Abstract
Objective: To compare preoperative membranous urethral length (MUL) measurements using magnetic resonance imaging (MRI) with two-dimensional transperineal ultrasound imaging (TPUS) in two supine positions on two separate days in men prior to radical prostatectomy.
Materials and methods: MUL was prospectively measured in 18 male volunteers using MRI and on two separate occasions in two different patient positions using TPUS; the patient supine with the knees extended (Supine) and supine with the knees flexed to 70 degrees (Supine KF). Agreement between TPUS and MRI measurements of MUL was assessed using Bland-Altman method comparison techniques and a two-way mixed-effects single measures intraclass correlation (ICC). Test-retest reliability was assessed using a two-way random effects single measures ICC.
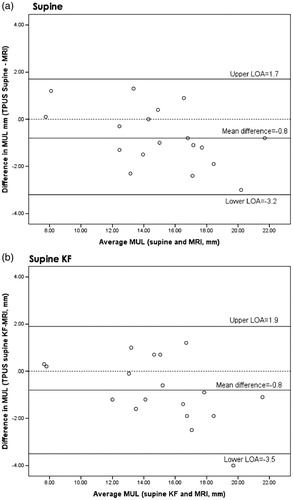
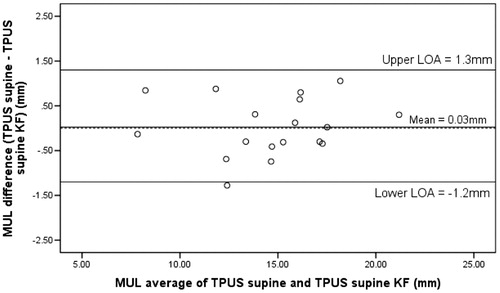
Results: The mean difference in MUL measurements between MRI and i) TPUS Supine was −0.8 mm (95% limits of agreement (LOA): −3.2, 1.7) and ii) TPUS Supine KF was −0.8mm (95% LOA: −3.5, 1.9). ICC indicated a point estimate of excellent agreement between MRI and TPUS Supine ICC 0.93 (95% CI: 0.76, 0.98) and TPUS Supine KF ICC 0.91 (95%CI 0.79, 0.97). There was excellent agreement between TPUS Supine and TPUS Supine KF (ICC 0.98, 95% CI: 0.96, 0.99) with a mean difference of 0.3mm (95% LOA: −1.2 to 1.3mm).
Conclusions: Preoperative MUL can be reliably measured using TPUS and demonstrates excellent agreement with MRI measurements of MUL. TPUS provides clinicians with an accessible non-invasive alternative to MRI for the measurement of MUL that can be used in outpatient urological settings and for patients where MRI is contraindicated.
Introduction
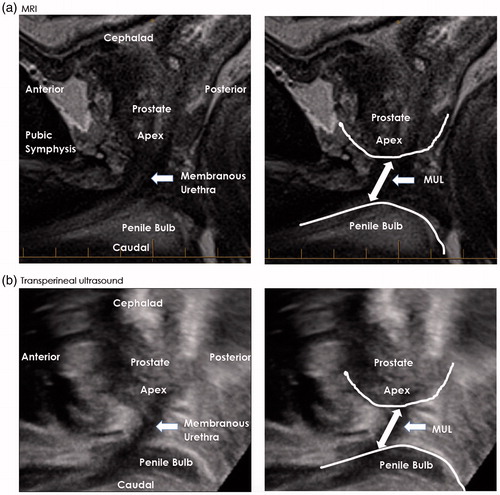
The preoperative length of the membranous urethra (MUL) is a patient-related anatomical factor that affects continence recovery following radical prostatectomy (RP) [Citation1–3]. The measurement of MUL can be undertaken using T2-weighted magnetic resonance imaging (MRI), which is considered the gold standard (). An understanding of MUL can be of value to clinicians and patients to assist with risk stratification prior to surgery, surgical planning and/or when counselling to explain a delay in continence recovery following RP. Acquiring MUL measurements in routine urological clinical practice is often limited to facilities that can refer patients to time- and resource-intensive MRI radiological services. Further, it is not possible to measure MUL routinely when MRI examination is contraindicated. The development of an alternative, non-invasive imaging method that is reliable, clinically accessible, less resource intensive and has good agreement with the gold standard MRI for the measurement of MUL is warranted.
