Abstract
Objective
Patients with clinical T1 renal cell carcinoma (cT1RCC) have risks for recurrence and reduced overall survival despite being in the best prognostic group. This study aimed to evaluate the association of different treatments on disease recurrence and overall survival using clinical and pathological characteristics in a nation-wide cT1RCC cohort.
Materials and methods
A total of 4,965 patients, registered in the National Swedish Kidney Cancer Register (NSKCR) between 2005 and 2014, with ≥ 5-years follow-up were identified: 3,040 males and 1,925 females, mean age 65 years. Times to recurrence and overall survival were analyzed with Kaplan-Meier curves, log-rank test, and Cox regression models.
Results
Age, TNM-stage, tumor size, RCC-type, and performed treatment were all associated with disease recurrence. Patients selected for ablative treatments had increased risk for recurrent disease: hazard ratio (HR) = 3.79 [95% confidence interval (CI) = 2.69–5.32]. In multivariate analyses, age, gender, tumor size, RCC-type, N-stage, recurrence and performed treatment were all independently associated with overall survival. Patients with chRCC had a 41% better overall survival (HR = 0.59, 95% CI = 0.44–0.78; p < 0.001) than ccRCC. Patients treated with partial nephrectomy (PN) had an 18% better overall survival (HR = 0.83, 95% CI = 0.71–0.95, p < 0.001) than patients treated with radical nephrectomy.
Conclusions
Age, gender, T-stage, tumor size, RCC type and treatment modality are all associated with risk of recurrence. Furthermore, age, male gender, tumor size, N-stage and recurrence are associated with reduced overall survival. Patients with chRCC, compared with ccRCC and pRCC patients, and PN compared with RN treated patients, had an advantageous overall survival, indicating a possible survival advantage of nephron sparing treatment.
Introduction
Renal cell carcinoma (RCC) represents about 3% of all malignancies [Citation1]. With an annual increase of about 2% in Europe during the last decades, there were approximately 99,200 newly-diagnosed RCCs within the European Union in 2018 [Citation1]. One reason for the increased incidence might be the frequent use of cross-sectional imaging. Today, >60% of new RCCs are incidentally diagnosed, resulting in generally lower tumor stages [Citation2]. This stage migration has resulted in >60% of new RCCs being classified as T1, with mostly low malignant properties. Therefore, the treatment of T1 RCC has elaborated from open radical nephrectomy towards nephron-sparing procedures [Citation3,Citation4]. It has been claimed that the oncological outcome is similar between nephron-sparing surgery and radical nephrectomy for T1 RCC patients [Citation3,Citation5,Citation6]. Most guidelines recommend nephron sparing surgery when feasible [Citation3,Citation4]. However, small RCCs may also invade and metastasize [Citation7]. Upstaging from cT1 at preoperative imaging to pT3 has previously been reported in several studies after surgery [Citation8,Citation9]. Any upstaging to pT3 may entail a higher risk for local tumor recurrence and metastases, and a risk for impaired survival after nephron-sparing treatments.
Aim
The aim of this nation-wide population-based cohort study was to evaluate the occurrence of local recurrences and distant metastases in clinical non-metastatic T1 RCC patients and analyze the risk for recurrent disease and decreased overall survival in relation to patient and tumor characteristics as well as treatment modalities.
Materials and methods
Patients
Since January 2005, all Swedish patients diagnosed with RCC have been registered in the National Swedish Kidney Cancer Register (NSKCR). The coverage of the NSKCR is 99% as compared with the Swedish Cancer Register, in which all new cancer patients are registered according to law.
A total of 4,965 patients registered in the NSKCR with non-metastatic (M0) cT1 RCC from January 2005 to December 2014, having a potential follow-up time of ≥ 5-years after treatment, were included: 3,040 (61%) males and 1,925 (39%) females, with a mean age of 65 (median 67) years (). With a generated query from the NSKCR after 5 years, all M0 patients were approached via their clinical departments with retrospective evaluations of recurrences diagnosed within these 5-years. Exclusion criteria were metastases at diagnosis, cT-stage ≥ 2, tumor size > 7.0 cm or previous RCC treatment.
