Introduction
Vasculitis of the urinary bladder is rare and may represent a manifestation of systemic disease. Isolated vasculitis is even rarer, and at presentation may cause a diagnostic dilemma because of its tumor-like appearance [Citation1–4]. This study presents a case of isolated vasculitis of the bladder together with a note on prognosis.
Case report
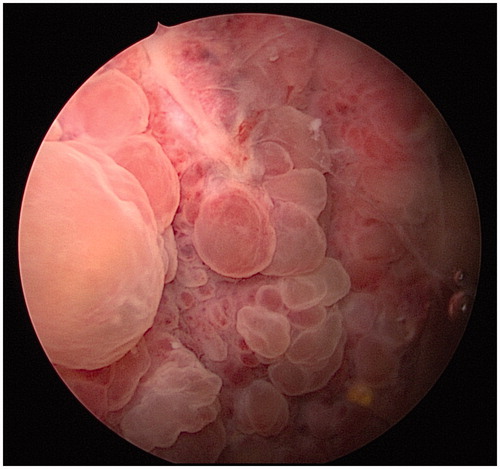
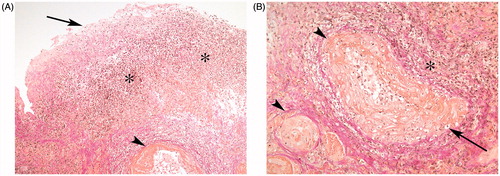
A 45-year-old man, previously healthy except for some anxiety problems, was repeatedly visiting the hospital’s emergency unit because of the sudden onset of macroscopic hematuria and bothersome micturition disturbance, with extreme urinary frequency and pain related to bladder filling. Trials with trimethoprim and ciprofloxacin yielded no relief of symptoms. A computed tomography scan was normal except for a thick-walled urinary bladder, measuring 12 mm, and an irregular bladder mucosa. C-reactive protein (CRP) and urinary cultures were normal. Cystourethroscopy revealed inflammation of the prostatic urethra and a dramatic reaction of the bladder mucosa, which bled easily and also presented a pronounced general edema, involving the ureteral orifices (). The bladder capacity during general anesthesia was found to be markedly reduced, at 110 ml. Biopsies obtained by means of transurethral resection revealed acute cystitis and vasculitis; hemorrhagic, deep, acute and chronic inflammation; and dilated vessels with fibrin degeneration and neutrophils in the walls, indicating an acute vasculitis (). Bladder cytology before the biopsy showed a cell-rich, severely hemorrhagic and moderately inflammatory bladder fluid including urothelial cells with reactive changes but without malignant cell atypia.
Figure 2. (A) Superficial part of the urinary bladder: ulceration with fibrin and inflammatory cells (arrow), chronic inflammation and granulation tissue (star), and dilated vessels with signs of vasculitis (arrowhead). Magnification 100×. (B) Deeper bladder wall: vessels with fibrinoid degeneration and neutrophils as in vasculitis (arrowhead) and chronic inflammation (star). Magnification 200×.
The patient was transferred to the Department of Rheumatology for further investigation. Upon probing his history, no other symptoms or signs indicating rheumatic disease were found. The patient was in good physical shape, and he did not smoke, use drugs or drink alcohol. Anti-nuclear antibodies, extractable nuclear antigen, anti-neutrophil cytoplasmic antibodies and lupus anticoagulant were negative. There were no signs of systemic inflammation, with normal CRP, erythrocyte sedimentation rate and complement levels; and no signs of other organ involvement, with normal creatinine, liver enzymes and blood count. Tests for Chlamydia trachomatis, Mycoplasma genitalium (both using the polymerase chain reaction technique), gonorrhea (with specific culture) and syphilis (in the Venereal Disease Research Laboratory) were all negative. Before the onset of symptoms, the patient had taken no prescribed medicines or herbal drugs.
Treatment with prednisone 30 mg once daily was started, under the working diagnosis of isolated urinary bladder vasculitis. The micturition symptoms decreased and macroscopic hematuria resolved. However, after 1 week the patient had another episode of hematuria and the prednisone dose was increased to 60 mg daily, with a good symptomatic response. Treatment with azathioprine 150 mg daily was started and the patient was discharged with regular follow-up visits to the outpatient clinic. The corticosteroids were tapered during a 3 month period. Azathioprine was maintained for 6 months.
When the patient returned 6 months later, he was free of urinary symptoms. On cystoscopy, the prostatic urethra and bladder mucosa were found to be normal, although the posterior bladder wall exhibited some spots with tiny attachments of fibrin on a pale mucosa, interpreted as healing signs. The patient’s medication was discontinued with no recurrence of symptoms. He was instructed to return to the clinic if he had any bladder symptoms. In spite of repeated health service contacts since then, there has been no contact or re-referral. Five years have passed without any indications of recurrence.
Discussion
The intensity of symptoms was extreme and quite frightening for the patient, who felt that he was about to die. The preliminary diagnosis was that of an extreme acute cystitis of unknown origin, although initially a malignant diagnosis was also contemplated. The biopsy revealed the true nature of his disease and adequate treatment brought the condition to remission. This entity is uncommon but should be kept in mind in cases with sudden onset of intense bladder pain and urgency combined with marked tumor-like, edematous reactions of the bladder mucosa as seen on cystoscopy. The provoking mechanism in this case was not identified. Still, following adequate treatment the prognosis seems to be favorable.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Fischer AH, Wallace VL, Keane TE, et al. Two cases of vasculitis of the urinary bladder: diagnostic and pathogenetic considerations. Arch Pathol Lab Med. 1998;122:903–906.
- Katz DJ, Sengupta S, Snow RM. Isolated vasculitis of the bladder. Urology. 2005;65:797.
- Becker A, Astroza G, Quenzada N, et al. Isolierte Manifestation einer nekrotisierenden Vaskulitis an der Harnblase. Urologe. 2008; 47:1347–1349.
- Kassir R, Mouracade P, Barabino G, et al. Vasculitis of the bladder: an extremely rare case report. Int J Surg Case Rep. 2013;4: 782–784.