Figure 1. (a) Preoperative T2-weighted midsagittal MRI image and (b) Transperineal ultrasound image for a single patient. Preoperative membranous urethral length (MUL) is measured from the prostatic apex to the point of entry of the membranous urethra at the penile bulb.
Transperineal ultrasound (TPUS) is a well-established non-invasive imaging modality used in outpatient urological clinical practice [Citation4–6], including for the assessment of male pelvic floor muscle function [Citation5–8]. TPUS has the potential to visualise the three anatomical landmarks required for MUL measurement: i) the apex of the prostate, ii) the membranous urethra and iii) the point of entry of the membranous urethra into the penile bulb (BU) [Citation9, Citation10]. While the quality of an ultrasound examination is operator dependent and can be affected by patient habitus, scanning procedures such as TPUS that allow for different patient positions can be advantageous for image optimisation and subsequent analysis. The clinical application of TPUS to reliably measure MUL and determine the level of agreement with MRI measurements of MUL in different supine positions has not been investigated. We undertook a prospective method comparison and reliability study to determine: i) the agreement between MRI and TPUS measurements of MUL in two supine positions, ii) the test-retest reliability of TPUS measurements over two separate days and iii) the agreement between the TPUS measurements of MUL in two positions in male patients prior to RP.
Materials and methods
Patients
Patients referred to an outpatient men’s health physiotherapy clinic for a standardised RP work-up for surgery were invited to participate. A component of the work-up includes routine TPUS assessment of the pelvic floor musculature and the use of TPUS as a patient visual biofeedback tool for the prescription of pelvic floor muscle training programs [Citation7]. Patients who had previously undergone a prostate MRI examination that included T2W sagittal, coronal and axial images for the measurement of MUL were included. Ethical approval was obtained from the Western Sydney Local Health District Human Research Ethics Committee and written informed consent was obtained from patients prior to their participation.
Study design
At the time of the initial consultation, patient characteristics including height, weight, BMI, age, and the preoperative PSA, prostate volume and the Gleason grading group were collected.
2D transperineal ultrasound
TPUS examination was undertaken on two separate days with the patient positioned: i) supine with the knees extended (Supine) and ii) supine with the knees flexed to 70 degrees (Supine KF). The knee flexion angle was confirmed using standard goniometry [Citation11].
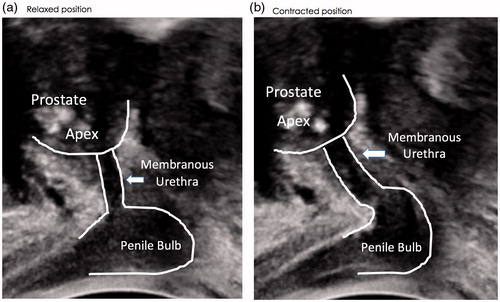
TPUS imaging was performed by a single continence physiotherapist (SFM) with clinical experience in the application of TPUS imaging in men for pelvic floor muscle assessment and training. To standardise bladder filling for image optimisation, patients were first asked to void their bladder and then consume 300mL of water 30 minutes prior to the TPUS examination. The TPUS imaging procedures were undertaken using a Philips iU22 ultrasound machine (Philips Healthcare, Australia), utilizing a grey-scale cine-loop format. A curved array ultrasound transducer (frequency 7.0 MHz) was used to image the pelvis with the transducer aligned on the perineum in the midsagittal plane [Citation8]. Patients were asked to manually lift their scrotum and testes to assist with placement of the transducer on the perineum. A lateral left to right sweep of the transducer was used to ensure that the apex of the prostate, membranous urethra and the BU were all visible (see ). During each ultrasound examination, patients were also asked to perform a voluntary pelvic floor contraction to further assist with the visualisation and identification of the apex of the prostate, membranous urethra and BU (see ). At the completion of the TPUS examination procedures, the cine-loop examination images were exported in the digital imaging and communications in medicine (DICOM) format for subsequent analysis.
Figure 2. Preoperative transperineal ultrasound (TPUS) images for a single patient a) at rest and b) during voluntary pelvic floor muscle contraction. The anterior/superior displacement of the apex of the prostate, dorsal compression of the membranous urethra by the action of the striated urethral sphincter and compression of the penile bulb (BU) during the cine-loop image sequences was used to identify and/or confirm the prostatic apex, membranous urethra and the BU for the measurement of membranous urethral length using TPUS.
