Abstract
Purpose
To test validity and responsiveness of Traffic Light System-BasicADL (TLS-BasicADL).
Method
Validity: Data according to TLS-BasicADL, modified Functional Independence Measure (FIM) and Barthel Index (BI) were collected from 50 patients with mixed medical diagnoses. Responsiveness: 106 patients following hip fracture assessed according to TLS-Basic ADL and modified Katz Index. Percentage change in TLS-BasicADL from pre-fracture status, to post-operatively, discharge and 1 month follow-up was calculated. TLS-BasicADL and modified Katz Index were also correlated at discharge and 1 month. For analysis of responsiveness, Spearman’s rho coefficient (rs) was used and for distribution at item level, percentage change and sign test.
Results
Validity: Strong-excellent correlations between TLS-BasicADL and modified FIM (0.65–0.95), TLS-BasicADL and modified BI (0.77–0.97) for individual items. Analysis of total scores revealed excellent correlations between instruments (0.96–0.98). Responsiveness: Significant differences between assessments for each item of TLS-BasicADL except upper hygiene, dressing and eating. Excellent correlation was found between TLS-BasicADL and modified Katz Index between pre-fracture – discharge (0.897) and moderate-strong (0.597) discharge − 1 month.
Conclusion
TLS-BasicADL is shown to have acceptable concurrent validity for measuring basic mobility and self-care in elderly patients with mixed medical diagnoses and responsive for patients following hip fracture surgery.
Trial registration
Investigation of responsiveness is registered in ClinicalTrials.gov Identifier: NCT03301584 (Retrospectively registered: 4th October 2017).
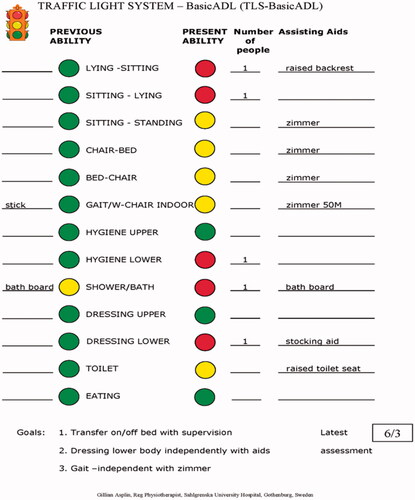
Traffic Light System-BasicADL (TLS-BasicADL) provides a simple assessment scale that highlights level of independence in basic activities of daily living.
TLS-BasicADL gives the multi/inter-disciplinary team a baseline showing the persons previous and present level of function and visual aid for discussing rehabilitation goals and need for future care.
TLS-BasicADL is shown to have acceptable concurrent validity for measuring basic mobility and self-care in elderly patients with mixed medical diagnoses and responsive for patients following hip fracture surgery.
KEYPHRASES
Introduction
The fastest growing population worldwide is that of older adults. Within Europe alone the number of people aged 85 years and older is estimated to increase from 14 to 19 million by 2020 and to 40 million by 2050 [Citation1]. The process of ageing can lead to increased vulnerability to various chronic conditions, functional limitations, disability and comorbidity, which in turn can result in decline in physical, social and psychological well-being and quality of life for the older person [Citation2]. These demographic changes and their consequences put greater demands on healthcare services to accommodate and provide optimal care and rehabilitation services. Multi- or interdisciplinary teams are often used to coordinate these resources around the patient [Citation3–5]. Advantages of structured teams that make use of patient outcome data have shown greater functional gains, improvements in mortality and reductions in costs. [Citation3,Citation4,Citation6].
It is important that the care pathways used to adopt a holistic approach to meet the complex medical, physical, social and psychological needs of the individual. Good communication and transfer of relevant information between services is essential to ensure patients continue to receive optimal care and rehabilitation. One component of this complex process is that of physical function and the ability to perform activities of daily living (ADL) [Citation2].
There is an array of different ADL assessment measures available however as described in a previous article, there is a lack of instruments providing information that can be quickly and easily understood by both team members and patients alike [Citation7].
