy group (31%) and the unhealthy group (12%) reported no musculoskeletal symptoms in the shoulder. For wrists and hands there were significantly (p < 0.001) more participants in the healthy group who reported no pain compared with the unhealthy group (37%). Sixty-one percent of the healthy group reported no pain in the lower back, which is significantly more (p < 0.01) than for the semi-healthy group (36%) and the unhealthy group (37%).
In 2014, the prevalence of good work ability in relation to physical demands was significantly higher in the healthy group (n = 66)) than in the semi-healthy group (n = 45) and the unhealthy group (n = 57), with 65%, 31% and 23% for the respective groups (p < 0.001). Good work ability in relation to mental demands was significantly (p < 0.01) higher in the healthy group (58%) than in the unhealthy group (32%). Significantly more participants in the healthy group (63%) and the semi healthy group (38%) reported no neck symptoms compared with the unhealthy group (12%) (p < 0.001 and p < 0.01 respectively). Where shoulder symptoms were concerned, significantly more members of the healthy group (p < 0.001) reported no pain (55%) than the unhealthy group (19%). For wrists, hands, upper and lower back and lower extremities, the healthy group was significantly (p < 0.01 and p < 0.001) more likely to report no pain than the unhealthy group. For lower back pain there was also a significant (p < 0.01) difference between the healthy (61%) and the semi-healthy group (36%). For neck and lower extremities there was also a significant (p < 0.01) difference between the semi-healthy group where 38 percent and 56 percent reports no pain compared with the unhealthy group where 12 percent and 23 percent reported no pain ().
Comparisons for work ability, prognosis of staying in work, sleep problems and musculoskeletal symptoms within groups in 2012 and 2014
There were no statistical differences for reported work ability and musculoskeletal pain when 2012 and 2014 were compared ().
Comparisons between groups in 2012 and 2014 for physical and psychosocial workplace conditions, perceived exertion, leadership, WEMS and SHIS
The results for the three health groups in relation to physical and psychosocial workplace conditions, perceived exertion, leadership, WEMS and SHIS for 2012 and 2014 are shown in .
In 2012, 58% of the healthy group reported low perceived exertion after work, which is a significant difference (p < 0.01) compared with the semi-healthy group (29%) and the unhealthy group (30%). Significantly more OHPs in the healthy and semi-healthy groups reported low psychosocial demands (49% and 42% respectively) compared with the unhealthy group (21%) (p < 0.01). The results for 2014 show that 62% of the healthy group and 58% of the semi-healthy group reported low psychosocial demands, which is significantly higher (p < 0.01) than the 33% reported by the unhealthy group. In the healthy group, 72% reported high SHIS. This is significantly (p < 0.001) higher than the semi-healthy and the unhealthy groups, 29% and 21% respectively.
Comparisons of physical, psychosocial workplace conditions, perceived exertion, leadership, WEMS and SHIS within groups in 2012 and 2014
In 2012, 21% of the healthy group reported good work posture, which is significantly (p < 0.01) more than the 8% reported in 2014. In 2012, 29% of the semi-healthy group reported low perceived exertion after work, which is significantly (p < 0.01) lower than the 58% reported in 2014. In the unhealthy group in year 2012 there was 44% who reported good leadership, which is significantly (p < 0.001) fewer than in 2014 where 75% reported good leadership.
For WEMS, the overall number of participants who reported good scores decreased between 2012 and 2014 in all three groups. In 2012, the percentages for WEMS were 53%, 49% and 40% in the healthy, semi-healthy and unhealthy groups respectively, compared with 15%, 16% and 7% in 2014 (p < 0.001, p < 0.01, p < 0.001). For SHIS, the percentage in the unhealthy group decreased between 2012 and 2014 from 49% to 21% (p < 0.01) ().
Multinomial logistic regression analysis in 2012
The multinomial regression analysis presented in indicates that the likelihood of the healthy group reporting no neck pain was 13.37 times higher (p = 0.001) than the unhealthy group. The semi-healthy group was 6.65 times more likely (p = 0.006) than the unhealthy group () to report no neck pain. The likelihood of reporting low exertion after work was 3.46 times higher (p = 0.04) in the healthy group and 3.88 times higher (p = 0.01) in the semi-healthy group than in the unhealthy group. The likelihood of the healthy group reporting good physical work ability, good SHIS and no sleep problems was respectively 7.99, 11.57 and 12.92 times higher than that of the unhealthy group.
Table 4. Multinomial regression analyses in 2012 for ‘explanatory in variables’ to belonging to the subgroups of Healthy and semi healthy Group.