Mri
Prior MRI examinations were completed with the patient in the supine position using a Siemens Magnetom 3T Verio system (Siemens, Munich, Germany). Standard sagittal, coronal and axial T2W sequences were used (TR/TE 3650/104ms; slice thickness 3mm; gap 0.6mm and field of view 200mm). The T2W sagittal, axial and coronal MRI images were downloaded and stored for subsequent analysis and comparison with the TPUS examination images for this study.
Image analysis
Standard DICOM viewer software (Intelerad Medical Systems, Canada) was used for all MUL measurements. All TPUS and MRI images were de-identified, coded and placed in a random order prior to analysis. All the defined measurements were checked by two experienced urologists (JSS and MIP) and an experienced radiologist (OA). Training and supervision were given to members of the investigating team (SFM and HL) by two experienced urologists (MIP and LC). SFM and HL performed all measurements blinded to all identifiable patient data, arriving at a single estimate for each measurement by consensus. MUL was measured in the midsagittal plane along the length of the membranous urethra from the apex of the prostate to the point of entry of the membranous urethra into BU [9] (see ). From the single prior MRI examination, measurement of MUL was undertaken on two separate days (one initial, one repeat) using the T2W midsagittal MRI images that were cross referenced with the coronal and axial plane images [Citation12]. MUL was measured three times for each TPUS examination and the mean of the three measures used for analysis.
Statistical analysis
Means and standard deviations (SD) were used to describe continuous variables. The test-retest reliability of MRI and TPUS measurements between day 1 and day 2 was performed using a two-way random effects single measures consistency model intraclass correlation coefficient (ICC) with 95% confidence intervals (CI). The agreement between the day 1 MRI and TPUS measurements of MUL was evaluated using Bland-Altman analysis that included a measure of bias (mean difference between MRI and TPUS measurements) with 95% limits of agreement (LOA) and associated plots [Citation13] and a two-way mixed effects single measures agreement model ICC with 95% CI. When a day 1 TPUS measurement was missing, a day 2 TPUS measurement of MUL was used. Calculated ICC’s were interpreted as: poor <0.5, moderate 0.5 to 0.74, good 0.75 to 0.9 and excellent >0.9 [Citation14]. Statistical analysis was performed using IMB SPSS v24.
Results
A total of 19 patients were referred to the preoperative men’s health physiotherapy clinic during the study period. One patient was excluded because he had not undergone a prior MRI examination due to the presence of an implanted metal device from a previous cardiac surgery. Eighteen patients met the inclusion criteria and consented to participate. Due to impending surgery two patients completed only a single TPUS examination. Sixteen patients completed two separate TPUS examination procedures on separate days. The mean (± SD) number of days between the two TPUS examinations was 8 ± 5 days. Cine-loop TPUS images of two patients in the Supine position and three patients in the Supine KF position on day 1 were excluded due to poor image quality that did not allow the clear identification of one or more of the anatomical landmarks used for the measurement of MUL. Patient characteristics are presented in . There were no musculoskeletal, neurological or cardiovascular comorbidities precluding any of the TPUS testing procedures. There was no history of previous urological surgery, including transurethral resection of the prostate in the entire cohort of patients.
Table 1. Patient characteristics.
MRI test-retest reliability
MRI measurements of MUL that were obtained on separate days using a single MRI examination for each patient (n = 18) were included in the analysis. The point estimate indicated excellent test-retest reliability (0.94) with 95% CI (0.85,0.98) indicating good to excellent reliability.
Agreement between MRI and TPUS measurements of MUL
The Bland-Altman plot is shown in . The mean difference between the MRI and TPUS Supine measurements of MUL was small (mean difference -0.8mm, 95% LOA: −3.2, 1.7) (). Two-way mixed effects ICC indicated a point estimate of excellent agreement (0.93) with 95% CI showing good to excellent agreement (0.76, 0.98). The mean difference between MRI and TPUS Supine KF measurements of MUL was also small (mean difference −0.8mm, 95% LOA: −3.5, 1.9) (), the ICC indicated a point estimate of excellent agreement (0.91, 95% CI: 0.79, 0.97).
