Abstract
Objective: To evaluate the effect of intrusive thoughts at diagnosis on quality of life, depressed mood and waking up with anxiety up to two years after radical prostatectomy.
Method: The Laparoscopic Prostatectomy Robot Open (LAPPRO) trial was a prospective, longitudinal multicenter study of 4003 patients undergoing radical prostatectomy. Questionnaire data were collected preoperatively, at 3, 12 and 24 months after surgery.
Results: The group of patients with intrusive thoughts at diagnosis had a statistically significant higher postoperative prevalence of impaired quality of life, depressed mood and waking up with anxiety as compared with the group of patients with no or minor intrusive thoughts. The highest risk increase for impaired QoL, depressed mood and waking up with anxiety ≥1/week was at 12, 3 and 3 months, respectively, where the three outcomes increased by 38% (RR: 1.38; 95%CI: 1.27–1.49)), 136% (RR: 2.36; 95%CI: 1.74–3.19)) and 165% (RR: 2.65; 95%CI: 2.22–3.17)), respectively.
Conclusions: The demonstrated link between intrusive thoughts and quality of life, depressed mood and waking up with anxiety deliver is further evidence to the idea that intrusive thoughts has potential as an endpoint for assessing and predicting psychological distress among men with prostate cancer diagnosis.
Trial registration number: ISRCTN06393679 (www.isrctn.com). Date of registration: 07/02/2008. Retrospectively registered.
Introduction
Prostate cancer is the second most frequently diagnosed cancer and the fifth leading cause of cancer death in men worldwide [Citation1]. Established risk factors are age, family history and ethnicity [Citation2]. Facing a diagnosis of a life-threating disease such as prostate cancer is a life-changing trauma which may render a flood of emotions and thoughts that can be difficult to handle for the patient. According to the social-cognitive processing model [Citation3], a traumatic event such as a cancer diagnosis is distressing because it challenges preexisting views of the self and the world [Citation4]. By cognitively processing the trauma, the patient can accept and being able to deal with the diagnosis and thereby reduce the distress. Being able to be emotionally expressive in a supportive social environment is one important part of this process [Citation3,Citation5].
Intrusive thoughts are unintentional recurrent and distressing thoughts about things one does not intend to think about, such as the cancer diagnosis [Citation6]. These thoughts can be seen as part of the acceptance cognitive process as they, in theory, emerge from the patients urge to integrate information associated with the diagnosis into their mental models [Citation3,Citation4]. Intrusive thoughts are from this perspective a sign of an ongoing or incomplete cognitive process and could be seen as a symptom relating to reduced psychological well-being [Citation6].
For successful management of distress it is necessary to assess reasonable structures of the causal relationships between different factors, such as intrusive thoughts and social constrains (barriers to emotional expression) associated with psychological well-being that is to identify the directions of the causal pathways. Whereas a majority of the studies seeking to explore the different associations have been cross-sectional and of moderate size [Citation5,Citation7,Citation8], some have been longitudinal [Citation9,Citation10]. One of these, the Laparoscopic Prostatectomy Robot Open (LAPPRO) trial, involved an in-depth assessment of psychological well-being using questionnaires extensively validated among patients with prostate cancer [Citation10]. In this study, Thorsteinsdottir [Citation6] found associations between intrusive thoughts at diagnosis and Quality of Life (QoL), depressed mood and waking up in the middle of the night with anxiety both at diagnosis as well as three months after radical prostatectomy. The analyses were unadjusted for confounders and were done while patient enrollment was ongoing and therefore only included one-third of the final cohort.
The aim of this study was to evaluate the effect of preoperative intrusive thoughts at diagnosis on quality of life, depressed mood and waking up with anxiety up to two years after radical prostatectomy in an adjusted analysis of the full cohort.
