ABSTRACT
When the organism encounters a foreign substance, it responds with mutual and regular interactions at different stages of the immune system. In airway diseases, the first encounter is at the epithelial level, where innate immune cells and their responses form the first leg of the protective mechanism. The most important barrier for environmental damage is the epithelial barrier. However, the epithelial barrier is not just a mechanical barrier. The formation of the microbiome on the epithelium and the tolerance or intolerance to environmental factors are vital. This vital balance is maintained between the epithelial surface and the subepithelial innate immune system. This is achieved by the epithelial line, which is a mechanical and functional barrier between them. In this respect, epithelial barrier function preservation has an important role in the development and prognosis of airway disease.
Subepithelial innate immune system
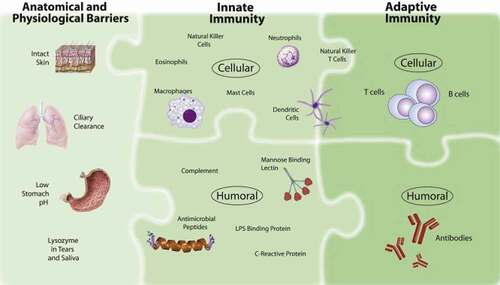
The functions that protect against diseases in living things, recognize pathogens and tumor cells and destroy them are expressed as the immune system. This system scans every foreign substance that enters or comes into contact with the body, and distinguishes it from healthy body cells and tissues. The body provides protection against bacteria, viruses and other foreign substances with many different mechanisms. These protective mechanisms consist of two interconnected defense systems and their subgroup elements.Citation1 These are the innate immune system and the adaptive immune system.
Basically, the immune system is divided into innate and adaptive immune systems. In the innate immune system, it distinguishes that the substance that enters the organism is foreign, but cannot distinguish the type of pathogen.Citation2 nonspecific resistance is shown by two lines of defense. These are skin epithelial tissue, respiratory tract, gastrointestinal tract and mucous membranes in the urogenital tract, while the first line of defense is; chemical signals, antimicrobial peptides, antiphagocytic and natural killer cells form the second line of defense associated with the inflammatory response.Citation3
Innate immune system; It consists of important elements such as epithelial barriers (skin, mucosa and secretions), complements, phagocytes (neutrophils, mononuclear cells), natural killer (NK) cells, and sub-components such as Toll-like Receptor (TLR). Epithelial cells act as a barrier, providing the first line of host defense, trapping and killing potential pathogens, and activating innate immune system cells. The physical barrier against the external environment is provided by the junctional complex, which is formed by tight junctions and adherens junctions underneath. An additional layer of defense is provided by the mucociliary apparatus. Mucins act in concert with antimicrobial peptides and the ciliary apparatus to trap and clear pathogens. In addition to its barrier role, the homeostatic mucin MUC5B indicates the role of mucins in regulating innate immune system responses by regulating alveolar macrophage function.Citation4
The adaptive immune system develops throughout the person’s life, distinguishes what does not belong to the organism and gives a specific response to different pathogens. The adaptive immune system is divided into humoral and cellular. Cellular immunity involves the generation of T cells capable of destroying exogenous and harmful endogenous antigen-bearing cells. Humoral immunity, on the other hand, plays a role in defense by transforming B cells into plasma cells that secrete immunoglobulins with antigen-specific activity.Citation5
Elimination of microorganism by adaptive immune response; By blocking the microbe by binding to the extracellular microbe by the antibodies produced by B cells or facilitating the destruction of the antibody-bound microbe by the cells of the innate immune system, increasing the microbicidal effect against the intracellular microbe phagocytosed by the cytokines produced by T (CD4+) cells, and by increasing the microbicidal effect of the cytotoxic T (CD8+) cells. It occurs by directly killing the infected cell. A notable feature of the adaptive immune system, and a key difference from the innate immune system, is its memory, which provides effective protection against repeated exposure to harmful microbial agents by accelerating and amplifying the response, even when events are separated by decades.Citation6,Citation7
Epithelial barrier
Epithelial tissue acts primarily as a physical, functional and immune barrier between the internal and external environment. This barrier function is maintained by cell-to-cell connections from the surface to the basal surface, such as cell junctions, adhesion junctions, and desmosomes.
