ABSTRACT
This review concentrates on the research concerning conjugates of anticancer drugs with versatile cell-penetrating peptides (CPPs). For a better insight into the relationship between the components of the constructs, it starts with the characteristic of the peptides and considers its following aspects: mechanisms of cellular internalization, interaction with cancer-modified membranes, selectivity against tumor tissue. Also, CPPs with anticancer activity have been distinguished and summarized with their mechanisms of action. With respect to the conjugates, the preclinical studies (in vitro, in vivo) indicated that they possess several merits in comparison to the parent drugs. They concerned not only better cellular internalization but also other improvements in pharmacokinetics (e.g. access to the brain tissue) and pharmacodynamics (e.g. overcoming drug resistance). The anticancer activity of the conjugates was usually superior to that of the unconjugated drug. Certain anticancer CPPs and conjugates entered clinical trials.
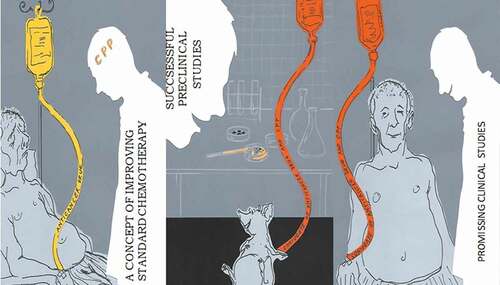
GraphicleAbstract
1. Introduction
Despite the great progress in pharmacotherapy, many diseases, as for example cancers, are still a great challenge for the clinicians. Their pharmacological treatment is often unsuccessful and burdened with severe complications and a high mortality rate. The main reason for this fact is the unsatisfactory efficacy of the drugs, which results from their pharmacokinetic and/or pharmacodynamic features, and the most important of which refer to low cellular bioavailability, poor penetration to the target, toxicity and development of drug resistance.
The ability to permeabilize in the membrane and gain access to the cytosolic compartment is largely dependent on the physicochemical qualities of the therapeutic entities including the most relevant such as lipophilicity (determined by drug hydrophilicity/hydrophobicity), polarity and molecular size. Among them, a fairly but not excessively hydrophobic character is most conducive to the drug transport; very large, polar hydrophilic molecules are being poorly internalized similarly as extremely hydrophobic (the former ones will fail to enter the membrane, the latter will enter readily but may have difficulty in leaving it).
Briefly, getting a drug to its target can be a considerable challenge because the compound has to cross fewer or more barriers along its way. They comprise endothelial (the blood–brain barrier [BBB]) and epithelial (gastrointestinal mucous, skin) sheets, which are represented by tightly interconnected cells resulting in highly impermeable structures that compartmentalize different physiological microenvironments.Citation1–4 Thus, transepithelial and transendothelial transports of drugs may become limited or even arrested
On the other hand, cellular internalization of the drug may be completely changed under pathological conditions. Such a phenomenon is characteristic of anticancer therapy. Intratumoral drug penetration and direct contact with the malignant cells are hampered by deregulation and disorganization of the tumor stroma (it becomes stiff and dense due to its reduced turnover and excessive production) and the abnormal blood flow with preference for the peripheral tumor region.Citation1,Citation2
At the cellular level, most anticancer drugs act on membrane surface receptors or have intracellular targets. In the latter case, a drug must cross the cellular membrane that constitutes an additional barrier for it. A further complication for drug traversing the cellular membranes is their remodeling induced by cancer itself, which brings about complex changes in the membrane structure and composition. They lead to a drop in anticancer drug efficacy manifested by simultaneous cancer cell proliferation, avoidance of apoptosis and development of cellular resistance.Citation5–8
Generally, anticancer therapy bears a high incidence of toxicity due to a low therapeutic index of the drugs and the simultaneous necessity for the usage of high doses in order to produce the clinical effect. An explanation for these unfavorable parameters of the anticancer therapy is lack of drug selectivity (they damage not only cancerous cells but also healthy rapidly growing ones) and poor bioaccessibility to the tumor cells. Another shortcoming of this therapy is multidrug resistance (MDR), which constitutes one of the dominant reasons for its failure. Versatile mechanisms are involved in this process including decreased drug uptake, increased drug efflux, reprogramming of the target structure, enhanced enzymatic inactivation, etc.
The presented limitations of cancer treatment have been imperative to the development of diverse strategies of targeted drug delivery to tumor tissue by exploiting passive and active technologies. The passive technologies may utilize such phenomena as charge selectivity (preference for negatively charged tumor membranes over those of neutral healthy ones)Citation9–11 and/or enhanced permeability and retention (EPR) effect that arises from the unique anatomical and pathophysiological characteristics of solid tumors (e.g. leaky vasculature, impaired lymphatic drainage).Citation12,Citation13 The active ones involve the usage of special ligands (e.g. transferrin, folate, epidermal growth factor, antibodies) that target molecules or receptors within the tumor cells. It should be emphasized that the EPR effect constitutes an indispensable step for starting the active targeted process.Citation13
An attractive application of the EPR effect in tumor chemotherapy comprises therapeutics in the form of liposomes, polymers or micelles.Citation14–16 This effect has also been utilized by experimental technologies based on cell-penetrating peptides coupled with diverse types of cargoes (low molecular weight anticancer drugs). The CPP may be a part of a simple construct or a component of a macromolecular delivery system.
CPPs constitute a class of oligopeptides rich in basic amino acids characterized by exceptional translocation properties across cell membranes including those which form vital biological barriers without significant interference with their integrity. These peptides originate from a wide variety of sources (as for example humans, mice, viruses, synthesis) and usually carry a positive net charge. It is generally accepted that both endocytosis and direct translocation contribute to the internalization process of the CPPs. Besides being inert vectors for translocating and transporting cargoes into the intracellular milieu, some of them also show biological activity [Citation17–22; Citation23–26].
This review will focus on CPPs conjugated covalently or noncovalently with anticancer drugs approved by the FDA. These constructs will be presented in terms of the anticancer efficacy and clinical potential in different types of tumors.
2. Classification of CPPs
CPPs are a class of diverse short sequence peptides (usually <30 amino acids) of natural (protein-derived or chimeric) or synthetic origin.Citation27,Citation28 There are several classifications of the CPPs, but none of them is ideal to the very end. They adopt versatile criteria, and the most often used is that which considers the physical–chemical properties of the amino acid components of the peptide. According to this classification they can be categorized into three main classes, i.e. hydrophilic (e.g. Tat), hydrophobic (e.g. Pep-7) and amphipathic (e.g. TP10) peptides. The latter ones contain both hydrophilic and hydrophobic domains and include primary (e.g. pVEC) and secondary (e.g. azurine-derived p28 peptide, proline-rich CPPs) compounds with peculiar α-helical or β-sheet structures.Citation29,Citation30 With respect to the net charge of the CPPs, most of them (83%) are cationic. Anionic CPPs do not form a class of their ownCitation31 nevertheless, SAP(E) and p28 may serve as examples of these peptides.Citation32–35
3. Internalization mechanisms of CPPs
The exact mechanisms by which CPPs cross the cell membrane still remain to be carefully clarified. One of the reasons for this fact is that the cellular membrane itself constitutes a highly complex and heterogeneous structure composed of specific domains as glycoproteins, polysaccharides and lipids. Moreover, the bending and fluidity properties of the membrane change together with local modifications in its potential.
According to the available data, CPPs are internalized by two possible main pathways, i.e. endocytosis (energy dependent) and/or direct translocation (energy independent). Endocytosis is of vital significance for the cationic CPPs and an exclusive mechanism for the anionic peptides.Citation29,Citation33,Citation35 The first phase which precedes endocytosis is usually an electrostatic interaction with negatively charged cell surface components such as proteoglycan glycosaminoglycan (GAG) platform (the major constituent of the extracellular matrix). This process is followed by actin remodeling and GTPase activation resulting in changes in membrane fluidity.Citation7,Citation36
It is not surprising that the anionic CPPs do not share the electrostatic mechanism with cationic peptides, but instead they use another process as the first step of cellular entry, i.e. peptide aggregation on the membrane surface.Citation33–35,Citation37–39
Next, the peptides undergo endocytosis, which comprises several diverse pathways classified as macropinocytosis, clathrin/caveolae-mediated endocytosis and clathrin/caveolae-independent endocytosis.Citation29,Citation40–42 Some CPPs have been shown to use more than one of these internalization routes, even simultaneously.Citation42 During endocytosis, a CPP remains entrapped in endosomes and therefore, after internalization a peptide must escape to the cytosol to avoid enzymatic degradation from lysosomes.Citation29,Citation41 Entrapment in the endosomal compartments appears to be the principal limiting factor in the efficient intracellular delivery of functional macromolecules, e.g. drugs. Hence, versatile approaches have been undertaken to facilitate the escape of CPPs from the endosomes.Citation29
On the other hand, direct translocation involves peptides entering straight through the cytosol after recruiting negatively charged phospholipid headgroups and/or exploiting membrane defects. Additionally, this process requires permanent or temporary membrane destabilization for internalization to occur. As a process which requires no energy, direct translocation is regarded as a single-step episode including mechanisms involving the formation of pores (“toroidal” or “barrel-stave”),Citation43–45 inverted micelles (entrapment of the peptide by membrane curvatures or invaginations and its release into the cytosol by their inversion)Citation46,Citation47 or a “carpet” with the positively charged segments of the peptide covering the negatively charged membrane (local reorganization and disruption of the membrane due to a change in the CPP secondary structure as the basic residues turn toward the membrane surface and the hydrophobic residues interact with the hydrophobic membrane core).Citation29,Citation30,Citation40,Citation41,Citation48–53
Whether a CPP utilizes endocytosis, direct translocation, or both processes for internalization depends on many factors, as for example the chemical structure of the peptide,Citation54 temperature,Citation55 the targeted cell type,Citation40 the condition of the lipid membrane.Citation51 Thus, it is rather impossible to ascribe a specific mechanism of internalization to each individual CPP. Taking into account one of the best known CPP, i.e. Tat, it employs, depending on the concentration, both direct translocation (forming transient pores)Citation44 and endocytosis (caveolae-mediated pathway or macropinocytosis).Citation56 On the other hand, the few known anionic peptides utilize only endocytosis (caveolae-dependent pathway) as a mechanism of cellular uptake.Citation33,Citation57,Citation58 In addition, the cargo (its type, size and charge) as well as the CPP-cargo formulation design may be decisive for the mechanism involved in membrane permeation.Citation59 It is likely that multiple mechanisms are active simultaneously, and the down-regulation of one pathway might lead to an upregulation of the other.Citation40
Irrespective of the route of internalization, the majority of the CPPs localizes in the cytoplasm or the nucleus.Citation28,Citation59,Citation60 They may also provide subcellular organelle delivery as happens in the case of mitochondria-specific CPPs, i.e. mitochondria-penetrating peptides or vesicle-based CPPs.Citation61,Citation62 It is worth stressing that the nucleus and the mitochondria are relevant targets for many cargoes including anticancer drugs.
4. The role of CPPs in cancer treatment
4.1. CPPs as vectors for anticancer drug delivery
4.1.1. Interaction of CPPs with cancer-modified cell membranes
The interaction of a CPP with cancerous cells should be considered in light of the current concept of cancer-induced modifications within the cell membrane itself. They concern both its heteropolysaccharide and lipid components, ensuring the uncontrolled growth, progression and invasiveness of the tumor cells.
The heteropolysaccharides such as GAGs are constituents of proteoglycans and include several categories: chondroitin sulfate, dermatan sulfate, heparan and heparin sulfates, hyaluronan. As a rule, they are overexpressed in cancerous membranes. Moreover, GAGs undergo complex disorganization which concerns their structural pattern and composition. They are implicated in various phases of carcinogenesis as for example the activation of crucial cell signaling cascade, epithelial/mesenchymal transition, the adaptive protection of malignant cells to natural killers.Citation6–8 Moreover, the higher abundance of GAGs in tumor cell membranes results in their increased anionic profile relative to those of non-transformed ones.Citation7
Also, the lipid component contributes to the anionic character of the cancerous membrane due to the exposition of the negatively charged phosphatidylserine (instead of electrically neutral zwitterionic lipids) in its outer leaflet which correlates with a more acidic pH of their external media as well. Furthermore, there are changes in cholesterol metabolism leading to either a lower or higher content relative to the type of cancer, stage and sensitivity. All these modifications result in denser packing of the lipids and a decreased fluidity of the membrane, turning the latter more rigid and less permeable for the drugs.Citation57,Citation63–65
Generally, the CPPs possessing mostly cationic nature due to arginine and lysine residues favor the negatively charged tumor membranes over those of healthy cells, which are electrically neutral. Of great importance is the electrostatic interaction of the positively charged arginine guanidinium head groups with the negatively charged GAGs, sialic acid or phospholipid head groups displayed in abundance on the surface of the tumor cells. This type of interaction ensures that the CPP indicates a certain level of selectivity to tumor cells referred to as passive charged selectivity. Although it is not complete, the CPPs themselves are not reported to produce toxicity below the concentrations of hundreds of μmoles.Citation9–11
4.1.2. Improvement of anticancer selectivity of CPPs
An innovation with respect to the classic peptides is the group of tumor-homing CPPs, which are originally obtained by mRNA display technology. The most characteristic feature of them is that they are able not only to distinguish between cancer and normal cells but also target specific tumor cell types. One of them which has been described in a more detailed way is CPP44. A critical role in its internalization plays endogenous M160 protein, which is overexpressed in myelogenous leukemias and hepatic tumors.Citation66
Another method of increasing the tumor cell selectivity of CPPs is utilization of a homing device such as an antibody or a targeting ligand (e.g. RGD peptides, folic acid, transferrin, hyaluronic acid) that will enable to attach to tumor cells through antigens or receptors on their surface, usually overexpressed in certain tumor types. For example, folate receptors are highly expressed in ovarian, cervical, breast, kidney, colorectal, lung and brain tumors.Citation28,Citation67–74 Versatile CPPs (e.g. octaarginine – R8, Tat) have been functionalized by a homing device demonstrating the potential usefulness for enhancing the delivery of a cargo to its target.Citation75
Also, there are novel active strategies, which adopt various methods of temporal inactivation of the CPPs by neutralizing their charge or placing a steric hindrance that restrains the nonspecific penetration of the peptides in normal tissue. The CPPs regain their activity within the tumor microenvironment thanks to specific triggers derived from intrinsic stimuli of the target site (acidic pH, MMP-2/9) or their extrinsic counterparts (topical application of heat, light, magnetism). Within this paradigm of controlled CPP delivery, the distinctive examples comprise activable CPPs, ATTEMPT (Antibody Targeted Triggered Electrically Modified Prodrug-Type strategy), Pop-up, cleavable protecting polymer strategies. A detailed description of all of them has been delivered by others.Citation28,Citation67,Citation73,Citation75–79
4.2. CPPs with additional anticancer activity
The privileged access of the CPPs to the tumor cells does not exhaust entirely their significance in the prospect of anticancer therapy. As has been indicated, some members of both cationic and anionic CPPs possess anticancer activity per se, which may be primarily accomplished by a lytic effect on the cancerous cell membrane or non-lytic actions. The diverse mechanisms responsible for this activity are summarized in . Taking into account the primary mode of action, the CPPs in question may be divided into four categories and each of them with the most recognizable representatives is outlined below.