Materials and methods
Laparoscopic Prostatectomy Robot Open (LAPPRO) is an open-label, multi-center, non-randomized prospective longitudinal trial [Citation10] (trial registration number: ISRCTN06393679). Inclusion criteria were ability to read and write Swedish, written informed consent, tumour stage cT1, cT2, or cT3, and no signs of distant metastases. The trial was approved by the regional ethics review board in Gothenburg (277‐07). The study is ongoing with a recent eight-year follow-up. The patients completed paper questionnaires at the time of admission for surgery at the hospital and at home 31,224 months after surgery. The primary objective of the study is to compare two surgical techniques in radical prostatectomy for prostate cancer (open retropubic and robot-assisted laparoscopic) with regard to self-reported urinary incontinence and erectile dysfunction.
Questionnaires
Questionnaires are generally said to be developed within the psychometric and clinimetric frameworks. Psychometrics broadly refers to the measurement of psychological constructs such as personality traits, for example intelligence, and dates back to the nineteenth century [Citation11]. Clinimetrics is a term introduced in the 1980s to define methods for assessing clinical phenomena, such as symptoms [Citation12,Citation13]. Even though there is no clear distinction between the two approaches, they can be broadly viewed as serving different purposes: Whereas psychometrics aims at optimally measuring a single construct such as depression using multiple items, the clinimetric approach seeks to establish items that can characterize various aspects of the construct (attribute) of interest, such as prevalence, intensity and associated distress [Citation14,Citation15]. For conceptual clarity, one symptom at a time is considered, excluding scales in which items are summarized [Citation15]. The questionnaire used in LAPPRO was based on the clinimetric approach.
The questionnaire development was made as follows. Starting with existing questionnaires from similar studies [Citation16], new study-specific questions were developed based on in-depth interviews with patient with prostate cancer, which was followed by contents analysis of what they reported. The questionnaires were subsequently contents validated by clinical experts and validated face-to-face with prostate cancer patients (an investigator accompanied them while completing the questionnaire and assessed their understanding of the items) and tested in a pilot study of 100 men with subsequent revisions, as described by Thorsteinsdottir et al. [Citation10]. The questions on intrusive thoughts, QoL, depressed mood and waking up with anxiety grew out of the work of Thorsteinsdottir, Valdimarsdóttir and Steineck [Citation10,Citation17]. This concept of validation has been used extensively in several studies [Citation18–21] within the Scandinavian Surgical Outcomes Research Group (SSORG).
Variables
Negative intrusive thoughts and the outcome variables QoL, depressed mood and waking up with anxiety were dichotomized in the same way as in previous analyses in the LAPPRO trial [Citation6,Citation22]. Negative intrusive thoughts (hereafter ‘Intrusive thoughts’) were addressed by ‘How often during the past month have you had negative thoughts about your prostate cancer, suddenly and unintentionally?’ The response options were: 1 ‘Never’, 2 ‘More seldom than once a week’, 3 ‘At least once a week’, 4 ‘At least three times a week’, 5 ‘At least once a day’, 6 ‘At least three times a day’ and 7 ‘At least seven times a day’. Responses were dichotomized with less than once per week (categories 1 and 2) as cut-off. ‘How would you describe your quality of life during the past month?’, with response according to a visual analogue scale anchored by 0 meaning ‘No quality of life’ and 6 ‘Best possible quality of life’. Responses were dichotomized with a cut-off point between 4 (0–4: low/moderate) and 5 (5–6: good/very good), where the former indicates an impaired quality of life. Depressed mood was evaluated by ‘Would you call yourself depressed?’, with response options 1 ‘Yes’ and 2 ‘No’. A similar item, ‘Are you depressed?’ has previously been shown to identify patients who are not depressed [Citation19]. Waking up with anxiety was detailed by the question: ‘Have you in the past month woken up in the night with nervousness, anxiety or feeling of discomfort?’ with the response categories: 1 ‘No’, 2 ‘Yes, but more seldom than once a week’, 3 ‘Yes, at least once a week’, 4 ‘Yes, at least three times a week’, 5 ‘Yes, every night’. Responses were dichotomized with less than once per week (categories 1 and 2) as cut-off.
The variables used for adjustment (age at diagnosis, American Society of Anesthesiologists (ASA) classification, alcohol consumption, comorbidity, cohabiting, education, postoperative bother due to urinary or erectile dysfunction and biochemical recurrence) in the adjusted statistical analyses were chosen based on clinical judgement and previous study results [Citation22–24]. Details on all variables are presented in the Supplement Table S1.