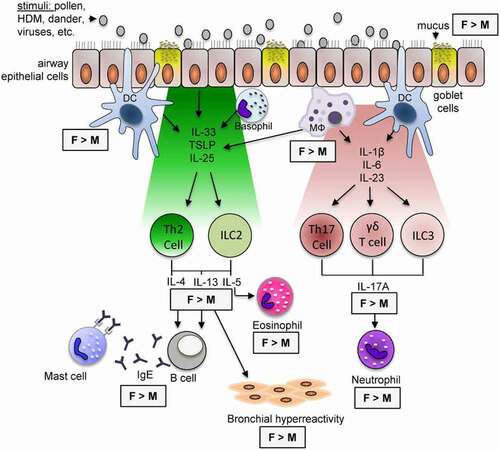
Airway diseases such as Allergic Rhinitis, Asthma, Chronic Rhinosinusitis, Chronic Obstructive Pulmonary Disease (COPD) related to airway epithelial barrier dysfunction are related to TJ defect and/or increased epithelial permeability. It has been shown that allergens and pathogens separate TJs between epithelial cells and stimulate the immune system.Citation10 The increased access of allergens, viruses and other environmental factors to the antigen
presenting cell in the submucosa as a result of epithelial dysfunction plays an important role in stimulating the Th2 type-mediated immune response and inducing epithelial mesenchymal transition (EMT). An important step of the Th2 immune response is eosinophil activation. IL-5 and IL-9 are responsible for the activation of eosinophils and mast cells, respectively. Th2 cells that co-open the TJ barrier, ILC2, and their secreted cytokines, IL-4 and IL-13, have been shown to significantly disrupt the bronchial epithelial barrier ().Citation9,Citation11 Two additional subsets of lymphoid cells sit at the interface of innate and adaptive immunity. These are Invariant natural killer T (iNKT) cells and mucosal-associated invariant T (MAIT) cells. Lymphoid cell subsets are at an important point because of their ability to recognize non-peptide antigens; iNKT cells recognize glycolipids, MAIT microbial metabolites. These antigens are presented by nonclassical antigen presenting molecules. It presents iNKT cells for CD1d and MAIT cells for MR1.Citation12
Figure 1. Epithelial barrier and its connections. Tight Junctions form an apical junction complex by forming a ring in the apicolateral region of the intestinal, skin and airway barrier. AJs in the lower region regulate the apical-basolateral membrane. TJs and AJs bind to the actin cytoskeleton via ZO-1, ZO-2, ZO-3. They are desmosomes that connect epithelial cells and disperse on the lateral surfaces. a-Catenins do not bind directly to cadherins; It binds to actin via ZO-1. Cadherins can become functional by interacting with catenin proteins.Citation9
Activated MAIT cells produce IFN, while iNKT cells IL-2, IL-3, IL-4, IL-5, IL-9, IL-10, IL-13, IL-17, including IFN-γ, TNF-alpha It produces many cytokines, including IL-21 and GM-CSF. Much less is known about MAIT cells. It is shown that both MAIT and iNKT cells can be potent modulators of the immune system by providing critical cytokines prior to adaptive immunity formation.Citation4,Citation7
Structure of allergens and effect on the epithelial barrier
Substances that form specific antibodies against themselves are called antigens. If this antigen causes allergic reactions then it is called allergen. Most allergens are small, stable and well-structured proteins. It is therefore suitable for structural studies with both X-ray crystallography and NMR spectroscopy. The most common allergens; aeroallergens, animal allergens, insect allergens, food allergens, drug allergens, occupational allergens. When the allergens taken through the skin pass the epidermal barrier, intercellular lipid lines form between the outer layer of corneocytes, hydrophobic and hydrophilic structures that organize skin permeability.Citation13 Allergens that penetrate the outer barrier of intact skin must be hydrophobic or bind to a lipophilic carrier. Specific enzyme stability is not required because they do not have protein-degrading enzymes.