In response to this, Traffic Light System-BasicADL (TLS-BasicADL) was developed to provide an interdisciplinary, multidimensional construct instrument for assessing and highlighting the older persons previous and present physical function and ADL ability; provide the team and patient with a common language defining the patients’ ADL ability; an instrument to discuss rehabilitation goals with the patient to assist in motivating them in reaching them thereby promoting self-determination and autonomy [Citation7]. A further important aspect is that of safety, TLS-BasicADL highlights level of assistance required for individual activities, and walking aids and assistive devices used to improve safety for the patient and carer.
The instrument is a dynamic document; as the patients’ ability to perform the activities changes, the colour coding markers are changed accordingly. This gives the patient and members of staff an update of level of assistance, aids presently in use and a basis for discussion regarding eventual changes in goal setting. This process follows the popular concept of person-centred care with the aim being for the patient to be well informed and actively participate in decision making regarding their healthcare and rehabilitation. The development and reliability of TLS-BasicADL has been described in an earlier article, with high inter-rater (PA = 86%; ICC = 0.90) and fair intra-rater reliability (PA = 73%) reported by occupational and physiotherapists who assessed 30 patients in an acute geriatric/orthopaedic ward [Citation7].
It is well recognised that in order to confidently interpret the results of assessment measures and outcomes used in clinical practice and research that certain psychometric properties should be fulfilled including reliability, validity and responsiveness [Citation8]. Should this not be the case, results may be inaccurate or biased leading to wrong decisions being made regarding subsequent diagnostic tests and treatments [Citation8,Citation9] ().
Validity
The validityof an instrument is the extent to which a particular use of the instrument and resulting measurement is meaningful and allows inferences to be made about the people under examination. Validity is traditionally established through studies of content, criterion and construct validity [Citation10].
Face and content validation is performed by consensus of an expert panel [Citation8] with face validity referring to whether the items appear, on the surface, to be measuring the construct of interest, and content validity whether the items are relevant and representative of the construct of interest [Citation10]. Criterion validation, believed to be the strongest form of validity [Citation9], is defined as the process of correlating the new instrument in question with another measure of the trait or disorder under study, known as a ‘gold standard’. This can be divided into two types: concurrent and predictive validation. Concurrent validation involves correlating the new instrument with the ‘gold standard’, both of which are given at the same time. Predictive validation on the other hand is concerned with the process of predicting an outcome e.g. diagnostic tests or treatment outcome [Citation10]. Construct validation, defined as the process of evaluating a new instrument where there is no existing instrument measuring that particular construct or there is dissatisfaction with the existing instrument and a need for improvement [Citation10]. The process to establish face and content validity was described in an earlier article [Citation7], hence this study will describe the methods used to examine concurrent validity with other ‘gold standards’ measuring the same construct.
Responsiveness
Responsiveness of an instrument has been defined in various ways e.g. the instruments ability to detect changes over time, the degree to which it can detect a meaningful change [Citation9,Citation11]. As with validity, there is no consensus regarding the methods for measuring responsiveness [Citation10,Citation11]. In circumstances where item for item is being analysed rather than total score, percentage of improvement, deterioration and no change may be studied for the specific instrument and correlated with another instrument measuring the same construct [Citation12].
The aim of this study was twofold: (1) to investigate concurrent validity of the TLS-BasicADL to measure basic transfers, ambulation and P-ADL compared with modified versions of Functional Independence Measure (FIM) [Citation13] and Barthel Index (BI) [Citation14] in patients with varying diagnoses, and (2) to investigate responsiveness of TLS-BasicADL to detect change in basic transfers, ambulation and P-ADL in patients following hip fracture surgery and to compare results with changes in modified Katz Index [Citation15].
Methods
Design and study population
Concurrent validation
A convenient sample of 50 patients admitted to the oncology/geriatric unit at (removed for blinding) during May 2007 and June 2008 with mixed medical diagnoses were included in the study.
