Abstract
Based on a nationwide register data we recently reported a link between male infertility and increased risk of early onset prostate cancer. However, mortality due to prostate cancer, which can be regarded as the ultimate proxy for its clinical significance, especially in the context of over-diagnosis and over-treatment, could not be explored in the previous study, since the follow-up period in most cases was too short. Data therefore must be retrieved from other cohorts, with longer follow-up. We sourced data from a population-based prospective cohort including 11,343 men aged over 45 years, enrolled in the 1970s. The results showed that childless men have higher risk for prostate cancer related mortality (HR: 1.49, 95% CI: 1.09–2.03, p = 0.01) compared to men with children, in particular when only married men, who most probably are involuntary childless, were considered (HR 1.54, 95% CI 1.13 − 2.10, p = 0.006). However, the prostate cancer incidence did not differ (HR = 1.04, 95% CI: 0.88–1.24). In conclusion, our results show that childless men are at higher risk for dying from prostate cancer, probably due to a more aggressive form of the disease.
Keywords:
Introduction
We have recently, in a register based study including more than 1.2 million men who became fathers during the period 1994–2014, found that those with children conceived by assisted reproduction, had 30–60% higher risk of prostate cancer (PCa) as compared to those who achieved fatherhood naturally [Citation1]. The risk was increased for all men requiring assisted reproduction, but most pronounced for men having to use intracytoplasmic sperm injection (ICSI) for fatherhood, which is a technique that is most frequently used for men with severely hampered sperm production, and for whom there is no possibility to become biological fathers by non-assisted means. This risk increase was most obvious for early onset PCa, diagnosed before 55 years of age. Clinically, early onset PCa has for decades, even before the introduction of prostate specific antigen (PSA) testing, been recognized to have poor prognosis. However, because of the, in this context, relatively short follow-up period, the risk for PCa related death, which is a robust marker of the clinical impact of this malignancy, could not be explored in the previous study population. In order to obtain such information, data need to be retrieved from cohorts based on even longer follow-up time than two decades as was the case in the cited study. We therefore used a large community based prospective cohort gathered in the 1970s with the aim to calculate PCa mortality estimates with childlessness as a proxy for severe male infertility.
Subjects and methods
Data was sourced from the population-based prospective Malmo Preventive Project, including 22,444 men (participation rate 71%), between 25 and 63 years of age, enrolled during the period 1974–1984, and followed until 2016. All participants underwent a physical examination at baseline, and laboratory investigations including body mass index (BMI; kg/m2), and blood pressure (mmHg). They also filled in a questionnaire regarding lifestyle factors, as well as family and medical history. By using childlessness as a proxy for severe male infertility, the participants were split into two groups according to fatherhood status at baseline. This information was gathered using two sources: (a) the baseline questionnaire and (b) the Swedish Tax Agency Statistics (STAS), which comprises the number of children of each man, and the personal ID (date of birth) of the men as consecutive numbers. Data was linked to the unique personal identification code assigned to all Swedish citizens. Mismatching information was regarded as conflicting information why such cases were excluded from further analysis as were the ones with missing information in both sources.
Only men older than 45 years (n = 11,343) were included in the analysis in order to reduce misclassification by inclusion of men who were too young to have fathered children at the time of enrolment. Data on incidence and death was sourced from the Swedish Cancer Registry and the Cause of Death Registry, respectively. The study was approved by the Swedish Ethical Review Authority (No. 85/2004).
The risk of having incident PCa was evaluated using multivariate Cox regression and presented as hazard ratios (HR) and corresponding 95% confidence intervals (95%CI) following men from baseline screening until first date of diagnosis of PCa, death from other causes, emigration, or end of follow-up on 31 December 2016. Age at baseline was adjusted for as a continuous co-variate. The analysis was accompanied with Kaplan–Meyer curves. The proportional hazards assumption was upheld for all analyses as assessed using log minus log plots.
Death from PCa was estimated with competing risk regression analysis with age as an underlying time scale using the PHREG procedure in SAS. Death due to other causes was treated as competing risk.
Three adjustment models were used:
Adjusted for smoking, education and marital status, the latter two differing between the childless men and fathers ().
Adjusted for: smoking, education and marital status + BMI and high blood pressure. The reason to include the latter two variables was that BMI and high blood pressure previously have been identified as possible risk factors for developing PCa [Citation2] Data on marital status (never married; married; divorced; widowed), number of cigarettes per day (0, 1–10, 10–20, 30–40, ≥40), and educational level (no education, primary school, secondary school or higher) was derived from the baseline questionnaire. BMI was available from the baseline investigation and was treated as a continuous co-variate. High blood pressure at baseline was defined as systolic pressure above 135 mmHg and/or diastolic pressure higher than 85 mmHg, after 10 minutes’ rest or use of antihypertensive treatment.