Agreement between TPUS supine and TPUS supine KF
Bland-Altman analysis between TPUS Supine and TPUS Supine KF showed a small mean difference of 0.03 mm (95% LOA: −1.2 to 1.3 mm) (). Excellent agreement was observed between the TPUS Supine and TPUS Supine KF (ICC 0.98, 95%CI: 0.96, 0.99).
TPUS test-retest reliability
Supine: The TPUS measurements of MUL in Supine on day 1 (14.6 ± 3.8 mm) and day 2 (14.4 ± 3.8 mm) were similar. The ICC (n = 14) was 0.97 (95% CI; 0.91, 0.99) indicating excellent reliability.
Supine KF: The TPUS measurements of MUL in Supine KF on day 1 (14.2 ± 3.7 mm) and day 2 (13.8 ± 3.6 mm) were similar with ICC (n = 13) showing excellent test-retest reliability (ICC 0.996, 95% CI: 0.988, 0.999).
Discussion
The measurement of MUL in men prior to RP has been identified as an important patient related prognostic risk factor for the recovery of continence following surgery [Citation1, Citation2]. Previously, resource intensive MRI imaging has been the only option available for clinicians to acquire measurements of MUL. To our knowledge, our investigation is first to report excellent agreement and small differences between MRI and TPUS measurements of MUL in two supine patient positions. TPUS measurement of MUL is a reliable, non-invasive alternative that has excellent agreement with MRI for the measurement of MUL in patients prior to RP.
Overall, the characteristics of our patients were typical of men undergoing RP [Citation1]. The TPUS examination procedures were not limited by any patient physical characteristics and the range of MUL measurements for our patients (7.5mm to 21.7mm) are within the range of MRI measurements of MUL that have been previously been reported [Citation1].
The excellent agreement and small differences between the MRI and TPUS measurements of MUL were consistent in both Supine and Supine KF patient positions. Mean difference showed that TPUS measurements of MUL were on average 0.8mm smaller than MRI with most differences smaller than 3mm. We do not consider such differences to be clinically significant. There was also excellent test-retest reliability for TPUS Supine and Supine KF. Our findings are similar to previous investigations that have reported the agreement between MRI and TPUS for the clinical examination of pelvic anatomical structures other than MUL [Citation15, Citation16].
TPUS imaging, while providing less delineation of the anatomical structures of the lower urinary tract compared to MRI, permitted the reliable measurement of MUL. We were able to repeatedly identify the apex of the prostate which was hypoechoic in appearance on the TPUS images due to the fluid filled acinar lumen that comprise the prostatic tissue [Citation17]. The outer aspect of the prostate was clearly delineated on our TPUS images when an interface appeared between the prostatic tissue and the surrounding adipose tissue. The membranous urethra was visualised as a clearly defined hypoechoic structure on all our TPUS images. Due to the highly vascular corpus spongiosum, the BU appeared as a hypoechoic structure on all TPUS images. A lateral sweep of the ultrasound probe assisted our identification of the outer border of the BU where the entry of the membranous urethra into the BU was defined.
Instructing patients to perform a voluntary contraction and relaxation of the pelvic floor musculature during the TPUS examination further assisted with image optimisation for the identification of anatomical landmarks used for the measurement of MUL. The activation of the puborectalis muscle of the levator ani group helped to confirm the position of the apex of the prostate due to the anterior/superior displacement of the prostate in relation to adjacent structures. Contraction of the bulbocavernosus muscle fibres that insert on the dorsal surface of the corpus spongiosum resulted in compression of the outer border of the BU further and assisted the identification of the point of entry of the membranous urethra into the BU [Citation18]. The BU membranous urethral junction was also confirmed with activation of the striated urethral sphincter which resulted in dorsal compression of the membranous urethra towards the medial dorsal raphe [Citation8, Citation18]. The clarity of our TPUS images is consistent with previous TPUS investigations that reported clear visualisation of the structures of the male lower urinary tract when assessing male pelvic floor muscle function [Citation6, Citation8, Citation15].