Responsiveness
A consecutive series of 106 patients, admitted to the geriatric/orthopaedic unit at (removed for blinding) following hip fracture from September 2013–May 2014 were included. Patients were previously independent in transfers, ambulation and P-ADL with exception of bathing/showering and recorded good intact level of cognition (score 8–10/10) according to Short Portable Mental Status Questionnaire (SPMSQ) [Citation16]. See for demographic characteristics of the study populations.
Table 1. Patient demographic characteristics of the concurrent validity study group (mixed diagnosis) and responsiveness study group (hip fracture).
Trial registration: Analysis of concurrent validation did not involve any clinical intervention, this part is therefore not registered in any clinical trial register. The investigation of the responsiveness of TLS-BasicADL was analysed from data collected in the clinical trial registered in; ClinicalTrials.gov Identifier: NCT03301584 (Retrospectively registered: 4th October 2017).
Methods of assessment
Concurrent validation
The patients were assessed prospectively on one occasion during their hospital admission using 3 different instruments: TLS-BasicADL, modified Functional Independence Measure (FIM) [Citation13] and modified Barthel Index (BI) [Citation14]. FIM and Barthel index were chosen as they are commonly used in research and clinical practice. The assessments were performed by a physiotherapist who had previous experience of using TLS-BasicADL and FIM.
Responsiveness
For analysis of responsiveness data were collected regarding the patients’ ability to perform transfers, ambulate and P-ADL according to TLS-BasicADL for 4 time-periods: retrospectively for pre-fracture status, and prospectively for post-operative, discharge and 1-month follow-up status. Data according to modified Katz Index [Citation15] were also collected for pre-fracture, discharge and 1-month follow-up for the same population. Information regarding pre-fracture status and 1-month follow-up was obtained through interview, with post-operative and discharge status collected through observational assessment. All data were collected by a research group during evaluation of an intervention study of patients following traumatic hip fracture [Citation17]. ADL staircase [Citation18] which is an extension of Katz ADL Index was the instrument chosen by the research group in order to collect data regarding instrumental ADL. ADL staircase comprises a basic ADL section and an instrumental ADL section. Data from the basic ADL section known as Katz ADL index and was used in this present study. Three physiotherapists and two occupational therapists performed the assessments. They had no treatment association with the patients. All therapists received training in both TLS-BasicADL and Katz Index prior to data collection and followed and filled in test protocols for both instruments.
Description of outcome measures
TLS-BasicADL is a 13-item instrument assessing level of independence in basic mobility and self-care activities. Total scores are not used in clinical practice but for the purpose of this validation study we scored all items; 1 (dependent), 2 (supervision) and 3(independent) giving a total score range from 13 (lowest) to 39 (highest) level of independence. [Citation7]
Functional Independence Measure (FIM) is an 18-item performance-based instrument (13 motor, 5 cognition) that are rated on a 7-level ordinal scale [Citation13]. They describe levels of complete dependence (1) to complete independence (7) in performing basic activities of daily living. Total scores range from 18 (lowest) to 126 (highest) level of independence. In this study only motor FIM items were assessed, and the instrument modified by excluding the items: bladder, bowel and stair as these items are not included in TLS-BasicADL. This left at total of 10 items with range 10–70.
Barthel Index (BI) is a 10-item instrument also describing level of independence in basic activities of daily living [Citation14]. Total scores range from 0 (lowest) to 100 (highest) level of independence. Again, the three items; bladder, bowel and stairs were excluded from assessment giving a modified 7-item total score from 0 to 70.
Katz’s index of ADL summarises the persons overall performance in six basic P-ADL functions: hygiene, dressing/undressing, ability to go to toilet, mobility, bowel and bladder control and food intake. Each function is graded as independent, partly independent or dependent. Before calculation of the total score, each item is dichotomised and the degree of dependency is estimated and graded, in a specific hierarchical order [Citation15]. For the purpose of this study we retained the three levels: (1) dependent, (2) partly independent, and (3) independent and modified the index by the removal of the item ‘bowel and bladder control’. This gave a 5-item total score ranging from 5 (total dependence) to 15 (independence) in basic activities of daily living.