Table 1. Representatives of CPPs with anticancer activity, mechanisms of action investigated on versatile experimental models
4.2.1. CPPs with strong cell membrane activity
Primary amphipathic CPPs like TP10 and sC18 form a helix in the presence of membrane phospholipids, which leads to an intense attack against negatively charged membrane components. As a consequence, destabilization or disruption of the cellular membrane (forming, e.g. transient prepores or barrel or toroidal pores) takes place.Citation48,Citation51 This membrane activity is responsible for the high cell-penetrating capacity of both peptides. On the other hand, the interaction between the CPPs in question and the membrane may be intense enough to cause a necrotic effect.Citation18,Citation80,Citation97–99
TP10 is a natural 21-residue chimeric CPP obtained by engineering mastoparan (a peptide derived from wasp venom) and the neuropeptide galanin linked through an extra lysine residue.Citation100 Unlike arginine-rich peptides, TP10 possesses four lysines which together with an N-terminus produce a charge of 5+ under neutral pH conditions. Many studies performed in vitro demonstrated an evident cytotoxic action of this peptide on versatile cancerous cell lines (HeLa, OS143B) at concentrations that were only negligibly harmful for nonmalignant cells.Citation18
The second amphipathic peptide (sC18) is derived from the cationic antimicrobial peptide CAP18. To obtain an enhanced cellular uptake, its dimeric version was designed in which the second unit was introduced at the side chain of Lys residue, ensuring that both N-termini of sC18 sequences remain free.Citation81 Owing to this procedure, which results in bringing the net positive charge to the value of 17, and the linear topology into the branched one (sC18)2 acquires a high cell-penetrating capacity and a rather selective action on tumorous cells. Also, its biodistribution within them changes with preference for the nuclei, where the peptide accumulates.Citation80
Indeed, further research on (sC18)2 confirmed its above-presented qualities, which are expressed not only by a broader spectrum of anticancer activity but also low toxicity. This was found on the basis of an experimental protocol that comprised 16 tumor cell lines obtained from distinct tissues such as, e.g. skin, lung, liver, breast, colon, prostate. Moreover, the values of IC50 for certain types of cancers were even more than 10-times lower (e.g. melanoma A2058, lung cancer H1650, liver cancer HepG2) in comparison to those calculated for healthy cells.Citation80,Citation81
The importance of branching and arginine number for activity has also been described for other CPPs.Citation40,Citation101
4.2.2. CPPs with pro-apoptotic activity
The most known CPPs within this group are p28-azurin derived,Citation33,Citation34 buforin IIb and its derivative BR2.Citation85,Citation86
The CPP which has gained considerable attention is p28, a 2.9-kDa fragment of bacterial protein – azurin (residues of 50–77). This CPP binds to the nuclear suppressor protein p53, inhibiting its proteasomal degradation, irrespective of whether it is of wild or mutated type. The main consequence of restoration of p53 function in cancerous cells is upregulation of p21 and p27 (cyclin-dependent kinase inhibitors), which leads to a decrease in CDK2-cyclin A complex (essential protein for mitosis) as well as FoxM1 (a transcription factor for G2/M progression). Thus, p28 is considered to be a cell cycle–specific cytostatic agent that induces apoptotic cell death via a p53-mediated block at the G2/M phase.Citation34,Citation39,Citation102
Latest findings report that this peptide also functions in a non-p53-mediated mechanism to inhibit tumor growth. Namely, thanks to the ability to enter endothelial cells, it also diminishes tumor neoangiogenesis by inhibition of the activity of VEGFR-2 and FGFR-1 kinases.Citation82
The promising preclinical anticancer activity and pharmacokinetics of p28 together with lack of immunogenicity and toxicityCitation83 were an incentive for entering two phase I clinical trial studies designated NCT00914914 and NCT01975116. The former one comprised adults (at age of ≥18) with refractory solid tumors, and the latter – children and adults (at age of 3–21) with versatile brain malignancies. Both studies indicated a good tolerance and safety profile of p28, even in children who were treated with the adult suggested phase II dose. This favorable outcome is not surprising since p28 has been characterized as a tumor-homing peptide that preferentially enters tumor cells, while sparing normal ones.Citation33 Although in pediatric tumors, this CPP was not effective enough as a single agent, a significant improvement in the survival of adults with versatile resistant solid tumors was encouraging researchers to perform combinatorial studies in which additive cell kill with chemotherapeutics could be exploited.Citation103,Citation104
Other examples of CPPs include synthetic peptides like buforin IIb and its derivative BR2. The first one indicates strong anticancer activity against a broad spectrum of cancerous cell strains, which implies that the molecular target(s) for buforin IIb is/are universally present in these cells. After being internalized via endocytosis (preceded by electrostatic interaction with cell surface gangliosides and sialic acid), this peptide is primarily accumulated in the nucleus. The cell killing effect is due to the induction of apoptosis by a mitochondria-dependent pathway.Citation85
Because of the α-helical structure at buforin IIb C-terminus, this peptide is also cytotoxic to normal cells, although at high concentrations. This cytotoxic effect was minimized by a procedure, which involved α-helicity reduction in the molecule of buforin IIb. As a result, another CPP, i.e. BR2 (17 amino acids) was obtained with the maintained strong anticancer activity of the parent peptide, but without toxicity to normal untransformed cells.Citation86,Citation105 These features of BR2 have been confirmed in experimental protocols in which this peptide was fused with a single chain variable fragment (scFv) of the antibody against mutated KRASCitation86 or with a recombinant fusion protein with truncated diphtheria toxin (DT386)Citation106 or was incorporated onto the surface of a liposome loaded with the anticancer agent cantharidin.Citation107 Importantly, BR2 displayed greater membrane translocation membrane efficacy and induced a higher degree of apoptosis in KRAS mutated cells than Tat.Citation86,Citation108 BR2 as a cancer-homing peptide has a great potential to become a useful delivery system for versatile anticancer drugs.
4.2.3. CPPs with pro-apoptotic and strong membrane activities
This group of CPPs includes lactoferricins (Lfcins) derived from bovine (LfcinB) and human (LfcinH) lactoferrins. They are amphipathic, highly positively charged but differ with respect to the lengths of the peptide and the amino acid sequence. Although both possess anticancer activity, the research focusing on LfcinB and its derivatives has been more fruitful, and therefore a short outline with the encouraging results is presented below.
LfcinB is a multifunction short cyclic cationic peptide (25 residues) derived from whey protein lactoferrin by its acid-pepsin hydrolysis. Its net charge is 8+ due to the presence of five arginines and three lysines in the molecule. LfcinB has been reported to be cytotoxic against human cell lines obtained from versatile cancers (breast, colon, stomach, melanoma, fibrosarcoma).Citation87,Citation88 Furthermore, the peptide inhibits liver and lung metastases of both murine melanomas and lymphomas.Citation87,Citation109,Citation110
The cytotoxic activity of this peptide has been attributed to the core sequence 20-RRWQWR-25 (LfcinB20-25), which is an amphipathic and positively charged (3+) motif.Citation111 Additionally, an increase in polyvalence resulting in enhanced hydrophobicity of the molecule improves much the selective toxicity against tumor cells, and this becomes a hallmark of the tetrameric peptide LfcinB(20–25)4.Citation89–91
Tetramerization of the minimal LfcinB motif results in the net positive charge of 12+ and a dendrimeric structure, which has been shown to maximize the efficacy of the peptide.Citation89 The improved selective anticancer effect of LfcinB(20–25)4 has become visible on several cancer cell lines as MCF7 (breast cancer), SCC15, CAL27 (oral cavity squamous-cell carcinomas – OSCCs) with 80%, 93% and 96% inhibition of cell viability, respectively.
The high antitumor activity of the peptide has been confirmed on the OSCC hamster experimental model, which mimics the tumorous pathogenic processes involved in human OSCC. The cytotoxic effect against tumor cells was executed by two different types of cellular death: apoptosis (activation of caspases or cathepsin B) and necrosis (membrane lytic effect). Specifically, apoptosis was the main mechanism of cell death at lower concentrations of LfcinB(20–25)4 while necrosis was found only at higher ones.Citation89,Citation90,Citation112
It is worth stressing that the peptide, due to the intrinsical bioactivity and solubility, meets the requirements for intratumoral administration, which as a local route produces a superior antitumor effect with less severe adverse reactions in comparison to that induced by systemic application.
The favorable features of LfcinB led to a vast number of studies on the structure–activity relationship of Lfcin-derivedCitation91 and synthetic model peptides, which resulted in designing and synthesizing an amphipathic helical nanopeptide LTX-315 whose residues have been optimized for antitumor activity.Citation92,Citation110,Citation113 Its cytotoxicity and the underlying mechanisms of action have been explored on several cancer cell lines as well as on tumor animal models that feature key aspects of human disease. As these studies indicated, LTX-315 possessed anticancer activity against a broad spectrum of malignancies, including melanoma, fibrosarcoma, mesenchymal subcutaneous sarcoma, breast cancer, etc.Citation93,Citation94,Citation114 The results obtained after a direct administration of this peptide into the tumor (e.g. mouse/rat established melanoma, sarcoma, triple-negative breast cancer) are particularly encouraging because of the complete tumor regression (fibrosarcoma in rats, melanoma in mice) or growth inhibition with a strong abscopal effect (tumor regression in nontreated distal lesions).Citation92,Citation94,Citation95 It is worth emphasizing that in humans, the above-mentioned tumors do not benefit much from the available drug therapy.
As far as the mechanisms involved in the anticancer activity of LTX315 are concerned, at least dual sequential phases are triggered by the peptide, i.e. a rapid direct cytotoxic effect (cell lysis of the vasculature) and a long-lasting one characterized by alterations of the tumor environment that involves infiltration with CD8+ T cells that display antitumor functions. The latter phase is particularly important in all these types of cancers that are poorly infiltrated with T cells as happens in melanoma, and therefore their conversion into highly immunogenic ones (transition from a “cold” to a “hot” tumor environment) provides a long-term immunity, preventing tumor regrowth after treatment.Citation92,Citation96,Citation110,Citation115
Generally, LTX-315 is a locally acting oncolytic agent of high efficacy and proper safety profile. The urgent need for new antitumor therapies and the promising pharmacological features of the compound in question have caused it to enter different settings of phase I and II clinical trials [NCT03725605, NCT01986426, NCT01058616, NCT01223209]. Those which involve combinations with the approved anticancer drug are described in Section 6.1.1.
4.2.4. CPPs with other activities
This Subsection focuses on synthetic CPPs composed entirely of arginine amino acids (R)n as, e.g. R8, R9, R12, R16. The minimal sequence necessary for cellular uptake is six arginines, and the peptide penetrating capacity of the plasma membrane increases with their number in the molecule.Citation116,Citation117 Much research has been devoted to the oligoarginine mechanisms of cellular entry, considering of which may be worthful in the context of anticancer activity of these peptides.
It is commonly accepted that internalization of oligoarginine peptides involves diverse types of endocytotic processes with the dominant role of macropinocytosis accompanied by actin cytoskeleton rearrangement.Citation116,Citation118–120 However, there is also ample evidence for the importance of direct passing through the cellular membrane.Citation55,Citation119,Citation121
Much attention has been attracted to R8, which is even considered to have the potential of a prototypic tumor-targeting vector due to selective accumulation in malignant cells with endocytosis playing a key role. This phenomenon was observed in experiments performed on tumor xenografted mice.Citation122
Considering the mechanism of anticancer activity of arginine-rich CPPs, the research concerning their usage with cargo or toxicity hinted at the involvement of cellular DNA and RNA. Putting it more precisely, the peptides indicate not only high affinity to nucleic acids but are also able to cause widespread defects in their metabolism.Citation116,Citation121,Citation122
5. Conjugation of CPPs with a cargo – two different strategies
The association of the CPPs with their cargo may be divided into covalently or noncovalently bound. Both formulation approaches have pros and cons. The advantage of the covalent one (chemical cross-linking between the CPP and cargo) is obtaining a final product with a well-defined chemical structure and reproducibility of the procedure.Citation123,Citation124 Of great importance is the cargo coupling position because it may impact the nascent conjugate with respect to its chemical stability (e.g. fragmentation), pharmacokinetics (e.g. uptake pathway) and/or pharmacodynamics (e.g. activity, cytotoxicity).Citation125–127 Moreover, the risk of unfavorable alteration of the biologic activity of the cargo must be considered.Citation128,Citation129
On the other hand, noncovalent interaction, i.e. physical complexation involves a simple bulk-mixing procedure of the compounds (CPP and cargo with or without a linker). This strategy, in comparison to the above-described one, is more simple and much easier to perform. Furthermore, it enables the usage of versatile cargos (with the preservation of their functionality) and low concentrations for induction of the biological response. However, the difficulty to control the final ratio and orientation of the peptide and cargo remains an important limitation of this method.Citation129
6. The anticancer activity improvement of the standard chemotherapeutics by CPPs
Classical cytotoxic anticancer drugs are known for targeting nonspecifically any rapidly dividing cells (irrespective of whether they are tumorous or not) due to their small size and lipophilicity. Also, loss of efficacy (caused by acquired drug resistance) and their inadequate pharmacokinetic characteristic with limited biodistribution often contribute to a poor final outcome of cancer management.
Recently, it has been found that the pharmacological properties of the chemotherapeutics may be improved by conjugating them with the CPPs, and this results in an increased efficacy of the transported drugs. Thanks to the presence of the CPP in the conjugate, the drug internalization is promoted with the consequence of high concentrations within the tumorous cells. What is more, certain areas in the body (e.g. the brain), which are frequently inaccessible for the therapeutics, become the target.Citation77
It is noteworthy that the improved pharmacokinetics is not the only factor that impacts the activity profile of the conjugate. There is also evidence for possible pharmacodynamic interactions between its constituents since certain CPPs possess anticancer action. An additional beneficial feature of coupling a chemotherapeutic with a CPP is overcoming MDR, which frequently occurs after repeated exposure of tumor cells to the same drug.
Exemplary conjugates of anticancer drugs with CPPs and the experimental models on which they were investigated are presented in .
Table 2. Representatives of conjugates of anticancer drugs with CPPs investigated on versatile experimental models
6.1. Combinations of a chemotherapeutic with a CPP possessing additional anticancer activity
At first, attention will be focused on such combinations whose CPP constituent itself succeeded with the resultant phase I clinical trials (LTX-315 and p28). Apart from these, research on this topic comprises preclinical studies, both in vitro and in vivo. Next, other conjugates with a CPP possessing anticancer activity (R8, (sC18)2, TP10) will be shortly considered.