Since both mucus and tissue of the respiratory tract act as an allergen reserve, inhaler allergens must be of particular size to enter the aqueous medium of mucosal surfaces with their broad solubility and mucus-binding properties.Citation15 Most mucus is secreted into the GI and respiratory tract, and most of it is digested and recycled. The rest is excreted in feces, sputum, saliva and nasal secretions, reproductive tract secretions and tears.Citation16
In the airway, mucus is continuously swept from distal to proximal. A thin layer of mucus gel is produced regularly and in small quantities by columnar (clara) cells in the small airways. In the large airways lined with pseudostratified epithelium, a thick mucus gel layer accumulates from the mucus carried from the distant airways and additional mucins are produced by the surface secretory cells and glands. After the mucus exits the trachea, it travels along the ciliary epithelium in the posterior part of the larynx. It then enters the pharynx and is swallowed, approximately 30 ml of airway mucus daily is eliminated by the GIS. The viscosity and elasticity of mucus in airway diseases makes it vulnerable to allergens.Citation17,Citation18
The proteolytic activity of the allergens themselves provides enhanced sensitization potential through disruption of the epithelial barrier layers.Citation19 High protein stability is required in allergen sensitization via the gastrointestinal tract because it is important to maintain proteolytic and hydrolytic resistance.Citation20
In developed countries, environmental pollution, changes in lifestyle and eating habits due to urbanization reveal contact with different allergens. This difference triggers the inflammatory response and manifests itself with allergic inflammatory diseases such as asthma and atopic dermatitis.Citation21,Citation22
It shows that there is a strong relationship between the characteristics of modern life and the allergen sensitization they require. Many factors such as family allergy history, infections, home furnishing materials (paint etc.), low ventilation rate, cesarean delivery play an important role in allergen sensitization ( and ).Citation8,Citation14,Citation24
Figure 2. Immune system: (1) Anatomical and physiological barriers; (2) innate immune system elements; (3) Adaptive immune system elements. The harmony between these systems ensures the correct functioning of the immune mechanism and the effective functioning of the immune system.Citation8
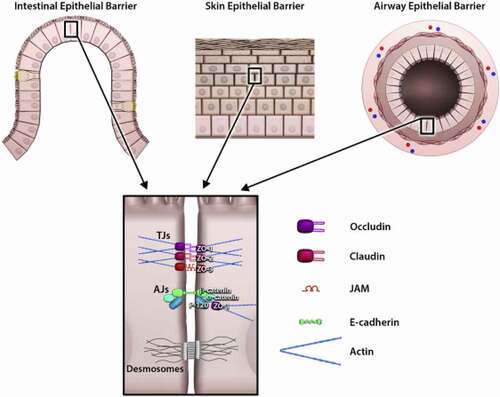
Figure 3. Microstructures of allergens and effector regions in diagnostic tests. IgE reactions are shown with different diagnostic principles and allergological tests. It indicates the fraction of total IgE antibody sIgE in serum specific for certain allergens. sIgEs show a particular sensitivity to the allergen to which they are specific. It responds in different ways in different effector organs with different diagnostic methods.Citation14
How does the innate immune system response if the epithelial barrier dysfunction?
Epithelial tissue, which is an element of innate immunity, can prevent the emergence of allergic inflammation through both the physical barrier function it creates and the cytokines and other mediators it secretes, and also plays an important role in the pathological and anatomical changes secondary to allergic inflammation.Citation25 Mediators released from epithelial cells provide chemotaxis of appropriate defense cells against released pathogens and stimuli.Citation21 In addition, secreted antimicrobial molecules, antiproteases, antioxidants and mucociliary actions ensure the retention and expulsion of foreign particles in the epithelial defense mechanism.Citation26
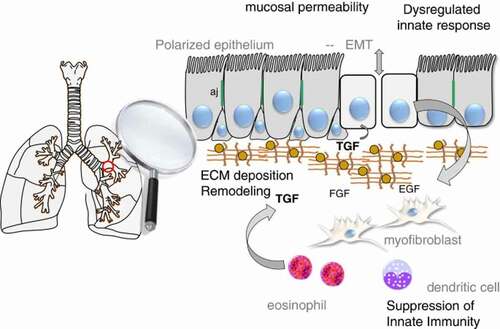