A-priori hypotheses about the expected strength and direction of relationships between the measures were not previously defined to avoid introduction of unintended bias into the results [Citation19].
Statistical analysis
For analysis of both concurrent validity and responsiveness, Spearman’s rho coefficient (rs) was used. For concurrent validity, correlation was calculated at both item level and for total scores of TLS-BasicADL, and the modified versions of FIM and BI.
The motor FIM was modified by removing the three items as described above, giving a total of 10 items with range 10–70. The 7-level scoring system was modified to three levels for correlation with TLS-BasicADL: level 1 (1–2), level 2 (3–5) and level 3 (6–7). The BI was also modified giving a 7-item total score from 0 to 70. TLS-BasicADL was for the purpose of the correlation analyses of total scores, given scores 1–3: 1 = dependent, 2 = supervision and 3 = independent giving a score of 13–39. All three instruments were adjusted to give scores out of 100.
For responsiveness, level of ability according to TLS-BasicADL: (1) pre-fracture, (2) post-op, (3) discharge and (4) 1 month follow-up are presented graphically showing the percentage of change between the different time periods in terms of independence, supervision and active help for the individual activities. Sign test has been used to analyse if the percentage of change was significant. Correlation of the differences in scores of TLS-BasicADL and modified Katz Index for the time periods: a) pre-fracture status and discharge and b) discharge and 1-month follow-up were also calculated for each item and for total scores. Katz was modified by excluding bowel and bladder.
Values used to describe the strength of the correlations were 0–0.19 (very weak), 0.20–0.39 (weak), 0.40–0.59 (moderate), 0.60–0.79 (strong) and 0.80–1.0 (excellent) [Citation20]. Analyses were performed with SPSS for Windows (Version 20, SPSS, Inc., Chicago, IL).
Floor and ceiling effects of TLS-BasicADL were considered to be present if more than 15% of the patients scored the lowest or highest possible score [Citation21].
Results
Concurrent validity: TLS-BasicADL, FIM and BI
The results in show strong to excellent correlations between TLS-BasicADL and modified FIM (0.65–0.95), and between TLS-BasicADL and modified BI (0.77–0.97) for individual items. The highest correlation was found between TLS-BasicADL and modified BI, in 7 of the 13 items, in 5 between TLS-BasicADL and modified FIM. A further analysis of total scores revealed excellent correlations between the 3 measurements (0.96–0.98), as shown in .
Table 2. Correlation between individual item scores of Traffic Light System-BasicADL and modified Functional Independence Measure and Barthel Index, respectively.
Table 3. Correlation between total scores of Traffic Light System-BasicADL and modified Functional Independence Measure and Barthel Index, respectively.
Responsiveness
TLS-BasicADL: percentage change in levels of independence, supervision and active help
The graphs in and highlight the distribution and changes in the patients’ ability to transfer and ambulate () and activities of daily living () in TLS-BasicADL. As can be seen in , between 5–10% of patients were independent post-operatively in all transfers and walking, however by discharge approximately 80–85% had regained their ability to transfer in/out of bed and 72% are were walking independently. By 1-month follow-up these figures were up to approximately 95%. All changes between the different assessment time points were significant, p < 0.001.
Figure 2. Distribution of TLS-BasicADL scores. Proportion of patients requiring help, supervision or independent in the individual items of transfers and gait prior to admission, post-op, at discharge and 1-month post-discharge.
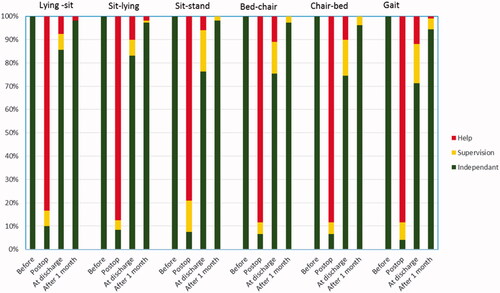
Figure 3. Distribution of TLS-BasicADL scores. Proportion of patients requiring help, supervision or independent in the individual items of ADL prior to admission, post-op, at discharge and 1-month post-discharge.
