Abstract
Introduction
CoreTherm (ProstaLund AB, Lund, Sweden) is an outpatient treatment option in men with lower urinary tract symptoms and catheter-dependent men with chronic urinary retention caused by benign prostatic obstruction (BPO). CoreTherm is high-energy transurethral microwave thermotherapy with feedback technique. Modern treatment with CoreTherm includes transurethral intraprostatic injections of mepivacaine and adrenaline via the Schelin Catheter (ProstaLund AB, Lund, Sweden) and is often referred to as the CoreTherm Concept.
Objectives
The aim of this study was to evaluate the short- and long-term retreatment risk in men with large prostates and BPO or chronic urinary retention, all primarily treated with CoreTherm.
Material and Methods
All men from the same geographical area with prostate volumes ≥ 80 ml treated 1999–2015 with CoreTherm and having BPO or were catheter-dependent due to chronic urinary retention, were included. End of study period was defined as December 31, 2019.
Results
We identified and evaluated 570 men treated with CoreTherm, where 12% (71 patients) were surgically retreated during the follow-up. Mean follow-up was 11 years, and maximum follow-up was 20 years. The long-term retreatment rate in our study was 23%. A majority of these could be retreated with CoreTherm or TURP, with only 3% requiring open surgery.
Conclusion
We conclude that CoreTherm is a suitable outpatient treatment option in patients with profoundly enlarged prostates, regardless of age, prostate size, and reason for treatment.
Introduction
Benign prostatic obstruction (BPO) can cause lower urinary tract symptoms or chronic urinary retention with subsequent catheter-dependency. These men can be cured by removal of the obstructing prostatic tissue, henceforth men with lower urinary tract symptoms due to BPO are referred to as men with BPO. The tissue removal can be achieved surgically by resection or enucleation. Transurethral resection of the prostate (TURP) or open surgery with adenoma enucleation has, for decades most often been considered the gold standard treatments in men with BPO, as well as in catheter bound men due to chronic urinary retention [Citation1–3].
The recommended upper prostate volume limit suitable to consider enucleation surgery instead of TURP is relative rather than absolute. In guidelines from the European Association of Urology (EAU) and American Urological Association (AUA), a prostate volume of >80–100 ml is where TURP could be deselected in favour of enucleative intervention [Citation1–3]. Moreover, in recent years, several other modalities have emerged as treatment alternatives in men with BPO, such as prostatic artery embolisation, vapor treatment (Rezum) and enucleation, resection or vapourisation using different laser devices [Citation4–7].
A specific challenge is addressing the elderly patient with the heavily enlarged prostate, where relative or absolute contraindications for surgery are often present. A minimally invasive option, suitable also for fragile patients is transurethral microwave thermotherapy (TUMT) with feedback technique (CoreTherm, ProstaLund AB, Lund, Sweden). This outpatient option to surgery causes coagulative necrosis in the transitional zone of the prostate. That CoreTherm leads to prostate volume reduction has been shown by magnetic resonance imaging, histopathology and transrectal ultrasound [Citation3,Citation8]. CoreTherm is a technically advanced TUMT that includes intraprostatic temperature measurements in real time during the procedure [Citation9].
Treatment with the CoreTherm Concept is almost identical to treatment with CoreTherm or ProstaLund Feedback Treatment (PLFT), but also includes intraprostatic administration of mepivacaine and adrenaline via a special injection device, the Schelin Catheter (ProstaLund AB, Lund, Sweden) [Citation10,Citation11], leading to improved cell kill. This modern treatment with CoreTherm is nowadays, after the introduction of the injection catheter two decades ago almost exclusively performed in conjunction with injections of mepivacaine and adrenaline. The calculated cell kill is based on a software algorithm and provides data on prostate tissue ablation in real time, thereby enabling tailoring of treatment [Citation3,Citation12].
CoreTherm is associated with few complications and is easy to learn, especially when using the alternative treatment endpoint [Citation12]. Furthermore, treatment with CoreTherm is also a feasible option for patients with urinary retention [Citation14,Citation15], most often caused by BPO [Citation13].
The aim of this study was to evaluate the short- and long-term retreatment risk after treatment with CoreTherm in patients with large prostates and BPO or catheter-dependency due to chronic urinary retention.