In epithelial barrier dysfunction, it is important in increasing the access of allergens and viruses to the antigen presenting cell in the submucosa, stimulating the TH2 type-mediated immune response and inducing EMT/remodeling. In epithelial barrier dysfunction, the penetration of allergens into the tissue is facilitated, the access of allergens to the antigen presenting cell in the submucosa increases, and the extension of spasmogenic agonists to smooth muscle increases.Citation17 Again, in epithelial barrier damage, junctional proteins associated with indirectly released inflammatory mediators are suppressed or they are separated by binding directly to allergens. Some protease secreting environmental factors, protease secreting eosinophils and neutrophils can degrade ZO-1 and E-cadherin molecules.Citation6,Citation27,Citation28 E–cadherin regulates cell proliferation and differentiation by regulating epidermal growth factor receptor (EGFR) and Beta-catenin activities (). E-Cadherin normally prevents the activation of EGFR, if there is a decrease or deterioration in E-Cadherin expression, epithelial mesenchymal transition (EMT) is stimulated, EGFR binds to the EGF ligand, resulting in a process that results in cell proliferation and goblet cell metaplasia. Disruption of E-Cadherin activation also results in dispersal of actin filaments, functional and morphological disruption of Tight Junction barriers.Citation29 Thus, it causes an increase in the access of the allergen to the antigen presenting cell from the submucosa, stimulating the Th2 type-mediated immune response and inducing EMT.Citation17,Citation30,Citation31
Figure 4. Schematic view of epithelial mesenchymal transition in the airway. It has an important place in the epithelium in asthma. In the relationship expressed as the epithelial mesenchymal unit, signals are sent through the mesenchymal in the epithelial sub-epithelial environment. It ensures the integrity of this unit of growth. Epithelial growth factor (EGF), Fibroblast growth factor (FGF), cytokines (such as IL-6, IL-1p, TGF-beta) release increases.Citation32
Epithelial barrier dysfunction and innate immune response in remodeling
During the early and late phase response in allergic airway diseases, an important condition in the disease symptoms that progress parallel to inflammation is remodeling. Remodeling sentence can also be called ‘remodeling of the extracellular matrix’ ().Citation9,Citation23
Figure 5. Triggers and mechanisms in airway changes, with gender differences. In asthma-related airway inflammatory diseases, the affected areas and the responses shown may vary according to gender. There are also gender differences in type-2 and IL-17A mediated airway inflammation.Citation23
TGF-Beta released from the epithelial cell is the main growth factor that enables the transformation of fibroblasts in the submucosa into myofibroblasts. Cells transformed into myofibroblasts cause smooth muscle hypertrophy by secreting ET-1(Endothelin-1), remodeling by secreting neural growth factor (NGF), and vascularization by secreting VEGF, causing 3 main components of remodeling.Citation33
Barrier function is maintained by adherens junctions, homophilic E-Cadherin interactions, and intercellular contact formation.Citation34 E-Cadherin binds to the actin cytoskeleton with Beta-Catenin stabilizing cell-cell. E-Cadherin downregulation is an essential component of the epithelial-mesenchymal transition (EMT), a process involved in cell migration, repair, and tissue remodeling. Many allergens contain proteases that cause epithelial damage. Proteases can also activate the ‘protease-activated receptor’ (PAR), which leads to proinflammatory gene transcription.Citation35 PAR activation disrupts E-Cadherin-mediated cell-cell contact. Damaged epithelium induces the mesenchymal phenotype by showing increased sensitivity to noxious stimuli and inadequate repair response. Insufficient epithelial repair marker CD44 is supported by epidermal growth factor receptor (EGFR) and increased expression of TGF-Beta in damaged epithelium.Citation29
In this most important process in epithelial barrier function, remodeling, when the structure of E-cadherin-Beta-Catenin is disrupted, Beta-Catenin released from its cytosolic part is released. Translocation of liberated Beta-Catenin to the nucleus and activation of Wnt/Beta-Catenin signals are an important step in tissue remodeling.Citation30,Citation36
Relationship of prognosis with epithelial barrier dysfunction and innate immune system