Table 1. The distribution of patient’s characteristics in relation to renal cell carcinoma (RCC) type, of 4,965 patients with cT1 RCC extracted from the National Swedish Kidney Cancer Register, years 2005–2014.
Time to disease recurrence free survival (RFS) was calculated from date of diagnosis to date of recurrence. The patient’s unique Swedish personal identity number was linked to the Swedish National Population Register for obtaining information about overall survival. Survival time was defined as time from date of diagnosis to date of death of any cause or being alive at the end of follow-up (31 December 2018 for patients registered in the NSKCR during the years 2005–2012 or 31 December 2020 for patients registered during the years 2013–2014). Part of this cohort, patients with cT1a RCC diagnosed during the years 2005–2012 (n = 1,935), were included in a recent study [Citation33,Citation10,Citation31,Citation32]. Information about patients’ age, gender, TNM stage, RCC type, tumor size and primary treatments were obtained from the NSKCR. Patients classified as Nx in the register were re-classified as N0/NX. Tumor size was defined as the largest diameter of the tumor at CT. Tumor stage was defined according to the 7th TNM classification and RCC type according to the WHO classification [Citation11,Citation12]. Radiofrequency ablation (n = 267), cryoablation (n = 35) and HIFU (n = 2) were merged into the single variable ablative treatments. Recurrence was defined as: residual tumor in the treated kidney after primary ablation or partial nephrectomy, local recurrent disease in the kidney fossa after any treatment or observed distant metastases.
Ethical approval
The study was approved by the regional Ethical Review Board of Northern Sweden (Dnr 2012-418-31 M) and the Swedish Ethical Review Agency (Dnr 2019-02579).
Statistical analysis
Categorical variables are presented as frequencies and percentages, n (%), while continuous and ordinal variables are given as means ± standard deviations (SDs). Differences between groups were tested using Pearson’s χ2-test for categorical variables and the Mann-Whitney U test for continuous variables. Overall survival was analyzed by log-rank tests and accompanied by Kaplan-Meier curves. The associations of patient and tumor characteristics with recurrence and with overall survival were assessed by uni- and multivariate Cox regression analysis, with the results presented as hazard ratios (HRs) with 95% confidence intervals (CIs). IBM SPSS Statistics 26.0 was used for statistical analysis. Two-tailed p-values < 0.05 were considered statistically significant.
Results
Patient and tumor characteristics
Each patient was followed-up for ≥ 5 years, including date of recurrence and site of recurrence, with a mean ± SD follow-up time of 7.4 ± 2.9 years. Among the 4,965 patients, 56% had cT1a and 44% had cT1b RCC. After surgery and histological examination, 561 (11%; 4% of cT1a and 19% of cT1b) patients were upstaged to pT3 (). Tumor size associated significantly with T3a upstaging (p < 0.001). Clear cell RCC (ccRCC) was the most common RCC type (76%), followed by papillary RCC (pRCC; 14%) and chromophobe RCC (chRCC; 6%). For 90 patients (1.8%) a variety of other RCC types were registered, while for 93 (1.9%) patients histology was unknown, mostly in patients being treated non-surgically ().
Treatment
Most (60%) patients were treated with radical nephrectomy, followed by partial nephrectomy in 30% and ablative therapy in 6% of the patients. Additionally, 21 patients were treated with various other surgical procedures and 134 (2.7%) of the cT1 patients were non-surgically treated (). The proportion of radical nephrectomy increased with tumor size and was more frequent than partial nephrectomy in tumors with a size of 40–70 mm (p < 0.001). Ablative therapy was rarely performed in cT1b (). Patients treated with PN had a mean age of 61 years, significantly younger than those treated with RN (66 years), ablation (68 years) and surveillance (76 years) (data not shown).
Table 2. Recurrent disease in relation to tumor size and to the performed treatment shown in 4,965 patients with cT1M0 renal cell carcinoma.
Recurrence
As shown in , 578 (11.6%) patients were diagnosed with recurrent disease: 44.3% had lung metastases, 18.7% bone, 16.6% in the treated kidney and 9.9% in lymph nodes. Local recurrence in the renal fossa was found in 1.0% of the patients, with no significant difference between the RCC types (). Lung recurrences were observed more often among ccRCC than in pRCC-patients (p = 0.001), but no significant differences were observed for other recurrence sites. With only 12 chRCC-patients diagnosed with recurrence, no meaningful statistical analyses could be performed for this group.
