Abstract
Objectives
A nationwide population-based register study will evaluate the risk of postoperative inguinal hernia repair after primary curative-intent treatment of prostate carcinoma (PCa).
Background
Several previous studies have suggested an increased risk of inguinal hernia repair after prostatectomy. Only a few studies have compared the risk by PCa treatment modalities.
Methods
Data were collected between the years 1998 and 2016 from the national hospital discharge database HILMO and between the years 1998 and 2015 from the Finnish cancer registry to identify all men with prostate cancer with data on primary treatment available and information on inguinal hernia diagnoses and procedures among them. The risk of inguinal hernia repair among men managed with prostatectomy was compared to those treated with radiation therapy. Participants treated with prostatectomy were analyzed as a whole and separately stratified into subgroups managed with mini-invasive or open surgery. Multivariate Cox regression with adjustment for age and comorbidities was used for analysis.
Results
A total of 7207 cases of PCa were included in the study. 4595 men were treated with radical prostatectomy and 2612 with radiation therapy. Overall, the risk of hernia repair was higher among men treated with prostatectomy compared to men who received radiation therapy as the primary PCa treatment (HR 1.42, 95% CI 1.14–1.77). The risk did not differ markedly by the prostatectomy method.
Conclusion
Prostate cancer treatment with prostatectomy is associated with an increased risk of inguinal hernia surgery than external beam radiation therapy treatment. This risk should be taken into account when planning PCa treatment.
Background
Prostate carcinoma (PCa) is the most common cancer among men [Citation1]. Radical prostatectomy and external beam radiation therapy (EBRT) are the most common curative treatment options in localized PCa. Several previous studies have reported a high risk of developing inguinal hernia after prostatectomy [Citation2–5]. The method of prostatectomy may matter. The risk appears to be connected to open prostatectomy, probably due to damage to anatomical structures supporting the inguinal region during surgery [Citation6–10]. In minimally invasive surgery, the surgeon has a better view of the operation area in an open procedure, thus potentially better can preserve supporting structures of the inguinal region [Citation11].
Standard prostatectomy involves cutting vas deferens, and it has been proposed that sequentially retracting vas may pull the peritoneum towards the inguinal canal and facilitate hernia formation [Citation12]. Techniques like spermatic cord isolation have been proposed to avoid this. However, separation of the peritoneum from elements of the spermatic cord is not currently standard procedure in any prostatectomy technique.
In contrast, inguinal structures are not damaged in EBRT, which presumably would lead to a lower risk of inguinal hernias after treatment. So far, two studies comparing hernia incidence after prostatectomy and radiation therapy have been published [Citation13,Citation14]. These extensive population-based studies reported a two-fold risk increase for inguinal hernia after radical prostatectomy compared to those treated with EBRT. The finding was confirmed in a meta-analysis [Citation15].
Inguinal hernia is a clinically significant condition as it causes pain and discomfort. Inguinal hernias also have a slight possibility of intestinal strangulation, especially in the elderly age group. Treatment of symptomatic inguinal hernia is a repair with mesh to reinforce the inguinal canal. The operation may have serious adverse effects as up to 20% of inguinal hernia patients develop chronic pain post-operatively, which severely impairs quality of life in 1–2% of cases [Citation16].
To evaluate the incidence of inguinal hernia repair after prostate cancer treatment, we performed a nationwide population-based registry study comparing the risk of surgical hernia repair after open and laparoscopic prostatectomy or EBRT for prostate cancer. We hypothesize that surgically managed PCa patients have a higher risk of undergoing hernia repair than EBRT-treated patients. Further, we hypothesize that mini-invasive laparoscopic surgery is associated with a lower risk of subsequent hernia repair than open procedures.
Material and methods
Study cohort
The study cohort was formed by linking information from two national registries; the national hospital discharge registry HILMO and Finnish Cancer Registry (FCR). The administrator, the National Research and Development Centre for Welfare and Health, permitted the registries.