The airway epithelium has an important barrier function for the immune system in the interaction with the external environment.Citation37,Citation38 The airway epithelium consists of ciliated columnar cells, goblet cells, and clara cells. These cells regularly line the airway lumen. Protects against inhaled environmental factors such as aeroallergens, pollutants, pathogens.Citation39 Structural and functional disorders in the airway epithelium cause an abnormal signal to the immune system and structural cells, causing allergic airway remodeling, inflammation, and hypersensitivity.Citation40
Epithelial barrier disruption causes the release of some cytokines and growth factors from the epithelium with the deterioration of the repair mechanism of the airway epithelium. IL-33, IL-25 and thymic stromal lymphopoietin (TSLP), released by allergens activating the epithelium, aid in antigen presentation of dendritic cells. In addition, these cells that secrete IL-33 and IL-25 cause the secretion of IL-5 and IL-13 from natural T cells in the airway, thereby helping Th2 type inflammation.Citation21,Citation41 IgE synthesis has an important role in airway eosinophilia, smooth muscle hypertrophy, mucus formation and airway hypersensitivity via IL-3, 4, 5, 13 and Granulocyte-Macrophage colony stimulating factor (GM-CSF), a group of cytokines produced by Th2 in the pathogenesis of barrier dysfunction.Citation42
The epithelial barrier is also an important innate element after contact with the SARS-CoV virus. After exposure, the virus attaches to epithelial cells in the nasal cavity and begins to replicate. Angiotensin converting enzyme 2 (ACE2) acts as the primary receptor for SARS-CoV2 and SARS-CoV. Local spread of the virus in the nasal epithelium and activation of the innate immune response allow it to be detected in the nasal swab. Thus, the disease process begins with the infection of these epithelial cells.Citation43,Citation44
In conclusion
A successful immune response has a very important role in the prognosis of airway disease in epithelial barrier dysfunction. However, it is inevitable that the protection of barrier function is the most important step in the innate immune system.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Tomar N, De RK. A brief outline of the immune system. Methods Mol Biol. 2014;1184:1–9.
- Litman GW, Cannon JP, Dishaw LJ. Reconstructing immune phylogeny: new perspectives. Nat Rev Immunol. 2005 Nov;5(11):866–879. doi:10.1038/nri1712.
- Fair WR, Couch J, Wehner N. Prostatic antibacterial factor. Identity and significance. Urology. 1976 Feb;7(2):169–177. doi:10.1016/0090-4295(76)90305-8.
- Adkinson NF, et al. Middleton’s allergy: principles and practice. Eighth ed. Elsevier Inc; 2013.
- Abbas A, Lichtman A, Pillai S. Cellular and molecular immunology, Nineth ed. Elsevier Inc; 2016.
- Holgate ST. Innate and adaptive immune responses in asthma. Nat Med. 2012 May 4;18(5):673–683. doi:10.1038/nm.2731.
- Macdonald TT, Monteleone G. Immunity, inflammation, and allergy in the gut. Science. 2005 Mar 25;307(5717):1920–1925. doi:10.1126/science.1106442.
- Maeda K, Caldez MJ, Akira S. Innate immunity in allergy. Allergy. 2019 Sep;74(9):1660–1674. doi:10.1111/all.13788.
- Celebi Sözener Z, Cevhertas L, Nadeau K, Akdis M, Akdis CA. Environmental factors in epithelial barrier dysfunction. J Allergy Clin Immunol. 2020 Jun;145(6):1517–1528. doi:10.1016/j.jaci.2020.04.024.
- Georas SN, Rezaee F. Epithelial barrier function: at the front line of asthma immunology and allergic airway inflammation. J Allergy Clin Immunol. 2014 Sep;134(3):509–520. doi:10.1016/j.jaci.2014.05.049.
- Wawrzyniak P, Wawrzyniak M, Wanke K, Sokolowska M, Bendelja K, Rückert B, Globinska A, Jakiela B, Kast JI, Idzko M, et al. Regulation of bronchial epithelial barrier integrity by type 2 cytokines and histone deacetylases in asthmatic patients. J Allergy Clin Immunol. 2017 Jan;139(1):93–103. doi:10.1016/j.jaci.2016.03.050.
- Steelant B, Farré R, Wawrzyniak P, Belmans J, Dekimpe E, Vanheel H, Van Gerven L, Kortekaas Krohn I, Bullens DMA, Ceuppens JL, et al. Impaired barrier function in patients with house dust mite-induced allergic rhinitis is accompanied by decreased occludin and zonula occludens-1 expression. J Allergy Clin Immunol. 2016 Apr;137(4):1043–1053.e5. doi:10.1016/j.jaci.2015.10.050.