Statistical analysis
The prevalence of impaired QoL, depressed mood and waking up with anxiety preoperatively and 3, 12, and 24 months postoperatively was estimated by a marginal binomial model with identity link, intrusive thoughts at diagnosis, time and the interaction (intrusive thoughts *time) as fixed effects. The intra-subjects dependence (i.e. due to subject specific effects on the outcome) was accounted for by using generalized estimating equations (GEE) for parameter estimation with an empirical ‘sandwich’ estimator of the standard errors [Citation25]. Results were presented graphically as prevalence estimates and 95%CI.
The effect of intrusive thoughts on the outcome variables at 3, 12 and 24 months after surgery was evaluated using both unadjusted and adjusted analyses. The adjusted analysis with a binomial distribution encountered convergence problems during the iterative parameter estimation. Therefore the modified Poisson regression approach by Zou [Citation26] was used where intrusive thoughts at diagnosis, time and the interaction and the variables used for adjustment was included as fixed effects. In a marginal model the estimator of the difference intrusive thoughts ≥1/week vs <1/week targets the expected difference in outcomes between the population with ≥1/week and <1/week, respectively. This is in contrast with the random effects model which estimates the corresponding difference conditional on the subject specific effects which enables estimation of individual effects [Citation25,Citation27].
In order to avoid list-wise deletion due to missing values in the variables used for adjustment, multiple imputations with chained equations (MICE) were used to generate 50 data sets with imputed data [Citation28]. Parameter estimates were pooled from the 50 datasets and the effects of intrusive thoughts were presented as risk ratios (RR), 95%CIs and p-values. The SAS procedures GENMOD, MI and MIANALYZE were used for the statistical analyses SAS 9.4 (SAS Institute, Cary, NC) and R package ggplot [Citation29] was used for graphics.
Results
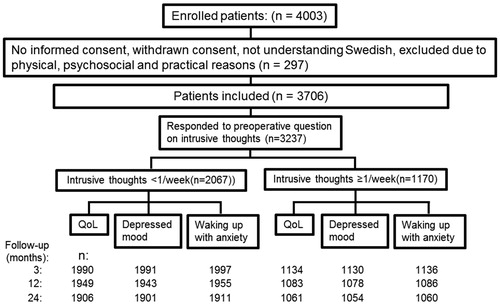
In total, 4003 patients were enrolled in LAPPRO from 1 September 2008 to 7 November 2011 (). For the 3706 eligible patients, the response rate for the question on preoperative intrusive thoughts was 3237 (87%). Response rate for questions related to the outcomes ranged from 90% to 97% (). Patient characteristics are presented in .
Table 1. Patient characteristics.
Preoperatively 1170 (36%) of the patients had intrusive thoughts ≥1/week. Age, civil status, educational level and residence were not significantly different among patients with intrusive thoughts <1/week and ≥1/week. Patients with intrusive thoughts ≥1/week had preoperatively worse QoL (66% vs 35%), had more often depressed mood (15% vs 4%) and waking up with anxiety (47% vs 11%) and lower self-esteem (16% vs 4%). The preoperative bother due to urinary and erectile dysfunction did not differ.
While postoperative QoL and waking up with anxiety improved over time in both groups, depressed mood was stable (). The group of patients with preoperative intrusive thoughts ≥1/week had a statistically significant higher prevalence of impaired QoL, depressed mood and waking up with anxiety ≥1/week as compared with the group of patients with intrusive thoughts <1/week, see . The highest risk increase for impaired QoL, depressed mood and waking up with anxiety ≥1/week was at 12, 3 and 3 months, respectively, where the three outcomes increased 38% (RR: 1.38; 95%CI: 1.27–1.49), 136% (RR: 2.36; 95%CI: 1.74–3.19) and 165% (RR: 2.65; 95%CI: 2.22–3.17), respectively.
Figure 2. Risk (%) with 95% confidence intervals, preoperatively and 3, 12 and 24 months postoperatively.