HILMO database contains registered information on diagnoses (as ICD-10 codes) and medical procedures (coded according to Nordic Classification of Surgical Procedures) along with dates of treatment from all in- and outpatient hospital visits. Reporting is mandatory for all Finnish health care units, both private and public. HILMO information is used for planning and management of the Finnish healthcare system by the national authority. For the present study, all inguinal hernia repairs among men during the years 1998–2016 in Finland were identified from HILMO. The information started in 1998 when the ICD-10 coding system was adopted. At the time of data collection, 2016 was the last year with complete data available. Information in HILMO and cancer registry is completed annually, so available information lags one to two years behind the date when data is obtained. The procedures were identified using Nordic Classification of Surgical Procedures (NOMESCO) codes for the search (Supplementary Table 1). Additionally, further inguinal hernia cases were identified based on ICD-10 codes K40 and K41. A total of 193,378 men with a record of inguinal hernia operation were collected from the HILMO database. Additionally, we obtained information on comorbid conditions atrial fibrillation (I48), chronic obstructive pulmonary disease (J44), asthma (J45), kidney insufficiency (N18), diabetes (E10-E14), sleep apnea (G47.3), heart condition (I20-I21, I25, I34-I37, I42.0, I42.9, I50), stroke acute or post (I63 and I69), deteriorating brain disease (F00-F03, G30, G20), liver disease (K70-K76) and other cancers besides prostate cancer (Supplementary Table 2). These conditions were chosen as they are involved in the Charlson comorbidity index commonly used as a measure of comorbidity, thus affecting subjects' ability to tolerate surgical or oncological treatment [Citation17].
Finnish Cancer Registry was used to obtain information on 11,699 prostate cancer cases diagnosed in Finland during 1998–2015. FCR covers information on 99% of cancer diagnoses made in Finland [Citation18]. The data also included information on the date of diagnosis, tumor extent at diagnosis, primary treatment, and date of death. Information on prostate cancer management was supplemented by searching the HILMO database for codes indicating external beam radiation therapy (KE002, KE009, WF002, WF099), open prostatectomy (KEC00), or laparoscopic prostatectomy (KEC01). Additional procedure code ZXC96 indicated robot-assisted surgery.
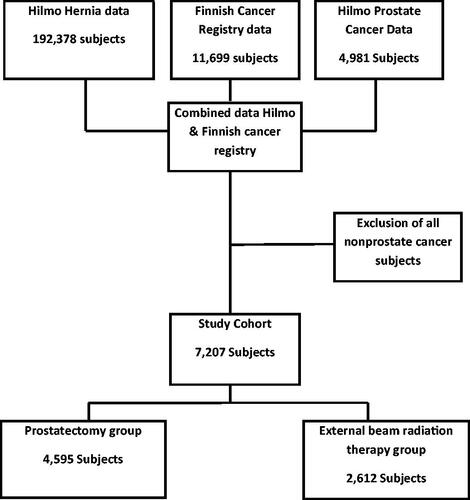
The information from the registries was linked based on a unique personal social security number that is given to all Finnish residents. After combining data from both registries and limiting to men with sufficient data to calculate follow-up time after diagnosis, we had 4595 men with prostate cancer primarily managed with prostatectomy and 2612 with external beam radiation therapy ().
Figure 1. Flowchart of the study. The study population is 7207 Finnish men diagnosed with prostate cancer during 1998–2016.
Using HILMO data, we could determine if hernia repair was done before or after prostate carcinoma treatment. The total size of the prostatectomy group was 4595 men; of these, 2268 men had information available on prostatectomy techniques.
Data analysis
Distribution differences in baseline characteristics were compared by primary PCa treatment method using the chi-square test (categorized variables) or Mann–Whitney U test (continuous variables).
We used Cox regression to calculate hazard ratios (HRs), 95% CIs, and Kaplan–Meier curves for the overall risk of hernia surgery after PCa treatment with months since PCa diagnosis as the time metric. Endpoints for follow-up were the date of first hernia surgery, death, or 31 December 2015, whichever came first. The Cox regression model was adjusted for age and all above-listed comorbidities. Each comorbid condition was classified as a dichotomous variable (ever/never).