Material and methods
Patients
After ethical approval (Regional Ethics Review Board in Linköping: dnr 2010/394-31; 2015/471-32), data were collected from medical records and local data registers. The database included all men from the same geographical area with prostate volumes ≥80 ml treated with CoreTherm due to BPO, or who were catheter-dependent due to chronic urinary retention. All patients were seen at either the outpatient department at the local hospital or at one complementary outpatient clinic outside the hospital. Pre-treatment data from the medical records consisted of age at time of treatment, catheter use, and prostate volume, measured by transrectal ultrasound.
At the time of the study there were no standardised routine to record the pre- and post-operative symptoms at the clinics. The international prostate symptom score (IPSS), or a modified Madsen-Iversen score (by interview), was used to evaluate symptoms in most cases before and three months after treatment [Citation16,Citation17]. The quality of life (QoL) question was the IPSS-standard (self-administered or by interview), as well as uroflowmetry with peak urinary flow (Qmax) and a post-void residual volume measurement by ultrasound. Urodynamic studies were only undertaken in cases of pronounced storage symptoms or the presence of overt neurological disease, in many aspects used as recently suggested by Drake et al. [Citation18] and further commented in the editorial by Malde et al. [Citation19].
Retreatment with CoreTherm was undertaken at both clinics, but TURP or open surgery was performed as an inpatient procedure at the hospital clinic. Data on retreatment were collected retrospectively from the medical records of both clinics. Data on administration of a urinary catheter in patients without retreatment are not readily available from these records and are therefore lacking.
Procedure
Prior to treatment, all patients received medication orally, but as the study covered an extended period, some components of this premedication had been subject to ongoing modifications. Routinely all patients consistently received paracetamol and a muscarinic receptor antagonist or the beta3-adrenoceptor agonist mirabegron.
Antibiotic prophylaxis was given either as a single dose or during the entire catheter period. A non-steroidal anti-inflammatory drug was also used in most cases, if no contraindications were present. From 2003, the CoreTherm Concept, rather than CoreTherm, was the standard treatment, the Schelin Catheter was used for intraprostatic injections with mepivacaine and adrenaline. Treatment data: treatment time, energy consumption and calculated cell kill were collected from the computer software. Application procedure of mepivacaine and adrenaline, pre- and postoperative medication and follow-up protocol are identical to what has been previously described from our group [Citation3,Citation10,Citation12].
Statistics
The primary endpoint of the present study was the rate of successful primary treatment: one minus failure was defined as a new treatment <1 year or still being catheter dependent at the three months follow-up. Thus, the primary endpoint does not include avoidance of a new catheter after the stipulated three months follow-up, if this did not lead to a new treatment.
The secondary endpoint was long-term retreatment free survival, including subgroup analysis of age categories, patients with BPO versus chronic urinary retention and prostate volume, by survival analysis using the Kaplan–Maier method. Baseline and treatment data were analysed to calculate mean, standard deviation median and range.
Analyses were made to compare the outcome for men in different age groups, with BPO versus chronic urinary retention and gland size ≤100 ml versus >100 ml. Differences between groups at or after intervention were analysed using Kruskal–Wallis ANOVA followed by Mann–Whitney’s U-test in case of significance. Univariate and multivariate Cox regression models were used on available baseline data to calculate hazard rate ratios for individuals needing reintervention. End points were, apart from reoperation and mortality, also diagnosis of prostate cancer. In the multivariate Cox regression model, parameters with p ≤ 0.1 in the univariate analyses were included. P-value <0.05 were thereafter considered as a statistical significance difference.
The patients were enrolled at the date of the first treatment with CoreTherm. End of study period was defined as December 31, 2019. Follow-up was censored if a patient died or was diagnosed with prostate cancer during the study period. Statistica version 13.5.0.17 (TIBCO Software, Inc., Palo Alto, CA, USA) was used for all statistics.
Results
Between 1999 and 2015, a total of 570 men from the including clinics catchment area with BPO or having a catheter due to chronic urinary retention were treated with CoreTherm. Totally 338 men (59%) were treated at the hospital clinic and 232 (41%) were treated at the outpatient clinic. A total of 237 men (42%) used a catheter due to chronic urinary retention. Mean follow-up was 11 years, and maximum follow-up was 20 years. Baseline data are presented in . Data on treatment time, energy consumption, calculated cell kill, IPSS, Madsen–Iversen score, Qmax, QoL and retreatment rates are presented in , showing a significantly higher score regarding IPSS, Madsen-Iversen score (voiding) and QoL in the group retreated <1 year. The catheter time (the time between treatment and first trial without a catheter) after treatment was, with few exceptions, three to six weeks. Overall retreatment rates were low (). In total, 71 of 570 men (12%) were surgically retreated, out of which 17 men (3%) had, and 61 men (11%) were retreated with CoreTherm (). Among the 237 men who used a catheter due to chronic urinary retention, a total of 192 men (81%) were catheter-free at follow-up. In the univariate and multivariate analysis, on available baseline data and categories as presented in , only age was significant (values for categorised data from in ). A total of 50 men were diagnosed with prostate cancer and thus were censored at time of diagnosis. No patient developed post treatment urinary incontinence.