Table 3. Distribution of sites of disease recurrence in relation to histological tumor type in 578 patients among the 4,965 patients with cT1M0 renal cell carcinoma at primary diagnosis.
Recurrence was more common among patients with ccRCC (13%) than pRCC (9%) or chRCC (4%) (p = 0.009 and p = 0.004, respectively; ). Patients treated with radical nephrectomy or ablation experienced recurrence more often than partial nephrectomy-treated patients (14% and 17%, respectively, vs 7%; p < 0.001; ). Of the 53 recurrences among ablation-treated patients, 38 were registered as local recurrences only in the treated kidney and two patients had local recurrences but also distant metastases. Among patients treated with partial nephrectomy, 3.2% had local kidney recurrences, significantly less frequent than patients treated with ablation (p < 0.001). In total, 15 (4.9%) ablation treated patients were diagnosed with distant metastases, which did not differ from patients treated with partial nephrectomy (p = 0.116).
There were no differences in recurrences between genders in univariate analysis, while higher age significantly associated with higher recurrence risk (p < 0.001; data not shown). shows the relations between pT-stage, RCC type, recurrence, and overall death. Significant differences in recurrence free-survival (RFS) were found for T-Stage, RCC type, type of treatment and N-stage (all p < 0.001; data not shown). More advanced T-stages had shorter RFS (p < 0.001), while ccRCC and pRCC patients had shorter RFS than those with chRCC (p < 0.001 and p = 0.012, respectively). Patients treated with partial nephrectomy had longer RFS than patients treated with both radical nephrectomy and ablation (p < 0.001), while there was no significant difference between radical nephrectomy and ablation (p = 0.114).
Table 4. Distribution of survival status in relation to RCC type, pT stage, occurrence of recurrent disease and survival in 4,965 patients with cT1 renal cell carcinoma.
In adjusted analyses of RFS, women had a 17% significantly lower risk for recurrence than men (HR = 0.83; 95% CI = 0.70–0.99) while higher age entailed a 1.6% increased risk for recurrence per year of age (). Moreover, increased tumor size was associated with a 2.7% increased risk for recurrence per mm of tumor size (HR = 1.03; 95% CI = 1.02–1.04). Higher T-stages implied increased risks of recurrence, HRs (95% CI) = 1.32 (0.97–1.80) and 2.83 (2.04–3.93) for pT1b and pT3a, respectively, compared with pT1a (). While patients treated with partial nephrectomy and radical nephrectomy did not differ significantly in recurrence risk, having had an ablation implied a 3.8-times higher risk of experiencing recurrence during follow-up (p < 0.001), compared with radical nephrectomy (). Patients with pRCC and chRCC, compared with ccRCC, had significantly lower risks for disease recurrence; HR = 0.75 (95% CI = 0.57–0.98) and 0.33 (95% CI = 0.19–0.54), respectively (). A positive lymph node status entailed a nearly 5-times higher risk for recurrent disease (). Supplementary Table S1 shows, after excluding patients with local recurrence only, comparable results in adjusted multivariate analysis.
Table 5. Results for Cox regression analysis of factors important for time to recurrent disease in 4,965 patients with non-metastatic cT1 renal cell carcinoma.
Overall survival
Univariate association of T-stage, N-stage, RCC type, type of treatment and recurrence in relation to overall survival is illustrated by Kaplan-Meier curves in ). Age had a major impact on overall survival while gender showed no significant difference (data not shown). Increase in T-stage and tumor size were associated with worse overall survival (p < 0.001), while patients with ccRCC had worse overall survival than patients with pRCC or chRCC. Patients treated with partial nephrectomy had better overall survival than those treated with radical nephrectomy or ablation (all p < 0.001).