Participants with EBRT as the primary PCa treatment were used as the reference group in all analyses. Participants treated with prostatectomy were analyzed together in the primary analysis regardless of the surgical technique. Subgroup analyses were stratified by the surgery method: open or minimally invasive. The latter group was further stratified into robot-assisted laparoscopic prostatectomy and conventional laparoscopic prostatectomy subgroups.
In sensitivity analyses, two methods analyzed the effect of the previous hernia; first, we limited the study population to men with no previous inguinal hernia operation before PCa diagnosis. Additionally, another analysis further adjusted the Cox regression model for previous hernia repair.
Statistical Package for Social Science for Windows, version 26.0 (SPSS), was used for all statistical analyses. p-Value < 0.05 was set for statistical significance.
Results
Population characteristics
Compared to men treated with EBRT, men in the prostatectomy group were younger; the median age at diagnosis was 65 (IQR 60–70) vs. 70 (IQR 65–75) in the prostatectomy group and EBRT group, respectively (). After treatment, 25.5% of men treated with prostatectomy and 3.9% of men treated with EBRT underwent hernia repair. We had exact surgical technique information for 2268 subjects; 1796 men underwent open and 467 minimally invasive procedures. Those treated with robot-assisted prostatectomy, a total of 405, were included in the latter subgroup. Other 2327 were considered as having undergone prostatectomy of a non-specified technique.
Table 1. Population characteristics.
Comorbidities were rare regardless of the primary PCa treatment method. Prevalence distribution of comorbidities was similar in both groups, except for diabetes which was slightly more common in the prostatectomy group vs. EBRT group (1.9% vs. 0.8%, respectively) (). In the prostatectomy group, the extent of PCa was more often local or locally advanced than in the EBRT group (). However, the proportion of men with unknown or missing information on tumor extent was higher in the EBRT group. The proportion of metastatic cancer was similar in both groups.
In the prostatectomy group, 1172 (25.5%) men underwent subsequent hernia repair. The majority (95.6%) were done using the open method. Only 73 (6.9%) procedures were laparoscopic. In the ERBT group, 103 (3.9%) men had a hernia repair. The repair type distribution was similar to the other group; 94 (91.3%) were open, and 11 (10.7%) were laparoscopic repairs. A few subjects in both groups have had both open and laparoscopic repair due to recurrent hernias.
Risk of inguinal hernia repair by prostate cancer treatment method
In general, the risk of inguinal hernia repair after any form of prostatectomy was higher compared to the EBRT group even after adjustment for comorbidities (multivariable-adjusted HR 1.42, 95% CI 1.14–1.77) (; ).
Figure 2. Survival curves for inguinal hernia repair-free time after prostate cancer primary treatment by the method. It is calculated with Cox regression adjusted for age.
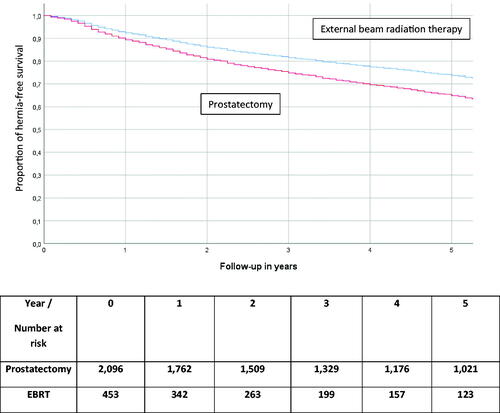
Table 2. Risk of undergoing inguinal hernia repair after prostate cancer treatment, by primary treatment type.
When stratifying the analysis by prostatectomy techniques, the risk association was similar regardless of the surgical technique.
The risk of a femoral hernia could not be evaluated separately as the study population included only ten men with femoral hernia repair after PCa treatment.
Sensitivity analyses
When the analysis was limited to 1216 men (1077 and 139 men treated with surgery and ERBT, respectively) with no record of inguinal hernia repair before PCa diagnosis, the risk increase in the prostatectomy group was reversed; HR 0.62 CI 95% 0.50–0.78 compared to the EBRT group (). That is, prostatectomy was associated with a lower risk of hernia repair than EBRT.