6.1.1. Anticancer drugs+LTX-315 and conjugates of cytotoxic chemotherapeutics with p28
Although this subsection concentrates on the CPPs conjugated with the chemotherapeutics, an exception has been made for LTX-315 peptide, which is administered not in the form of a conjugate with an anticancer drug, but separately (intratumorally) with one of the two distinct MABs (iv). As has been mentioned before, monotherapy with this CPP disintegrates cytoplasmic organelles and induces immunogenic cell death. Because of these properties, LTX-315 entered phase I clinical trials, which aimed at demonstrating the safety of the CPP itself and the potential to enhance the systemic anticancer activity of such compounds as ipilimumab and pembrolizumab.Citation115,Citation180 The results of the trials confirmed its antitumoral efficacy, also when used in combination with each of the aforementioned drugs. The response to either ipilimumab or pembrolizumab (both are immune checkpoint inhibitors, ICIs) in the presence of LTX-315 (intratumoral injection) was increased, leading to an improved prognosis in patients with melanoma or triple-negative breast cancer (NCT01986426).Citation180
Moreover, there are promising results of preclinical studies with LTX-315 (intratumoral) and doxorubicin (DOX; iv) obtained on a triple-negative breast cancer model in mice. The usage of both compounds in combination resulted in an additive anticancer effect manifested by a complete regression of the tumor in the majority of treated animals.Citation114 This additive effect together with that established for LTX-315 and ICIs has been interpreted in view of the changes in the immune system of the tumor environment induced by each constituent of the therapy. Such interaction of the peptide and ICIs could have been predicted, but rather not in the case of DOX. However, recent reports demonstrated that DOX, apart from its intercalating action, has the potential to stimulate anticancer immune responses by a selective elimination of the immunosuppressive cells and is able to induce immunogenic cell death.Citation114,Citation181,Citation182
Research on the combinations of p28 with anticancer drugs includes preclinical studies with non-covalent conjugates. This peptide after mixing with a representative of DNA-damaging (i.e. doxorubicin, dacarbazine, temozolomide) or antimitotic (i.e. paclitaxel, docetaxel) drugs was tested on a variety of cancer cells expressing wild or mutated types of p53. The experiments were performed in vitro (cell lines of myriad cancer types) and in vivo (mice of both sexes). It is worth noticing that p53 protein is inactivated or malfunctioning in about 50% of human cancers, and therefore strategies have been undertaken to restore its guardian function of the cell cycle. One of these strategies includes an experimental protocol with the above-presented p28 mixtures. Their components produced an additive effect expressed by improved efficacy and lower toxicity, as compared to those observed after each single chemotherapeutic. The potential therapeutic value of the mixtures has been further analyzed in light of the possible mechanisms.Citation84
It has been demonstrated that p28 and the tested anticancer drugs produce an increase in p53, but by utilizing distinct pathways. The CPP by attaching DNA-binding domain of this protein, blocks the E3 ligase Cop1 and thereby induces a post-translational increase in the level and activity of p53.Citation183,Citation184 By contrast, DNA damaging drugs produce this effect by activation of the ATM (Ataxia Telangiectasia Mutated protein) pathway in response to the double-strand breaks in the DNA, whereas the antimitotic agents do this via post-transcriptional modifications within the p53 protein itself. Reestablishing p53 in cancer cells, irrespective of the mechanism involved, brings about cell cycle arrest, DNA repair or apoptosis. However, the recovery of p53 function induced by chemotherapeutics is not always effective enough since the drugs secondarily trigger checkpoint signaling and initiate DNA repair pathways, including the p53-independent ones.Citation84 Their abrogation is a proper move to the improvement of the anticancer activity with a simultaneous drop in the risk of resistance. It has been found that such a phenomenon occurs if p28 is added to the chemotherapeutic. As has been stressed this CPP is a non-genotoxic specific cell cycle inhibitor at G2-M phase, which activates the p53/p21 axis significantly reducing CDK2 levels.Citation184,Citation185
6.1.2. Conjugates of cytotoxic chemotherapeutics with other CPPs possessing anticancer activity
Versatile anticancer chemotherapeutics have been conjugated with oligoarginine peptides. The conjugates mostly explored are those whose CPP component is pure R8. This CPP has been coupled with such drugs as, e.g. DOX,Citation122 paclitaxel,Citation155 bleomycin,Citation179 methotrexateCitation168 and other.Citation186 The majority of the formulations were reported to be effective in vitro as well as in vivo (tumor xenograft bearing mice), and some of them showed several other merits in comparison to the unconjugated drugs. The most important ones comprise the potential to overcome MDR and the improvement in physicochemical as well as pharmacokinetic qualities, as has been observed in the case of a paclitaxel covalent conjugate with R8. As has been demonstrated, this formulation presented higher efficacy over that of paclitaxel alone, but only against paclitaxel-resistant tumors (overexpressed P-gp efflux pumps). This quality of the conjugate became visible in vitro (lower IC50 values) on a panel of resistant ovarian and breast cancer cell lines (OVCA429T, OVCA433T, MCF7-Pgp) and in vivo (prolongation of the survival rate in mice) on an ovarian cancer mouse model.Citation155
The resistance to many chemotherapeutics, including that of paclitaxel, develops because their hydrophobic nature makes them appropriate substrates for P-gp efflux pumps.Citation187 Attachment of the drug to R8 decreases hydrophobicity in favor of hydrophilicity and thereby the conjugate is able to avoid P-gp-based resistance. Furthermore, its high aqueous solubility facilitates the administration and provides more constant concentrations (minimizing peak-trough effects) due to sustained release of the free drug from the conjugate.Citation155
The potential of R8 to improve anticancer activity was also assessed after its conjugation with DOX as a model compound. Despite its hydrophilic nature, DOX in the neutral form has the capacity to enter the intracellular compartment by itself and therefore, does not require the assistance of a CPP for this purpose. Theoretically, the response to the conjugate in DOX-sensitive cancers should be comparable to that after the free drug administration. However, the experimental data do not always confirm this assumption.
There are reports indicating an improvement of the conjugated-DOX bioactivity, but this effect was usually limited to a particular concentration/dose and/or the type of cancer cell line.Citation122,Citation130 For example, R8-DOX conjugate at the concentration of 10 μM showed higher cytotoxicity against HeLa cells in comparison to that produced by the free drug, even at the concentration of 20 μM.Citation122 Interestingly, the increased cytotoxicity was a characteristic feature of the DOX covalent formulation with R8, and not of the non-covalent one. This experimental outcome is compatible with the idea that due to covalent conjugation a new entity is established which often presents more favorable qualities than those of the free drug. What is more, the above-mentioned covalent conjugate demonstrated anticancer activity also in tumor xenografted mice. Both R8-DOX and the free drug induced the same percentage decrease in the tumor size, although the conjugate did so at a lower dose and without loss of mouse weight. The improved activity of the conjugate has been assigned to the R8-induced increase in the affinity of DOX to its targets within the cell.Citation122
Drug delivery potential together with a lytic effect on cell membranes is characteristic of (sC18)2 and TP10. Each CPP has been utilized in the form of the conjugate with standard anticancer chemotherapeutics, i.e. (sC18)2 as a covalent formulation with chlorambucilCitation81 or actinomycin D,Citation80 and TP10Citation18 as a mixture with cisplatin. The data on their action are scarce and comes from in vitro studies on diverse tumor cell lines.
For example, the conjugated form of chlorambucil or actinomycin D with (sC18)2 demonstrated evident cytotoxicity on the breast cancer (MCF7) cell line. Interestingly, the unconjugated drugs were not cytotoxic at all, and this lack of effect has been attributed to their poor cellular internalization. Undoubtedly, the transport of chlorambucil and actinomycin D into the cancer cells has been evidently improved in the presence of (sC18)2, and thereby the drugs gained access to the intracellular targets, e.g. DNA, which becomes alkylated (chlorambucil) or intercalated (actinomycin D). Whether the increase in cytotoxicity of the conjugates results exclusively from a much better entrance of the drug into the cancer cells still remains an open issue; obviously, the membrane lytic effect of the CPP component cannot be excluded.Citation80,Citation81
Similarly to the covalently conjugated drugs, the mixture of TP10 and cisplatin indicated a strong cytotoxic effect on two tumor cell lines as HeLa – cervical cancer and OS143B – osteosarcoma. Further analysis of this effect demonstrated that the magnitude of the response equals at least the sum of that produced by the CPP and the drug alone. This additive action could have been expected since TP10 and cisplatin have a distinct anticancer mechanism of action, i.e. lytic effect on the cell membrane and cytotoxicity induced by alkylation of DNA, respectively.Citation18
6.2. Other combinations of a chemotherapeutic with a CPP
At present, formulations of anticancer chemotherapeutics with CPPs that exploit passive targeting will be considered. The chosen CPPs are cationic and fall into natural (Tat, penetratin, maurocalcine (MCa), DPV1047, SynB family, Angiopep-2, LMWP, pVec) and synthetic (CADY, KRP) categories. They have been conjugated with representatives of anticancer drugs indicating diverse mechanisms of action. Their description starts with conjugates whose preclinical outcome made them eligible for clinical studies, i.e. SN38 (the active form of irinotecan)/DPV1047 and paclitaxel/Angiopep-2.
6.2.1. SN38/DPV1047 and paclitaxel/Angiopep-2 conjugates
DPV1047 is a highly charged 19 amino acid oligopeptide that partially originates from an anti-DNA antibody and is internalized via clathrin-and caveolae-independent endocytosis.Citation188 The peptide belongs to the collection of human-derived peptides denominated Vectocell. Thanks to the antibody sequence, DPV1047 can enter the cell and be transported to the nucleus.
DPV1047 has been covalently bound to SN38 via a specific esterase-sensitive cross-linker, and the product is known as DTS-108. Its significant clinical advantage is derived from the circumvention of the limitations of irinotecan which is a prodrug of SN38. Irinotecan is a topoisomerase I inhibitor, and the drug itself has a very weak intrinsic antitumor activity since its biotransformation into the active form (SN38) in humans is variable with the final yield of only 2–8% of the administered drug dose.Citation189 Also, due to the poor solubility and toxicity profile (high incidence of life-threatening diarrhea, bone marrow suppression), SN38 is unsuitable as a therapeutic.Citation190 On the other hand, its conjugation with a CPP renders the compound soluble for iv administration in purely aqueous vehicles and makes it not reliant on hepatic activation and metabolism. Instead, the conjugate linker is cleaved by the blood esterases with the resultant release of a high pool of active SN38.Citation191
The clinical trials with DTS-108 were preceded by preclinical studies estimating its efficacy and toxicokinetics on versatile models (three colon, a lung and a mammary adenocarcinomas) and species (dog, mouse, rat).Citation191 The conjugate was shown to be cytotoxic in the above-mentioned panel of cancer cell lines with IC50 values even 1000 times lower than those calculated for irinotecan. For example, IC50 of DTS-108 for LS174T colon cancer cell line was 2 nmol/L and that of irinotecan 35 μmol/L. An analysis of the amount of SN38, as a result of the conversion of the prodrugs, was performed on the basis of the experimental data obtained from the administration of DTS-108 (three different doses including maximum tolerated dose-MTD) and irinotecan (MTD) in dogs (the dog is a relevant model that mirrors the human pharmacokinetics of irinotecan). The conjugate, irrespective of the dose, always generated much bigger amounts of the active metabolite, as compared to those induced by irinotecan. It is worth stressing that the two smaller doses of DTS-108 did not produce any intestinal toxicity since a negligible amount of SN38 is present in the intestine due to the conjugate non-hepatic mode of activation and weaker liver metabolism in comparison to those of irinotecan. The modified pharmacokinetics of DTS-108 improved antitumoral efficacy, which was indicated on the nude mice or rats bearing versatile human cancer xenografts. Moreover, the conjugate produced a synergistic or an additive effect if used together with 5-fluorouracil or bevacizumab, respectively.Citation191
A phase I clinical trial comprised patients with advanced/metastatic carcinomas and its outcome has been summarized in a study delivered by Coriat et al.Citation175 Its purpose was to ascertain the dose-limiting toxicities (DLTs), MTD and the recommended Phase II dose (RP2D) in patients (male, female) with different tumor types (mostly of gastrointestinal origin) and multiple-site metastases who experienced relapse after prior chemotherapy regimen(s). DTS-108 at the RP2D (313 mg/m2) permitted four times higher SN38 concentrations during the tested time intervals than irinotecan at the equivalent dose. The objective antitumor activity was manifested by maintaining the status of the stable disease for six DTS-108 cycles or longer, and proceeded with only moderate digestive toxicity and without clinically significant hematologic toxicity.Citation175
Angiopep-2 is a 19-mer CPP derived from the family of Kunitz domain peptides. It is able to attach up to three molecules onto the peptide backbone. Its primary sequence and charge (2+) are crucial for the passage across the BBB. This peptide possesses an extraordinary potential for stimulating brain-targeted drug delivery through LRP-1-mediated transcytosis. LRP-1 is a member of the low-density lipoprotein receptor family, which is highly represented on the BBB and, more importantly, it is also over-expressed in human glioma cells.Citation149,Citation192
The chemical properties of Angiopep-2 permitted its covalent conjugation with three molecules of paclitaxel, a broad spectrum antimitotic agent. The resultant product – Ang1005 – shows superiority over paclitaxel regarding the access to the brain. By contrast, the conjugate being a prodrug (Ang1005 is cleaved by esterases to release paclitaxel) is not a substrate of drug efflux transporters (P-gp and other) and guarantees therapeutic concentrations of paclitaxel within the brain tissue. Additionally, Regina et al.Citation160 found that the conjugate with paclitaxel inhibited growth of human glioblastoma (U87 MG) more potently than paclitaxel and significantly increased mouse survival rates.
The promising outcome of the preclinical research concerning Angiopep-2/paclitaxel (ANG1005)Citation160 has brought about many clinical trials and the most encouraging are presented below.Citation161,Citation193
Kurzrock et al.Citation194 and Drappatz et al.Citation161 summarized phase I clinical trial results (NCT00539383; NCT00539344) that covered the experimental material obtained after ANG1005 (also known under the name GNR1005) treatment of patients with recurrent glioma or brain metastasis due to breast and lung cancers. In both cases, the compound was well tolerated and effective enough to initiate subsequent phases of clinical trials. Phase II comprised the usage of the conjugate and a mAb. Bevacizumab was chosen for glioma (recurrent WHO grade III) and trastuzumab for brain metastatic changes of breast cancer (NCT01967810; NCT01480582; NCT01679743). Also, an open-label ANG1005 – phase III study has started in patients with HER2-negative breast cancer with newly diagnosed leptomeningeal carcinomatosis and previously treated brain metastases (NCT03613181). The recruitment has already been finished, and the end of the study is projected for December 2022.
6.2.2. Preclinical studies of anticancer drugs with CPPs
They include research on conjugates of DOX, L-asparaginase, gemcitabine, methotrexate with the CPPs brought up in Subsection 6.2. The majority of the conjugates are covalent formulations which have been tested both in vitro and in vivo. Considering the drug component, most records concern doxorubicin. This is not surprising since this chemotherapeutic has a wide antitumor spectrum (hematological malignancies, solid tumors), compared with other anticancer drugs. Therefore, the presentation of the conjugates will start with those which possess DOX in the construct.
6.2.2.1. Conjugates of DOX with a CPP
The purpose of the preclinical studies is to get over the drawbacks of DOX, which limit its clinical usage. The most significant among them are poor BBB penetration, chemoresistance and numerous serious adverse reactions, including dose-dependent cardiotoxicity. Thus, by conjugation of DOX with myriads of CPPs, an attempt has been made to improve its pharmacological profile, especially in the context of the presented limitations. It is noteworthy that the improvement of the chemotherapeutic cellular entrance is here of minor importance since DOX very easily transfers the cell membrane. Hence, the outline of the preclinical trials will be as follows.
6.2.2.1.1. Overriding DOX resistance by its conjugation with a CPP
Overriding DOX resistance has become visible when its covalent forms with Tat, penetratin and MCa were tested on several DOX-resistant cancer cell lines.Citation136–138,Citation146,Citation147,Citation194,Citation195 At first, a brief characteristic of these CPPs follows.