Discussion
The aim of this prospective study was to analyse the extent to which health and work-related factors influence the ability to stay healthy at work over time. The study, which adopts a salutogenic perspective, contributes to a better understanding of which work- and health-related factors can explain why some Oral Health Providers (OHPs) remain healthy over time, with no reported sickness absence or sickness presenteeism. The main results demonstrated that OHPs who remained healthy reported health-related factors as having good self-reported physical work ability; no neck pain; perceived low exertion at the end of the working day; and not having any sleep problems. Furthermore, those OHPs who remained healthy over time scored significantly higher on health indicators i.e. the Salutogenic Health Indicator Scale (SHIS), than employees in the unhealthy group. In line with our findings, one recent review by Salazar et al. [Citation25] concludes that both personal and work-related factors influence health and wellbeing among dentists. In their study, job resources and wellbeing, job satisfaction, and engagement in their work were reported as factors related to health at work. Our prospective cohort study of OHPs adds new knowledge to what we already know about the salutogenic work perspective.
The SHIS measurement covers cognitive, physical and psychosomatic dimensions of health, which was also a prominent factor for perceived health in the healthy group in 2014. The SHIS could potentially be used to identify and discuss health issues at work, since it has been developed from theories of health and wellbeing. The SHIS has been used in previous research by Ejlertsson et al. [Citation26], who found that recovery, work‒life balance and work experiences were all related to self-rated health as measured by SHIS among primary healthcare employees. In this study, physical factors such as absence of neck pain, low physical exertion during the working day and good physical work ability increased the likelihood of being healthy over the long term. These factors in combination with the restorative benefits of quality sleep may have resulted in better SHIS. Previous research has shown that occupational factors such as high physical and mental workload can interfere with sleep. Conversely, sleep disturbances can negatively influence occupational health and employee safety. Poor sleep is also associated with musculoskeletal disorders. A recent Swedish study found that poor sleep, high amounts of stress, and multi-site pain were associated with reduced work ability in dentists [Citation27].
Previous studies confirm the relationship between employee wellbeing and satisfaction with working conditions [Citation28,Citation29]. In a study by Ljungblad et al. [Citation28], the psychosocial working conditions and health promotion measures in the workplace were analysed in relation to employees’ reported health and sickness absence. They found that employees reported better self-reported health and less sickness absence if they worked in settings where the staff rated the psychosocial working conditions and specific health-promoting measures as good. The relationship between psychosocial work factors and job satisfaction has also been highlighted in a study by Andersen et al. [Citation29] where social support from superiors and colleagues as well as influence at work was most strongly associated with job satisfaction.
The importance for dentists of being able to have influence at work is supported by Ordell et al. [Citation16], who also emphasise the importance of professional development for overall job satisfaction among dentists. Furthermore, in dentistry there are many challenging encounters every day with patients. These have a direct effect on how the work environment is perceived by OHPs [Citation8]. Uncooperative patients contribute to higher perceived stress among OHPs [Citation2]. Interestingly, in our study we found that some health-related factors at work decreased over time. For the healthy group it was work posture and for the semi-healthy group it was higher perceived exertion at the end of the working day. The unhealthy group reported poorer leadership over time as well as a decrease in SHIS. Furthermore, all three groups scored worse for WEMS. The cause of the decrease of these factors over the years was not analysed in this study. However, earlier studies have shown similar results and highlights dental organisational changes, structures and affiliations as possible explanations of negative effects on the work environment [Citation17,Citation30]. Poor management and a lack of supportive working conditions are commonly reported stressors among dentists [Citation25]. From a salutogenic perspective, previous research emphasises the importance of a supportive leadership style for promoting employee health [Citation28]. Ordell et al. [Citation16] showed in their study of Swedish dentists that organisational factors which stress the importance of professional values and perceived influence at work gave higher job satisfaction. These are work related factors which managements should address in order to promote health among OHPs. In a recent paper Jensen et al. [Citation31] shared lessons learnt from a six-year OSH-program, providing occupational health practice guidelines developed in the program by means of a practice-based research network approach. A combination of individual work-oriented interventions and organisational interventions seems to be the key to promoting employee health and preventing and tackling occupational disorders. However, there is a lack of high-quality studies of interventions in dental clinics which focus on a wide range of OHPs.
The current study has a salutogenic approach, i.e. it describes health-promoting factors in the workplace. However, we do also recognise the importance of sickness presenteeism. Every day many OHPs go to work despite being unwell. Previous research has shown that going to work when feeling ill is a known risk factor for future sickness and reduced health. A Swedish study by Gustafsson et al. [Citation32] shows that sickness presenteeism is highest among those with the lowest level of work ability. On the other hand, there are differences in how individuals perceive and cope with stressors in working life [Citation12], i.e. their ability to use internal and/or external resources to promote health, described as the salutogenic concept sense of coherence (SOC) [Citation11]. Some individuals have the ability to deal with demands as challenges rather than as threats. In other words, they have a high level of SOC. Where the employee feels that the resources to cope with work demands are available and also chooses an appropriate coping strategy [Citation12], this may explain not only healthy worker presenteeism but also some sickness presenteeism.