Figure 1. Kaplan-Meier curves of univariate overall survival probability in relation to (a) T stage, pT1a, versus pT1b versus pT3a, (p < 0.001 for all pair-wise differences), (b) patients with recurrent disease versus no recurrence (p < 0.001), (c) RCC types (p < 0.001 for chromophobe RCC versus papillary RCC versus clear cell RCC), and (d) treatment with partial nephrectomy, ablative treatment, and radical nephrectomy (p < 0.001 for partial nephrectomy versus ablation, and versus radical nephrectomy, respectively). Number of patients at risk are shown below corresponding time points.
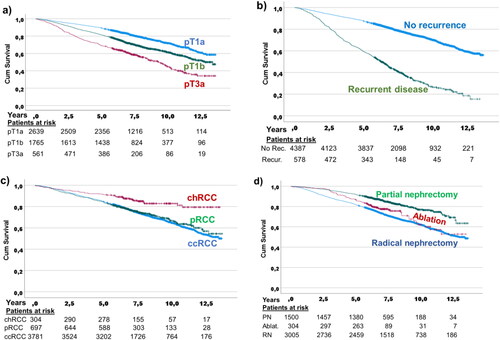
In adjusted analyses, higher age increased the risk for overall death by 6.7% per year of age, while females had longer OS than males (). Larger tumor size significantly increased the risk for overall death during follow-up by 14% for each cm larger size (). Partial nephrectomy treated patients had significantly longer overall survival compared with radical nephrectomy, HR = 0.82 (95% CI = 0.71–0.95; p = 0.010), while ablation did not differ significantly from RN-treated patients (). T-stage did not remain significant in the adjusted analyses, including recurrence in the model. For RCC type, chRCC implied a significantly better overall survival than having ccRCC, HR = 0.59 (95% CI = 0.44–0.78; p < 0.001), while patients with pRCC had a similar overall survival risk as ccRCC. Moreover, patients with other RCC types and patients with unknown RCC types had significantly higher risks for adverse overall survival. Both N-stage and recurrence entailed higher risks for reduced overall survival, HRs (95% CI) = 2.20 (1.62–2.99) and 2.86 (2.53–3.24), respectively (). Supplementary Table S2 includes an adjusted multivariate analysis without influence of recurrence in the model, showing comparable results.
Table 6. Results from Cox regression analysis of factors important for overall survival in 4,965 patients with non-metastatic cT1 renal cell carcinoma, adjusted for age, gender, tumor size, RCC type, pT-stage, given treatment, recurrence status and N-stage.
Discussion
This real-world nation-wide register-based total population cohort study of cT1 RCC patients showed that several factors affected recurrence and overall survival. Patients were treated based on decisions taken by the individual urologist and the patient’s preferences. Generally, it is assumed that non-metastatic cT1 RCC patients have an excellent prognosis, being in the most advantageous RCC stage [Citation3]. However, as shown in the present study, the risk for disease progression and early death is not trivial. A significant proportion of these cT1 patients were afflicted with upstaging and recurrences, features associated with adverse survival.
Results in perspective
Our results showed that, in adjusted analyses, the risks for recurrence and overall death increased by 2.7% and 1.4%, respectively, per mm increase in tumor size. Thus, tumor size seems to be important for the ultimate clinical course even in small RCCs. These results indicate that increase in tumor size is an independent risk factor for recurrence and death. Thus, early tumor treatment is desirable. This conclusion is strengthened by the fact that older patients in our study had higher risks, possibly due to longer time of tumor growth before diagnosis. As expected, higher age at diagnosis was also independently associated with shorter overall survival.
The present study also showed that upstaging from cT1 to pT3 was predictive of tumor recurrence and reduced overall survival, in line with previous studies suggesting that upstaging was afflicted with a more aggressive disease [Citation13,Citation14,Citation15]. In our study, 11.3% of cT1 were upstaged to pT3, a proportion slightly higher than the 9.3% reported by Nayak et al. [Citation8] but in concordance with the 11.4% observed in a recent multi-site study comprising 8185 cT1-2 RCC patients [Citation13]. In another recent review and metanalysis of 21,869 patients with cT1 RCCs, 5.7% were upstaged [Citation14]. The higher proportion of upstaging observed in the present study might be due to the use of an unselected nation-wide total population group of patients. Thus, improved radiological staging of cT1 tumors seems warranted [Citation16,Citation17]. In the adjusted analysis in our study, T-stage did not remain a significant predictor of OS when recurrence was included in the analysis. Moreover, the rarely occurring (1.2%) N1 disease was significantly associated with recurrence and worse overall survival in adjusted analyses, confirming previous reports [Citation18].