The peptides are derived from human immunodeficiency virus type 1 (Tat), Antennapedia homeodomain (penetratin) and the Tunisian chactid scorpion toxin (MCa). Tat contains six arginines (therefore it is also classified into arginine-rich CPPs) and two lysine residues in the sequence that provides a total 8+ charge of the molecule. Penetratin contains three arginines and four lysisns (total charge 7+) in its molecule, and MCa is a 33-mer highly polar basic peptide containing 12 positively charged residues (seven Lys, four Arg and one Gly). Both latter peptides possess amphipathic properties.Citation40,Citation196,Citation197
The processes involved in Tat, penetratin and MCa internalizations comprise distinct types of direct translocation (inverted micelle formation, transient pore formation) and endocytosis (clathrin-mediated endocytosis, lipid raft-dependent macropinocytosis).Citation196–199
Aroui et al. tested DOX conjugates with the above presented CPPs on several cell lines with different sensitivity to DOX, i.e. human triple-negative breast adenocarcinoma – MDA-MB-231, Chinese hamster ovary – CHO, human umbilical venous endothelial cells – HUVEC, differentiated NG108.15 neuronal cells, MCF7. As could be expected, conjugation of DOX to CPPs increases the efficacy of DOX both in terms of effective concentrations and maximum effect only in resistant cell lines (MDA-MB-231, CHO, HUVEC). For instance, in the MDA-MB-231 cell line, the calculated values of EC50 with the maximum effects of DOX and the conjugates (determined at the concentration of 10 μM) are as follows: DOX – 2.7 μM/~70%, DOX-MCa – 0.32 μM/~90%, DOX-Tat – 0.25 μM/~81%, DOX-penetratin – 0.41 μM/~95%. The improvement in the activity of the conjugates has been attributed to a much higher level of accumulation of the conjugates in the resistant cell lines, as compared to free DOX. This effect does not result from an increased internalization (on the contrary, it may even decrease) but from evading the P-gp efflux pump which constitutes one of the principal mechanisms of resistance to DOX.Citation136–138,Citation146,Citation147,Citation194,Citation195
Also, the reports focus on the processes engaged in apoptotic MDA-MB-231 cell death due to treatment with DOX-CPPs conjugates. As compared to free DOX, apoptosis appears at concentrations 5 times lower and involves different signaling pathways. Apart from the BAX-dependent mitochondrial one (a characteristic feature of DOX), the conjugates trigger an additional non-mitochondrial apoptotic pathway (via TRIAL) which is intrinsically inactive in, e.g. MDA-MB 231 breast cancer cell line with TRIAL expression.Citation136–138,Citation194 Also, Zhang et al. has noticed overriding DOX-resistance by Tat-DOX conjugates, but in MDR-human cervical cancer cell line (KB-V1).Citation134
It is worth adding that DOX-sensitive cancer cell lines responded to CPP formulations only when a large amount of DOX in the construct was present (‘pop-up’ strategy with 15 wt% of DOX in multifunctional micelle with Tat).Citation139,Citation144
6.2.2.1.2. Reduction of DOX toxicity by its conjugation with a CPP
It is obvious that any targeted therapy of DOX will lead to a reduction of its global toxicity. One of them was the introduction of the liposomal form of the drug, which improved the safety profile of the chemotherapeutic. Liposomal DOX, similarly to DOX-CPP constructs, accumulates in solid tumor tissues via an enhanced EPR effect. Furthermore, due to its encapsulation within the liposome, the drug acquires different pharmacokinetic qualities, i.e. clearance and volume of distribution decrease, and half-life extends up to 72 h. Thus, Li et al.Citation152 performed a comparative analysis of pharmacological activities of three forms of DOX – the conjugated, the liposomal and the free one. The chosen CPP for conjugation with DOX was CADY-1, which is a synthetic, cationic peptide.
CADY-1 is a chimeric 24-residue secondary amphipathic peptide, which is internalized by direct translocation. Being a representative of self-assembled peptides, this CPP is capable of forming a stable complex with a drug by simple bulk mixing.Citation152,Citation200
As has been indicated in mice, the conjugate and the liposomal form of DOX possess similar blood residence time and toxicity with LD50 ca. 30 mg/kg (LD50 of free DOX ca. 17 mg/kg). However, the complex possessed higher potency and efficacy than the liposomal form or the free drug. This has been indicated on the basis of in vitro (cell viability, cell-penetrating activity) and in vivo (HeLa tumor xenografted mice) experiments. The level of the conjugate internalization was 3 times higher than that determined for the liposomal form or the free drug. The tumor xenografted mice responded with a 5-d extension of survival to CADY1-DOX complex treatment, compared to that induced by liposomal DOX.Citation152
Taking into account the characteristic of CADY-1/DOX complex, it could be regarded as a replacement for the liposomal form of DOX in future treatment. It is worth stressing that the synthesis of the CADY-1 peptide is not complicated and easy to scale up with current technology.Citation152
Also, an improvement of the pharmacological profile has been obtained in the case of covalent DOX conjugation with another synthetic, cationic CPP, i.e. KRP. This peptide is a novel lysine-rich basic CPP whose internalization involves endocytosis. Linking KRP with the drug by two stable bonds (thioether and amide) blocks the release of free DOX from the conjugate in the systemic circulation and reduces the risk of its toxic effect on normal tissues. Thanks to the latter feature, the therapeutic index of DOX increases. Additionally, the presence of two nuclear localization sequences in the KRP molecule ensures DOX a specific targeting to its site of action reflected by an augmented tumor-killing effect.Citation150
6.2.2.2. CPP as a vector for DOX transport through the BBB
An essential aspect of the CPP role in cancer treatment concerns the ability to serve as a vector for drug transport through the BBB without compromising its integrity. A vast number of anticancer drugs including DOX has poor access to the brain tissue, even though their capacity to transfer the cell membrane is high. This is caused by a high rate of active removal from the brain tissue by the efflux pumps. Bypassing these mechanisms would enable the drug to attain appropriate concentrations indispensable for the brain tumor treatment. In this context, covalent conjugates of DOX with BBB penetrable CPPs have been thoroughly evaluated with respect to the healthy brain tissue (penetratin-, SynB family-DOX conjugates), and next to the tumor transformed one (Angiopep2-DOX conjugates).
Considering the CPP component of the conjugates, the one which requires a short description is SynB family, i.e. SynB1 and SynB3 peptides (a truncated derivative of SynB1). They are derived from the porcine antimicrobial peptide – protegrin 1 and possess six (SynB1) or five (SynB3) arginines in the molecule. Their prevalent uptake mechanism is endocytosis.Citation153
Rousselle et al.Citation145,Citation153 deliver research on BBB penetration of DOX-penetratin and DOX-SynB1 conjugates performed on rats (in situ) and DOX-SynB1/SynB3 conjugates in mice (in situ, in vivo). The in situ rat and mouse brain perfusion methods indicated that vectorization of DOX brought about a 20- or 30-fold increase in the brain uptake of the conjugates, respectively. This increase was caused by the avoidance of the efflux activity of P-gp at the level of BBB. The type of transport involved in the conjugate internalization points to adsorptive-mediated endocytosis.Citation145,Citation153 Moreover, the in vivo study showed an altered tissue distribution profile with much lower concentration of the CPP-modified DOX in the heart, which could potentially reduce the cardiotoxicity concerns.Citation145
The anticancer activity of DOX (3 molecules) conjugates with Angiopep-2 have been tested on glioma U87 cell line and in mice bearing U87 glioma tumors. The in vitro study indicated a comparable cytotoxicity of the conjugate to that produced by the parent drug. On the other hand, in the in vivo experiments, the conjugate was present in the tumor implanted hemisphere in the amount two times bigger than that of DOX. Also, there was a dramatically higher BBB influx rate of the conjugate in comparison to the free drug (mouse brain perfusion method) which was ascribed to the bypass of DOX-induced efflux mechanisms. This has been further verified on Mdr-1a (-/-) knockout mice, which demonstrated a much higher brain penetration of the conjugate in comparison to that of the parent drug, implicating also other efflux pumps that limit the entry of the unconjugated compound into the brain (e.g. BCRP, ABCG2).Citation148
To increase the therapeutic result of glioma therapy, an effective option is the usage of polytherapy. With this in mind, two anticancer therapeutics – DOX and erlotinib have been loaded into dual functionalized liposomes containing on their surface a CPP (Tat or QLPVM) and transferrin (active targeting due to expression of transferrin receptors on endothelial and glioblastoma cells). However, this construct, not being a conjugate, has been added because it constitutes a very innovative targeted delivery system for a CPP and more than one drug. The construct was tested on an in vitro brain tumor model as well as in vivo and ex vivo after iv administration in mice. The experiments revealed an efficient co-transfer of DOX and erlotinib across the BBB (co-culture endothelial barrier), which led to a significant increase in DOX and erlotinib content in mice brain, as compared to the free drugs. Simultaneously, no signs of organ toxicity such as necrosis, nuclei enlargement, inflammation or diffuse fibrosis of myocardium were observed. The brain accumulation of both drugs enabled them to act more efficaciously, resulting in tumor regression, which was reflected by a significant decrease in the percentage of tumor cell viability and a higher number of dead tumor cells.Citation141
6.2.2.3. Conjugates of L-asparaginase with Tat or LMWP
As a short description of Tat has been presented previously, only that of LMWP is provided. It can be readily produced in mass quantities by enzymatic digestion of native protamine with the final result of a peptide fragment (MW: about 1.8 kDa) with 10 arginine residues. The peptide displays a significant similarity to Tat as far as the structure, transcellular localization behavior and kinetics are concerned. LMWP efficiently transfers the cargo into the nucleus and cytoplasm in a short time period.Citation201
Tat and LMWP have been covalently conjugated with L-asparaginase, which is the primary drug for the treatment of acute lymphoblastic leukemia (ALL). Each of the conjugates constitutes a component of a complex construct, i.e. the Tat conjugate of heparin/protamine regulated delivery system known as ATTEMPTS,Citation172 and the LMWP conjugate of the encapsulated red blood cell (RBC) carrier system.Citation171 These strategies aim at reducing the pitfalls of L-asparaginase treatment (immunological reactions, liver dysfunctions and other toxicities, protection from proteolytic degradation and metabolic clearance).
The primary significance of the ATTEMPTS method lies in its capability of allowing only the tumor cells to carry their self-destructing agent, i.e. the cellularly delivered asparaginase by Tat. By this means the cancer cells are deprived of asparagine, while its nearly normal concentration is maintained in the circulation. What is more, thanks to this approach, a higher efficacy (leukemia MOLT-4 cell line) and a prolonged mean survival time (leukemia bearing mice) have been achieved in comparison to those of the free drug.Citation172
As regards the LMWP-mediated RBC encapsulation of asparaginase, this method ensures on the one hand, retention of the complete structural and functional integrity of the erythrocytes, which may serve as a drug reservoir, and, on the other, protection of the loaded drug against the physiological environment. Thus, the pharmacokinetic and pharmacodynamic parameters of asparaginase have been changed with resultant prolongation of its plasma half-life (4.5 ± 0.5 d whereas that of RBCs loaded with asparaginase via a hypotonic method was 2.4 ± 0.7 d), safety of iv usage (erythrocytes help avoiding immune response toward the encapsulated drugs), increase in efficacy with the median survival time of the lymphoma tumor bearing mice by ca. 44% in comparison to the control group.Citation171
6.2.2.4. Conjugates of cytotoxic antimetabolites with CPPs
The conjugates taken into account comprise gemcitabine+pVEC, gemcitabine+penetratin, and methotrexate+penetratin. pVEC, being a peptide of 18 amino acids, is derived from the cadherin murine vascular endothelium. It enters the cell by direct and endocytic mechanisms of internalization.Citation202,Citation203
Gemcitabine is an antimetabolite of pyrimidine nucleosides, which is used in various types of solid tumors comprising first-line treatment of pancreatic, metastatic bladder or non-small cell lung cancers. One of the drawbacks is its poor pharmacokinetic profile including hydrophilicity, low oral bioavailability, transporter dependent cellular uptake (nucleoside transporter deficiency is related to different forms of drug resistance) and rapid inactivation by cytidine deaminase in plasma and liver. In order to diminish the process of inactivation, gemcitabine has been conjugated with pVEC or penetratin. Conjugation of the drug with the CPP masks its aniline moiety, which results in higher availability of gemcitabine for cellular internalization, facilitated additionally by the presence of the peptide. What is more, both gemcitabine conjugates acquired prolonged half-lives (9.6 d-gemcitabine/penetratin or 42 h-gemcitabine/pVEC) and enhanced antitumor activity, which was determined on three human cancer cell lines (KN-28-gastric cancer, Caco-2 – colorectal adenocarcinoma and HT-29 – colon cancer).Citation169
Methotrexate (MTX) is an effective anticancer drug which is widely used in several types of solid tumors as well as hematological malignancies. As a folic acid analogue, it inhibits dihydrofolate reductase and, by this means, the synthesis of tetrahydrofolate. The latter one is a key factor involved in the production of thymidylate and purine nucleotides, thereby interfering with the formation of DNA and RNA that finally results in cell death. Inside the cell, MTX undergoes polyglutamation by folylpolyglutamate synthetase (FPGS), and this process is crucial for the therapeutic action. Polyglutamylated forms of the drug retain within the cancer cells and determine the cytotoxic action of this chemotherapeutic. Furthermore, their decreased formation is one of the mechanisms responsible for MTX resistance.
The process of cellular polyglutamylation is not always efficient enough, and even absent in resistant tumor cells which leads to a dramatic drop in the therapeutic activity of MTX. To overcome this unfortunate impediment, Szabo et al.Citation168 undertook a strategy with a “ready-made” pentaglutamylated MTX coupled covalently to penetratin. The presence of the CPP was indispensable for the cellular entrance of this form of drug.
The conjugates were tested in vitro (cellular uptake and cytotoxicity profiles) on MCF7-sensitive or MDA-MB-231-resistant breast cancer cell lines. As could have been expected, the pentaglutamylated MTX–penetratin conjugate indicated activity exclusively against drug-resistant MDA-MB-231 cells, and the efficacy was higher than that of the free MTX on sensitive cells. The cytotoxicity on this resistant cell line, expressed by the IC50 value, was 0.1 μM (IC50 of MTX >100).Citation168
Generally, there is no direct correlation between the degree of internalization and activity. Despite the high efficacy of the pentaglutamylated MTX–penetratin conjugate, its uptake in both MCF7 and MDA-MB-231 cell lines was smaller compared with that of non-glutamylated form of the conjugate. The reason for this is an electrostatic interaction between the anionic (mainly glutamic acid residues) and cationic (arginine residues) domains within the construct. Introducing a spacer (tetrapeptide) between these domains attenuates the interaction, resulting in improved cellular internalization. It is intriguing that the pentaglutamylated MTX–penetratin conjugate equipped with such a spacer revealed cytotoxic activity also on MTX-sensitive cells (IC50 = 0.3 μM).Citation168
7. Conclusions
Concerning CPPs
As potential vectors for cellular delivery of small molecule drugs, they indicate a certain level of selectivity to cancer cells, called passive selectivity.
Besides drug transporting activity, certain peptides possess anticancer activity per se, accomplished mainly by membrane lytic effect, proapoptotic activity, or both actions.
Among the anticancer peptides, the most promising are p28 and LTX-315. Of great interest is particularly the latter one, the first locally acting oncolytic agent that reorganizes the tumor microenvironment. It entered several settings of phase I and II clinical trials.
Concerning combinations of anticancer drugs with CPPs
The research includes preclinical studies carried out both in vitro (versatile cancer cell lines) and in vivo (usually tumor xenograft bearing mice). They indicated an improved pharmacologic profile of the conjugates in comparison to the unconjugated drugs. It concerned mainly better cellular internalization (in case a drug showed a poor one) and circumvention of tissue barriers (e.g. access to the brain tissue), overcoming drug resistance and lowering toxicity. These qualities of the conjugates brought about superior anticancer activity over that of the anticancer drugs alone. Most records concern conjugates of DOX with a CPP.
A few preclinical studies were the basis for entering clinical trials. The first phase entered four entities: LTX 315+ ipilimumab, LTX-315+ pembrolizumab as well as two conjugates, i.e. DTS-108 and Ang1005. The trials with the latter one comprise also phase II and the unfinished phase III. So far, their outcome has been favorable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Varnamkhasti BS, Jafari S, Taghavi F, Alaei L, Izadi Z, Lotfabadi A, Dehghanian M, Jaymand M, Derakhshankhah H, Saboury AA. Cell-penetrating peptides: as a promising theranostics strategy to circumvent the blood-brain barrier for CNS diseases. Curr Drug Deliv. 2020;17(5):35–63. doi:https://doi.org/10.2174/1567201817666200415111755.
- Yeste J, Illa X, Alvarez M, Villa R. Engineering and monitoring cellular barrier models. J Biol Eng. 2018;12(1):18. doi:https://doi.org/10.1186/s13036-018-0108-5.