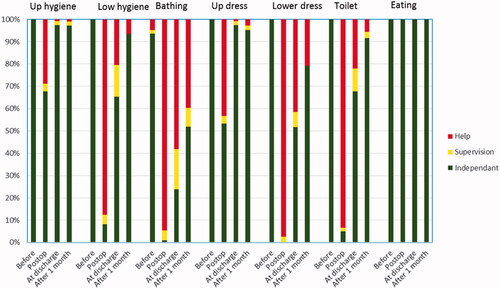
highlights three activities in particular; bathing, dressing lower body and going to the toilet showing that less than 5% of the study group were independent post-operatively. At discharge just over 25% were independent in bathing, 50% in dressing lower body and approximately 65% going to the toilet. By one month approximately 50%, 80% and 90% were independent respectively showing that bathing and dressing lower body are the two activities that patients are least independent in. All changes between the different assessment time points were significant, p < 0.001 except for eating for all time periods, and upper hygiene and dressing between discharge and 1-month follow-up due to higher level of retained upper body function in this patient group.
TLS-BasicADL and modified Katz Index
The correlations of the differences in total scores of TLS-BasicADL and modified Katz Index showed excellent correlation for the period, pre-fracture status and discharge (0.897) and moderate correlation, for discharge to 1-month follow-up (0.597). Correlations at item level varied from very weak in upper body hygiene and dressing for both time periods. Excellent correlation was found for items of lower body dressing and toileting from pre-fracture to discharge. The majority of items showed moderate to strong correlations for both time periods, with slightly better results for the pre-fracture to discharge period (see ).
Table 4. Correlations between differences in scores for modified Katz Index and Traffic Light System-BasicADL at both item level and total scores for time periods; pre-fracture status to discharge and discharge to 1-month follow-up.
Floor and ceiling effects
There was no floor effect reported for any of the assessment time periods. There was however a ceiling effect found at pre-fracture, discharge and 1-month follow up (95%, 23% and 50%, respectively).
Discussion
Scales are used in many ways, however, their suitability depends on whether they have been validated for that particular purpose or not [Citation10]. Nunally [Citation22], also states that it is not the measurement instrument that is validated, but rather the use to which the instrument is put.
Whilst TLS-BasicADL has been used in clinical practice for many years, investigation of the instrument’s psychometric properties are in their infancy. This is the first study investigating the properties of concurrent validity and responsiveness of TLS-BasicADL. The results of this study while reporting TLS-BasicADL to have strong to excellent concurrent validity and responsiveness is limited to the group of inpatients with mixed medical diagnoses and inpatients following hip fracture surgery respectively. Furthermore, with regard to reliability, high inter-rater (PA = 86%; ICC = 0.90) and fair intra-rater reliability (PA = 73%) has previously been reported for patients in an acute geriatric/orthopaedic ward [Citation7].
The three well-established instruments we have used to correlate TLS-BasicADLwith in this study have in contrast been evaluated in different populations and under varying circumstances. Studies concerning BI have reported fair (elderly population) [Citation23] to excellent reliability (acute stroke and neurological rehab population) [Citation24,Citation25], and excellent validity in acute stroke populations when comparing BI and FIM [Citation24,Citation26]. FIM has also shown varying results from poor to excellent inter-and intra-rater reliability and validity in various different populations including elderly adults, spinal cord injuries and stroke [Citation24,Citation27,Citation28]. And for Katz Index, inter-rater reliability has been reported at 0.95 and a coefficient of reproducibility at 0.96–0.99 [Citation15,Citation29,Citation30]. Construct validity has also been studied by correlating scores on Katz Index with Barthel Index in frail elderly (r = 0.78) [Citation31], and stroke, kappa = 0.77 [Citation32].