In the present study, RCC type was another important factor for disease recurrence and overall survival. Patients with chRCC entailed significantly fewer recurrences than other RCC-types, in concordance with earlier studies [Citation19,Citation20]. In adjusted analysis, patients with chRCC and pRCC had better RFS than those with ccRCC. In contrast to Abu-Ghanem et al. [Citation20], we found no obvious difference in pattern of recurrence sites based on RCC type, except a higher rate of lung recurrences in ccRCC than in pRCC patients. In adjusted analyses, chRCC implied a 42% lower risk for impaired overall survival compared with ccRCC.
Treatment of cT1 RCC patients is based on several considerations adjusted by recommendations and surgeons’ preferences [Citation3,Citation4]. The proportion of radical nephrectomy in this study was 60%, with an increasing proportion of nephron sparing treatments over time [Citation2]. Local recurrence was most common in patients selected for ablation, in line with previous reports [Citation21,Citation22]. A majority of the recurrences after ablative treatments were localized in the treated kidney. Nevertheless, it implies a need for a more intense imaging follow-up and retreatment after ablation than after surgical resection, supporting established guidelines [Citation3,Citation4]. Most previous studies comparing oncological outcomes of partial and radical nephrectomies were retrospective and mostly with a limited number of included patients [Citation23]. The differences in recurrence may be attributed to factors such as central versus peripheral tumor location, tumor complexity, and tumor size, factors that may influence the treatment decision towards radical nephrectomy and therefore entail more frequent recurrences and tumors with poorer prognosis than after partial nephrectomy [Citation24]. Similarly, patients selected for ablation may be unsuitable for partial nephrectomy, due to age, co-morbidities, or tumor associated factors that may have influenced the clinical outcome.
It has been debated whether partial nephrectomy improves overall survival compared with radical nephrectomy. Partial nephrectomy preserves kidney function better than radical nephrectomy, thereby potentially reducing the risk of developing cardiovascular disorders [Citation25]. Particularly in patients with pre-existing reduced kidney function, partial nephrectomy is the treatment of choice to limit the risk for haemodialysis. Huang et al. [Citation26] found that 26% of patients with newly-diagnosed RCC had a glomerular filtration rate ≤ 60 mL/min, even though their baseline serum creatinine levels were in the normal range. Compared with radical nephrectomy, several retrospective analyses have suggested a decreased cardiovascular-specific mortality and improved overall survival for patients treated with partial nephrectomy [Citation3,Citation27]. In some series this held true only for younger patients [Citation28]. However, there were obvious evidence limitations, with most studies afflicted by a low methodological quality. In the only randomized clinical trial, prematurely closed and heavily underpowered, partial nephrectomy seemed to be inferior to radical nephrectomy in terms of overall survival in the intention-to-treat analyses [Citation29]. The present study, using real-word data, showed that partial nephrectomy-treated patients had an 18% lower risk for reduced overall survival compared with radical nephrectomy. This survival advantage was independent of patients’ age, gender, T-stage, tumor size, and RCC type, results supporting a recent systematic review by Chung et al. [Citation30], who found significantly improved overall survival for patients treated with partial nephrectomy (HR = 0.74; 95% CI = 0.75–0.95) compared with radical nephrectomy. Despite higher mean age at diagnosis, ablation-treated patients had a non-significantly similar risk for overall death in adjusted analysis, in line with a recent study of cT1a RCC [Citation10]. Using the SEER cancer database, Tang et al. [Citation31] showed the importance of tumor size for both all-cause mortality and cancer-specific mortality when analyzing partial nephrectomy, ablative treatment and active surveillance, respectively. In a multicenter review of 1,783 cT1 RCC patients without chronic kidney disease, the authors concluded that patients who benefit most from PN were those with relevant co-morbidities [Citation32]. Our results indicate that PN-treated patients have an OS advantage, possibly due to preserved renal function.
