Abstract
Purpose: The aim of this study was to investigate the effects of a multidisciplinary group information as a part of a Stepped Care tinnitus management model. The Tinnitus Handicap Inventory (THI) and the Hospital Anxiety and Depression Scale (HADS) were administered before and after the group information to evaluate the effects.
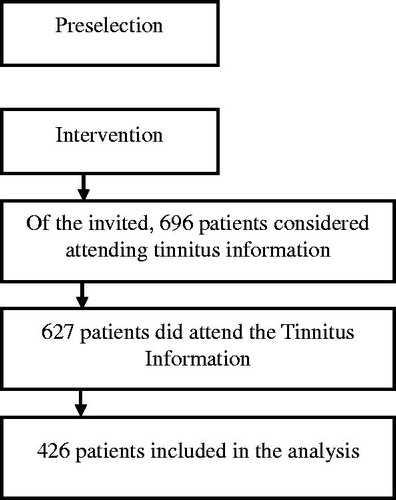
Method: In total, 627 patients participated in half-day tinnitus information meetings from 2004 to 2011 in our clinic. We retrieved 426 patients for analysis with complete scores on the THI, HADS, and a questionnaire covering background information. These three questionnaires were used before the information meeting, and the THI and HADS at a 1-month follow-up.
Results: Significant decreases were found in scores on the THI (p < .001) and the HADS-A (p < .05), pre- and post-information session. However, no significant changes were observed on the HADS-D.
Conclusion: An information meeting as a part of multidisciplinary Stepped Care model can be an effective initial approach to manage tinnitus, and serve as a filter for patients who need additional treatment.
Introduction
Tinnitus is the perception of sound(s) without an audible external source. It is widely regarded as a symptom, rather than a disease on its own [Citation1]. The overall prevalence of tinnitus in the general adult population is about 10–15%, with 1–3% of the population having severe, distressing tinnitus [Citation2]. There are many proposed etiologies of tinnitus and, although several treatment options have been tested, no single cure exists for the condition [Citation3]. However, there is evidence in favour of cognitive-behavioural therapy (CBT) as a way to reduce the distress associated with tinnitus [Citation4,Citation5]. The prevalence of tinnitus increases with age [Citation6], with a peak at 14.3% in people between 60 and 69 years of age [Citation2]. Hence, tinnitus is often accompanied by some degree of hearing impairment [Citation7], which in many cases is a sensorineural hearing loss, either cochlear or retrocochlear [Citation3].
Tinnitus is usually perceived only by the patient (with the exception of objective tinnitus). Thus, all diagnosis and treatment of tinnitus rely on self-report once hearing tests, and if needed, other audiological examinations have been completed. There are many questionnaires available, but the Tinnitus Handicap Inventory (THI) [Citation8] is a widely used instrument in many clinical settings and has gained recognition as a useful tool for quantifying the impact of tinnitus on daily life [Citation9].
The level of tinnitus annoyance varies among persons with tinnitus [Citation10,Citation11], and overall quality of life can be affected [Citation7,Citation12,Citation13]. Severe tinnitus can disturb daily activities and reduce quality of life. Psychological distress such as depression, anxiety and sleep disturbance is also commonly reported among patients with severe tinnitus [Citation14].
The notion of a multiprofessional approach to the management of tinnitus has been suggested by many researchers and clinicians over the years [Citation15–17], including specialized services [Citation18]. To reduce tinnitus annoyance, all factors contributing to tinnitus disturbance should be addressed during management. A multidisciplinary management approach is often necessary and could be helpful for patients with complex symptomatology [Citation3]. Outcomes could be improved by using techniques such as education, counselling and empathetic support along with potential pharmacological or other treatment protocols [Citation19]. However, it can be difficult to select the appropriate staff in a multidisciplinary team as there may be a variation of professions involved, their skills and experience of tinnitus including referral patterns [Citation20].