Table 3. Effect of previous inguinal hernia operation on the risk of undergoing inguinal hernia repair after prostatectomy.
1656 men had a history of inguinal hernia before Pca diagnosis. 1120 and 536 men were treated with surgery and EBRT, respectively. Notably, all 297 men in this subgroup who had an inguinal hernia repair after PCa treatment were primarily treated with surgery.
When the primary analysis was further adjusted for the previous hernia, the risk increase was mitigated HR 1.10 CL 95% (0.88–1.38), confirming that the history of hernia repairs was a significant predictive factor for further hernia operations ().
Discussion
Our study on register-based real-life data confirms that men with localized PCa treated with prostatectomy have an elevated risk of subsequent surgical inguinal hernia repair compared to those treated with EBRT. The risk association does not seem to depend on the surgical technique. However, an increased risk was limited to men with inguinal hernia repair before PCa diagnosis in the sensitivity analysis. This increased risk suggests that PCa surgery may predispose men with previously weakened inguinal canal structures to new hernias but may not adversely affect those with no previous evidence of an inguinal hernia.
Several previous studies have shown a similar risk increase among men undergoing radical prostatectomy. All studies have been large population-based series. A Swedish study compared inguinal hernia risk between subjects after radical prostatectomy and controls and subjects who received EBRT. They had a large population of over 9000 EBRT subjects and over 19,000 prostatectomy subjects. The risk of inguinal hernia was over 1,5-fold when comparing the prostatectomy group to EBRT [Citation13]. The Canadian study group has published two studies. The first compares inguinal hernia risk among different urological procedures, and the second compares radical prostatectomy and EBRT. The highest risk was associated with radical prostatectomy in both studies, nearly two-fold compared to EBRT [Citation14]. A recent meta-analysis came to a similar conclusion. The highest risk was associated to open prostatectomy followed by mini-invasive techniques [Citation19].
Several studies have contemplated how prostatectomy may cause inguinal hernia [Citation20]. Open proceccus vaginalis during the operation is suggested as one reason [Citation21]. It is known that patent processus vaginalis predisposes to inguinal hernias, so men with that may be especially prone to developing an inguinal hernia after prostatectomy. Concordantly, in subgroup analyses, the risk increase was observed only in men with previous hernia diagnoses, underlining the role of predisposing anatomical factors in the risk association.
Future studies on prophylactic mesh placement during prostatectomy should probably focus on men with previous hernias or open processus vaginalis detected during surgery. Modifications to the surgical technique in robot-assisted radical prostatectomy, such as Retzius-space sparing approach, have been associated with decreased risk of inguinal hernia afterward [Citation22]. Our study does not support the role of surgical technique in the risk associated as the risk increase was similar regardless of the surgical method. However, the Retzius-space preservation approach was not widely used in Finland during the study period. Thus, the effect of such technique modifications on the risk of hernia repair needs further studies.
Two possible modifications to the minimally invasive prostatectomy technique to lower the risk of inguinal hernia after surgery have been proposed. They are the spermatic cord isolation method and the processus vaginalis transection method. The first one is the method where the peritoneum is dissected bluntly free from elements of the spermatic cord at the level of the internal inguinal canal. The second method includes similar steps added with transection and ligation of processus vaginalis just distal to the peritoneum. These techniques are intriguing as they may prevent the retraction of transected vas deferens from pulling the peritoneum towards the inguinal canal. They have been suggested to lower the risk of post-surgical inguinal hernia after prostatectomy. Still, the evidence, even from randomized studies, has not changed the standard prostatectomy technique [Citation19].
Spermatic cord isolation and processus vaginalis transection are standard techniques in minimally invasive hernia repair. Standard hernia repair includes placing mesh to reinforce the weakened inguinal canal region. To our knowledge, using mesh as a prophylactic method during prostatectomy has not been studied. After prostatectomy, the mesh may be exposed to contaminated urine, thus to possible infection. However, multiple studies have evaluated simultaneous inguinal hernia repair and robot-assisted laparoscopic radical prostatectomy. In these publications, mesh placement has not increased morbidity or complications of prostatectomy [Citation23,Citation24]. In line with that, prophylactic mesh placement has been under active study focusing on preventing parastomal hernia, and results suggest this to be a safe approach despite high contamination risk [Citation25,Citation26].
