Abstract
Intracerebral hemorrhage (ICH) is an important public health problem associated with high mortality and morbidity. The aim of this study was to evaluate the clinical efficacy of integrated traditional Chinese (TCM) and Western medicine (WM) therapy for acute hypertensive ICH. Randomized controlled trials were searched in PubMed, Medline, Embase, Wanfang and CNKI database published between January 2000 and June 2016. Our results showed that integrated TCM and WM therapy appeared to be able to improve the clinical effect for patients with acute hypertensive ICH.
Introduction
Intracerebral hemorrhage (ICH) is intra-parenchymal bleeding with localized hematoma formation, which can enlarge over a period of time and directly contribute to neurological deterioration (Alqadri and Qureshi Citation2012). It is a devastating disease with high mortality and morbidity, accounting for about 10–15% of all the strokes (Keep et al. Citation2012). ICH is more common in elderly people and in those of African or Asian ethnicity. Every year, the overall incidence is 12 to 15 cases per 100,000 population (Gebel and Broderick Citation2000). The major risk factors for ICH are chronic arterial hypertension and oral anticoagulation (Elliott and Smith Citation2010). Of which, chronic hypertension-initiated ICH secondary to pathologic changes is responsible for 75% of all the cases of primary ICH. Early management focusing on treatment of intracranial complications and reduction of ICH volume might be useful for improving clinical outcome.
Surgical treatment is a likely benefit for those patients with altered consciousness or neurological deterioration. A meta-analysis conducted by Prasad et al. indicated that surgical treatment could reduce the chances of death or disability (Prasad et al. Citation2009). However, another clinical trial conducted by Mendelow et al. failed to show a benefit of surgery over conservative treatment in acute ICH (Mendelow et al. Citation2005). Therefore, there is an urgent need to develop effective therapeutic approaches to improve the clinical outcome of ICH.
Traditional Chinese medicine (TCM) therapies including acupuncture, herbal medicine, and other non-medication therapies have been used for treating patients with stroke for thousand years (Lu et al. Citation2012; Gong and Sucher Citation2002). Although TCMs have a long tradition of therapeutic benefit for a wide variety of conditions in China, and similarly for the popularity of neuroprotectives in the targeting brain function, they are not recommended in current national stroke guidelines. Western medicine (WM) has long influenced large regions outside the West. Study has shown that WM treatment may have a positive effect on improving the motor function of stroke patients (Lee et al. Citation2013). While for ICH, the incidence is substantially increased in those receiving anticoagulant therapy. Overall, WM are favorable in acute disease situations; TCM offer more opportunities in chronic conditions and for prevention (van der Greef et al. Citation2010). Connecting WM and TCM may be an essential therapy to treat ICH cases. The purpose of this study was to evaluate the efficacy and safety of TCM combined with WM therapy for acute hypertension ICH.
Materials and methods
Literature search
We conducted a comprehensive literature search for relevant reports published between January 2005 and June 2015 using the electronic database of PubMed, Medline, Embase, Wanfang and CNKI (China National Knowledge Infrastructure). We retrieved the related articles using the following terms: “acute intracerebral hemorrhage or ICH”, “hypertensive”, “traditional Chinese medicine”, “Western medicine” and “integrated or combined” as well as their combinations. The corresponding Chinese terms were used in the Chinese library. References of retrieved articles were searched with no language restrictions.
Criteria for inclusion
The inclusion criteria were as follows: (1) the paper should be randomized controlled clinical trials evaluating the effect of TCM combined with WM therapy on acute hypertension ICH; (2) patients with acute hypertension ICH should meet the following standard: diagnosis of ICH was made on the basis of the Chinese national criteria of cerebral hemorrhage in Diagnostic Essentials of Various Cerebrovascular Diseases revised at the Fourth National Conferences in 1996 (Chen Citation1996); diagnosis of hypertension was made on the basis of the ‘‘Definition and Classification of Hypertension’’ from 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension (Organization WH, Group ISoHW, Citation2003); (3) the patients of the control group were given modern Western conventional treatments; (4) the patients in trial groups were given TCM therapy in addition to the baseline medication similar to the control groups, and the TCM therapy only included herbal medicine; and (5) the primary outcome measurement was clinical effective rate and neurological deficit scores; the secondary outcome measurement was mortality and adverse events at the end of long-term follow-up of at least 2 weeks.