Strengths and limitations
Important limitations of the present study were that confounders such as concomitant diseases, performance status, and cause of death were unavailable. Since there likely was a bias in the selection of the primary treatment, a comprehensive comparison between the given treatments was not possible. Furthermore, it should be noted that the study period includes early learning curves for the different ablation techniques and laparoscopic and robotic assisted partial nephrectomies, respectively, and the results therefore may not be representative of today’s standard of treatment. With register-based data being collected from a wide range of hospitals, complete uniformity in data collection was unattainable and may have resulted in coding discrepancies. All patients, evaluated with CT or MRI at primary diagnosis, were treated based on patients and surgeons’ preferences. The NSKCR has, however, showed a high comparability and validity [Citation33]. Important strengths of the present study were that the participants constituted a non-selected nation-wide total population cohort of practically all RCC patients in Sweden, all having valid overall survival data available.
Conclusions
Our study of cT1 RCC patients showed that age, gender, T-stage, tumor size, RCC type and treatment modality all associated with risk of recurrence. Furthermore, age, male gender, tumor size, N-stage and recurrence associated with reduced overall survival. Patients with chRCC, compared with ccRCC and pRCC and patients treated with partial nephrectomy compared with radical nephrectomy had an advantageous overall survival, indicating a possible survival advantage of nephron sparing treatment.
Supplemental Material
Download Zip (101.1 KB)Acknowledgements
Thanks to the members of the NSKCR steering committee. The authors specially thank Soheila Hosseinnia and other collaborators at the Regional Cancer Centre Stockholm-Gotland for providing data from the NSKCR.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–1953.
- Thorstenson A, Harmenberg U, Lindblad P, et al. Impact of quality indicators on adherence to National and European guidelines for renal cell carcinoma. Scand J Urol. 2016;50(1):2–8.
- Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European association of urology guidelines on renal cell carcinoma: the 2022 update. Eur Urol. 2022;82(4):399–410. Epub ahead of print. PMID: 35346519.
- Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA guideline. J Urol. 2017;198(3):520–529.
- Weight CJ, Lythgoe C, Unnikrishnan R, et al. Partial nephrectomy does not compromise survival in patients with pathologic upstaging to pT2/pT3 or high-grade renal tumors compared with radical nephrectomy. Urology. 2011;77(5):1142–1146.
- Deng H, Fan Y, Yuan F, et al. Partial nephrectomy provides equivalent oncologic outcomes and better renal function preservation than radical nephrectomy for pathological T3a renal cell carcinoma: a meta-analysis. Int Braz J Urol. 2021;47(1):46–60.
- Dabestani S, Thorstenson A, Lindblad P, et al. Renal cell carcinoma recurrences and metastases in primary non-metastatic patients: a population-based study. World J Urol. 2016;34(8):1081–1086.
- Ramaswamy K, Kheterpal E, Pham H, et al. Significance of pathologic T3a upstaging in clinical T1 renal masses undergoing nephrectomy. Clin Genitourin Cancer. 2015;13(4):344–349.
- Nayak JG, Patel P, Saarela O, et al. Pathological upstaging of clinical T1 to pathological T3a renal cell carcinoma: a multi-institutional analysis of short-term outcomes. Urology. 2016;94:154–160.
- Almdalal T, Sundqvist P, Harmenberg U, et al. Clinical T1a renal cell carcinoma, not always harmless – a national register study. Eur Urol Open Sci. 2022;39:22–28.
- Sobin LH, Gospodarowicz MK, Wittekind C, editors. 2009. TNM classification of malignant tumours. 7th ed. New York: Wiley-Liss.
- Moch H, Cubilla AL, Humphrey PA, et al. The 2016 WHO classification of tumours of the urinary system and male genital organs-part A: renal, penile, and testicular tumours. Eur Urol. 2016;70(1):93–105.
- Patel SH, Uzzo RG, Larcher A, et al. Oncologic and functional outcomes of radical and partial nephrectomy in pT3a pathologically upstaged renal cell carcinoma: a multi-institutional analysis. Clin Genitourin Cancer. 2020;18(6):e723–e729.
- Veccia A, Falagario U, Martini A, et al. Upstaging to pT3a in patients undergoing partial or radical nephrectomy for cT1 renal tumors: a systematic review and meta-analysis of outcomes and predictive factors. Eur Urol Focus. 2021;7(3):574–581.