The management of adults with tinnitus in the two hearing clinics in Östergötland County (population around 400,000), Sweden, consists of a detailed medical evaluation before specific treatment routines, and has been running since 2004. A multidisciplinary team approach, using a team consisting of audiologist, psychologist, otolaryngologist and a counsellor, is used to meet the needs of the patient. This approach allows a framework for organization of health services on the basis of individual needs of patients, with a gradual increase in the intensity of care at each level. Such treatment strategy is sometimes referred to as Stepped Care [Citation21]. Stepped Care, adapted for tinnitus management, has several elements, including an investigation with short information about the audiological findings and also screening questions about tinnitus performed by an audiologist (Step 1). It should be stressed that all patients are examined before this first step to rule out organic causes of tinnitus such as vestibular schwannoma [Citation22], and if such problems are detected further medical examinations such as magnetic resonance imaging. If there are no organic causes in need of examinations (including other disorders not necessarily related to tinnitus), the patient is seen for a tinnitus session. If the patients are satisfied with the first step no further treatment is provided. If not, patients are offered to take part in an information meeting organized by a multidisciplinary team (Step 2). Sometimes, if patients need more resources, then group CBT or individual therapy with the counsellor and/or psychologist can be recommended after the information meeting (Step 3). Other forms of additional treatment such as fitting of new hearing aids can also follow at Step 3.
The aim of this study was to evaluate the effects the multidisciplinary group information as a part of a Stepped Care model, using THI and Hospital Anxiety and Depression Scale (HADS) [Citation23] before and 1 month after group information.
Method
Participants
The study was based on data from consecutive patients who sought care for tinnitus at the two hearing clinics in Östergötland County, Sweden, during 2004–2011 and were diagnosed with subjective tinnitus. Patients who did not speak fluent Swedish and had an interpreter during the hearing clinics visit were excluded ().
Ethical considerations
No ethical permission application was sought for this study because of the rules for monitoring of existing treatment models within the public health care and no additional procedures apart from clinical regular practice were evaluated (e.g. no randomization). The Declaration of Helsinki was followed.
Outcome measures
Three self-report measures were used on a routine basis. A questionnaire covering demographics, tinnitus duration, location and characteristics as well as beliefs about future tinnitus change was used. Hearing loss, sensitivity to and fear of noise, and the potential masking of tinnitus by external sounds were also investigated. Finally, occupational status and earlier tinnitus treatments were addressed.
THI. THI is a commonly used tinnitus-specific questionnaire, designed to examine the functional, emotional and catastrophic response reactions to tinnitus [Citation8]. It contains 25 items, each scores on a three-degree scale (4/2/0 points per item) yielding a score of 0–100. The THI has a good internal consistency for the total scale with an α of .93 and almost as good internal consistencies for the functional and emotional scales (α of .86 and .87, respectively). The catastrophic scale has a lower α value of .68. We used the total scale in this report as the scale most likely measures one factor [Citation24]. Scores on the THI can be categorized into four different categories of distress based on quartiles calculated by Newman et al. [Citation9]. The ranges and labels of the categories are: 0–16, no handicap; 18–36, mild handicap; 38–56, moderate handicap; 58–100, severe handicap.
HADS. HADS is a self-report measure developed by Zigmond and Snaith [Citation23] used for the screening of symptoms of depression and anxiety levels in patients with somatic illnesses. To differentiate the psychological or ‘mood’ state from physical conditions the test omits questions regarded associated somatic conditions, for example, dizziness and headache. The HADS includes 14 items, where each of the questions has four response choices (0–3). There are two subscales, one for anxiety (HADS A) and one for depression (HADS D), consisting of seven items each. Higher scores indicate more symptoms. The results can be interpreted as; 0–7 no risk for anxiety/depression (low), 8–10 anxiety and depression is possibly present, ≥11 suggests that anxiety/depression exist (high) [Citation23].
Procedure
Initial assessment. The hearing clinics in Östergötland County receive patients from surrounding districts by referral from a physician or by self-referral. An audiologist or an ENT physician sorted the referrals based on the clinical presentation. Patients with severe tinnitus annoyance who needed immediate help were contacted directly, usually a phone call the same day, and were offered an audiological evaluation by an audiologist as soon as possible.
Audiological investigations were conducted with the audiological evaluation protocols used routinely for patients with hearing loss who attend the ENT clinic. Pure tone audiometry (PTA; 0.125–8 kHz) using an Aurical audiometer (Control Panel MADSEN 2-Kanal, GN Otometrics, Taastrup, Denmark) was performed in a sound-proof room. A standardized questionnaire was filled out by the audiologist after the audiological investigation, where questions about patients’ medical history were asked (e.g. possible medication, sleep disturbance, noise exposure and vertigo). In case of asymmetric hearing loss, vertigo or other clinically relevant findings or eardrum pathologies, a physician specialized in ENT was consulted. The test results were explained for all patients who then were given the choice to undertake hearing aid fitting. For patients who choose to begin hearing rehabilitation at the clinic, the choice of hearing aid was based on audiological findings.