Figure 1. (A–D). A total of 570 men registered in the same geographical area with prostate volumes ≥80 ml treated 1999–2015 with CoreTherm due to lower urinary tract symptoms and benign prostatic obstruction, or who were catheter-dependent due to chronic urinary retention were subject to follow-up until December 31, 2019. Kaplan–Meier curves, calculated for retreatment free survival. All 570 patients are included in (A–D) and numbers at risk are presented at 10 intervals. In (B), age data were divided into quartiles, but as the curves of the two youngest quartiles were superimposed, these graphs were merged. (C) data are dichotomised between men with benign prostatic obstruction (LUTS/BPO) and men using catheter due to chronic urinary retention (CUR) and in (D) dichotomised by gland size.
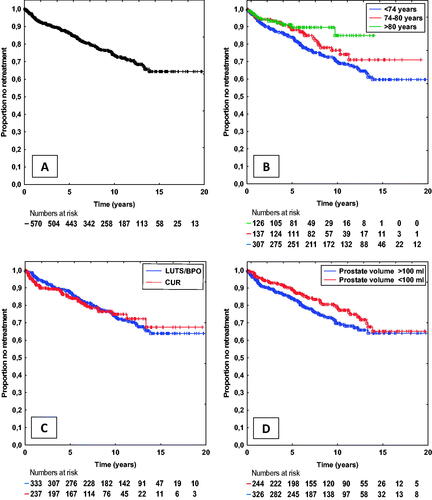
Table 1. Patient characteristics before treatment.
Table 2. A total of 570 men registered in the same geographical area with prostate volumes ≥80 ml treated 1999–2015 with CoreTherm due to lower urinary tract symptoms and benign prostatic obstruction, or who were catheter-dependent due to chronic urinary retention were subject to follow-up until December 31, 2019.
Table 3. A total of 570 men registered in the same geographical area with prostate volumes ≥80 ml treated 1999-2015 with CoreTherm due to lower urinary tract symptoms and benign prostatic obstruction, or who were catheter-dependent due to chronic urinary retention were subject to follow-up until December 31, 2019.
Age data demonstrates a long-term success rate for all patient groups, with an apparent age-dependent discrepancy, with the lowest retreatment rate for the oldest age group (). Data dichotomised between men with BPO, or catheter-bound men demonstrate a similar long-term success rate () as is also valid for data dichotomised by gland size ().
Discussion
This study showed low short- and long-term retreatment risk for CoreTherm in men with large prostates. The Kaplan–Meier analyses demonstrated low retreatment risk irrespective of treatment cause, patient age or glandular size. The long-term results, with a mean follow-up of 11 years and maximum follow-up of 20 years, apparent from the present study, strongly suggests it should have definitive place in the treatment arsenal for urologists worldwide.
The long-term retreatment rate in our study was 23%. A majority of these could be retreated with CoreTherm or TURP, with only 3% requiring open surgery. As the study consisted of a selected group of patients with large prostates where the primary treatment in most cases otherwise would have been open surgery, this must be considered rewarding. The fact that a minimally invasive procedure as CoreTherm often constitutes the only possible curative treatment option in elderly fragile patients with chronic urinary retention, otherwise doomed to lifelong catheter dependency, further underscores the importance of the results of this study. All retreatments with CoreTherm, TURP or open surgery were included in the present series, meaning that technical failures or other malfunctions using CoreTherm were not accounted for. Also, retreatment within 3-6 months after a technically successful treatment with CoreTherm is most often a too early intervention. A prolonged post-treatment period of up to 6 months may be required to achieve optimal symptom amelioration after treatment, particularly in patients having pronounced storage symptoms, a phenomenon previously seen after TURP [Citation20], as well as prolonged healing of the prostatic necrosis, which is more likely in the elderly patient population. Furthermore, in some cases, treatment with CoreTherm was used by intent in patients with trilobal enlargement, an underutilised treatment strategy that may be appropriate in some cases.