Presuming that socially determined childlessness is less frequent among men having a partner as compared to singles, a sub-analysis including only married men was performed, with adjustments for smoking, education, BMI and high blood pressure.
Table 1. Socio-demographic and lifestyle characteristics of childless men, older than 45 years at baseline.
Analyses were performed using SPSS v.25 and SAS 9.4 (SAS University Edition). A p value less than 0.05 was considered significant.
Results
At enrolment, in total, 2134 men (19%) were childless, whereas 9209 (81%) were fathers (). The men were followed for up to 42 years (mean 29.0; SD 10.3). During the follow-up, 1458 men (13%) were diagnosed with PCa and 406 men died from the disease, corresponding to 4% of the total cohort. Mean age at PCa diagnosis was 72.4 (SD 9.9) years for childless men and 71.3 (SD 10.6) for fathers. Mean age of death for the cohort from PCa was 76 (SD 7.4) years.
The risk of dying from PCa was significantly higher in childless men than in men having children (HR: 1.50; 95% CI:1.10–2.04, p = 0.01), with risk estimates remaining almost the same after adjustment for BMI and hypertension (HR: 1.49, 95% CI: 1.09–2.03, p = 0.01; , ). The HR was even higher if only married men were considered (HR: 1.54 (95%CI: 1.13–2.10, p = 0.006). When evaluating all cases, including those non-fatal, there was no difference in the risk of being diagnosed with PCa, neither in model 1 (HR = 1.04, 95% CI: 0.87–1.24, p = 0.66), nor in model 2 (HR = 1.04, 95% CI: 0.88–1.24) or model 3 (HR: 1.01 (95%CI: 0.85–1.19, p = 0.94; ).
Figure 1. Cumulative hazard ratio for prostate cancer mortality (cause-specific model) among fathers and childless men.
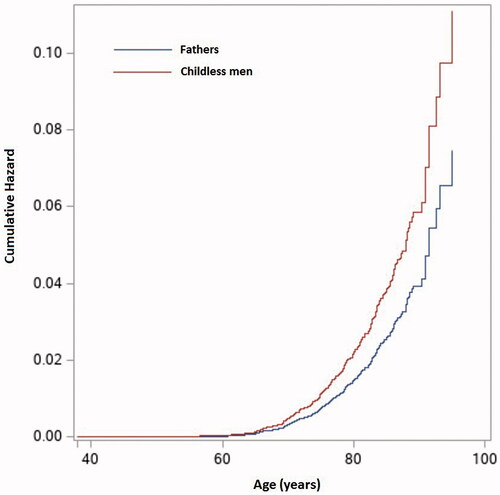
Table 2. Hazard ratios (HR) and 95% confidence interval (CI) for incident prostate cancer (PCa) and PCa mortality among childless men and fathers.
Discussion
Our results show that despite no group difference in PCa incidence, childless men have 50% higher PCa specific mortality compared to those having children. The results remained robust after adjusting for a number of social and metabolic factors as well as for treatment of hypertension, meaning that underlying biological factors probably are operating and resulting via hampered fertility and involuntary childlessness. This is suggesting that childless men have no excess in the risk of developing PCa, but a poorer outcome once being diagnosed with the disease. Presuming this, our results seem to support previous findings indicating a higher risk of developing a more clinically significant disease presenting as early-onset and high risk PCa among infertile men [Citation1,Citation3].
In our analysis, the clinical significance is reflected by the higher PCa mortality rate in childless men, but without any difference in the PCa incidence compared to men who became fathers. A plausible explanation for this discrepancy is that men having a family are more prone to undergo health controls [Citation4]. Regarding PSA testing, these men would consequently be more prone to be diagnosed with indolent, clinically less relevant, good-prognosis PCa. Still, whereas PSA testing has a significant impact on the incidence of new PCa cases, the effect on mortality rates is more marginal [Citation5], and can, therefore, hardly affect the PCa mortality risk being the main outcome of the current study.
A limitation of the current study is that we could not account for the participants´ intention to become fathers, the partners’ fertility status, adopted children, or becoming a father despite low fertility by use of assisted reproduction. However, adoption rates in Sweden were low at the time when the cohort was enrolled, in the late 1970s and early 1980s, and ICSI was rarely implemented before 1992 [Citation6,Citation7] making these unlikely sources of significant bias. In addition, according to a recent register study, 75% of the male cases are most likely involuntarily childless [Citation8]. Another drawback was that the information on marital status did not account for cohabiting, but non-married, couples. However, according to previous research, only 6.5% of all Swedish couples were cohabiting in the mid-1970s [Citation9], meaning that cohabitation is no big source of bias. Furthermore, our sub-analysis restricted only to married men showed even higher mortality estimates for those who were childless. Thus, in the context of using childlessness as proxy for reduced male fertility, the risk of misclassification seems relatively low, can be considered as non-differential, and will bias the result towards the null.