- Khafagy ES, Morishita M. Oral biodrug delivery using cell-penetrating peptide. Adv Drug Deliv Rev. 2012;64(6):531–539. doi:https://doi.org/10.1016/j.addr.2011.12.014.
- Zou LL, Ma JL, Wang T, Yang TB, Liu CB. Cell-penetrating peptide-mediated therapeutic molecule delivery into the central nervous system. Curr Neuropharmacol. 2013;11(2):197–208. doi:https://doi.org/10.2174/1570159X11311020006.
- Bernardes N, Fialho AM. Perturbing the dynamics and organization of cell membrane components: a new paradigm for cancer-targeted therapies. Int J Mol Sci. 2018;19(12):3871. doi:https://doi.org/10.3390/ijms19123871.
- Afratis N, Gialeli C, Nikitovic D, Tsegenidis T, Karousou E, Theocharis AD, Pavão MS, Tzanakakis GN, Karamanos NK. Glycosaminoglycans: key players in cancer cell biology and treatment. The FEBS J. 2012;279(7):1177–1197. doi:https://doi.org/10.1111/j.1742-4658.2012.08529.x.
- Jobin M-L, Alves ID. On the importance of electrostatic interactions between cell penetrating peptides and membranes: a pathway toward tumor cell selectivity? Biochimie. 2014;107:154–159. doi:https://doi.org/10.1016/j.biochi.2014.07.022.
- Nikitovic D, Berdiaki A, Spyridaki I, Krasanakis T, Tsatsakis A, Tzanakakis GN. Proteoglycans-Biomarkers and targets in cancer therapy. Front Endocrinol. 2018;9:69. https://doi.org/https://doi.org/10.3389/fendo.2018.00069.
- Shin MC, Zhang J, Min KA, Lee K, Byun Y, David AE, He H, Yang VC. Cell-penetrating peptides: achievements and challenges in application for cancer treatment. J Biomed Mater Res A. 2014;102(2):575–587. doi:https://doi.org/10.1002/jbm.a.34859.
- Shin MC, Zhang J, Min KA, He H, David AE, Huang Y, Yang VC. PTD-modified ATTEMPTS for enhanced toxin-based cancer therapy: an in vivo proof-of-concept study. Pharm Res. 2015;32:2690–2703. doi:https://doi.org/10.1007/s11095-015-1653-y.
- Kalyane D, Raval N, Maheshwari R, Tambe V, Kalia K, Tekade RK. Employment of enhanced permeability and retention effect (EPR): nanoparticle-based precision tools for targeting of therapeutic and diagnostic agent in cancer. Mater Sci Eng C. 2019;98:1252–1276. doi:https://doi.org/10.1016/j.msec.2019.01.066.
- Duncan R. Polymer therapeutics: top 10 selling pharmaceuticals - what next? JCR. 2014;190:371–380. doi:https://doi.org/10.1016/j.jconrel.2014.05.001.
- Yin H, Liao L, Fang J. Enhanced Permeability and Retention (EPR) effect based tumor targeting: the concept, application and prospect. JSM Clin Oncol Res. 2014;2:1010. doi:https://doi.org/10.5497/wjp.v4.i2.168.
- Vicent MJ, Ringsdorf H, Duncan R. Polymer therapeutics: clinical applications and challenges for development. Adv Drug Deliv Rev. 2009;61(13):1117–1120. doi:https://doi.org/10.1016/j.addr.2009.08.001.
- Torchilin V. Tumor delivery of macromolecular drugs based on the EPR effect. Adv Drug Deliv Rev. 2011;63(3):131–135. doi:https://doi.org/10.1016/j.addr.2010.03.011.
- Maeda H. Maeda Polymer therapeutics and the EPR effect. J Drug Target. 2017;25(9–10):781–785. doi:https://doi.org/10.1080/1061186X.2017.1365878.
- Fang B, Jiang L, Zhang M, Ren FZ. A novel cell-penetrating peptide TAT-A1 delivers siRNA into tumor cells selectively. Biochimie. 2013;95(2):251–257. doi:https://doi.org/10.1016/j.biochi.2012.09.020.
- Rusiecka I, Ruczyński J, Alenowicz M, Rekowski P, Kocić, I. Transportan 10 improves the anticancer activity of cisplatin. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2016;389:485–497. doi:https://doi.org/10.1007/s00210-016-1219-5.
- Rusiecka I, Ruczyński J, Kozłowska A, Backtrog E, Mucha P, Kocić I, Rekowski P. TP10-Dopamine conjugate as a potential therapeutic agent in the treatment of parkinson’s disease. Bioconjug Chem. 2019;30(3):760–774. doi:https://doi.org/10.1021/acs.bioconjchem.8b00894.
- Ruczyński J, Rusiecka I, Turecka K, Kozłowska A, Alenowicz M, Gągało I, Kawiak A, Rekowski P, Waleron K, Kocić I. Transportan 10 improves the pharmacokinetics and pharmacodynamics of vancomycin. Sci Rep. 2019;9(1):3247. doi:https://doi.org/10.1038/s41598-019-40103-w.
- Zhang H, Zhao Q, Bhattacharya S, Waheed AA, Tong X, Hong A, Heck S, Curreli F, Goger M, Cowburn D, et al. A cell-penetrating helical peptide as a potential HIV-1 inhibitor. J Mol Biol. 2008;378(3):565–580. doi:https://doi.org/10.1016/j.jmb.2008.02.066.
- Xie J, Gou Y, Zhao Q, Li S, Zhang W, Song J, Mou L, Li J, Wang K, Zhang B, et al. Antimicrobial activities and action mechanism studies of transportan 10 and its analogues against multidrug-resistant bacteria. J Peptide Sci. 2015;21(7):599–607. doi:https://doi.org/10.1002/psc.2781.
- Gomarasca M, Martins TFC, Greune L, Hardwidge PR, Schmidt MA, Rüter C. Bacterium-Derived cell-penetrating peptides deliver gentamicin to kill intracellular pathogens. Antimicrob Agents Chemother. 2017;61(4):e02545–e02616. doi:https://doi.org/10.1128/AAC.02545-16.
- Bárány-Wallje E, Andersson A, Gräslund A, Mäler L. NMR solution structure and position of transportation in neutral phospholipid bicelles. FEBS Lett. 2004;567(2–3):265–269. doi:https://doi.org/10.1016/j.febslet.2004.04.079.
- Eriksson OS, Geörg M, Sjölinder H, Sillard R, Lindberg S, Langel Ü, Jonsson AB. Identification of cell-penetrating peptides that are bactericidal to Neisseria meningitidis and prevent inflammatory responses upon infection. Antimicrob Agents Chemother. 2013;57(8):3704–3712. doi:https://doi.org/10.1128/AAC.00624-13.
- Xu J, Xu B, Shou D, Xia X, Hu Y. Preparation and evaluation of vancomycin-loaded n-trimethyl chitosan nanoparticles. Polymers. 2015;7(9):1850–1870. doi:https://doi.org/10.3390/polym7091488.
- Jafari S, Dizaj SM, Adibkia K. Cell-penetrating peptides and their analogues as novel nanocarriers for drug delivery. BioImpacts. 2015;5(2):103–111. doi:https://doi.org/10.15171/bi.2015.10.
- Xie J, Bi Y, Zhang H, Dong S, Teng L, Lee RJ, Yang Z. Cell-Penetrating peptides in diagnosis and treatment of human diseases: from preclinical research to clinical application. Front Pharmacol. 2020;11:697. doi:https://doi.org/10.3389/fphar.2020.00697.
- Guidotti G, Brambilla L, Rossi D. Cell-Penetrating peptides: from basic research to clinics. Trends Pharmacol Sci. 2017;38(4):406–424. doi:https://doi.org/10.1016/j.tips.2017.01.003.
- Ruseska I, Zimmer A. Internalization mechanisms of cell-penetrating peptides. Beilstein J Nanotechnol. 2020;11:101–123. https://doi.org/https://doi.org/10.3762/bjnano.11.10.
- Ashrafuzzaman M. Nanoscale biophysics of the cell, first ed. ed. Springer; Heidelberg, Germany,2018
- Martín I, Teixidó M, Giralt E. Design, synthesis and characterization of a new anionic cell-penetrating peptide: SAP(E). Chembiochem: A European Journal of Chemical Biology. 2011;12(6):896–903. doi:https://doi.org/10.1002/cbic.201000679.
- Taylor BN, Mehta RR, Yamada T, Lekmine F, Christov K, Chakrabarty AM, Green A, Bratescu L, Shilkaitis A, Beattie CW, et al. Noncationic peptides obtained from azurin preferentially enter cancer cells. Cancer Res. 2009;69(2):537–546. doi:https://doi.org/10.1158/0008-5472.CAN-08-2932.
- Abuei H, Behbahani AB, Dehbidi GR, Pirouzfar M, Zare F, Farhadi A. Construction, expression, and purification of p28 as a cell-penetrating peptide with anticancer effects on Burkitt’s lymphoma cell line. SEMJ. 2019;20:e85190. doi:https://doi.org/10.5812/semj.85190.
- Yaghoubi A, Khazaei M, Avan A, Hasanian SM, Cho WC, Soleimanpour S. p28 bacterial peptide, as an anticancer agent. Front Oncol. 2020;10:1303. https://doi.org/https://doi.org/10.3389/fonc.2020.01303.
- Delaroche D, Cantrelle FX, Subra F, Van Heijenoort C, Guittet E, Jiao CY, Blanchoin L, Chassaing G, Lavielle S, Auclair C, et al. Cell-penetrating peptides with intracellular actin-remodeling activity in malignant fibroblasts. J Biol Chem. 2010;5(10):7712–7721. doi:https://doi.org/10.1074/jbc.M109.045872.
- Franz J, Lelle M, Peneva K, Bonn M, Weidner T. SAP(E) - A cell-penetrating polyproline helix at lipid interfaces. Biochim Biophys Acta. 2016;1858(9):2028–2034. doi:https://doi.org/10.1016/j.bbamem.2016.05.021.
- Martín I, Teixidó M, Giralt E. Design, synthesis and characterization of a new anionic cell-penetrating peptide: SAP(E). Chembiochem. 2011;12(6):896–903. doi:https://doi.org/10.1002/cbic.201000679.
- Tripathi PP, Arami H, Banga I, Gupta J, Gandhi S. Cell penetrating peptides in preclinical and clinical cancer diagnosis and therapy. Oncotarget. 2018;9(98):37252–37267. doi:https://doi.org/10.18632/oncotarget.26442.
- Madani F, Lindberg S, Langel Ü, Futaki S, Gräslund A. Mechanisms of cellular uptake of cell-penetrating peptides. J Biophys. 2011;2011:414729. https://doi.org/https://doi.org/10.1155/2011/414729.
- Lindgren M, Hällbrink M, Prochiantz A, Langel Ü. Cell-penetrating peptides. TIPS. 2000;21:99–103. doi:https://doi.org/10.1016/S0165-6147(00)01447-4.
- Ramsey JD, Flynn NH. Cell-penetrating peptides transport therapeutics into cells. Pharmacol Ther. 2015;154:78–86. https://doi.org/https://doi.org/10.1016/j.pharmthera.2015.07.003.
- Mishra A, Gordon V, Yang L, Coridan R, Wong G. HIV TAT forms pores in membranes by inducing saddle-splay curvature: potential role of bidentate hydrogen bonding. Angew Chem Int Ed Engl. 2008;47(16):2986–2989. doi:https://doi.org/10.1002/anie.200704444.
- Mishra A, Lai GH, Schmidt NW, Sun VZ, Rodriguez AR, Tong R, Tang L, Cheng J, Deming TJ, Kamei DT, et al. Translocation of HIV TAT peptide and analogues induced by multiplexed membrane and cytoskeletal interactions. Proc Natl Acad Sci USA. 2011;108(41):16883–16888. doi:https://doi.org/10.1073/pnas.1108795108.
- Ciobanasu C, Siebrasse JP, Kubitscheck U. Cell-penetrating HIV1 TAT peptides can generate pores in model membranes. Biophys J. 2010;99(1):153–162. doi:https://doi.org/10.1016/j.bpj.2010.03.065.
- Berlose JP, Convert O, Derossi D, Brunissen A, Chassaing G. Conformational and associative behaviours of the third helix of antennapedia homeodomain in membrane-mimetic environments. Eur J Biochem. 1996;242(2):372–386. doi:https://doi.org/10.1111/j.1432-1033.1996.0372r.x.
- Kawamoto S, Takasu M, Miyakawa T, Morikawa R, Oda T, Futaki S, Nagao H. Inverted micelle formation of cell-penetrating peptide studied by coarse-grained simulation: importance of attractive force between cell-penetrating peptides and lipid head group. J Chem Phys. 2011;134(9):095103. doi:https://doi.org/10.1063/1.3555531.
- Islam MZ, Sharmin S, Levadnyy V, Alam Shibly SU, Yamazaki M. Effects of mechanical properties of lipid bilayers on the entry of cell-penetrating peptides into single vesicles. Langmuir. 2017;33(9):2433–2443. doi:https://doi.org/10.1021/acs.langmuir.6b03111.
- Islam MZ, Sharmin S, Moniruzzaman M, Yamazaki M. Elementary processes for the entry of cell-penetrating peptides into lipid bilayer vesicles and bacterial cells. Appl Microbiol Biotechnol. 2018;102(9):3879–3892. doi:https://doi.org/10.1007/s00253-018-8889-5.
- Sharmin S, Islam MZ, Karal MA, Shibly SUA, Dohra H, Yamazaki M. Effects of lipid composition on the entry of cell-penetrating peptide oligoarginine into single vesicles . Biochem. 2016;55(30):4154–4165. doi:https://doi.org/10.1021/acs.biochem.6b00189.
- Hasan M, Moghal MMR, Saha SK, Yamazaki M. The role of membrane tension in the action of antimicrobial peptides and cell-penetrating peptides in biomembranes. Biophys Rev. 2019;11(3):431–448. doi:https://doi.org/10.1007/s12551-019-00542-1.
- Choi YS, David AE. Cell penetrating peptides and the mechanisms for intracellular entry. Curr Pharm Biotechnol. 2014;15(3):192–199. doi:https://doi.org/10.2174/1389201015666140617093331.
- Lindgren M, Langel Ü. Classes and prediction of cell-penetrating peptides. Methods Mol Biol. 2011;683:3–19. https://doi.org/https://doi.org/10.1007/978-1-60761-919-2_1.
- Magzoub M, Kilk K, Eriksson LE, Langel Ü, Gräslund A. Interaction and structure induction of cell-penetrating peptides in the presence of phospholipid vesicles. Biochim Biophys Acta. 2001;1512(1):77–89. doi:https://doi.org/10.1016/s0005-2736(01)00304-2.
- Allolio C, Magarkar A, Jurkiewicz P, Baxová K, Javanainen M, Mason PE, Šachl R, Cebecauer M, Hof M, Horinek D, et al. Arginine-rich cell-penetrating peptides induce membrane multilamellarity and subsequently enter via formation of a fusion pore. Proc Natl Acad Sci USA. 2018;115(47):11923–11928. doi:https://doi.org/10.1073/pnas.1811520115.
- Duchardt F, Fotin-Mleczek M, Schwarz H, Fischer R, Brock R. A comprehensive model for the cellular uptake of cationic cell-penetrating peptides. Traffic. 2007;8(7):848–866. doi:https://doi.org/10.1111/j.1600-0854.2007.00572.x.
- Bernardes N, Fialho AM. Perturbing the dynamics and organization of cell membrane components: a new paradigm for cancer-targeted therapies. Int J Mol Sci. 2018;19(12):3871. doi:https://doi.org/10.3390/ijms19123871.