Data extraction
Two investigators independently assessed the quality of the included studies according to the descriptions provided by the authors of the included trials. Any disagreement was subsequently resolved by discussion with a third author. The following information was extracted from each article: first-author, publication year, mean age, total number, neurological deficit score and Glasgow coma scale before treatment.
Statistical analysis
The I2 test was used to assess the proportion of statistical heterogeneity and the Q-statistic test was used to define the degree of heterogeneity. A P value less than 0.10 for the Q-test and I2 more than 50% was considered significant among the studies. The fixed-effects model is used when the effects are assumed to be homogenous, while the random-effects model is used when they are heterogenous. The odd ratio (OR) and risk ratio (RR) with their corresponding 95% confidence intervals (95% CIs) were employed to assess the effect. If continuous data were available, weighted mean difference or standardized mean difference was to be calculated. The Z test was employed to determine the significance of the pooled ORs, and a P value less than 0.05 was considered statistically significant. The figures were obtained from the statistical software in Review Manager (version 5.2, The Cochrane Collaboration)
Results
Study selection
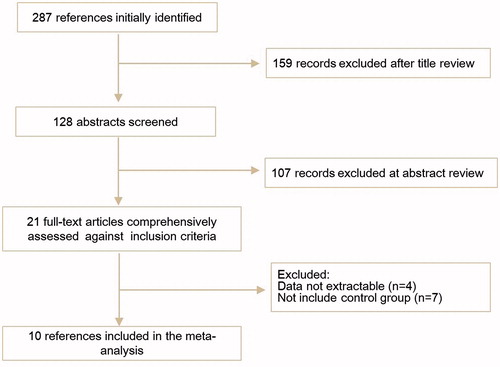
The electronic database search identified 287 references. After applying the inclusion criteria, 10 articles including 976 ICH cases were ultimately included in the systematic review and meta-analysis. The study selection process was shown in .
All the 10 reports were conducted in Chinese and published between 2001 and 2014 (Chen Citation2007, Feng and Lou Citation2013, Jin Citation2014, Liang and Zhang Citation2006, Liu Citation2001, Liu and Liu Citation2010, Sun et al. Citation2012, Wang et al. Citation2009, Wang Citation2011, Wen et al. Citation2012). The mean ages of patients were above 54 and all of them had undergone a CT/MRI scanning to confirm the diagnosis. The detailed characteristics of the studies included were shown in .
Table 1. Main characteristics of the included studies.
Clinical outcome
Clinical effective rate
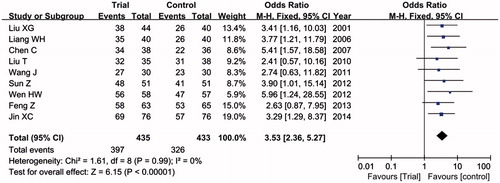
Nine articles reported the clinical effective rate. No significantly heterogeneity was found among studies (I2 = 0, P = 0.99), and the fixed-effects model was employed to assess the effective rate. Overall, the clinical effective rate was higher in patients with trial group than that in control group (91.3% versus 75.3%). As shown in , we found that TCM in combination with WM therapy had further improved the clinical effective rate in patients with acute hypertensive ICH when comparing with WM control (OR = 3.53, 95% CI = 2.36–5.27, P < 0.00001).