TLS-BasicADL is used as a clinical instrument to collect information regarding the person’s previous and present ability in basic ADL. Deterioration in ability is a recognised consequence of hip fracture with patients regaining function at varying rates and to varying levels. The population examined in this study of responsiveness was known to have been independent prior to fracture with the aim of treatment to regain previous level of independence. The data were collected from 4 different time periods; pre-fracture, post-operatively, discharge and 1-month follow-up to analyse this anticipated change over time and highlight activities patients were still not fully independent in. To further examine the responsiveness of these changes, data were collected according to the Katz Index another well-recognised instrument, which was for the purpose of the analyses of responsiveness defined of as the gold standard; pre-fracture, discharge and 1 month follow-up. Excellent correlations were recorded for differences in total scores of TLS-BasicADL and modified Katz Index for the period, pre-fracture status and discharge (0.897) and moderate to strong correlation, for discharge to 1 month follow-up (0.597). At item level, correlations varied from very weak to excellent. Items of upper body hygiene and dressing showed to be weak for both time periods, this was due to upper body activities in TLS-BasicADL being assessed separately to lower body activities, whereas in Katz ADL Index they are assessed as one activity. Upper limb function is generally not affected in patients with hip-fracture, a finding which is supported by the results of the sign test analysis which verified a high level of upper body function for all assessment time-points. Excellent correlations were however found for items of lower body dressing and toileting from pre-fracture to discharge. The majority of items showed moderate to strong correlations for both time periods, with slightly better results for the pre-fracture to discharge period. A correlation of ≥0.50 is expected when analysing instruments measuring a similar concept [Citation33], our results may therefore be interpreted as acceptable for the use of TLS-Basic ADL in clinical practice.
While the reliability and validity of an instrument is important when developing a standardised measure, it does not necessarily mean that clinical practitioners will choose to use it in the clinical setting. The overall clinical utility of the instrument is therefore also important to study, this includes aspects such as: appropriateness, accessibility, practicability and acceptability [Citation34]. With regard to these aspects, through studying, reporting and publishing on reliability and validity of TLS-BasicADL the instrument is made more accessible to a wider public. Also, certification is not required and the simplistic format and instruction manual of the instrument is designed for ease of use.
Since investigating TLS-BasicADL for concurrent validity, two further studies investigating clinical utility and patients experiences of using TLS-BasicADL have been performed [Citation17,Citation35]. In the first study investigating early co-ordinated rehabilitation after hip fracture surgery TLS-BasicADL was used as a tool to communicate with the patient previous and present function and ADL status, and as a visual aid for discussing and updating rehabilitation goals [Citation17]. The results of this study showed that patients in the intervention group experienced higher levels of patient participation and reported greater levels of independence in ADL at discharge compared to the control group. A further study has investigated patients experiences of recovery after hip fracture during the acute inpatient phase including the use of TLS-BasicADL [Citation35]. The instrument was described as easy to understand, included appropriate and relevant activities and valued by patients as the protocol highlighted for staff the activities patients required help with.
Strengths and limitations
While the results of this study are promising, it is important to take into consideration that this is the first study to investigate the validity of TLS-BasicADL. A strength of this study is the use of two different rather than a single population, showing it can be utilised not only in the first mixed medical group but also for patients after hip fracture. However, larger sample sizes are to be recommended in future studies to improve generalisability. Secondly, correlations were performed using data from three of the most commonly used instruments; FIM, Barthel Index and Katz Index. The analyses were made at both item level and total score, while total scores for TLS-BasicADL are not used in the clinical setting they were reported in this study in order to give the reader as broad a view as possible. Thirdly, the same assessor was used for the collection of data of concurrent validity with the tests performed and interpreted in a structured manner. There are however some limitations, a-priori hypotheses about the expected strength and direction of relationships between the measures was not defined. This can introduce unintended bias into the results in favour of the instrument. Concerning responsiveness, ceiling effects were found at both discharge (23%) and 1-month follow-up (50%), this is however not unexpected as our study sample comprised a select group previously independent in transfers, ambulation and P-ADL with the exception of bathing. As can be seen in the and the differences between ability post-op and at discharge are considerable. However, had we recruited patients less independent pre-operatively the results would probably have shown greater variance, both at discharge and 1-month follow-up with lower ceiling and higher floor effects. In situations where independence is achieved, addition measures that complement TLS-BasicADL may be used to detect continued progress, for example balance tests or gait speed [Citation36].