- Bernardes N, Garizo AR, Pinto SN, Caniço B, Perdigão C, Fernandes F, Fialho AM. Azurin interaction with the lipid raft components ganglioside GM-1 and caveolin-1 increases membrane fluidity and sensitivity to anti-cancer drugs. Cell Cycle. 2018;17(13):1649–1666. doi:https://doi.org/10.1080/15384101.2018.1489178.
- Fonseca SB, Pereira MP, Kelley SO. Recent advances in the use of cell-penetrating peptides for medical and biological applications. Adv Drug Deliv Rev. 2009;61(11):953–964. doi:https://doi.org/10.1016/j.addr.2009.06.001.
- Zaro JL, Vekich JE, Tran T, Shen WC. Nuclear localization of cell-penetrating peptides is dependent on endocytosis rather than cytosolic delivery in CHO cells. Mol Pharm. 2009;6(2):337–344. doi:https://doi.org/10.1021/mp800239p.
- Horton KL, Stewart KM, Fonseca SB, Guo Q, Kelley SO. Mitochondria-penetrating peptides. Chem Biol. 2008;15(4):375–382. doi:https://doi.org/10.1016/j.chembiol.2008.03.015.
- Yamada Y, Satrialdi RM, Sakurai Y, Sakurai Y, Sakurai Y, Harashima H, Harashima H. Mitochondrial delivery of an anticancer drug via systemic administration using a mitochondrial delivery system that inhibits the growth of drug-resistant cancer engrafted on mice. J Pharm Sci. 2020;109(8):2493–2500. doi:https://doi.org/10.1016/j.xphs.2020.04.020.
- Yamada Y, Akita H, Kamiya H, Kogure K, Yamamoto T, Shinohara Y, Yamashita K, Kobayashi H, Kikuchi H, Harashima H. MITO-Porter: a liposome-based carrier system for delivery of macromolecules into mitochondria via membrane fusion. Biochim et Biophys Acta. 2008;1778(2):423–432. doi:https://doi.org/10.1016/j.bbamem.2007.11.002.
- Zalba S, Ten Hagen TL. Cell membrane modulation as adjuvant in cancer therapy. Cancer Treat Rev. 2017;52:48–57. https://doi.org/https://doi.org/10.1016/j.ctrv.2016.10.008.
- Tan LT, Chan KG, Pusparajah P, Lee WL, Chuah LH, Khan TM, Lee LH, Goh BH. Targeting membrane lipid a potential cancer cure? Front. Pharmacol. 2017;8:12. doi:https://doi.org/10.3389/fphar.2017.00012.
- Kondo E, Saito K, Tashiro Y, Kamide K, Uno S, Furuya T, Mashita M, Nakajima K, Tsumuraya T, Kobayashi N, et al. Tumour lineage-homing cell-penetrating peptides as anticancer molecular delivery systems. Nature Communications. 2012;3(1):951. doi:https://doi.org/10.1038/ncomms1952.
- Borrelli A, Tornesello AL, Tornesello ML, Buonaguro FM. Cell penetrating peptides as molecular carriers for anti-cancer agents. Molecules. 2018;23(2):295. doi:https://doi.org/10.3390/molecules23020295.
- Parker N, Turk MJ, Westrick E, Lewis JD, Low PS, Leamon CP. Folate receptor expression in carcinomas and normal tissues determined by a quantitative radioligand binding assay. Anal Biochem. 2005;338(2):284–293. doi:https://doi.org/10.1016/j.ab.2004.12.026.
- Meng F, Sun Y, Lee RJ, Wang G, Zheng X, Zhang H, Fu Y, Yan G, Wang Y, Deng W, et al. Folate receptor-targeted albumin nanoparticles based on microfluidic technology to deliver cabazitaxel. Cancers (Basel). 2019;11(10):1571. doi:https://doi.org/10.3390/cancers11101571.
- Xie J, Teng L, Yang Z, Zhou C, Liu Y, Yung BC, Lee RJ. A polyethylenimine-linoleic acid conjugate for antisense oligonucleotide delivery. Biomed Res Int. 2013;2013:710502. https://doi.org/https://doi.org/10.1155/2013/710502.
- Xie J, Yang Z, Zhou C, Zhu J, Lee RJ, Teng L. Nanotechnology for the delivery of phytochemicals in cancer therapy. Biotechnol Adv. 2016;34(4):343–353. doi:https://doi.org/10.1016/j.biotechadv.2016.04.002.
- Yang Z, Yu B, Zhu J, Huang X, Xie J, Xu S, Yang X, Wang X, Yung BC, Lee LJ, et al. A microfluidic method to synthesize transferrin-lipid nanoparticles loaded with siRNA LOR-1284 for therapy of acute myeloid leukemia. Nanoscale. 2014;6(16):9742–9751. doi:https://doi.org/10.1039/C4NR01510J.
- Yang X, Yang S, Chai H, Yang Z, Lee RJ, Liao W, Teng L, Novel Isoquinoline A, Seno M. Derivative anticancer agent and its targeted delivery to tumor cells using transferrin-conjugated liposomes. PLoS One. 2015;10(8):e0136649. doi:https://doi.org/10.1371/journal.pone.0136649.
- Zhou C, Yang Z, Teng L. Nanomedicine based on nucleic acids: pharmacokinetic and pharmacodynamic perspectives. Curr Pharm Biotechnol. 2014;15(9):829–838. doi:https://doi.org/10.2174/1389201015666141020155620.
- Raucher D, Ryu JS. Cell-penetrating peptides: strategies for anticancer treatment. Trends Mol Med. 2015;21(9):560–570. doi:https://doi.org/10.1016/j.molmed.2015.06.005.
- Habault J, Poyet JL. Recent advances in cell penetrating peptide-based anticancer therapies. Molecules. 2019;24(5):927. doi:https://doi.org/10.3390/molecules24050927.
- Shi NQ, Qi XR, Xiang B, Zhang Y. A survey on “Trojan Horse” peptides: opportunities, issues and controlled entry to “Troy”. J Control Release. 2014;194:53–70. doi:https://doi.org/10.1016/j.jconrel.2014.08.014.
- Tang H, Su ZD, Wei HH, Chen W, Lin H. Prediction of cell-penetrating peptides with feature selection techniques. Biochem. Biophys Res Commun. 2016;477(1):150–154. doi:https://doi.org/10.1016/j.bbrc.2016.06.035.
- Savariar EN, Felsen CN, Nashi N, Jiang T, Ellies LG, Steinbach P, Tsien RY, Nguyen QT. Real-time in vivo molecular detection of primary tumors and metastases with ratiometric activatable cell-penetrating peptides. Cancer Res. 2013;73(2):855–864. doi:https://doi.org/10.1158/0008-5472.CAN-12-2969.
- Gronewold A, Horn M, Ranđelović I, Tóvári J, Vázquez SM, Schomäcker K, Neundorf I. Characterization of a cell-penetrating peptide with potential anticancer activity. Chem Med Chem. 2017;12(1):42–49. doi:https://doi.org/10.1002/cmdc.201600498.
- Hoyer J, Schatzschneider U, Schulz-Siegmund M, Neundorf I. Dimerization of a cell-penetrating peptide leads to enhanced cellular uptake and drug delivery. Beilstein J Org Chem. 2012;8:1788–1797. doi:https://doi.org/10.3762/bjoc.8.204.
- Mehta RR, Yamada T, Taylor BN, Christov K, King ML, Majumdar D, Lekmine F, Tiruppathi C, Shilkaitis A, Bratescu L, et al. A cell penetrating peptide derived from azurin inhibits angiogenesis and tumor growth by inhibiting phosphorylation of VEGFR-2. FAK and Akt Angiogenesis. 2011;14(3):355–369. doi:https://doi.org/10.1007/s10456-011-9220-6.
- Jia L, Gorman GS, Coward LU, Noker PE, McCormick D, Horn TL, Harder JB, Muzzio M, Prabhakar B, Ganesh B, et al. Preclinical pharmacokinetics, metabolism, and toxicity of azurin-p28 (NSC745104) a peptide inhibitor of p53 ubiquitination. Cancer Chemother. Pharmacol. 2011;68:513–524. https://doi.org/https://doi.org/10.1007/s00280-010-1518-3.
- Yamada T, Gupta TKD, Beattie CW. p28-Mediated activation of p53 in G2–M phase of the cell cycle enhances the efficacy of DNA damaging and antimitotic chemotherapy. Cancer Res. 2016;76(8):2354–2365. doi:https://doi.org/10.1158/0008-5472.CAN-15-2355.
- Lee HS, Park CB, Kim JM, Jang SA, Park IY, Kim MS, Cho JH, Kim SC. Mechanism of anticancer activity of buforin IIb, a histone H2A-derived peptide. Cancer Lett. 2008;271(1):47–55. doi:https://doi.org/10.1016/j.canlet.2008.05.041.
- Lim KJ, Sung BH, Shin JR, Lee YW, Kim DJ, Yang KS, Kim SC, Sobol RW. A cancer specific cell-penetrating peptide, BR2, for the efficient delivery of an scFv into cancer cells. PLoS One. 2013;8(6):e66084. doi:https://doi.org/10.1371/journal.pone.0066084.
- Yoo YC, Watanabe S, Watanabe R, Hata K, Shimazaki K, Azuma I. Bovine lactoferrin and lactoferricin, a peptide derived from bovine lactoferrin, inhibit tumor metastasis in mice. Jpn J Cancer Res. 1997;88(2):184–190. doi:https://doi.org/10.1111/j.1349-7006.1997.tb00364.x.
- Mader JS, Salsman J, Conrad DM, Hoskin DW. Bovine lactoferricin selectively induces apoptosis in human leukemia and carcinoma cell lines. Mol Cancer Ther. 2005;4(4):612–624. doi:https://doi.org/10.1158/1535-7163.MCT-04-0077.
- Solarte VA, Conget P, Vernot JP, Rosas JE, Rivera ZJ, García JE, Arango-Rodríguez ML, Ahmad A. A tetrameric peptide derived from bovine lactoferricin as a potential therapeutic tool for oral squamous cell carcinoma: a preclinical model. PLoS One. 2017;12(3):e0174707. doi:https://doi.org/10.1371/journal.pone.0174707.
- Guerra JR, Cárdenas AB, Ochoa-Zarzosa A, Meza JL, Umaña Pérez YA, Fierro-Medina R, Rivera Monroy ZJ, García Castañeda JE. The tetrameric peptide LfcinB (20–25) 4 derived from bovine lactoferricin induces apoptosis in the MCF-7 breast cancer cell line. RSC Adv. 2019;9(36):20497–20504. doi:https://doi.org/10.1039/C9RA04145A.
- Vargas Casanova Y, Rodríguez Guerra JA, Umaña Pérez YA, Leal Castro AL, Almanzar Reina G, García Castañeda JE, Rivera Monroy ZJ. Antibacterial synthetic peptides derived from bovine lactoferricin exhibit cytotoxic effect against MDA-MB-468 and MDA-MB-231 breast cancer cell lines. Molecules. 2017;22(10):1641. doi:https://doi.org/10.3390/molecules22101641.
- Liao HW, Garris C, Pfirschke C, Rickelt S, Arlauckas S, Siwicki M, Kohler RH, Weissleder R, Sundvold-Gjerstad V, Sveinbjørnsson B, et al. LTX-315 sequentially promotes lymphocyte-independent and lymphocyte-dependent antitumor effects. Cell Stress. 2019;3(11):348–360. doi:https://doi.org/10.15698/cst2019.11.204.
- Zhou H, Forveille S, Sauvat A, Yamazaki T, Senovilla L, Ma Y, Liu P, Yang H, Bezu L, Müller K, et al. The oncolytic peptide LTX-315 triggers immunogenic cell death. Cell Death Dis. 2016;7(3):e2134. doi:https://doi.org/10.1038/cddis.2016.47.
- Camilio KA, Berge G, Ravuri CS, Rekdal O, Sveinbjørnsson B. Complete regression and systemic protective immune responses obtained in B16 melanomas after treatment with LTX-315. Cancer immunol. Immunother. 2014;63(6):601–613. doi:https://doi.org/10.1007/s00262-014-1540-0.
- Nestvold J, Wang MY, Camilio KA, Zinöcker S, Tjelle TE, Lindberg A, Haug BE, Kvalheim G, Sveinbjørnsson B, Rekdal Ø. Oncolytic peptide LTX-315 induces an immune-mediated abscopal effect in a rat sarcoma model. Oncoimmunology. 2017;6(8):e1338236. doi:https://doi.org/10.1080/2162402X.2017.1338236.
- Forveille S, Zhou H, Sauvat A, Bezu L, Müller K, Liu P, Zitvogel L, Pierron G, Rekdal Ø, Kepp O, et al. The oncolytic peptide LTX-315 triggers necrotic cell death. Cell Cycle. 2015;14(21):3506–3512. doi:https://doi.org/10.1080/15384101.2015.1093710.
- Moghal MMR, Islam MZ, Sharmin S, Levadnyy V, Moniruzzaman M, Yamazaki M. Continuous detection of entry of cell-penetrating peptide transportan 10 into single vesicles. Chem Phys Lipids. 2018;212:120–129. https://doi.org/https://doi.org/10.1016/j.chemphyslip.2018.02.001.
- Moghal MMR, Islam MZ, Hossain F, Saha SK, Yamazaki M. Role of membrane potential on entry of cell-penetrating peptide transportan 10 into single vesicles. Biophys J. 2020;118(1):57–69. doi:https://doi.org/10.1016/j.bpj.2019.11.012.
- Moghal MMR, Hossain F, Yamazak M. Action of antimicrobial peptides and cell-penetrating peptides on membrane potential revealed by the single GUV method. Biophys Rev. 2020;12(2):339–348. doi:https://doi.org/10.1007/s12551-020-00662-z.
- Yandek LE, Pokorny A, Florén A, Knoelke K, Langel Ü, Almeida PFF. Mechanism of the cell-penetrating peptide transportan 10 permeation of lipid bilayers. Biophys J. 2007;92(7):2434–2444. doi:https://doi.org/10.1529/biophysj.106.100198.
- Cahill K. Molecular electroporation and the transduction of oligoarginines. Phys Biol. 2009;7(1):16001. doi:https://doi.org/10.1088/1478-3975/7/1/016001.
- Yamada T, Gupta TKD, Beattie CW. p28, an anionic cell-penetrating peptide, increases the activity of wild type and mutated p53 without altering its conformation. Mol Pharm. 2013;10(9):3375–3383. doi:https://doi.org/10.1021/mp400221r.
- Warso MA, Richards JM, Mehta D, Christov K, Schaeffer C, Rae Bressler L, Yamada T, Majumdar D, Kennedy SA, Beattie CW, Das Gupta TK, A first-in-class, first-in-human, phase I trial of p28, a non-HDM2-mediated peptide inhibitor of p53 ubiquitination in patients with advanced solid tumours. Br. J. Cancer. 2013, 108, 1061–1070. https://doi.org/https://doi.org/10.1038/bjc.2013.74
- Lulla RR, Goldman S, Yamada T, Beattie CW, Bressler L, Pacini M, Pollack IF, Fisher PG, Packer RJ, Dunkel IJ, et al. Phase I trial of p28 (NSC745104), a non-HDM2-mediated peptide inhibitor of p53 ubiquitination in pediatric patients with recurrent or progressive central nervous system tumors: a pediatric brain tumor consortium study. Neuro Oncol. 2016;18(9):1319–1325. doi:https://doi.org/10.1093/neuonc/now047.
- Bolhassani A, Jafarzade BS, Mardani G. In vitro and in vivo delivery of therapeutic proteins using cell penetrating peptides. Peptides. 2017;87:50–63. doi:https://doi.org/10.1016/j.peptides.2016.11.011.