Methodological considerations
Our results give rise to some methodological reflections. A strength of the study is that it is based on a prospective design that is appropriate for studying the dynamics of variables or phenomena over time with the same Oral Health Providers; dentists, dental hygienists and dental nurses. Another strength is the comprehensive number of measures recorded. Access to register data about sickness absence, not only self-reported measures would have been preferable to get a more exact data. The questions on sickness presence and sickness absence have been used in previous research. It is a weakness of this study that the items have not been validated as single items. Moreover, no information about the cause of sickness absence was available, which could be of value for future studies focussing on pathological perspectives, which was not the purpose of this study. However, the results convey a personal view of the questions, which is an important perspective. Another limitation is the dropout rate of 67%. However, it is not uncommon for longitudinal studies to have a large drop-out rate. A review of the databases in 2012 and 2014 seems to indicate random deletion, which reduces the risk of a study sample that is skewed and not representative. However, the group size is fully sufficient for chi2 and McNemar's tests with a power of more than 80 percent.
Practical implications
Previous studies of oral health professionals have largely focussed on health- and work-related problems. These are of course important when considering work adjustments which can prevent occupational injuries. On the basis of our findings, we suggest that future intervention studies should have a salutogenic approach, which looks at how workplace resources may impact employee well-being. Focussing on job resources is also found to lead to work engagement among employees [Citation12]. Also, managers needs to considering that employees have different needs of adjustments at work because of their health status, being healthy or having different mental and/or physical health issues. Work-oriented interventions such as ergonomics, equipment and exercise have been shown to have promising results for health [Citation10,Citation33–35], but was outside the scope of this study. A sustainable working life is also targeted by the Swedish work environment authorities and in collaborations with the EU-OSHA Campaign Healthy Workplaces Lighten the Load. By collaborating, we can tackle work-related disorders and promote a healthy working life for OHPs in dental organisations.
Conclusions
Healthy OHPs, with no sick leave or sickness presence, reported much better salutogenic health (SHIS) and physical work ability, lower perceived exertion at the end of the working day and no sleeping problem than the unhealthy group of OHPs. Some important healthy work related factors (WEMS) decreased over the two years for all groups. Understanding the relationship between working conditions and well-being is crucial to being able to design specific interventions for OHPs which will improve their working conditions and health. We suggest that future intervention studies should focus on how workplace resources influence employee health and well-being.
Acknowledgements
The authors thank all employees who participated in this study.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Rolander B, Wåhlin C, Johnston V, et al. Changes in division of labour and tasks within public dentistry: relationship to employees work demands, health and work ability. Acta Odontol Scand. 2016;74:471–479.
- Moodley R, Naidoo S, Wyk JV. The prevalence of occupational health-related problems in dentistry: a review of the literature. J Occup Health. 2018;60:111–125.
- Rolander B, Jonker D, Winkel J, et al. Working conditions, health and productivity among dentists in Swedish public dental care – a prospective study during a 5-year period of rationalisation. Ergonomics. 2013;56:1376–1386.
- Bozkurt S, Demirsoy N, Gunendi Z. Risk factors associated with work-related musculoskeletal disorders in dentistry. Clin Invest Med. 2016;39:27527.
- Hayes MJ, Smith DR, Cockrell D. An international review of musculoskeletal disorders in the dental hygiene profession. Int Dent J. 2010;60:343–352.
- Wåhlin C, Kvarnström S, Öhrn A, et al. Patient and healthcare worker safety risks and injuries. Learning from incident reporting. Eur J Physiother. 2020;22:44–50.
- Gustafsson CH, Ostberg AL. Experiences from the merger of clinics in the Swedish Public Dental Service – the employee perspective. Open Dent J. 2017;11:503–511.
- Goetz K, Schuldei R, Steinhauser J. Working conditions, job satisfaction and challenging encounters in dentistry: a cross-sectional study. Int Dent J. 2019;69:44–49.
- Singh P, Aulak DS, Mangat SS, Aulak MS. Systematic review: factors contributing to burnout in dentistry. Occup Med. 2016;66:27–31.
- De Sio S, Traversini V, Rinaldo F, et al. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: an umbrella review. PeerJ. 2018;6:e4154.
- Lindstrom B, Eriksson M. Contextualizing salutogenesis and Antonovsky in public health development. Health Promot Int. 2006;21:238–244.