Neurological deficit improvement
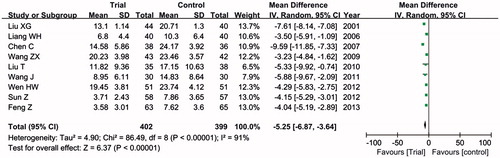
Data extracted from nine studies displayed the neurological deficit scores and showed heterogeneity in the consistency of the trial results (P < 0.01, I2 > 50%), so the random-effects model was used to evaluate the neurological deficit improvement. As shown in , the combined effects of nine independent trial results demonstrated that patients with acute hypertensive ICH receiving TCM combined with WM therapy had significantly improved neurological deficit scores when compared with the control group (MD = −5.25, 95% CI = −6.87, −3.64, P < 0.00001).
The volume of ICH reduction
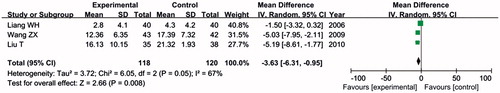
Three studies showed the volume of ICH before and after treatment. As shown in , the combined effects indicated that patients with acute hypertensive ICH in trial group had significantly reduced the volume of hemorrhage when compared with the control group (MD = −3.63, 95% CI = −6.31, −0.95, P = 0.008) in random-effects model.
Adverse events
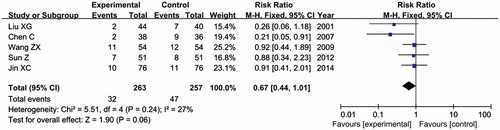
Mortality and rehemorrhage
Five trials reported these outcome measures. The frequency of mortality in trial group was little than that in control group (12.2% versus 18.3%). Overall, there was no significant difference in both groups (RR = 0.67, 95% CI = 0.44–1.01, P = 0.06) as shown in .
Only two studies reported the rehemorrhage. There was no significant difference in two groups as well (OR = 1.09, 95% CI = 0.49–2.41, P = 0.84).
Other adverse events
One study showed the fever in four cases, other studies did not show any other adverse events, so we cannot perform statistical analysis.
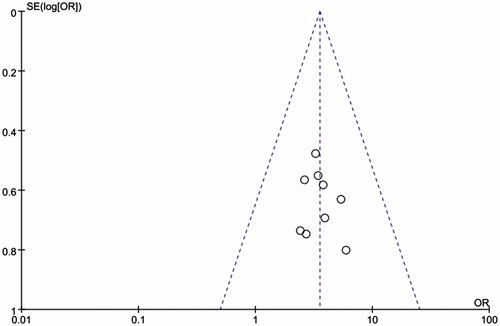
Sensitivity analysis and publication bias
For this meta-analysis, the influence of a single study on the overall meta-analysis estimate was investigated by omitting one study at a time, respectively. The OR was not significantly influenced by omitting any single study. But when study of Liu XG et al. was excluded from this meta-analysis, the heterogeneity between studies was decreased (I2 = 71%, P = 0.0.001).
The funnel plot for this meta-analysis of the effect of regional or general anesthesia in patients with hip fracture surgery revealed no evidence of asymmetry (P > 0.10; ). Thus, there was no publication bias in this meta-analysis.
Discussion
ICH remains a major public health problem with high rates of mortality, morbidity, and disability. Following the initial hemorrhage, hematoma expansion and perihematoma edema result in secondary brain damage and worsened outcome. Up to now, there has not been significant improvement in outcomes (Freeman and Aguilar Citation2012). Our study is the first meta-analysis evaluating the clinical outcome of TCM combined with WM therapy for acute hypertensive ICH. The results indicate that TCM combined with WM therapy appears to be effective for improving clinical effective rate and neurological deficit scores, reducing the volume of hemorrhage in patients with acute hypertensive ICH.