- Shafiee F, Rabbani M, Jahanian-Najafabadi A. Production and evaluation of cytotoxic effects of DT386-BR2 fusion protein as a novel anti-cancer agent. J Microbiol Methods. 2016;130:100–105. https://doi.org/https://doi.org/10.1016/j.mimet.2016.09.004.
- Zhang X, Lin C, Lu A, Lin G, Chen H, Liu Q, Yang Z, Zhang H, Liposomes equipped with cell penetrating peptide BR2 enhances chemotherapeutic effects of cantharidin against hepatocellular carcinoma. Drug Deliv. 2017; 24: 986–998. https://doi.org/https://doi.org/10.1080/10717544.2017.1340361
- Kebebe D, Liu Y, Wu Y, Vilakhamxay M, Liu Z, Li J. Tumor-targeting delivery of herb-based drugs with cell-penetrating/tumor-targeting peptide-modified nanocarriers. Int J Nanomedicine. 2018;13:1425–1442. doi:https://doi.org/10.2147/IJN.S156616.
- Jiang R, Lönnerdal B. Bovine lactoferrin and lactoferricin exert antitumor activities on human colorectal cancer cells (HT-29) by activating various signaling pathways. Biochem Cell Biol. 2017;95(1):99–109. doi:https://doi.org/10.1139/bcb-2016-0094.
- Zweytick D. LTX-315 – a promising novel antitumor peptide and immunotherapeutic agent. Cell Stress. 2019;3(11):328–329. doi:https://doi.org/10.15698/cst2019.11.202.
- Hao Y, Yang N, Teng D, Wang X, Mao R, Wang J. A review of the design and modification of lactoferricins and their derivatives. Biometals. 2018;31(3):331–341. doi:https://doi.org/10.1007/s10534-018-0086-6.
- Sadiq IZ, Babagana K, Danlami D, Abdullahi LI, Khan AR. Molecular therapeutic cancer peptides: a closer look at bovine lactoferricin. AJBGMB. 2018;1:1–9. doi:https://doi.org/10.9734/ajbgmb/2018/v1i2471.
- Haug BE, Camilio KA, Eliassen LT, Stensen W, Svendsen JS, Berg K, Mortensen B, Serin G, Mirjolet JF, Bichat F, et al. Discovery of a 9-mer cationic peptide (LTX-315) as a potential first in class oncolytic peptide. J Med Chem. 2016;59(7):2918–2927. doi:https://doi.org/10.1021/acs.jmedchem.5b02025.
- Camilio KA, Wang MY, Mauseth B, Waagene S, Kvalheim G, Rekdal Ø, Sveinbjørnsson B, Mælandsmo GM. Combining the oncolytic peptide LTX-315 with doxorubicin demonstrates therapeutic potential in a triple-negative breast cancer model. Breast Cancer Res. 2019;21(1):9. doi:https://doi.org/10.1186/s13058-018-1092-x.
- Sveinbjørnsson B, Camilio KA, Haug BE, Rekdal Ø. LTX-315: a first-in-class oncolytic peptide that reprograms the tumor microenvironment. Future Med Chem. 2017;9(12):1339–1344. doi:https://doi.org/10.4155/fmc-2017-0088.
- Nakase I, Noguchi K, Aoki A, Takatani-Nakase T, Fujii I, Futaki S. Arginine-rich cell-penetrating peptide-modified extracellular vesicles for active macropinocytosis induction and efficient intracellular delivery. Sci Rep. 2017;7(1):1991. doi:https://doi.org/10.1038/s41598-017-02014-6.
- Guo Z, Peng H, Kang J, Sun D. Cell-penetrating peptides: possible transduction mechanisms and therapeutic applications. Biomed Rep. 2016;4(5):528–534. doi:https://doi.org/10.3892/br.2016.639.
- Nakase I, Niwa M, Takeuchi T, Sonomura K, Kawabata N, Koike Y, Takehashi M, Tanaka S, Ueda K, Simpson JC, et al. Cellular uptake of arginine-rich peptides: roles for macropinocytosis and actin rearrangement. Mol Ther. 2004;10(6):1011–1022. doi:https://doi.org/10.1016/j.ymthe.2004.08.010.
- Takeuchi T, Futaki S. Current understanding of direct translocation of arginine-rich cell-penetrating peptides and its internalization mechanisms. Chem Pharm Bull (Tokyo). 2016;64(10):1431–1437.
- He L, Sayers EJ, Watson P, Jones AT. Contrasting roles for actin in the cellular uptake of cell penetrating peptide conjugates. Scie Rep. 2018:8. doi:https://doi.org/10.1038/s41598-018-25600-8.
- Lafarga V, Sirozh O, Díaz-López I, Galarreta A, Hisaoka M, Zarzuela E, Boskovic J, Jovanovic B, Fernandez-Leiro R, Muñoz J, et al. Widespread displacement of DNA- and RNA-binding factors underlies toxicity of arginine-rich cell-penetrating peptides. EMBO J. 2021;40(13):103311. doi:https://doi.org/10.15252/embj.2019103311.
- Nakase I, Konishi Y, Ueda M, Saji H, Futaki S. Accumulation of arginine-rich cell-penetrating peptides in tumors and the potential for anticancer drug delivery in vivo. J Control Release. 2012;159(2):181–188. doi:https://doi.org/10.1016/j.jconrel.2012.01.016.
- Kristensen M, Nielsen HM. Cell-penetrating peptides as tools to enhance non-injectable delivery of biopharmaceuticals. Tissue Barriers. 2016;4(2):1178369–1178384. doi:https://doi.org/10.1080/21688370.2016.1178369.
- Kristensen M, Birch D, Nielsen HM. Applications and challenges for use of cell-penetrating peptides as delivery vectors for peptide and protein cargos. Int J Mol Sci. 2016;17(2):185–202. doi:https://doi.org/10.3390/ijms17020185.
- Xue G, Liu Z, Wang L, Zu L. The role of basic residues in the fragmentation process of the lysine rich cell-penetrating peptide TP10. J Mass Spectrom. 2015;50(1):220–227. doi:https://doi.org/10.1002/jms.3524.
- El-Andaloussi S, Järver P, Johansson HJ, Langel Ü. Cargo-dependent cytotoxicity and delivery efficacy of cell-penetrating peptides: a comparative study. Biochem J. 2007;407(2):285–292. doi:https://doi.org/10.1042/BJ20070507.
- Song J, Kai M, Zhang W, Zhang J, Liu L, Zhang B, Liu X, Wang R. Cellular uptake of transportan 10 and its analogs in live cells: selectivity and structure-activity relationship studies. Peptides. 2011;32(9):1934–1941. doi:https://doi.org/10.1016/j.peptides.2011.07.018.
- Juliano R, Alam MR, Dixit V, Kang H. Mechanisms and strategies for effective delivery of antisense and siRNA oligonucleotides. Nucleic Acids Res. 2008;36(12):4158–4171. doi:https://doi.org/10.1093/nar/gkn342.
- Durzyńska J, Przysiecka Ł, Nawrot R, Barylski J, Nowicki G, Warowicka A, Musidlak O, Goździcka-Józefiak A. Viral and other cell-penetrating peptides as vectors of therapeutic agents in medicine. J Pharmacol Exp Ther. 2015;354(1):32–42. doi:https://doi.org/10.1124/jpet.115.223305.
- Lelle M, Frick SU, Steinbrink K, Peneva K. Novel cleavable cell-penetrating peptide-drug conjugates: synthesis and characterization. J Pept Sci. 2014;20(5):323–333. doi:https://doi.org/10.1002/psc.2617.
- Shi NQ, Gao W, Xiang B, Qi XR. Enhancing cellular uptake of activable cell-penetrating peptide-doxorubicin conjugate by enzymatic cleavage. Int J Nanomedicine. 2012;7:1613–1621. https://doi.org/https://doi.org/10.2147/IJN.S30104.
- Movafegh B, Jalal R, Mohammadi Z, Aldaghi SA. Poly-L-arginine: enhancing cytotoxicity and cellular uptake of doxorubicin and necrotic cell death. Anticancer Agents Med Chem. 2018;18(10):1448–1456. doi:https://doi.org/10.2174/1871520618666180412114750.
- Nasrolahi Shirazi A, Tiwari R, Chhikara BS, Mandal D, Parang K. A. Nasrolahi Shirazi, R. Tiwari, B.S. Chhikara, D. Mandal, K. Parang, Design and biological evaluation of cell-penetrating peptide-doxorubicin conjugates as prodrugs. Mol Pharm. 2013;10(2):488–499. doi:https://doi.org/10.1021/mp3004034.
- Zhang P, Cheetham AG, Lock LL, Cui H. Cellular uptake and cytotoxicity of drug-peptide conjugates regulated by conjugation site. Bioconjug Chem. 2013;24(4):604–613. doi:https://doi.org/10.1021/bc300585h.
- Lee JY, Choi YS, Suh JS, Kwon YM, Yang VC, Lee SJ, Chung CP, Park YJ. Cell-penetrating chitosan/doxorubicin/TAT conjugates for efficient cancer therapy. Int J Cancer. 2011;128(10):2470–2480. doi:https://doi.org/10.1002/ijc.25578.
- Aroui S, Brahim S, de Waard M, Bréard J, Kenani A. Efficient induction of apoptosis by doxorubicin coupled to cell-penetrating peptides compared to unconjugated doxorubicin in the human breast cancer cell line MDA-MB 231. Cancer Lett. 2009;285(1):28–38. doi:https://doi.org/10.1016/j.canlet.2009.04.044.
- Aroui S, Brahim S, Hamelin J, de Waard M, Bréard J, Kenani A, Conjugation of doxorubicin to cell penetrating peptides sensitizes human breast MDA-MB 231 cancer cells to endogenous TRAIL-induced apoptosis. Apoptosis 2009; 14: 1352–1365. https://doi.org/https://doi.org/10.1007/s10495-009-0397-8
- Aroui S, Brahim S, Waard MD, Kenani A. Cytotoxicity, intracellular distribution and uptake of doxorubicin and doxorubicin coupled to cell-penetrating peptides in different cell lines: a comparative study. Biochem Biophys Res Commun. 2010;391(1):419–425. doi:https://doi.org/10.1016/j.bbrc.2009.11.073.
- Chen Z, Zhang P, Cheetham AG, Moon JH, Moxley JW, Lin YA, Cui H. Controlled release of free doxorubicin from peptide-drug conjugates by drug loading. J Control Release. 2014;191:123–130. https://doi.org/https://doi.org/10.1016/j.jconrel.2014.05.051.
- Liang JF, Yang VC. Synthesis of doxorubicin-peptide conjugate with multidrug resistant tumor cell killing activity. Bioorg Med Chem Lett. 2005;15(22):5071–5075. doi:https://doi.org/10.1016/j.bmcl.2005.07.087.
- Lakkadwala S, Dos Santos Rodrigues B, Sun C, Singh J. Biodistribution of TAT or QLPVM coupled to receptor targeted liposomes for delivery of anticancer therapeutics to brain in vitro and in vivo. Nanomedicine. 2020;23:102112. doi:https://doi.org/10.1016/j.nano.2019.102112.
- Liu Z, Xiong M, Gong J, Zhang Y, Bai N, Luo Y, Li L, Wei Y, Liu Y, Tan X, et al. Legumain protease-activated TAT-liposome cargo for targeting tumours and their microenvironment. Nat Commun. 2014;5(1):4280. doi:https://doi.org/10.1038/ncomms5280.
- Sethuraman VA, Lee MC, Bae YH. A biodegradable pH-sensitive micelle system for targeting acidic solid tumors. Pharm Res. 2008;25(3):657–666. doi:https://doi.org/10.1007/s11095-007-9480-4.
- Lee ES, Gao Z, Kim D, Park K, Kwon IC, Bae YH. Super pH-sensitive multifunctional polymeric micelle for tumor pH(e) specific TAT exposure and multidrug resistance. J Control Release. 2008;129(3):228–236. doi:https://doi.org/10.1016/j.jconrel.2008.04.024.
- Rousselle C, Clair P, Lefauconnier JM, Kaczorek M, Scherrmann JM, Temsamani J. New advances in the transport of doxorubicin through the blood-brain barrier by a peptide vector-mediated strategy. Mol Pharmacol. 2000;57(4):679–686. doi:https://doi.org/10.1124/mol.57.4.679.
- Aroui S, Mili D, Brahim S, de Waard M, Kenani A. Doxorubicin coupled to penetratin promotes apoptosis in CHO cells by a mechanism involving c-Jun NH2-terminal kinase. Biochem Biophys Res Commun. 2010;396(4):908–914. doi:https://doi.org/10.1016/j.bbrc.2010.05.020.
- Aroui S, Dardevet L, Ben Ajmia W, De Boisvilliers M, Perrin F, Laajimi A, Boumendjel A, Kenani A, Muller JM, de Waard M, et al. Conjugate induces apoptosis of human glioblastoma cells by acting through the ROS-ERK/AKT-p53 pathway. Mol Pharm. 2015;12(12):4336–4348. doi:https://doi.org/10.1021/acs.molpharmaceut.5b00531.
- Ché C, Yang G, Thiot C, Lacoste JC, Demeule CM, Régina A, Béliveau R, Castaigne JP, Castaigne J-P. New Angiopep-modified doxorubicin (ANG1007) and etoposide (ANG1009) chemotherapeutics with increased brain penetration. J Med Chem. 2010;53(7):2814–2824. doi:https://doi.org/10.1021/jm9016637.
- Figueiredo P, Balasubramanian V, Shahbazi M-A, Correia A, Wu D, Palivan CG, Hirvonen JT, Santos HA. Angiopep2-functionalized polymersomes for targeted doxorubicin delivery to glioblastoma cells. . International Journal of Pharmaceutics. 2016;511(2):794–803. doi:https://doi.org/10.1016/j.ijpharm.2016.07.066.
- Soudy R, Chen C, Kaur K. Novel peptide-doxorubucin conjugates for targeting breast cancer cells including the multidrug resistant cells. J Med Chem. 2013;56(19):7564–7573. doi:https://doi.org/10.1021/jm400647r.
- Yu M, Li X, Huang X, Zhang J, Zhang Y, Wang H. New cell-penetrating peptide (KRP) with multiple physicochemical properties endows doxorubicin with tumor targeting and improves its therapeutic index. ACS Appl Mater Interfaces. 2019;11(2):2448–2458. doi:https://doi.org/10.1021/acsami.8b21027.
- Li Y, Zheng X, Cao Z, Xu W, Zhang J, Gong M. Self-assembled peptide (CADY-1) improved the clinical application of doxorubicin. Int J Pharm. 2012;434(1–2):209–214. doi:https://doi.org/10.1016/j.ijpharm.2012.06.003.
- Rousselle C, Smirnova M, Clair P, Lefauconnier JM, Chavanieu A, Calas B, Scherrmann JM, Temsamani J. Enhanced delivery of doxorubicin into the brain via a peptide-vector-mediated strategy: saturation kinetics and specificity. J Pharmacol Exp Ther. 2001;296:124–131.
- Liu Y, Ran R, Chen J, Kuang Q, Tang J, Mei L, Zhang Q, Gao H, Zhang Z, He Q. Paclitaxel loaded liposomes decorated with a multifunctional tandem peptide for glioma targeting. Biomaterials. 2014;35(17):4835–4847. doi:https://doi.org/10.1016/j.biomaterials.2014.02.031.
- Dubikovskaya EA, Thorne SH, Pillow TH, Contag CH, Wender PA. Overcoming multidrug resistance of small-molecule therapeutics through conjugation with releasable octaarginine transporters. Proc Natl Acad Sci USA. 2008;105(34):12128–12133. doi:https://doi.org/10.1073/pnas.0805374105.