- Chevinsky M, Imnadze M, Sankin A, et al. Pathological stage T3a significantly increases disease recurrence across all tumor sizes in renal cell carcinoma. J Urol. 2015;194(2):310–315.
- Teishima J, Hayashi T, Kitano H, et al. Impact of radiological morphology of clinical T1 renal cell carcinoma on the prediction of upstaging to pathological T3. Jpn J Clin Oncol. 2020;50(4):473–478.
- Renard AS, Nedelcu C, Paisant A, et al. Is multidetector CT-scan able to detect T3a renal tumor before surgery? Scand J Urol. 2019;53(5):350–355.
- Kim SH, Park B, Hwang EC, et al. Prognostic significance of pathologic nodal positivity in non-metastatic patients with renal cell carcinoma who underwent radical or partial nephrectomy. Sci Rep. 2021;11(1):3079.
- Noguchi G, Nakaigawa N, Taguri M, et al. Time-dependent change in relapse sites of renal cell carcinoma after curative surgery. Clin Exp Metastasis. 2018;35(1–2):69–75.
- Abu-Ghanem Y, Powles T, Capitanio U, et al. The impact of histological subtype on the incidence, timing, and patterns of recurrence in patients with renal cell carcinoma after surgery-results from RECUR consortium. Eur Urol Oncol. 2021;4(3):473–482.
- Jiang K, Tang K, Guo X, et al. Laparoscopic cryoablation vs. percutaneous cryoablation for treatment of small renal masses: a systematic review and meta-analysis. Oncotarget. 2017;8(16):27635–27644.
- Abu-Ghanem Y, Fernández-Pello S, Bex A, et al. Limitations of available studies prevent reliable comparison between tumour ablation and partial nephrectomy for patients with localised renal masses: a systematic review from the European Association of Urology Renal Cell Cancer Guideline Panel. Eur Urol Oncol. 2020;3(4):433–452.
- MacLennan S, Imamura M, Lapitan MC, et al. Systematic review of perioperative and quality-of-life outcomes following surgical management of localised renal cancer. Eur Urol. 2012;62(6):1097–1117.
- Correa AF, Toussi A, Amin M, et al. Small renal masses in close proximity to the collecting system and renal sinus are enriched for malignancy and high fuhrman grade and should be considered for early intervention. Clin Genitourin Cancer. 2018;16(4):e729–e733.
- Ljungberg B, Hedin O, Lundstam S, et al. Nephron sparing surgery associated with better survival than radical nephrectomy in patients treated for unforeseen benign renal tumors. Urology. 2016;93:117–123.
- Huang WC, Levey AS, Serio AM, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. 2006;7(9):735–740.
- Kates M, Badalato GM, Pitman M, et al. Increased risk of overall and cardiovascular mortality after radical nephrectomy for renal cell carcinoma 2 cm or less. J Urol. 2011;186(4):1247–1253.
- Sun M, Becker A, Tian Z, et al. Management of localized kidney cancer: calculating cancer-specific mortality and competing risks of death for surgery and nonsurgical management. Eur Urol. 2014;65(1):235–241.
- Van Poppel H, Da Pozzo L, Albrecht W, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59(4):543–552.
- Chung DY, Kang DH, Kim JW, et al. Comparison of oncologic outcomes between partial nephrectomy and radical nephrectomy in patients who were upstaged from cT1 renal tumor to pT3a renal cell carcinoma: an updated systematic review and meta-analysis. Ther Adv Urol. 2020;12:1756287220981508.
- Tang Y, Liu F, Mao X, et al. The impact of tumor size on the survival of patients with small renal masses: a population-based study. Cancer Med. 2022;11(12):2377–2385.
- Larcher A, Capitanio U, Terrone C, et al. Elective nephron sparing surgery decreases other cause mortality relative to radical nephrectomy only in specific subgroups of patients with renal cell carcinoma. J Urol. 2016;196(4):1008–1013.
- Landberg A, Bruce D, Lindblad P, et al. Validation of data quality in the National Swedish Kidney Cancer Register. Scand J Urol. 2021;18:1–7.