China has a relatively higher incidence of hemorrhagic stroke than Western countries do. The distinction of therapeutic strategy for stroke between China and the West is the use of TCM. TCM is useful model for scientific therapies and has been practice worldwide (Lao et al. Citation2012). It is a holistic approach and healthcare-focused medical system, showing great advantages in early intervention, combination therapies and personalized medicine. TCM has rich experience over 3000 years of continuous practice and refinement through observations, testing and critical thinking in treating ill-health, attempting to bring the body, mind and spirit into harmony (Gao Citation2013). Nowadays, TCM is getting more and more popular in improving health condition of human beings and preventing or healing diseases. However, due to lack of scientific, technologic approaches and poor understanding of TCM regimens, TCM faces severe challenges and suffers from insufficient modern research, restricting the development of TCM in the world.
Western medicine was first introduced into China from the middle of the seventeenth century. More and more people realize that both TCM and WM have their own merits and advise that the two systems should benefit from each other's strong points. Therefore, a new approach of integrating TCM with WM is a right orientation for developing in China (Jingfeng Citation1988; Keji and Hao Citation2003). Several researches have studied the role of integrated TCM and WM therapy in treatment of diseases. Zhang et al. have demonstrated that integrated TCM and WM has some positive effects on lung infiltrate absorption in SARS patients, and is recommended as an adjunct treatment for SARS (Zhang et al. Citation2004). Li et al. have found that it is strongly significant to pay close attention to TCM therapeutics and natural medicines for treatment of diabetes mellitus and its complications (Li et al. Citation2004). Liu et al. have proved that integrated TCM and WM is effective for most severe acute pancreatitis cases (Liu et al. Citation2004). Sucher et al. have shown that the combination of principles of modern molecular medicine with certain ideas of traditional empirical Chinese medicine may be beneficial in translational medicine in general (Sucher Citation2006).
TCM has also played an important role in stroke patients for thousands of years. Currently, various unconventional local therapeutic traditions are widely used for stroke treatment in China. TCM is widely used in Taiwan and other Asian countries. Traditional Chinese herbal medicine has been described in ancient medicine systems as a treatment for various ailments associated with stroke (Chen Citation2011). Liao et al. showed that TCM is popular and well accepted in Taiwan, and patients with stroke have a higher TCM utilization rate than people without stroke (Liao et al. Citation2012). Gong et al. demonstrated that TCM provides an extensive and knowledge-rich foundation for implementing a strategically focused pharmacological research program aimed at the development of new drugs (Gong and Sucher Citation1999). Zheng et al. found that scalp acupuncture therapy is widely used to treat acute hypertensive ICH in TCM (Zheng et al. Citation2011). However, a meta-analysis conducted by Wu et al. found that there was insufficient good quality evidence on the effects of traditional Chinese patent medicine in ischemic stroke on the primary outcome (death or dependency) (Wu et al. Citation2007).
Furthermore, hypertension is the main risk factor of developing IHC, and over 50% of cases have a history of it (Thrift et al. Citation1998). Numerous studies have assessed the efficiency of TCM for treating hypertension, and provided the best evidence supporting the use of TCM for patients who suffer from hypertension (Wang et al. Citation2012; Xiong et al. Citation2012). Most of them have positive findings that favor the practice of TCM. These studies reveal the multi-protective mechanisms of Chinese herbal formulas for treating hypertension. Study conducted by Luiz et al. showed a strong association between TCM syndrome and hypertension (Luiz et al. Citation2011). A recent study system elaborated the Chinese herbal formulas for treating hypertension in traditional Chinese medicine (Xiong et al. Citation2013). Therefore, there is a great possibility for TCM in treating hypertension-induced disease.
In conclusion, our results indicate that integrated TCM and WM therapy is a potentially promising approach for improvement of clinical effective rate, recovery of neurological deficits and reduction of hemorrhage volume which induced by acute hypertensive ICH. However, well-designed clinical trials are needed to further evaluate the clinical outcomes.
Disclosure statement
All authors declared no conflict of interest.
References
- Alqadri SL, Qureshi AI. 2012. Management of acute hypertensive response in patients with intracerebral hemorrhage. Curr Atheroscler Rep. 14:322–327.