Although acquiring clear TPUS images is technically challenging, we were able to acquire TPUS images for the entire cohort of patients in at least one supine position for the subsequent measurement of MUL using standard DICOM viewer software. Since ultrasound imaging quality can be affected by operator and patient factors, individual preference may be given by clinicians to select a particular patient positon in supine. Altering the knee flexion angle to change the degree of pelvic tilt may improve contact of the transducer on the perineum and allow for improved image acquisition. The high level of agreement between MRI and TPUS in Supine and Supine KF positions gives clinicians two imaging methods and two TPUS positions for the measurement of MUL. To manage the technical challenges associated with acquiring and interpreting TPUS images for the wider uptake of MUL measurement using TPUS, we recommend interdisciplinary training programs undertaken by experienced clinicians including urologists and continence physiotherapists in high volume centres.
Our investigation has some limitations. Our results are based on eighteen patients, however, the cohort presented with a range of MUL values typical of the range in MUL that have been reported in other studies [Citation1]. All TPUS cine-loop investigations were undertaken by one investigator. The amount of pressure applied to the ultrasound probe when it is placed against the perineum could have influenced our measurement of MUL. However, the excellent agreement of MUL measurements between different days and when compared to MRI would suggest that probe pressure was not a significant factor. Our MUL measurements comprised a single estimate arrived at by two investigators via consensus using previously recorded TPUS images. Future studies could investigate the inter-observer variability in TPUS imaging and inter-observer variability in MUL measurements.
Conclusions
Preoperative MUL is an important prognostic risk factor for continence recovery that can be reliably measured using TPUS with the patient positioned in either supine with the knees extended or supine with the knees flexed to 70 degrees. The excellent agreement between TPUS and MRI measurements of MUL provides clinicians with an accessible non-invasive alternative to MRI, especially when assessing patients in urological outpatient settings and for those patients where MRI examination is contraindicated.
Biographical notes
Our international collaborative interdisciplinary clinical research team includes:
| Abbreviations and acronyms | ||
| BU | = | Penile bulb |
| DICOM | = | Digital imaging and communications in medicine |
| Supine KF | = | Patient positioned in supine with the knees flexed to 70 degrees |
| MRI | = | Magnetic resonance imaging |
| MUL | = | Membranous urethral length |
| RP | = | Radical prostatectomy |
| TPUS | = | Transperineal ultrasound |
Acknowledgements
The authors acknowledge the support and assistance that was received from The Clinical Research Institute, The University of Sydney and EVERX for the maintenance of the ultrasound equipment. Acquisition of the MRI images was provided by Dr Philip Vladica. Advice was received for the preparation of the manuscript from Professor Gregory C. Gass, Physical Therapy Program, University of Jamestown, North Dakota and from C. Skowron and K. Sterns.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
Notes on contributors
Sean F. Mungovan
Sean F. Mungovan: Clinical researcher and physiotherapist from Sydney, Australia, who has a primary clinical and academic interest in the urological assessment and continence management for men prior to and following radical prostatectomy.
Henk B. Luiting
Dr Henk B. Luiting: Urological surgical trainee and PhD clinical research student from The Netherlands who has an interest in the assessment of the urological system and the functional outcomes of men undergoing radical prostatectomy surgery.
Petra L. Graham
Dr Petra L. Graham: Academic and biostatistician at Macquarie University, Sydney, Australia, with expertise in meta-analysis and longitudinal modelling in men’s health applications.
Jaspreet S. Sandhu
Dr Jaspreet S. Sandhu: Urological surgeon at Memorial Sloan-Kettering Cancer Center, New York who has a primary clinical and academic area of interest in the assessment and management of urinary incontinence following radical prostatectomy.
Oguz Akin
Dr Oguz Akin: Radiologist at Memorial Sloan-Kettering Cancer Center, New York who has a primary clinical and academic interest in imaging for cancer assessment and management.
Lewis Chan
Professor Lewis Chan: Functional urological surgeon at the University of Sydney and Concord Hospital, Sydney, Australia, with a subspecialty in urological imaging and the surgical management of urinary incontinence in men following radical prostatectomy. Professor Chan is active in ultrasound training for urologists and physiotherapists internationally.
Manish I. Patel
Professor Manish I. Patel: Urological surgeon at The University of Sydney and Westmead Hospital, Sydney Australia, who has a primary clinical and academic interest in radical prostatectomy surgery.
References
- Mungovan SF, Sandhu JS, Akin O, et al. Preoperative membranous urethral length measurement and continence recovery following radical prostatectomy: A systematic review and meta-analysis. Eur Urol. 2017;71:368–378. doi: 10.1016/j.eururo.2016.06.023.