It can also be questioned whether TLS-BasicADL is too crude an instrument, with too few levels of grading. This was however one of the main purposes of developing the instrument. That the simplicity of the measure would encourage clinical use in an inpatient setting, with the information collected providing easily understood information, a common language to discuss goals, facilitating team collaboration, and patient participation, self-determination and autonomy. TLS-BasicADL does not claim to provide the full comprehensive picture of the older persons physical, social and psychological well-being and quality of life, but a building block towards understanding the patients’ previous and present functional status and their physical resources in order to plan in-patient rehabilitation and need for future care and rehabilitation services. Measuring over time is of value for both the patient and team. It is important that the patient receives feedback regarding their progress to maintain/promote participation and to feel well-informed regarding future needs and planning. Team members can also through regular evaluations adapt treatments accordingly to suit the needs of the patient and thereby strengthen team collaboration.
Continued research is required to further investigate the validity of TLS-BasicADL. This should include investigating larger and more representative groups of patients, with varying levels of previous function, e.g. following hip fracture, after stroke. Other methods for differentiating between levels of independence and to provide a ‘more diversified and information-rich picture’ is to add the dimensions of degree of difficulty with or without assistive aids, and/or satisfaction when performing an activity [Citation37]. Examples of instruments that have been developed or extended include; ADL staircase that was combined with ‘self-rating of difficulty’ has been studied in community dwelling older adults and Performance and Satisfaction in Activities of daily Living (PS-ADL) developed for patients with RA [Citation38].
As the older adult population increases so do the demands on the healthcare services. An important aim during the limited period of hospital stay is for the patient to regain as high a level of independence in basic ADL as possible prior to discharge, which also has an impact on the need for continued health- and social services.
Conclusion
TLS-BasicADL is shown to have acceptable concurrent validity for measuring basic mobility and self-care in elderly patients with mixed medical diagnoses and responsive for patients following hip fracture surgery. Continued research is required to further investigate reliability, validity, clinical utility and the patient’s perspective in larger more representative patient groups.
Disclosure statement
There is no conflict of interest that may have influenced the professional judgement of the authors.
Additional information
Funding
References
- World Health Organization [Internet]. 2021. Healthy ageing. Available from: http://www.euro.who.int/en/health-topics/Life-stages/.
- Roaldsen KS, Halvarsson A, Sarlija B, et al. Self-reported function and disability in late life – cross-cultural adaptation and validation of the Swedish version of the late-life function and disability instrument. Disabil Rehabil. 2014;36(10):813–817.
- Neuman, et al. Interdisciplinary team working in physical and rehabilitation medicine. J Rehabil Med. 2010;42:4–8.
- Strasser DC, Falconer JA, Herrin JS, et al. Team functioning and patient outcomes in stroke rehabilitation. Arch Phys Med Rehabil. 2005;86(3):403–409.
- Wade DT. Goal planning in stroke rehabilitation: how? Top Stroke Rehabil. 1999;6(2):16–36.
- Cameron ID, Kurrle SE. 1: Rehabilitation and older people. Med J Aust. 2002;177(7):387–391.
- Asplin G, Kjellby-Wendt G, Fagevik Olsen M. TLS-BasicADL: development and reliability of a new assessment scale to measure basic mobility and self-care. Int J Ther Rehabil. 2014;21(9):421–426.
- de Morton NA, Davidson M, Keating JL, et al. Validity, responsiveness and the minimal clinically important difference for the de Morton Mobility Index (DEMMI) in an older acute medical population. BMC Geriatr. 2010;10:72.
- Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19(4):539–549.
- Streiner C, Norman G. 2008. Health Measurement Scales – a practical guide to their developments and use. 4th ed. Oxford: Oxford University Press.