- Pepe D, Carvalho VF, McCall M, de Lemos DP, Lopes LB. Transportan in nanocarriers improves skin localization and antitumor activity of paclitaxel. Int J Nanomedicine. 2016;11:2009–2019. https://doi.org/https://doi.org/10.2147/IJN.S97331.
- Duan Z, Chen C, Qin J, Liu Q, Wang Q, Xu X, Wang J. Cell-penetrating peptide conjugates to enhance the antitumor effect of paclitaxel on drug-resistant lung cancer. Drug Deliv. 2017;24(1):752–764. doi:https://doi.org/10.1080/10717544.2017.1321060.
- Wang S, Zhelev NZ, Duff S, Fischer PM. Synthesis and biological activity of conjugates between paclitaxel and the cell delivery vector penetratin. Bioorg Med Chem Lett. 2006;16(10):2628–2631. doi:https://doi.org/10.1016/j.bmcl.2006.02.035.
- Kurzrock R, Gabrail N, Chandhasin C, Moulder S, Smith C, Brenner A, Sankhala K, Mita A, Elian K, Bouchard D, et al. Safety, pharmacokinetics, and activity of GRN1005, a novel conjugate of angiopep-2, a peptide facilitating brain penetration, and paclitaxel, in patients with advanced solid tumors. Mol Cancer Ther. 2012;11(2):308–316. doi:https://doi.org/10.1158/1535-7163.MCT-11-0566.
- Régina A, Demeule M, Ché C, Lavallée I, Poirier J, Gabathuler R, Béliveau R, Castaigne JP. Antitumour activity of ANG1005, a conjugate between paclitaxel and the new brain delivery vector Angiopep-2. Br J Pharmacol. 2008;155(2):185–197. doi:https://doi.org/10.1038/bjp.2008.260.
- Drappatz J, Brenner A, Wong ET, Eichler A, Schiff D, Mikkelsen GT, Meyers CA, Meyers CA, Meyers CA, Fielding RM, et al. Phase I study of GRN1005 in recurrent malignant glioma. Clin Cancer Res. 2013;19(6):1567–1576. doi:https://doi.org/10.1158/1078-0432.CCR-12-2481.
- Yu DH, Lu Q, Xie J, Fang C, Chen HZ. Peptide-conjugated biodegradable nanoparticles as a carrier to target paclitaxel to tumor neovasculature. Biomaterials. 2010;31(8):2278–2292. doi:https://doi.org/10.1016/j.biomaterials.2009.11.047.
- Ho K, Morfin C, Slowinska K. The limitations of collagen/CPP hybrid peptides as carriers for cancer drugs to FaDu cells. Molecules. 2019;24(4):676. doi:https://doi.org/10.3390/molecules24040676.
- Ayalew L, Acuna J, Urfano SF, Morfin C, Sablan A, Oh M, Gamboa A, Slowinska K. Conjugation of paclitaxel to hybrid peptide carrier and biological evaluation in Jurkat and A549 cancer cell lines. ACS Med Chem Lett. 2017;8(8):814–819. doi:https://doi.org/10.1021/acsmedchemlett.7b00117.
- Gao W, Xiang B, Meng TT, Liu F, Qi XR. Chemotherapeutic drug delivery to cancer cells using a combination of folate targeting and tumor microenvironment-sensitive polypeptides. Biomaterials. 2013;34(16):4137–4149. doi:https://doi.org/10.1016/j.biomaterials.2013.02.014.
- Mäe M, Rautsi O, Enbäck J, Hällbrink M, Aizman KR, Lindgren M, Laakkonen P, Langel Ü. Tumour targeting with rationally modified cell-penetrating peptides. Int J Pept Res and Ther. 2012;18(4):361–371. doi:https://doi.org/10.1007/s10989-012-9312-1.
- Lindgren M, Rosenthal-Aizman K, Saar K, Eiríksdóttir E, Jiang Y, Sassian M, Ostlund P, Hällbrink M, Langel Ü. Overcoming methotrexate resistance in breast cancer tumour cells by the use of a new cell-penetrating peptide. Biochem Pharmacol. 2006;71(4):416–425. doi:https://doi.org/10.1016/j.bcp.2005.10.048.
- Szabó I, Orbán E, Schlosser G, Hudecz F, Bánóczi Z. Cell-penetrating conjugates of pentaglutamylated methotrexate as potential anticancer drugs against resistant tumor cells. Eur J Med Chem. 2016;115:361–368. https://doi.org/https://doi.org/10.1016/j.ejmech.2016.03.034.
- Vale N, Ferreira A, Fernandes I, Alves C, Araújo MJ, Mateus N, Gomes P. Gemcitabine anti-proliferative activity significantly enhanced upon conjugation with cell-penetrating peptides. Bioorg Med Chem Lett. 2017;27(13):2898–2901. doi:https://doi.org/10.1016/j.bmcl.2017.04.086.
- Ferreira A, Lapa R, Vale N. Combination of Gemcitabine with cell-penetrating peptides: a pharmacokinetic approach using in silico tools. Biomolecules. 2019;9(11):693. doi:https://doi.org/10.3390/biom9110693.
- Kwon YM, Chung HS, Moon C, Yockman J, Park YJ, Gitlin SD, David AEVC, Yang VC. Yang, L-Asparaginase encapsulated intact erythrocytes for treatment of acute lymphoblastic leukemia (ALL). J Control Release. 2009;139(3):182–189. doi:https://doi.org/10.1016/j.jconrel.2009.06.027.
- Kwon YM, Li YT, Liang JF, Park YJ, Chang LC, Yang VC. PTD-modified ATTEMPTS system for enhanced asparaginase therapy: a proof-of-concept investigation. J Control Release. 2008;130(3):252–258. doi:https://doi.org/10.1016/j.jconrel.2008.06.017.
- Myrberg H, Zhang L, Mäe M, Langel Ü. Design of a tumor-homing cell-penetrating peptide. Bioconjug Chem. 2008;19(1):70–75. doi:https://doi.org/10.1021/bc0701139.
- Klimpel A, Neundorf I. Bifunctional peptide hybrids targeting the matrix of mitochondria. J Control Release. 2018;291:147–156. https://doi.org/https://doi.org/10.1016/j.jconrel.2018.10.029.
- Coriat R, Faivre SJ, Mir O, Dreyer C, Ropert S, Bouattour M, Desjardins R, Goldwasser F, Raymond E. Pharmacokinetics and safety of DTS-108, a human oligopeptide bound to SN-38 with an esterase-sensitive cross-linker in patients with advanced malignancies: a Phase I study. Int J Nanomedicine. 2016;11:6207–6216. doi:https://doi.org/10.2147/IJN.S110274.
- Song J, Zhang Y, Zhang W, Chen J, Yang X, Ma P, Zhang B, Liu B, Ni J, Wang R. Cell penetrating peptide TAT can kill cancer cells via membrane disruption after attachment of camptothecin. Peptides. 2015;63:143–149. doi:https://doi.org/10.1016/j.peptides.2014.12.001.
- Taki H, Kanazawa T, Akiyama F, Takashima Y, Okada H. Intranasal delivery of camptothecin-loaded tat-modified nanomicells for treatment of intracranial brain tumors. Pharmaceuticals (Basel). 2012 Oct 15;5(10):1092–1102. PMID: 24281259; PMCID: PMC3816654. doi:https://doi.org/10.3390/ph5101092.
- Feni L, Parente S, Robert C, Gazzola S, Arosio D, Piarulli U, Neundorf I. Kiss and run: promoting effective and targeted cellular uptake of a drug delivery vehicle composed of an integrin-targeting diketopiperazine peptidomimetic and a cell-penetrating peptide. Bioconjug Chem. 2019;30(7):2011–2202. doi:https://doi.org/10.1021/acs.bioconjchem.9b00292.
- Koshkaryev A, Piroyan A, Torchilin VP. Bleomycin in octaarginine-modified fusogenic liposomes results in improved tumor growth inhibition. Cancer Lett. 2013;334(2):293–301. doi:https://doi.org/10.1016/j.canlet.2012.06.008.
- Spicer JF, Marabelle A, Baurain J, Awada A, Kristeleit RS, Jossang DE, Jebsen N, Loirat D, Armstrong AC, Curigliano G, et al. A phase I/II study of the oncolytic peptide LTX-315 combined with checkpoint inhibition generates de novo T-cell responses and clinical benefit in patients with advanced solid tumors. J Clin Oncol. 2018;36(15_suppl):3094. doi:https://doi.org/10.1200/JCO.2018.36.15_suppl.3094.
- Eid RA, Razavi GS, Mkrtichyan M, Janik J, Khleif SN. Old-School chemotherapy in immunotherapeutic combination in cancer, a low-cost drug repurposed. Cancer Immunol Res. 2016;4(5):377–382. doi:https://doi.org/10.1158/2326-6066.CIR-16-0048.
- Alizadeh D, Trad M, Hanke NT, Larmonier CB, Janikashvili N, Bonnotte B, Katsanis E, Larmonier N. Doxorubicin eliminates myeloid-derived suppressor cells and enhances the efficacy of adoptive T-cell transfer in breast cancer. Cancer Res. 2014;74(1):104–118. doi:https://doi.org/10.1158/0008-5472.CAN-13-1545.
- Wang H, Ma X, Ren S, Buolamwini JK, Yan C. A small-molecule inhibitor of MDMX activates p53 and induces apoptosis. Mol Cancer Ther. 2011;10(1):69–79. doi:https://doi.org/10.1158/1535-7163.MCT-10-0581.
- Dornan D, Bheddah S, Newton K, Ince W, Frantz GD, Dowd P, Koeppen H, Dixit VM, French DM. COP1, the negative regulator of p53, is overexpressed in breast and ovarian adenocarcinomas. Cancer Res. 2004;64(20):7226–7230. doi:https://doi.org/10.1158/0008-5472.CAN-04-2601.
- Johnson N, Shapiro G. Cyclin-dependent kinases (cdks) and the DNA damage response: rationale for cdk inhibitor–chemotherapy combinations as an anticancer strategy for solid tumors. Expert Opin Ther Targets. 2010;14(11):1199–1212. doi:https://doi.org/10.1517/14728222.2010.525221.
- Allen TM. Ligand-targeted therapeutics in anticancer therapy. Nat Rev Cancer. 2002;2(10):750–763. doi:https://doi.org/10.1038/nrc903.
- Terwogt JMM, ten Bokkel Huinink WW, Schellens JH, Schot M, Mandjes IA, Zurlo MG, Rocchetti M, Rosing H, Koopman FJ, Beijnen JH. Phase I clinical and pharmacokinetic study of PNU166945, a novel water-soluble polymer-conjugated prodrug of paclitaxel. Anticancer Drugs. 2001;12(4):315–323. doi:https://doi.org/10.1097/00001813-200104000-00003.
- De Coupade C, Fittipaldi A, Chagnas V, Michel M, Carlier S, Tasciotti E, Darmon A, Ravel D, Kearsey J, Giacca M, et al. Novel human-derived cell-penetrating peptides for specific subcellular delivery of therapeutic biomolecules. Biochem J. 2005;390(2):407–418. doi:https://doi.org/10.1042/BJ20050401.
- Senter PD, Beam KS, Mixan B, Wahl AF. Identification and activities of human carboxylesterases for the activation of CPT-11, a clinically approved anticancer drug. Bioconjug Chem. 2001;12(6):1074–1080. doi:https://doi.org/10.1021/bc0155420.
- Gupta E, Lestingi TM, Mick R, Ramirez J, Vokes EE, Ratain MJ. Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res. 1994;54:3723–3725.
- Meyer-Losic F, Nicolazzi C, Quinonero J, Ribes F, Michel M, Dubois V, De Coupade C, Boukaissi M, Chéné AS, Tranchant I, et al. DTS-108, A novel peptidic prodrug of SN38: in vivo efficacy and toxicokinetic studies. Clin Cancer Res. 2008;14(7):2145–2153. doi:https://doi.org/10.1158/1078-0432.CCR-07-4580.
- Demeule M, Régina A, Ché C, Poirier J, Nguyen T, Gabathuler R, Castaigne JP, Béliveau R. Identification and design of peptides as a new drug delivery system for the brain. J Pharmacol Exp Ther. 2008;324(3):1064–1072. doi:https://doi.org/10.1124/jpet.107.131318.
- Cai W, Chen G, Luo Q, Liu J, Guo X, Zhang T, Ma F, Yuan L, Li B, Cai J. PMP22 regulates self-renewal and chemoresistance of gastric cancer cells. Molecular Cancer Therapeutics. 2017;16(6):1187–1198. doi:https://doi.org/10.1158/1535-7163.MCT-16-0750.
- Aroui S, Ram N, Appaix F, Ronjat M, Kenani A, Pirollet F, de Waard M. Maurocalcine as a non toxic drug carrier overcomes doxorubicin resistance in the cancer cell line MDA-MB 231. Pharm Res. 2009;26(4):836–845. doi:https://doi.org/10.1007/s11095-008-9782-1.
- Aroui S, Kenani A. Cell-penetrating peptides: a challenge for drug delivery. In: Stefaniu A, Rasul A, Hussain G, editors. Cheminformatics and its Applications. Rijeka, Croatia, IntechOpen Limited; 2020. p. 209. doi:https://doi.org/10.5772/intechopen.91684.
- Ronjat M, Feng W, Dardevet L, Dong Y, Khoury SA, Chatelain FC, Vialla V, Chahboun S, Lesage F, Darbon H, et al. In cellulo phosphorylation induces pharmacological reprogramming of maurocalcin, a cell-penetrating venom peptide. PNAS. 2016;113(17):E2460–E2468. doi:https://doi.org/10.1073/pnas.1517342113.
- Boisseau S, Mabrouk K, Ram N, Garmy N, Collin V, Tadmouri A, Mikati M, Sabatier JM, Ronjat M, Fantini J, et al. Cell penetration properties of maurocalcine, a natural venom peptide active on the intracellular ryanodine receptor. Biochim Biophys Acta. 2006;1758(3):308–319. doi:https://doi.org/10.1016/j.bbamem.2006.02.007.
- Alves ID, Bechara C, Walrant A, Zaltsman Y, Jiao CY, Sagan S, Gasset M. Relationships between membrane binding, affinity and cell internalization efficacy of a cell-penetrating peptide: penetratin as a case study. PLoS One. 2011;6(9):e24096. doi:https://doi.org/10.1371/journal.pone.0024096.
- Jiao CY, Delaroche D, Burlina F, Alves ID, Chassaing G, Sagan S. Translocation and endocytosis for cell-penetrating peptide internalization. J Biol Chem. 2009;284(49):33957–33965. doi:https://doi.org/10.1074/jbc.M109.056309.
- Zhang X, Zhang X, Wang X, Wang T, Bai B, Zhang N, Zhao Y, Yu Y, Wang B. Efficient delivery of triptolide plus a mir-30-5p inhibitor through the use of near infrared laser responsive or CADY modified MSNs for efficacy in rheumatoid arthritis therapeutics. Front Bioeng Biotechnol. 2020;8:170. https://doi.org/https://doi.org/10.3389/fbioe.2020.00170.
- Park YJ, Liang JF, Ko KS, Kim SW, Yang VC. Low molecular weight protamine as an efficient and nontoxic gene carrier: in vitro study. J Gene Med. 2003;5(8):700–711. doi:https://doi.org/10.1002/jgm.402.
- Elmquist A, Lindgren M, Bartfai T, Langel U. VE-cadherin-derived cell-penetrating peptide, pVEC, with carrier functions. Exp Cell Res. 2001;269(2):237–244. doi:https://doi.org/10.1006/excr.2001.5316.
- Elmquist A, Hansen M, Langel Ü. Structure-activity relationship study of the cell-penetrating peptide pVEC. Biochim Biophys Acta. 2006;1758(6):721–729. doi:https://doi.org/10.1016/j.bbamem.2006.05.013.
