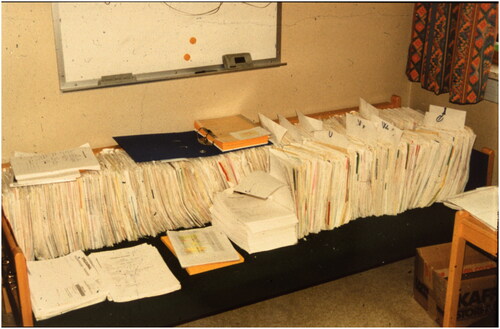
The medical record has during ages served as the main documentation of medical practice and is still mandatory for practicing doctors in most countries. From handwritten notes in a protocol kept by the physician, each patients’ history and documents at some point were filed separately demanding indexes and archives. As medical professions expanded and became more specialized, the medical record contained an increasing range of documents. The growing pile of paper became a challenge, in terms of storage, logistics and extraction of relevant information ().
Figure 1. A part of the data source for the authors’ thesis occupies the couch of the supervisor (Photo ESH).
The introduction of electronic health records (EHR’s) reduced the need for paper dramatically, and all documents could suddenly be accessed by a few clicks on the computer. However, although sorting of documents is easier, the amount of information is expanding exponentially and the need for electronic storage seems endless. Digital pathology and radiology produce an enormous number of bytes, and the current energy crisis in Europe has emphasized that even data servers need electricity. A shortage in available electricity may limit the future expansion of data storage. Further, the overwhelming amount of information is also a huge ordeal for the clinicians, that sometimes “do not see the forest for only trees” [Citation1].
The medical record is not merely a data file but traditionally also a concept of how to document a patient meeting. The patient’s social situation, medical history, allergies and medication, which is continuous as well as changing information, is documented together with the current issue and status. Although the EHR is digital, it still resembles the old paper journal with unstructured entries by every physician with previous medical history endlessly repeated. In this way, the implementation of the EHR, in many institutions, has just been “putting electricity to the paper”. Innovations in informatics are not merely obtained by introducing hardware and software, reshaping content and work processes are equally important parts, and these parts have been neglected.
Medical registries gather – and structure data, often in an SQL-based database, to enable analysis. Unlike text documents, structured data can be presented in graphs and timelines in real-time that make an overview of the medical history easier for the treating physician. In the present issue of the Journal, Charlotte Alverbratt and colleagues have studied time spent and quality of data extraction from the Patient-overview Prostate Cancer (PPC) a decision aid and compared this to time spent when extracting from two conventional EHR’s [Citation2]. As expected, it took less time for clinicians to retrieve key information and with fewer errors when using PPC than using the EHR’s, as previously demonstrated by Hoopes et al. [Citation3]. The study by Alverbratt et al. demonstrates how using data from a decision aid in the clinical setting can ease the clinician’s work and facilitate re-use of the collected data. This demonstrates an untapped potential many years after the introduction of EHR [Citation4].
Nevertheless, PPC as well as the primary registration in The National Prostate Cancer Register (NPCR) of Sweden, like the Norwegian counterpart, are registries based on double data entry, meaning that data is mostly retrieved from the unstructured text in the EHR, and manually entered into a database. After years of experience, most registries are still unable to reuse already entered data in the EHR. The Danish Prostate Cancer Registry and a local Norwegian registry at Innlandet Hospital Trust are two exceptions, converting SNOMED coding or structured digital formulas in the clinical workflow to registry data [Citation5]. This demonstrates the path that further innovations must take in order to reduce workload and streamline management of clinical data, both for documentation in the EHR and for registry use.
As for many oncological conditions, men with prostate cancer often suffer from several medical conditions. Thus, information on prostate cancer treatment is not only of interest for the urologist or oncologist but is also crucial in the generic EHR shared by many specialties and professionals. Therefore, modern applications must be able to integrate disease-specific instruments like the PPC in the patient’s EHR. Recognizing that there are hundreds of medical conditions in need of specific instruments, further innovation must standardize information and be based on branching of these instruments from the main list of diagnoses, medication and procedures in the EHR. There is an urgent need to stop documenting the medical story at each encounter, and replace this with an editable reader-friendly document containing both past events and continuous data. An overview of the medical history should only be a few clicks away, leaving more time for the patient. This calls for collaborations between physicians, documentarists, and database experts in order to reshape EHR. As a prerequisite clinicians must also go from documenting prose to entering more structured data in the workflow. For this to become reality, the content of future EHR’s has to be just as good as their format.
Department of Urology, Vestfold Hospital Trust, Tønsberg, Norway
Norwegian Prostate Cancer Registry, Oslo, Norway
Institute for Cancer Genomics and Informatics, Oslo University Hospital, Oslo, Norway
[email protected]
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Sullivan F, Mitchell E. Has general practitioner computing made a difference to patient care? A systematic review of published reports. BMJ. 1995;311(7009):848–852.
- Alverbratt C, Vikman H, Hjälm Eriksson M, et al. Time difference in retrieving clinical information in patient-overview prostate cancer compared to electronic health records. Scand J Urol. 2022;2:1–7.
- Hoopes M, Voss R, Angier H, et al. Assessing cancer history accuracy in primary care electronic health records through cancer registry linkage. J Natl Cancer Inst. 2021;113(7):924–932.
- Bettencourt-Silva JH, Clark J, Cooper CS, et al. Building data-driven pathways from routinely collected hospital data: a case study on prostate cancer. JMIR Med Inform. 2015;3(3):e26.
- Helgstrand JT, Klemann N, Røder MA, et al. Danish prostate cancer registry – methodology and early results from a novel national database. Clin Epidemiol. 2016;8:351–360.