Although microwave treatment only ablates the tissue in the bladder neck, some patients may benefit from a wider bladder neck despite the presence of a third lobe, thus leading to voiding improvement and a reduced bother score. If a patient fails to improve after treatment with CoreTherm, surgery can perhaps be performed by resection of the median lobe alone, reducing operative time and hence risk for elderly fragile patients. Unfortunately, due to lack of systematic data on trilobal enlargement in our study, we could not systematically evaluate or report this interesting issue, although a median lobe was often present at the time of surgery. One of the first clinical studies that showed CoreTherm as an option even in heavily enlarged prostates was a prospective randomised multicentre study of 120 patients with chronic urinary retention by Schelin in 2006 [Citation15]. The primary objective was to evaluate CoreTherm versus TURP and open enucleative surgery in patients with chronic urinary retention. The authors could find no significant statistical difference between groups, and the conclusion was that results were comparable, regardless of method. In total, 79% of the patients treated with CoreTherm were relieved of their catheter as compared to 86% in the surgical arm. These data tally with the findings in the present study, where 192 patients (81%) were relieved of their catheter.
That CoreTherm can be an excellent option in elderly fragile patients with chronic urinary retention was shown by Aagaard et al. in a study of 124 patients judged unsuitable for surgery due to comorbidity [Citation14]. In their study, 77 patients (62%) were deemed unfit for surgery. Besides an increased QoL in 98 patients (79%) after treatment, a total of 95 patients (77%) were relieved of their catheter. The study also included 21 patients with prostate volumes >100 ml (range 103–300 ml), with CoreTherm as their only option to become catheter-free. The results from that report are also in line with the results reported here, even though the number of patients in our study that were truly unfit for surgery has not been disclosed. Nevertheless, 126 patients (22%) were older than 80 years, and avoidance of surgery in these men was most likely of value to reduce both morbidity and mortality rates. In a randomised clinical study, comparing long term effects for HoLEP versus open surgery in prostates >100 ml, results were comparable. Retreatment rates and voiding improvement were at the same level for both methods [Citation21]. Compared to the retreatment rates in our study, it appears that HoLEP, as well as other enucleating techniques, often have retreatment rates at a level that resection or thermoablative methods cannot reach. However, comparing surgical inpatient interventions, often requiring anaesthesiologic resources with a minimally invasive outpatient option as CoreTherm must be made with caution, considering morbidity, mortality and costs.
The strength of this study was that a large cohort of patients with heavily enlarged prostates allowed for long-term evaluation of retreatment events. The same type of TUMT device (CoreTherm) was used in all patients, an undisputable strength of this study. A limitation of the present study is the retrospective nature of data from collection from different, prospectively registered sources and that no standardised long-term follow-up was performed for the entire cohort, patients may therefore have been lost to follow-up. Hence, the material might be biased out of these respects. Systematic data on post treatment drug use, post treatment urinary tract infections, complete post treatment clinical parameters, such as peak urinary flow, as well as administration of a urinary catheter in patients not receiving retreatment are lacking. The obvious lower retreatment risk for elderly patients (illustrated in ) is possibly multifactorial, but avoidance of reintervention in patients with more frequent comorbidity, is at least partially a feasible explanation. Nevertheless, treatment as well as retreatment with CoreTherm still seems a viable option.
However, in the area where patients were included, there are no urological health care providers besides those included in the study. Thus, it is unlikely that many patients would have sought urological health care outside these two institutions unless they had changed their place of residency. All Swedish patients, however, have a unique identification number by which they can be located and, hence, we could identify and exclude the patients that had moved from the catchment area.
Conclusion
We conclude that treatment with the CoreTherm is a suitable outpatient treatment option in patients with profoundly enlarged prostates, regardless of age, prostate size and treatment cause.
Acknowledgement
The authors gratefully acknowledge Dr Sonny Schelin for invaluable support and advice.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Gravas S, Cornu JN, Gacci M, EAU Guidelines on Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO), et al. 2020. European association of urology guidelines 2020 edition. Presented at the EAU annual congress amsterdam 2020. Arnhem, The Netherlands: European Association of Urology Guidelines Office; 2020.
- Parsons JK, Dahm P, Kohler TS, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2020. J Urol. 2020;204(4):799–804.