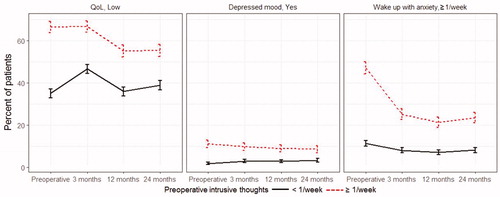
Table 2. Prevalence of endpoints and estimated effect of intrusive thoughts at baseline.
Discussion
In this prospective trial, we evaluated the effect of preoperative intrusive thoughts on quality of life, depressed mood and waking up with anxiety up to two years after radical prostatectomy. The results showed that there is an association between intrusive thoughts and quality of life, depressed mood and waking up with anxiety. Our study strengthened the previously found link between intrusive thoughts and the studied outcomes [Citation6] as we studied a larger cohort, have longer follow-up and addressed causality by adjusted analyses.
From the perspective that intrusive thoughts is a sign of an ongoing or incomplete cognitive processing and could be seen as a symptom relating to anxiety and depressive mood, self-assessed intrusive thoughts could potentially be a surrogate endpoint for use in evaluating interventions aiming for reducing distress. Expressive writing has been suggested as an intervention aimed to promote wellbeing by facilitating emotional and cognitive processes [Citation30]. In a typical writing session, as instructed by the urologist or urology nurse, the patient write about their deepest thoughts and feelings related to the experience of having prostate cancer during approximately 20 min, 3–4 times per week, see [Citation31] and the references therein. The efficiency of expressive writing is however unclear [Citation30,Citation31]. However, as Zachariae and O'Toole [Citation30] put it, due to the feasibility of the intervention, even small treatment effects in subgroups of patients could be clinically relevant. In a report by Siemsen [Citation32], expressive writing was found to moderate the effects of social constraints on intrusive thoughts among patients with prostate cancer, i.e. expressive writing could potentially be effective in a subgroup of patients experiencing constraints on their emotional disclosure. Regardless, the high prevalence indicates there is an unmet need to treat intrusive thoughts: Preoperatively the prevalence was 36% and 20% after 24 months as reported in Bock [Citation22], which is similar to a prevalence of 21% observed in a sample of the Swedish general population [Citation33].
It is, as previously mentioned, important to establish the causal pathways between the different factors associated with psychological well-being. Social constrains has been associated both with distress [Citation34,Citation35] and intrusive thoughts [Citation17,Citation23] and Kollberg et al. [Citation23] and Lepore et al. [Citation34] suggest intrusive thoughts being a mediator between social constraints and psychological well‐being. Whereas suffering from an initial depression may well increase the risk for intrusive thoughts, the proposed pathway appear to involve depressed mood as well [Citation36,Citation37]. Fear of cancer recurrence has also been identified as a risk factor for impaired QoL [Citation38–40]. Thorsteinsdottir et al. [Citation24] identified preoperative uncertainty of cure, alcohol consumption, physical health, antidepressant medication, not being prepared for urinary symptoms, age and physical pain as risk factors for intrusive thoughts. Preoperative levels of alcohol consumption was also found in Bock [Citation22] associated with elevated risk of intrusive thoughts of up to two years after surgery. In an earlier publication of Thorsteinsdottir et al. [Citation6] associations were found between intrusive thoughts at diagnosis and Quality of Life (QoL), depressed mood and waking up in the middle of the night with anxiety both at diagnosis as well as three months after radical prostatectomy.
The marginal statistical model estimates the expected difference in outcome between intrusive thoughts ≥1/week and <1/week on a population level. This is in contrast to the random effects model that can make statements on the difference on a subject level. The choice of model depends on the scientific question raised and have implications on the clinical interpretation. The former model addresses question in line with a public health perspective; how much will the population prevalence of impaired QoL be reduced by a treatment against intrusive thoughts? The latter model answers questions like: what´s the chance of improving a certain patients QoL by reducing his intrusive thoughts? An in-depth methodological discussion is beyond the scope of this article but there is an extensive debate on the pros and cons of the different approaches [Citation41,Citation42].