The level of hearing loss was described according to the American Speech-Language-Hearing Association (ASHA) definition (ASHA 2011). Normal hearing was referred to as a PTA between −10 and 15 dB HL, a slight hearing loss (PTA) between 16 and 25 dB HL. A mild hearing loss was greater than 26 dB (PTA >26dB) up to 40 dB, moderate hearing loss 41 > PTA <55. A severe moderate hearing loss was defined if 56 > PTA <70, a severe hearing loss if 71 > PTA< 90, and a profound hearing loss was defined as PTA >91.
Furthermore, patients’ hearing loss was classified as a unilateral hearing loss when one of the ears was within normal limits, i.e. pure tone average (PTA, average of 0.5, 1, 2 and 4 kHz) was ≤20 dB HL, and the PTA of the other ear was >20 dB HL. Bilateral hearing loss was defined as a hearing loss where PTA for both ears was >20 dB HL and could either be symmetric or asymmetric hearing loss. A hearing loss was classified as an asymmetric hearing loss if the difference between the PTA for the two ears was larger than 15 dB HL.
Intervention. Following the medical and audiological examinations including the three questionnaires (see below), the team leader (counsellor) made a decision to invite the tinnitus patient to tinnitus information or not, sometimes consulting other team members such as the audiologist who had seen the patient.
Tinnitus information. The patients were sent the self-report instruments 3 weeks before the group information with return envelope. The subsequent group information (in small groups of 15–30 patients) involved a multidisciplinary team consisting of two audiologists, a social worker, a psychologist/research professor, an ENT physician/medical audiologist, and during the first meetings a physiotherapist. Information was given of potential causes and different degrees of tinnitus, available methods of measurement, treatment options, and efficacy and effectiveness of different treatment methods. The impact of tinnitus annoyance on work, relations, sleep and mental health was also covered. The patients then participated in a Questions and Answers (Q&A) session and could ask questions on different aspects of tinnitus which were handled by the multidisciplinary team. The session usually lasts for 3 h with a coffee break for 20 min before starting up the Q&A section. The group session was evaluated with the help of self-report questionnaires sent to the patients 4 weeks after the group information. They could also ask for additional help as part of the Stepped Care procedure. In addition, participants for subsequent group CBT [Citation25] were recruited at this stage.
Statistical analyses
Pre- and post-information session ratings were compared with Student’s t-test and Wilcoxon signed rank test. Variables are presented in the tables as means and SD, except for the median value in one variable with a skewed data distribution. The values at baseline and values at follow-up are given for each group. The level of significance was set at p < .05.
Results
Patient characteristics
In total, there were 426 patients included in the analysis of this study (complete data available at both pre- and post-information session). Background data for all patients are presented in . There were 211 females (49.5%) who participated in this study. The mean age of the whole group was 54.67 (SD = 13.45) years. There were 299 patients (70.2%) who perceived hearing loss. The results showed that 196 had bilateral tinnitus (45.8%). The median value for tinnitus duration in 373 patients was 5 years, while 33 patients described their duration as ‘for a long time’ and 20 did not answer the question. Our assumption is that the median value, also including the 33 patients stating ‘for a long time’ will remain at 5 years, due to the observed data distribution. The PTA for best- and worst ear (19.14 ± 13.62 dB and 27.44 (SD = 19.76) dB for the entire group are presented in . The results for the self-reported sensitivity to sound showed that a high sensitivity to sound was, where 115 (27.0%) perceived to be quite sensitive while 124 (29.1%) stated themselves to be very sensitive (see ).
Table 1. Background data for patients (n = 426).
Changes following tinnitus information
The results showed significant changes in THI scores using paired samples t-test (p < .001) and for the anxiety subscale in the HADS questionnaire (p < .05). However, no significant changes could be seen for the subscale D in the HAD questionnaire (p < .18; see ). THI scores were divided into four handicap categories according to the quartile ranges defined by Newman et al. [Citation26] (see ). In line with the analysis of continuous data, THI categories changed between pre-treatment and follow-up (p < .0001).
Table 2. Means and SDs before and after attending the multidisciplinary tinnitus information session (n = 426).