- Chen C. Clinical Research on middle-Multiplicity Hypertensive Cerebral Hemorrhage of the Cooperation of Chinese and Western Medicine. Guangzhou: Guangzhou University of Chinese Medicine. 2007.
- Chen QT. 1996. Classification, diagnostic criteria and evaluation of neurological impairment for stroke patients. Neurosci Soc Chinese Soc Neurosurg. 29:379–380.
- Chen Y. 2011. Traditional Chinese herbal medicine and cerebral ischemia. Front Biosci (Elite Ed) 4:809–817.
- Elliott J, Smith M. 2010. The acute management of intracerebral hemorrhage: a clinical review. Anesth Analg. 110:1419–1427.
- Feng Z, Lou Y. 2013. Curative effect observation of the integrative medicine on treating cerebral hemorrhage. Clinical J Chinese Med. 5:8–10.
- Freeman WD, Aguilar MI. 2012. Intracranial hemorrhage: diagnosis and management. Neurol Clin. 30:211–240.
- Gao D. Traditional Chinese Medicine: The Complete Guide to Acupressure, Acupuncture, Chinese Herbal Medicine, Food Cures and Qi Gong. London: Carlton Books; 2013.
- Gebel JM, Broderick JP. 2000. Intracerebral hemorrhage. Neurol Clin. 18:419–438.
- Gong X, Sucher N. 2002. Stroke therapy in traditional Chinese medicine (TCM): prospects for drug discovery and development. Phytomedicine. 9:478–484.
- Gong X, Sucher NJ. 1999. Stroke therapy in traditional Chinese medicine (TCM): prospects for drug discovery and development. Trends Pharmacol Sci. 20:191–196.
- Jin X. 2014. Combining traditional Chinese and western medicine therapy for hypertension cerebral hemorrhage in 76 cases. Chinese Med Modern Distance Educ China. 11:34–35.
- Jingfeng C. 1988. Integration of traditional Chinese medicine with Western medicine—right or wrong? Soc Sci Med. 27:521–529.
- Keep RF, Hua Y, Xi G. 2012. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 11:720–731.
- Keji C, Hao X. 2003. The integration of traditional Chinese medicine and Western medicine. Eur Rev. 11:225–235.
- Lao L, Xu L, Xu S. Traditional Chinese Medicine. Integrative Pediatric Oncology. Beijing: Springer; 2012. pp. 1251–35.
- Lee J, Lee E, Woo S, Cho K. 2013. Comparative study of combination therapy of Korean–/INS; Western medical treatment versus Western medical treatment only in acute ischemic stroke patients. J Neurol Sci. 333:e221–e2e2.
- Li W, Zheng H, Bukuru J, De Kimpe N. 2004. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J Ethnopharmacol. 92:1–21.
- Liang W, Zhang W. 2006. Clinical observation of integrated traditional Chinese and Western medicine therapy for hypertensive cerebral hemorrhage. Shanxi J Traditional. 22:32–33.
- Liao C-C, Lin J-G, Tsai C-C, Lane H-L, Su T-C, Wang H-H, et al. 2012. An investigation of the use of traditional Chinese medicine in stroke patients in Taiwan. Evidence-Based Complement Alternat Med. 2012:387164.
- Liu T, Liu Y. 2010. 35 cases of hypertensive cerebral hemorrhage treated by combined Chinese and Western medicine. Liaoning J Tradition Chinese Med. 37:1556–1557.
- Liu X, Jiang J, Huang Z, Tian B, Hu W, Xia Q, et al. 2004. Clinical study on the treatment of severe acute pancreatitis by integrated traditional Chinese medicine and Western medicine. Sichuan Da Xue Xue Bao Yi Xue Ban = J Sichuan Univ Med Sci Ed. 35:204–208.
- Liu X. 2001. 44 cases of hypertensive cerebral hemorrhage treated by combined Chinese and Western medicine. Hunan Guiding J TCMP. 7:157.