A limitation is the non-randomized design and lack of data prior to diagnosis. Another limitation is that we cannot fully establish to which extent the causality goes in reverse direction from distress to intrusive thoughts. A third is the that since the study is limited to patients undergoing prostatectomy and patients with more advanced disease were excluded we were not able to account for the relationship between more advanced prostate cancer and and psychiatric illness that has been previously observed [Citation43,Citation44], nor to compare with patients undergoing radiotherapy.
Intrusive thoughts predict quality of life, depressed mood and waking up with anxiety among patients diagnosed with prostate cancer. This strengthens the evidence that intrusive thoughts have potential as an endpoint for assessing psychological distress which is of importance in clinical practice and well as in the design of clinical trials.
Table_S1.docx
Download MS Word (16.1 KB)Acknowledgements
The authors gratefully acknowledge the participants in the LAPPRO trial.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
- Gann PH. Risk factors for prostate cancer. Rev Urol. 2002;4(Suppl. 5):S3–S10.
- Lepore SJ. A social–cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. Washington DC: American Psychological Association; 2001. p. 99–116.
- Horowitz MJ. Stress response syndromes. 2nd edn. Northvale NJ: Aronson; 1986.
- Darabos K, Hoyt MA. Masculine norms about emotionality and social constraints in young and older adult men with cancer. J Behav Med. 2017;40(2):259–270.
- Thorsteinsdottir T, Hedelin M, Stranne J, et al. Intrusive thoughts and quality of life among men with prostate cancer before and three months after surgery. Health Qual Life Out. 2013;Sep 11:11.
- Javaid D, Rubina H, Rehna T. Cognitive processes of cancer patients: a major threat to patients’ quality of life. J Coll Physicians Surg Pak. 2018;28(3):218–221.
- Yanez B, Bustillo N, Antoni M, et al. The importance of perceived stress management skills for patients with prostate cancer in active surveillance. J Behav Med. 2015;38(2):214–223.
- Roberts KJ, Lepore SJ, Helgeson V. Social-cognitive correlates of adjustment to prostate cancer. Psychooncology. 2006;15(3):183–192.
- Thorsteinsdottir T, Stranne J, Carlsson S, et al. LAPPRO: a prospective multicentre comparative study of robot-assisted laparoscopic and retropubic radical prostatectomy for prostate cancer. Scand J Urol Nephrol. 2011;45(2):102–112.
- Bech P. Clinical psychometrics. 1st edn. New York: John Wiley & Sons; 2012.
- Feinstein AR. Clinimetrics. 1st edn. New Haven, CT: Yale University Press; 1987.
- Fava GA, Tomba E, Sonino N. Clinimetrics: the science of clinical measurements. Int J Clin Pract. 2012;66(1):11–15.
- de Vet HCW, Terwee CB, Bouter L-M. Clinimetrics and psychometrics: two sides of the same coin. J Clin Epidemiology. 2003;56(12):1146–1147.
- Steineck G, Bergmark K, Henningsohn L, et al. Symptom documentation in cancer survivors as a basis for therapy modifications. Acta Oncol. 2002;41(3):244–252.
- Johansson E, Steineck G, Holmberg L, et al. Long-term quality-of-life outcomes after radical prostatectomy or watchful waiting: the Scandinavian Prostate Cancer Group-4 randomised trial. Lancet Oncol. 2011;12(9):891–899.
- Agustsdottir S, Kristinsdottir A, Jonsdottir K, et al. The impact of dispositional emotional expressivity and social constraints on distress among prostate cancer patients in Iceland. Br J Health Psychol. 2010;15(1):51–61.
- Ledebo A, Bock D, Prytz M, et al. Urogenital function three years after abdominoperineal excision for rectal cancer. Colorectal Dis. 2018;20(6):O123–134.
- Asplund D, Prytz M, Bock D, et al. Persistent perineal morbidity is common following abdominoperineal excision for rectal cancer. Int J Colorectal Dis. 2015;30(11):1563–1570.
- Bock D, Angenete E, Gonzales E, et al. Assessing health, quality of life and urogenital function in a sample of the Swedish general population: a cross sectional study. BMJ Open. 2018;8(5):e021974–6.
- Walming S, Block M, Bock D, et al. Timely access to care in rectal cancer treatment and the effect on quality of life. Colorectal Dis. 2018;20(2):126–133.