- De Benedetto A, Rafaels NM, McGirt LY, Ivanov AI, Georas SN, Cheadle C, Berger AE, Zhang K, Vidyasagar S, Yoshida T, et al. Tight junction defects in patients with atopic dermatitis. J Allergy Clin Immunol. 2011 Mar;127(3):773–86.e1-7. doi:10.1016/j.jaci.2010.10.018.
- Klimek L, Schendzielorz P. Early detection of allergic diseases in otorhinolaryngology. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2008;7:Doc04. doi:10.3205/cto000049.
- Rimmer J, Santos C, Yli-Panula E, Noronha V, Viander M, Hogan SP. Clinical and laboratory studies of the fate of intranasal allergen. PLoS One. 2015 May 13;10(5):e0127477. doi:10.1371/journal.pone.0127477.
- Cone RA. Barrier properties of mucus. Adv Drug Deliv Rev. 2009 Feb 27;61(2):75–85. doi:10.1016/j.addr.2008.09.008.
- Knight DA, Stick SM, Hackett TL. Defective function at the epithelial junction: a novel therapeutic frontier in asthma? J Allergy Clin Immunol. 2011 Sep;128(3):557–558. doi:10.1016/j.jaci.2011.07.031.
- Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med. 2010 Dec 2;363(23):2233–2247. doi:10.1056/NEJMra0910061.
- Wan H, Winton HL, Soeller C, Tovey ER, Gruenert DC, Thompson PJ, Stewart GA, Taylor GW, Garrod DR, Cannell MB, et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J Clin Invest. 1999 Jul;104(1):123–133. doi:10.1172/JCI5844.
- Breiteneder H, Mills EN. Molecular properties of food allergens. J Allergy Clin Immunol. 2005 Jan;115(1):14–23; quiz 24. doi:10.1016/j.jaci.2004.10.022.
- Proud D, Leigh R. Epithelial cells and airway diseases. Immunol Rev. 2011 Jul;242(1):186–204. doi:10.1111/j.1600-065X.2011.01033.x.
- Carder M, Seed MJ, Money A, Agius RM, van Tongeren M. Occupational and work-related respiratory disease attributed to cleaning products. Occup Environ Med. 2019 Aug;76(8):530–536. doi:10.1136/oemed-2018-105646.
- Fuseini H, Newcomb DC. Mechanisms driving gender differences in asthma. Curr Allergy Asthma Rep. 2017 Mar;17(3):19. doi:10.1007/s11882-017-0686-1.
- Undem BJ, McAlexander M, Hunter DD. Neurobiology of the upper and lower airways. Allergy. 1999;54(s57):81–93. doi:10.1111/j.1398-9995.1999.tb04409.x.
- Chakraborty S, Castranova V, Perez MK, Piedimonte G. Nanoparticles-induced apoptosis of human airway epithelium is mediated by proNGF/p75NTR signaling. J Toxicol Environ Health A. 2017;80(1):53–68. doi:10.1080/15287394.2016.1238329.
- Ganesan S, Comstock AT, Sajjan US. Barrier function of airway tract epithelium. Tissue Barriers. 2013 Oct 1;1(4):e24997. doi:10.4161/tisb.24997.
- De Boer WI, Sharma HS, Baelemans SM, Hoogsteden HC, Lambrecht BN, Braunstahl GJ. Altered expression of epithelial junctional proteins in atopic asthma: possible role in inflammation. Can J Physiol Pharmacol. 2008 Mar;86(3):105–112. doi:10.1139/Y08-004.
- Vinhas R, Cortes L, Cardoso I, Mendes VM, Manadas B, Todo-Bom A, Pires E, Veríssimo P. Pollen proteases compromise the airway epithelial barrier through degradation of transmembrane adhesion proteins and lung bioactive peptides. Allergy. 2011 Aug;66(8):1088–1098. doi:10.1111/j.1398-9995.2011.02598.x.