Our study has several important strengths: it reflects the daily practice based on real-life register data. We adjusted the analysis for comorbidities and tumor extent, which may differ between men treated with prostatectomy and EBRT. The completeness and accuracy of data in the national registries used for this study are well-established [Citation18]. We were able to consider the timing of hernia surgery to PCa management and previous hernia repairs. The latter is essential to notify as hernia recurrence is common.
We did not have information on smoking habits or BMI. Smoking is a known risk factor in wound healing and thus may promote hernia formation in an incisional hernia. Smoking has not been found to increase the risk for inguinal hernia after prostatectomy [Citation27]. High BMI causes increased intra-abdominal pressure, which also may predispose to hernias. On the other hand, also low BMI has been associated with an increased risk of inguinal hernia [Citation27–30]. This study's lack of information on BMI and smoking may have been confounding factors, but their role is unclear. We did not have information on whether participants had lymphadenectomy along with prostatectomy. Such information would possibly have allowed the identification of subgroups with a particularly elevated risk of inguinal hernia. Further studies are needed to explore this question.
Further, we cannot rule out selection bias despite the similar distribution of comorbidities between the prostatectomy and EBRT groups; men whose PCa is managed surgically may be more eligible to undergo further surgical operations. Mortality during the follow-up was lower in the prostatectomy group (159/1000) than in the EBRT group (244/1000), which may be an expression of the same thing. In general, the male population has a 0.4–0.7% approximated annual incidence of inguinal hernia, which has to be considered interpreting the results. Even though we had information for a long period, some subjects may have had an inguinal hernia repair before 1998, which may have introduced a bias towards the null. Further, there has been a profound change in prostatectomy technique from open to minimally invasive during our study timeline. Thus follow-up periods after minimally invasive surgery are generally shorter than for open procedures.
Conclusions
The risk of subsequent surgical repair of inguinal hernia after primary PCa treatment is 40% higher in men managed with prostatectomy compared to men managed with radiotherapy. It should be noted when planning prostate cancer treatment. The risk increase is limited to men with an inguinal hernia diagnosis before prostate cancer diagnosis. Possible future studies on spermatic cord isolation and prophylactic mesh placement during surgery should be focused on this group.
Supplemental Material
Download MS Word (14 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2018;68(1):7–30.
- Regan TC, Mordkin RM, Constantinople NL, et al. Incidence of inguinal hernias following radical retropubic prostatectomy. Urology. 1996;47(4):536–537.
- Nielsen ME, Walsh PC. Systematic detection and repair of subclinical inguinal hernias at radical retropubic prostatectomy. Urology. 2005;66(5):1034–1037.
- Abe T, Shinohara N, Harabayashi T, et al. Postoperative inguinal hernia after radical prostatectomy for prostate cancer. Urology. 2007;69(2):326–329.
- Stranne J, Lodding P. Inguinal hernia after radical retropubic prostatectomy: risk factors and prevention. Nat Rev Urol. 2011;8(5):267–273.
- Stranne J, Hugosson J, Lodding P. Inguinal hernia is a common complication in lower midline incision surgery. Hernia. 2007;11(3):247–252.
- Ichioka K, Yoshimura K, Utsunomiya N, et al. High incidence of inguinal hernia after radical retropubic prostatectomy. Urology. 2004;63(2):278–281.
- Stranne J, Hugosson J, Iversen P, et al. Inguinal hernia in stage M0 prostate cancer: a comparison of incidence in men treated with and without radical retropubic prostatectomy-an analysis of 1105 patients. Urology. 2005;65(5):847–851.
- Lodding P, Bergdahl C, Nyberg M, et al. Inguinal hernia after radical retropubic prostatectomy for prostate cancer: a study of incidence and risk factors in comparison to no operation and lymphadenectomy. J Urol. 2001;166(3):964–967. 2001
- Sun M, Lughezzani G, Alasker A, et al. Comparative study of inguinal hernia repair after radical prostatectomy, prostate biopsy, transurethral resection of the prostate or pelvic lymph node dissection. J Urol. 2010;183(3):970–976.