- Bock D, Angenete E, Bjartell A, et al. Habits and self-assessed quality of life, negative intrusive thoughts and depressed mood in patients with prostate cancer: a longitudinal study. Scand J Urol. 2017;51(5):353–359.
- Kollberg KS, Wilderang U, Thorsteinsdottir T, et al. Psychological well-being and private and professional psychosocial support after prostate cancer surgery: a follow-up at 3, 12, and 24 months after surgery. Eur Urol Focus. 2016;2(4):418–425.
- Thorsteinsdottir T, Valdimarsdottir H, Hauksdottir A, et al. Care-related predictors for negative intrusive thoughts after prostate cancer diagnosis-data from the prospective LAPPRO trial. Psychooncology. 2017;26(11):1749–1757.
- Fitzmaurice G, Davidian M, Verbeke G, et al. editors. Longitudinal data analysis. 1st edn. London: Chapman & Hall/CRC; 2008.
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706.
- Molenberghs G, Verbeke G. Meaningful statistical model formulations for repeated measures. Stat Sin. 2004;14:989–1020.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Statist Med. 2011;30(4):377–399.
- Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2018.
- Zachariae R, O'Toole MS. The effect of expressive writing intervention on psychological and physical health outcomes in cancer patients—a systematic review and meta-analysis. Psycho-Oncology. 2015;24(11):1349–1359.
- Kupeli N, Chatzitheodorou G, Troop NA, et al. Expressive writing as a therapeutic intervention for people with advanced disease: a systematic review. BMC Palliat Care. 2019;18(1):1–10.
- Siemsen AS. Expressive writing intervention among newly diagnosed prostate cancer patients: effectiveness on distress and intrusive thoughts and social constraints as a moderator. Reykjavik, Iceland: Reykjavik University; 2018.
- Prytz M, Ledebo A, Angenete E, et al. Association between operative technique and intrusive thoughts on health-related Quality of Life 3 years after APE/ELAPE for rectal cancer: results from a national Swedish cohort with comparison with normative Swedish data. Cancer Med. 2018;7(6):2727–2735.
- Lepore SJ, Helgeson V. Social constraints, intrusive thoughts, and mental health after prostate cancer. J Soc Clin Psychol. 1998;17(1):89–106.
- Zakowski SG, Ramati A, C M, et al. written emotional disclosure buffers the effects of social constraints on distress among cancer patients. Health Psychol. 2004;23(6):555–563.
- Cohee AA, Adams RN, Fife BL, et al. Cognitive Processing in Partners of Long-Term Breast Cancer Survivors. ONF. 2017;44(1):44–51.
- Lepore SJ. Expressive writing moderates the relation between intrusive thoughts and depressive symptoms. J Pers Soc Psychol. 1997;73(5):1030–1037.
- Bellizzi KM, Latini DM, Cowan JE, et al. Fear of recurrence, symptom burden, and health-related quality of life in men with prostate cancer. Urology. 2008;72(6):1269–1273.
- Hart SL, Latini DM, Cowan JE, et al. Fear of recurrence, treatment satisfaction, and quality of life after radical prostatectomy for prostate cancer. Support Care Cancer. 2008;16(2):161–169.
- van de Wal M, Langenberg S, Gielissen M, et al. Fear of cancer recurrence: a significant concern among partners of prostate cancer survivors. Psychooncology. 2017;26(12):2079–2085.
- Lindsey JK, Lambert P. On the appropriateness of marginal models for repeated measurements in clinical trials. Statist Med. 1998;17(4):447–469.
- Lee Y, Nelder JA. Conditional and marginal models: another view. Statist Sci. 2004;19(2):219–238.
- Bill-Axelson A, Garmo H, Lambe M, et al. Suicide risk in men with prostate-specific antigen–detected early prostate cancer: a nationwide population-based cohort study from PCBaSe Sweden. Eur Urol. 2010;57(3):390–395.
- Bill-Axelson A, Garmo H, Nyberg U, et al. Psychiatric treatment in men with prostate cancer – Results from a Nation-wide, population-based cohort study from PCBaSe Sweden. Eur J Cancer. 2011;47(14):2195–2201.