- Lu A, Jiang M, Zhang C, Chan K. 2012. An integrative approach of linking traditional Chinese medicine pattern classification and biomedicine diagnosis. J Ethnopharmacol. 141:549–556.
- Luiz AB, Cordovil I, Barbosa Filho J, Ferreira AS. 2011. Zangfu zheng (patterns) are associated with clinical manifestations of zang shang (target-organ damage) in arterial hypertension. Chinese Med. 6:23.
- Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. 2005. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. The Lancet. 365:387–397.
- Organization WH, Group ISoHW. 2003. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertension. 21:1983–1992.
- Prasad K, Mendelow AD, Gregson B. 2009. Surgery for primary supratentorial intracerebral hematoma a meta-analysis of 10 randomized controlled trials. Stroke. 40:e624–e6e6.
- Sucher NJ. 2006. Insights from molecular investigations of traditional Chinese herbal stroke medicines: Implications for neuroprotective epilepsy therapy. Epilepsy Behav. 8:350–362.
- Sun Z, Yang R, Zhang H. 2012. Combing traditional Chinese and western medicine treatment for hypertension cerebral hemorrhage in 51 cases. Chinese J Exp Formulas Chinese Med. 18:271–273.
- Thrift AG, McNeil JJ, Forbes A, Donnan GA. 1998. Three important subgroups of hypertensive persons at greater risk of intracerebral hemorrhage. Melbourne Risk Factor Study Group. Hypertension. 31:1223–1229.
- van der Greef J, van Wietmarschen H, Schroën J, Wang M, Hankemeier T, Xu G. 2010. Systems biology-based diagnostic principles as pillars of the bridge between Chinese and Western medicine. Planta Medica. 76:2036.
- Wang J, Yao K, Yang X, Liu W, Feng B, Ma J, et al. 2012. Chinese patent medicine liu wei di huang wan combined with antihypertensive drugs, a new integrative medicine therapy, for the treatment of essential hypertension: a systematic review of randomized controlled trials. Evidence-Based Complement Alternat Med. 2012:714805.
- Wang J. The Clinical Study of Acute Hypertensive Cerebral Hemorrhage Treated with Combination of Chinese Traditional and Western Medicine. Dalian: Dalian Medical University. 2011.
- Wang Z, Zhang Z, Luo P. 2009. Clinical effect of combining traditional Chinese and western medicine therapy for hypertensive cerebral hemorrhage. Prac Clin J Integr Tradition Chinese West Med. 9:9–11.
- Wen H, Li Y, Zhang Y. 2012. Clinical observation of integrated traditional Chinese and western medicine therapy for hypertensive intracerebral hemorrhage. Chinese J Inform Tradition Chinese Med. 19:79–80.
- Wu B, Liu M, Liu H, Li W, Tan S, Zhang S, et al. 2007. Meta-analysis of traditional Chinese patent medicine for ischemic stroke. Stroke. 38:1973–1979.
- Xiong X, Yang X, Liu W, Feng B, Ma J, Du X, et al. 2012. Banxia baizhu tianma decoction for essential hypertension: a systematic review of randomized controlled trials. Evidence-Based Complement Alternat Med. 2012:271462.
- Xiong X, Yang X, Liu Y, Zhang Y, Wang P, Wang J. 2013. Chinese herbal formulas for treating hypertension in traditional Chinese medicine: perspective of modern science. Hypertension Res. 36:570–579.
- Zhang M-M, Liu X-M, He L. 2004. Effect of integrated traditional Chinese and Western medicine on SARS: a review of clinical evidence. World J Gastroenterol. 10:3500–3505.
- Zheng G-q, Zhao Z-M, Wang Y, Gu Y, Li Y, Chen X-m, et al. 2011. Meta-analysis of scalp acupuncture for acute hypertensive intracerebral hemorrhage. J Altern Complement Med. 17:293–299.