- Guyatt, et al. Methods to explain clinical significance of health status measures. Mayo Clin Proc. 2002;4:728.
- Husted JA, Cook RJ, Farewell VT, et al. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. 2000;53(5):459–468.
- Granger, et al. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil. 1986;1:59–74.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65.
- Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919.
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441.
- Asplin G, Carlsson G, Zidén L, et al. Early coordinated rehabilitation in acute phase after hip fracture – a model for increased patient participation. BMC Geriatr. 2017;17(1):240.
- Sonn U, Asberg KH. Assessment of activities of daily living in the elderly: a study of a population of 76 year olds in Gothenburg, Sweden. Scand J Rehabil Med. 1991;23(4):193–201.
- Wales K, Lannin NA, Clemson L, et al. Measuring functional ability in hospitalized older adults: a validation study. Disabil Rehabil. 2018;40(16):1972–1978.
- Cohen JW. 1988. Statistical power analysis for the behavioural sciences. 2nd ed. Mahwah (NJ): Lawrence Erlbaum Associates Inc.
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
- Nunally JC. 1970. Introduction to psychological measurement. New York: McGraw-Hill.
- Richards SH, Peters TJ, Coast J, et al. Inter-rater reliability of the Barthel ADL index: how does a researcher compare to a nurse? Clin Rehabil. 2000;14(1):72–78.
- Hseuh, et al. Psychometric characteristics of the Barthel activities of daily living index in stroke patients. J Formos Med Assoc. 2001;100(8):526–532.
- Rollnik JD. The early rehabilitation Barthel Index (ERBI). Rehabilitation. 2011;50(06):408–411.
- Wade DT, Hewer RL. Functional abilities after stroke: measurement, natural history and prognosis. J Neurol Neurosurg Psychiatry. 1987;50(2):177–182.
- Pollak N, Rheault W, Stoecker JL, et al. Reliability and validity of the FIM for persons aged 80 years and above from a multilevel continuing care retirement community. Arch Phys Med Rehabil. 1996;77(10):1056–1061.
- Kohler F, Dickson H, Redmond H, et al. Agreement of functional independence measure item scores in patients transferred from one rehabilitation setting to another. Eur J Phys Rehabil Med. 2009;45(4):479–485.
- Spector WD, Takada HA. Characteristics of nursing homes that affect resident outcomes. J Aging Health. 1991;3(4):427–454.
- Brorsson B, Asberg KH. Katz Index of Independence in ADL: reliability and validity in short term care. Scand J Rehabil Med. 1984;16(3):125–132.
- Rockwood K, Stolee P, Fox RA. Use of goal attainment scaling in measuring clinically important change in the frail elderly. J Clin Epidemiol. 1993;46(10):1113–1118.
- Gresham GE, Phillips TF, Labi MLC. ADL status in stroke: relative merits of three standard indices. Arch Phys Med Rehabil. 1980;61:355–358.
- De Vet HCW, Terwee CB, Mokkink LB, et al. Measurement in medicine. Cambridge: Cambridge University Press; 2011.
- Smart A. A multi-dimensional model of clinical utility. Int J Qual Health Care. 2006;18(5):377–382.
- Asplin G, Carlsson G, Fagevik Olsén M, et al. See me, teach me, guide me, but it’s up to me! Patients’ experiences of recovery during the acute phase after hip fracture. Eur J Physiother. 2019;1–9. DOI:10.1080/21679169.2019.1650394
- Wade DT. Measurement in neurological rehabilitation. Curr Opin Neurol Neurosurg. 1992;5(5):682–686.
- Iwarsson S, Horstmann V, Sonn U. Assessment of dependence in daily activities combined with a self-rating of difficulty. J Rehabil Med. 2009;41(3):150–156.
- Archenholtz B, Dellhag B. Validity and reliability of the instrument Performance and Satisfaction in Activities of Daily Living (PS-ADL) and its clinical applicability to adults with rheumatoid arthritis. Scand J Occup Ther. 2008;15(1):13–22.