- Stenmark F, Brudin L, Stranne J, et al. High-energy feedback microwave thermotherapy and intraprostatic injections of mepivacaine and adrenaline: an evaluation of calculated cell kill accuracy and responder rate. Scand J Urol. 2014;48(4):374–378.
- Shim SR, Kanhai KJ, Ko YM, et al. Efficacy and safety of prostatic arterial embolization: Systematic review with Meta-Analysis and Meta-Regression. J Urol. 2017;197(2):465–479.
- McVary KT, Rogers T, Roehrborn CG. Rezum water vapor thermal therapy for lower urinary tract symptoms associated With benign prostatic hyperplasia: 4-Year results From randomized controlled study. Urology. 2019;126:171–179.
- Bozzini G, Berti L, Aydoğan TB, et al. A prospective multicenter randomized comparison between holmium laser enucleation of the prostate (HoLEP) and thulium laser enucleation of the prostate (ThuLEP). World J Urol. 2021;39(7):2375–2382.
- Thomas JA, Tubaro A, Barber N, et al. A multicenter randomized noninferiority trial comparing GreenLight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of benign prostatic obstruction: Two-yr outcomes of the GOLIATH study. Eur Urol. 2016;69(1):94–102.
- Huidobro C, Bolmsjo M, Larson T, et al. Evaluation of microwave thermotherapy with histopathology, magnetic resonance imaging and temperature mapping. J Urol. 2004;171(2 Pt 1):672–678.
- Bolmsjo M, Sturesson C, Wagrell L, et al. Optimizing transurethral microwave thermotherapy: a model for studying power, blood flow, temperature variations and tissue destruction. Br J Urol. 1998;81(6):811–816.
- Schelin S. Mediating transurethral microwave thermotherapy by intraprostatic and periprostatic injections of mepivacaine epinephrine: effects on treatment time, energy consumption, and patient comfort. J Endourol. 2002;16(2):117–121.
- Schelin S. Transurethral resection of the prostate after intraprostatic injections of mepivacain epinephrine: a preliminary communication. Scand J Urol Nephrol. 2009;43(1):63–67.
- Stenmark F, Brudin L, Kjolhede H, et al. Prostate volume and age are predictors of energy delivery using the CoreTherm concept in patients with LUTS/BPO: a study on thermal dose. Scand J Urol. 2020;54(3):248–252.
- Verhamme KMC, Dieleman JP, van Wijk MAM, et al. Low incidence of acute urinary retention in the general male population: the triumph project. Eur Urol. 2005;47(4):494–498.
- Aagaard MF, Niebuhr MH, Jacobsen JD, et al. Transurethral microwave thermotherapy treatment of chronic urinary retention in patients unsuitable for surgery. Scand J Urol. 2014;48(3):290–294.
- Schelin S, Geertsen U, Walter S, et al. Feedback microwave thermotherapy versus TURP/prostate enucleation surgery in patients with benign prostatic hyperplasia and persistent urinary retention: a prospective, randomized, controlled, multicenter study. Urology. 2006;68(4):795–799.
- Barry MJ, Fowler FJ, Jr., O’Leary MP, The Measurement Committee of the American Urological Association, et al. The American urological association symptom index for benign prostatic hyperplasia. The measurement committee of the American urological association. J Urol. 1992;148(5 Part 1):1549–1557.
- Barry MJ, Fowler FJ, Jr., O’Leary MP, The Measurement Committee of the American Urological Association, et al. Correlation of the American urological association symptom index with self-administered versions of the Madsen-Iversen, boyarsky and Maine medical assessment program symptom indexes. Measurement committee of the American urological association. J Urol. 1992;148(5 Part 1):1558–1563.
- Drake MJ, Lewis AL, Young GJ, et al. Diagnostic assessment of lower urinary tract symptoms in men Considering prostate surgery: a noninferiority randomised controlled trial of urodynamics in 26 hospitals. Eur Urol. 2020;78(5):701–710.
- Malde S, Sahai A, Solomon ER, et al. Diagnostic assessment of lower urinary tract symptoms in men Considering prostate surgery: a noninferiority randomised controlled trial of urodynamics in 26 hospitals. Eur urol 2020;78:701-10. Eur Urol. 2020;78(6):e232–e3.
- Sagen E, Nelzen O, Peeker R. Transurethral resection of the prostate: fate of the non-responders. Scand J Urol. 2020;54(5):443–448.
- Kuntz RM, Lehrich K, Ahyai SA. Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol. 2008;53(1):160–166.