- Nawijn MC, Hackett TL, Postma DS, van Oosterhout Aj, Heijink IH, van Oosterhout AJM. E-cadherin: gatekeeper of airway mucosa and allergic sensitization. Trends Immunol. 2011 Jun;32(6):248–255. doi:10.1016/j.it.2011.03.004.
- Heijink IH, Postma DS, Noordhoek JA, Broekema M, Kapus A. House dust mite-promoted epithelial-to-mesenchymal transition in human bronchial epithelium. Am J Respir Cell Mol Biol. 2010 Jan;42(1):69–79. doi:10.1165/rcmb.2008-0449OC.
- Bartis D, Mise N, Mahida RY, Eickelberg O, Thickett DR. Epithelial-mesenchymal transition in lung development and disease: does it exist and is it important? Thorax. 2014 Aug;69(8):760–765. doi:10.1136/thoraxjnl-2013-204608.
- Ijaz T, Pazdrak K, Kalita M, Konig R, Choudhary S, Tian B, Boldogh I, Brasier AR. Systems biology approaches to understanding Epithelial Mesenchymal Transition (EMT) in mucosal remodeling and signaling in asthma. World Allergy Organ J. 2014 Jun 2;7(1):13. doi:10.1186/1939-4551-7-13.
- Cecchi L, D’Amato G, Annesi-Maesano I. External exposome and allergic respiratory and skin diseases. J Allergy Clin Immunol. 2018 Mar;141(3):846–857. doi:10.1016/j.jaci.2018.01.016.
- Yüksel H, Öcalan M. Measurement of airway epithelial permeability: methods and protocols. Methods Mol Biol. 2021;2367:149–163.
- Heijink IH, Kies PM, Kauffman HF, Postma DS, van Oosterhout Aj, Vellenga E, van Oosterhout AJM. Down-regulation of E-cadherin in human bronchial epithelial cells leads to epidermal growth factor receptor-dependent Th2 cell-promoting activity. J Immunol. 2007 Jun 15;178(12):7678–7685. doi:10.4049/jimmunol.178.12.7678.
- Masszi A, Fan L, Rosivall L, McCulloch CA, Rotstein OD, Mucsi I, Kapus A. Integrity of cell-cell contacts is a critical regulator of TGF-beta 1-induced epithelial-to-myofibroblast transition: role for beta-catenin. Am J Pathol. 2004 Dec;165(6):1955–1967. doi:10.1016/S0002-9440(10)63247-6.
- Blume C, Swindle EJ, Gilles S, Traidl-Hoffmann C, Davies DE. Low molecular weight components of pollen alter bronchial epithelial barrier functions. Tissue Barriers. 2015 Jul 15;3(3):e1062316. doi:10.1080/15476286.2015.1062316.
- Moheimani F, Hsu AC, Reid AT, Williams T, Kicic A, Stick SM, Hansbro PM, Wark PA, Knight DA. The genetic and epigenetic landscapes of the epithelium in asthma. Respir Res. 2016 Sep 22;17(1):119. doi:10.1186/s12931-016-0434-4.
- Bourdin A, Gras D, Vachier I, Chanez P. Upper airway x 1: allergic rhinitis and asthma: united disease through epithelial cells. Thorax. 2009 Nov;64(11):999–1004. doi:10.1136/thx.2008.112862.
- Heijink IH, Nawijn MC, Hackett TL. Airway epithelial barrier function regulates the pathogenesis of allergic asthma. Clin Exp Allergy. 2014;44(5):620–630. doi:10.1111/cea.12296.
- Holgate ST. The epithelium takes centre stage in asthma and atopic dermatitis. Trends Immunol. 2007 Jun;28(6):248–251. doi:10.1016/j.it.2007.04.007.
- Yuksel H, Ocalan M, Yilmaz O. E-Cadherin: an important functional molecule at respiratory barrier between defence and dysfunction. Front Physiol. 2021 Oct 4;12:720227. doi:10.3389/fphys.2021.720227.
- Wan Y, Shang J, Graham R, Baric RS, Li F, Gallagher T. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020 Mar 17;94(7):e00127–20. doi:10.1128/JVI.00127-20.
- Sivabakya TK, Srinivas G. Lung barrier function in COVID-19? SN Compr Clin Med. 2020 Aug;18:1–3.