Categorization of the men was based on their fatherhood status at baseline. Some of the men who were childless at baseline became fathers during the follow-up. However, this categorization strategy was kept to avoid so-called ‘immortal time bias’ [Citation10]. Any misclassification because of men who became fathers during the follow-up, but nevertheless being categorized as childless, would however tend to reduce the difference between the groups – not strengthen it – and can, therefore not explain the difference in PCa mortality observed.
Furthermore, the design of the study does not allow concluding if the observed associations are purely due to biological mechanisms linked to infertility or to some degree are a combination of these and socio-economic factors. The latter might have affected the health seeking behaviour resulting in, for example, postponing the contacts with the healthcare system, i.e. the uptake of PSA screening, eventually leading to a more advanced disease stage at time of diagnosis for childless men. Socio-economic factors such as low income and low education level have previously been shown to be associated with higher risk for PCa mortality [Citation11].
In our statistical analysis we adjusted for smoking, education, marital status, BMI and high blood pressure. Some of these factors may have changed during the follow up. However, we found almost identical HRs in adjusted and non-adjusted model, which indicates only minor effects of these co-variates on the final result.
Educational level was adjusted for in our model, but data on income was not available for the present study. The latter, however, is not likely to be a major source of bias since the income often changes positively as men get into relationships [Citation12] and want to become fathers [Citation13]. Consequently, income is dependent on other socioeconomic variables, such as marital status and education – both of which are adjusted for in the analyses.
Conclusion
Childless men may be a high-risk group for developing aggressive and clinically significant PCa. This is an important issue, since there is in general a significant risk of overtreatment of mild, not life-threatening PCa, if extensive PSA testing is offered. Infertility is encountered by 15–20% of all couples. Impairment of male fertility has been reported as predisposing to long-term morbidity and increased risk of aggressive PCa should be considered when discussing preventive measures in this relatively large proportion of men being in contact with health care due to fertility issues.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Al-Jebari Y, Elenkov A, Wirestrand E, et.al. Risk of prostate cancer for men fathering through assisted reproduction: nationwide population based register study. BMJ. 2019;366:l5214.
- Esposito K, Chiodini P, Capuano A, et al. Effect of metabolic syndrome and its components on prostate cancer risk: meta-analysis. J Endocrinol Invest. 2013;36:132–139.
- Walsh TJ, Schembri M, Turek PJ, et al. Increased risk of high-grade prostate cancer among infertile men. Cancer. 2010;116:2140–2147.
- Wirén SM, Drevin LI, Carlsson SV, et al. Fatherhood status and risk of prostate cancer: nationwide, population-based case-control study. Int J Cancer. 2013;133:937–943.
- Heidegger I. PSA screening – a matter of debate? Memo. 2019;12:244–248.
- Official Statistics of Sweden. Statistics – Health and Medical Care Pregnancies, Deliveries and Newborn Infants; The Swedish Medical Birth Register 1973–2014 Assisted Reproduction, treatment 1991–2013. 2015. Article number: 2015-12-27. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2015-12-27.pdf
- Adoptionstatistik. Available from: https://www.adoptionscentrum.se/contentassets/828f585ecc864b219766f8520509fc1c/antal-adoptioner-per-ar.pdf
- Gottvall K, Le. Graviditeter KK. Förlossningar och nyfödda barn. Medicinska födelseregistret 1973–2014 (Medical Birth Register). Assisterad Befruktning 1991–2013. 2015.
- Jan T. Married and unmarried cohabitation: the case of Sweden, with some comparisons. J Marriage Fam. 1975;37:677–682.
- Jones M, Fowler R. Immortal time bias in observational studies of time-to-event outcomes. J Crit Care. 2016;36:195–199.
- Tomic K, Ventimiglia E, Robinson D, et al. Socioeconomic status and diagnosis, treatment, and mortality in men with prostate cancer. Nationwide population-based study. Int J Cancer. 2018;142:2478–2484.
- Regnér H, Isacsson G. Inkomstskillnader mellan par och singlar. Är mönstren desamma för kvinnor och män? 2008. Available from: 4811348-Inkomstskillnader-mellan-par-och-singlar.html
- Chudnovskaya M. Trends in childlessness among highly educated men in Sweden. Eur J Popul. 2019;35:939–958.