- Jenny GJ, Bauer GF, Vinje HF, et al. The application of salutogenesis to work. In: Mittelmark MB, Sagy S, Eriksson M, et al., editors. The handbook of salutogenesis. Cham: Springer International Publishing; 2017. p. 197–210.
- Lindberg P, Vingard E. Indicators of healthy work environments-a systematic review. Work. 2012;41 Suppl 1:3032–3038.
- Lindmark U, Wagman P, Wahlin C, et al. Workplace health in dental care – a salutogenic approach. Int J Dent Hygiene. 2018;16:103–113.
- Ylipaa V, Arnetz BB, Benko SS, Ryden H. Physical and psychosocial work environments among Swedish dental hygienists: risk indicators for musculoskeletal complaints. Swed Dent J. 1997;21:111–120.
- Ordell S, Söderfeldt B, Hjalmers K, et al. Organization and overall job satisfaction among publicly employed, salaried dentists in Sweden and Denmark. Acta Odontol Scand. 2013;71:1443–1452.
- Rolander B, Lindmark U, Johnston V, et al. Organizational types in relation to exposure at work and sickness – a repeated cross-sectional study within public dentistry. Acta Odontol Scand. 2020;78:132–140.
- Ekberg K, Bjorkqvist B, Malm P, et al. Controlled two year follow up of rehabilitation for disorders in the neck and shoulders. Occup Environ Med. 1994;51:833–838.
- Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237.
- Tuomi K, Ilmarinen J, Jahkola A, et al. Work ability index. 1998.
- Rolander B, Bellner AL. Experience of musculo-skeletal disorders, intensity of pain, and general conditions in work – the case of employees in non-private dental clinics in a county in southern Sweden. Work. 2001;17:65–73.
- Ekberg K. An epidemiologic approach to disorders in the neck and shoulders [Medical Dissertations]. Linköping University; 1994.
- Nilsson P, Andersson HI, Ejlertsson G. The Work Experience Measurement Scale (WEMS): a useful tool in workplace health promotion. Work. 2013;45:379–387.
- Bringsen A, Andersson HI, Ejlertsson G. Development and quality analysis of the Salutogenic Health Indicator Scale (SHIS). Scand J Public Health. 2009;37:13–19.
- Salazar FBC, Sipiyaruk K, White S, et al. Key determinants of health and wellbeing of dentists within the UK: a rapid review of over two decades of research. Br Dent J. 2019;227:127–136.
- Ejlertsson L, Heijbel B, Ejlertsson G, et al. Recovery, work-life balance and work experiences important to self-rated health: a questionnaire study on salutogenic work factors among Swedish primary health care employees. Work. 2018;59:155–163.
- Marklund S, Mienna CS, Wahlström J, et al. Work ability and productivity among dentists: associations with musculoskeletal pain, stress, and sleep. Int Arch Occup Environ Health. 2020;93:271–278.
- Ljungblad C, Granström F, Dellve L, et al. Workplace health promotion and working conditions as determinants of employee health. Int J Workplace Health Manag. 2014;7:89–104.
- Andersen LL, Fishwick D, Robinson E, et al. Job satisfaction is more than a fruit basket, health checks and free exercise: cross-sectional study among 10,000 wage earners. Scand J Public Health. 2017;45:476–484.
- Berthelsen H, Westerlund H, Hakanen JJ, Kristensen TS. It is not just about occupation, but also about where you work. Community Dent Oral Epidemiol. 2017;45:372–379.
- Jensen IB, Björk Brämberg E, Wåhlin C, et al. Promoting evidence-based practice for improved occupational safety and health at workplaces in Sweden. Report on a practice-based research network approach. Int J Environ Res Public Health. 2020;17:5283.
- Gustafsson K, Marklund S, Leineweber C, et al. Presenteeism, psychosocial working conditions and work ability among care workers – a cross-sectional swedish population-based study. Int J Environ Res Public Health. 2020;17:2419.
- Yi Yiu X, Maguire A, Johnson M, et al. A 10-week exercise intervention can improve work posture but not neck/shoulder symptoms in dental health students: a pilot cohort study. WOR. 2020;67:239–249.
- Lindegård A, Nordander C, Jacobsson H, et al. Opting to wear prismatic spectacles was associated with reduced neck pain in dental personnel: a longitudinal cohort study. BMC Musculoskelet Disord. 2016;17:347.
- Letafatkar A, Rabiei P, Alamooti G, et al. Effect of therapeutic exercise routine on pain, disability, posture, and health status in dentists with chronic neck pain: a randomized controlled trial. Int Arch Occup Environ Health. 2020;93:281–290.