- Lin BM, Hyndman ME, Steele KE, et al. Incidence and risk factors for inguinal and incisional hernia after laparoscopic radical prostatectomy. Urology. 2011;77(4):957–962.
- Nilsson A, Carlsson S, Laven B, et al. Karolinska prostatectomy: a robot-assisted laparoscopic radical prostatectomy technique. Scand J Urol Nephrol. 2006;40(6):453–458.
- Nilsson H, Stranne J, Stattin P, et al. Incidence of groin hernia repair after radical prostatectomy: a population-based nationwide study. Ann Surg. 2014;259(6):1223–1227.
- Lughezzani G, Sun M, Perrotte P, et al. Comparative study of inguinal hernia repair rates after radical prostatectomy or external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2010;78(5):1307–1313.
- Zhu S, Zhang H, Xie L, et al. Risk factors and prevention of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol. 2013;189(3):884–890.
- Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13(4):343–403.
- Charlson M, Pompei P, Ales K, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
- Pukkala E, Engholm G, Højsgaard Schmidt LK, et al. Nordic cancer registries – an overview of their procedures and data comparability. Acta Oncol. 2018;57(4):440–455.
- Alder R, Zetner D, Rosenberg J. Incidence of inguinal hernia after radical prostatectomy: a systematic review and meta-analysis. J Urol. 2020;203(2):265–274.
- Stranne J, Hugosson J, Lodding P. Post-radical retropubic prostatectomy inguinal hernia: an analysis of risk factors with special reference to preoperative inguinal hernia morbidity and pelvic lymph node dissection. J Urol. 2006;176(5):2072–2076. 2006
- Lee DH, Jung HB, Chung MS, et al. Patent processus vaginalis in adults who underwent robot-assisted laparoscopic radical prostatectomy: predictive signs of postoperative inguinal hernia in the internal inguinal floor. Int J Urol. 2013;20(2):177–182.
- Chang KD, Abdel Raheem A, Santok GDR, et al. Anatomical retzius-space preservation is associated with lower incidence of postoperative inguinal hernia development after robot-assisted radical prostatectomy. Hernia. 2017;21(4):555–561.
- Rogers T, Parra-Davila E, Maclher F, et al. Robotic radical prostatectomy with concomitant repair of inguinal hernia: is it safe? J Robot Surg. 2018;12(2):325–330.
- Bajpai RR, Razdan S, Sanchez-Gonzalez MA, et al. Simultaneous robotic assisted laparoscopic prostatectomy (RALP) and inguinal herniorrhaphy (IHR): proof-of-concept analysis from a high-volume center. Hernia. 2020;24(1):107–113.
- Antoniou SA, Agresta F, Garcia Alamino JM, et al. European Hernia Society guidelines on prevention and treatment of parastomal hernias. Hernia. 2018;22(1):183–198.
- Cross AJ, Buchwald PL, Frizelle FA, et al. Meta-analysis of prophylactic mesh to prevent parastomal hernia. Br J Surg. 2017;104(3):179–186.
- Hemberg A, Holmberg H, Norberg M, et al. Tobacco use is not associated with groin hernia repair, a population-based study. Hernia. 2017;21(4):517–523.
- Nilsson H, Stranne J, Hugosson J, et al. Risk of hernia formation after radical prostatectomy: a comparison between open and robot-assisted laparoscopic radical prostatectomy within the prospectively controlled LAPPRO trial. Hernia. 2022;26(1):157–164.
- Zendejas B, Hernandez-Irizarry R, Ramirez T, et al. Relationship between body mass index and the incidence of inguinal hernia repairs: a population-based study in Olmsted County, MN. Hernia. 2014;18(2):283–288.
- Rabbani F, Yunis LH, Touijer K, et al. Predictors of inguinal hernia after radical prostatectomy. Urology. 2011;77(2):391–395.