- Grivas, N, van der Roest R, Schouten Det al. Quantitative assessment of fascia preservation improves the prediction of membranous urethral length and inner levator distance on continence outcome after robot-assisted radical prostatectomy. Neurourol Urodyn. 2017; doi: 10.1002/nau.23318.
- Song W, Kim CK, Park BK, et al. Impact of preoperative and postoperative membranous urethral length measured by 3 Tesla magnetic resonance imaging on urinary continence recovery after robotic-assisted radical prostatectomy. Can Urol Assoc J. 2017;11:E93–E99. doi: 10.5489/cuaj.4035.
- Dietz HP. Pelvic Floor Ultrasound: A Review. Clin Obstet Gynecol. 2017;60:58–81. doi: 10.1097/GRF.0000000000000264.
- Kirschner-Hermanns R, Najjari L, Brehmer B, et al. Two- and three-/four dimensional perineal ultrasonography in men with urinary incontinence after radical prostatectomy. BJU International. 2012;109:46–51. doi: 10.1111/j.1464-410X.2011.10191.x.
- Stafford, RE, van den Hoorn W, Coughlin G, et al. Postprostatectomy incontinence is related to pelvic floor displacements observed with trans-perineal ultrasound imaging. Neurourol Urodyn. 2018;37(2):658–665. doi: 10.1002/nau.23371.
- Stafford RE, Ashton-Miller JA, Constantinou C, et al. Pattern of activation of pelvic floor muscles in men differs with verbal instructions. Neurourol Urodynam. 2016;35:457–463.
- Stafford RE, Ashton-Miller JA, Constantinou CE, et al. Novel insight into the dynamics of male pelvic floor contractions through transperineal ultrasound imaging. J Urol. 2012;188:1224–1230. doi: 10.1016/j.juro.2012.06.028.
- Myers RP, Cahill DR, Devine RM, et al. Anatomy of radical prostatectomy as defined by magnetic resonance imaging. J Urol. 1998;159:2148–2158.
- Coakley FV, Eberhardt S, Kattan MW, et al. Urinary continence after radical retropubic prostatectomy: relationship with membranous urethral length on preoperative endorectal magnetic resonance imaging. J Urol. 2002;168:1032–1035. doi: 10.1097/01.ju.0000025881.75827.a5.
- Milanese S, Gordon S, Buettner P, et al. Reliability and concurrent validity of knee angle measurement: smart phone app versus universal goniometer used by experienced and novice clinicians. Man Ther. 2014;19:569–574. doi: 10.1016/j.math.2014.05.009.
- von Bodman C, Matsushita K, Savage C, et al. Recovery of urinary function after radical prostatectomy: predictors of urinary function on preoperative prostate magnetic resonance imaging. J Urol. 2012;187:945–950. doi: 10.1016/j.juro.2011.10.143.
- Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003;22:85–93. doi: 10.1002/uog.122.
- Portney L, Watkins M. Foundations of Clinical Research: applications to Practice. New Jersey: Prentice Hall; 2000.
- Stafford RE, Ashton-Miller JA, Constantinou CE, et al. A new method to quantify male pelvic floor displacement from 2D transperineal ultrasound images. Urology 2013;81:685–689. doi: 10.1016/j.urology.2012.11.034.
- Maconi G, Tonolini M, Monteleone M, et al. Transperineal perineal ultrasound versus magnetic resonance imaging in the assessment of perianal Crohn‘s disease. Inflamm Bowel Dis. 2013;19:2737–2743. doi: 10.1097/01.MIB.0000436274.95722.e5.
- Greene D, Ali A, Kinsella N, et al. Transrectal ultrasound and prostatic biopsy: Guidelines and recommendations for training. The British Association of Urologic Surgeons 2015. Available from: https://www.baus.org.uk/_userfiles/pages/files/Publications/Transrectal%20Ultrasound%20%20Prostatic%20Biopsy%20FINAL.pdf
- Stafford RE, Coughlin G, Lutton NJ, et al. Validity of estimation of pelvic floor muscle activity from transperineal ultrasound imaging in men. PLoS One. 2015;10:e0144342. doi: 10.1371/journal.pone.0144342.