Table 3. Pre- and post-categories of the Tinnitus Handicap Inventory.
Discussion
The aim of this study was to evaluate the effects of multidisciplinary group information as a part of a Stepped Care model for tinnitus. We evaluated the group information meeting part of Stepped Care tinnitus management, and found reductions in tinnitus distress after just one 3-h information session. Results showed that THI scores decreased significantly after attending the multidisciplinary group information.
The findings are in line with previous recommendations that a multiprofessional approach is beneficial in tinnitus management [Citation3]. Our results also showed a significant albeit small change in the anxiety subscale of the HADS. The score showed a very modest decrease from a mean of 6.7 at baseline to 6.4 at the 1-month follow-up, which has no clinical importance but still suggests that minor reductions in anxiety can occur. We did not find a significant reduction in the depression score of HADS. Depression is often a significant co-morbidity in a subgroup of ‘severe’ tinnitus sufferers, but as these patients are only a small proportion of persons with tinnitus [Citation27] floor effects are likely. This could explain the failure in clinical trials to show significant treatment effect on depression in tinnitus samples [Citation28]. A longitudinal follow-up would be desirable, which could demonstrate the possible effects of the further steps of the Stepped Care model (such as CBT) on depressive symptoms (in particular for patients with elevated levels of depression).
The Stepped Care model is believed to be an effective patient-centred treatment model that provides better access to optimal tinnitus-focused treatment and can make more resources available to patients with severe problems [Citation18]. With this method, patients could reach their optimal level of care with the appropriate caregiver more quickly. Findings from a randomized controlled trial suggest that a multidisciplinary approach could be an effective treatment method for patients with tinnitus, irrespective of the initial tinnitus severity [Citation29]. In addition, there were no adverse events in that trial [Citation29]. In addition to the benefits of working in a multidisciplinary setting, the team approach also facilitates referral to further medical examinations and interventions. For example, patients may be referred to further hearing tests, and while it is rare that more severe disorders are detected at a later stage (such as multiple sclerosis), the staff involved in tinnitus management can assist patients if they need to seek help for other medical problems not necessarily related to tinnitus.
Our study also has some limitations. Patients evaluated the effect of the group information a short time after the meeting (4 weeks), and it is possible that the symptom reductions reflect regression to the mean [Citation30]. It would be desirable to have a longitudinal follow-up at, say, at 6 or 12 months [Citation31] after the group information, to evaluate the long-term effects. Longitudinal studies could also lead to a better understanding of how tinnitus affects patients with impaired hearing and other comorbidities.
A second limitation study was the lack of control group (i.e. as usual care is practiced in many settings). The Stepped Care has been part of routine care in our ENT clinics in Östergötland since 2004, but could be compared against other management approaches such as brief individual information sessions or general advice in general practice settings.
Our findings provide initial support for role of Stepped Care management of tinnitus. Despite extensive research on tinnitus, there is still no ‘best’ management model for tinnitus that has been identified [Citation4]. Moreover, the current treatment strategies are diverse and often costly [Citation32]. The results of this study suggest that multidisciplinary group information, as a part of a Stepped Care model, can be applicable for clinical practice, and also reduce tinnitus annoyance.
Conclusions
In summary, the overall improvement in scores for THI show that a half-day information meeting held by a multiprofessional team can be effective as an early step in the management of tinnitus. Handling the information session in a larger group, instead of seeing all patients individually, presumably makes more resources available for patients in need of more intensive therapy (e.g. CBT). However, more research is needed to establish the effects, preferably in controlled studies.
Acknowledgements
We thank Karolina Rising and the tinnitus team at Linköping University Hospital including Mikael Schulin, Anna-Karin Strömberg, Mahnaz H Rudqvist, Marianne Karlsson, Elina Mäki-Torkko, and Ulrike Olofsson.
Disclosure statement
The authors have no relevant financial interest in this article. The authors alone are responsible for the content and writing of this paper.
Additional information
Funding
References
- Baguley D, McFerran D, Hall D. Tinnitus. Lancet. 2013;382:1600–1607.
- McCormack A, Edmondson-Jones M, Somerset S, et al. A systematic review of the reporting of tinnitus prevalence and severity. Hear Res. 2016;337:70–79.
- Baguley DM, Andersson G, McKenna L, et al. Tinnitus: a multidisciplinary approach. 2nd ed. Chichester: Wiley; 2013.
- Hoare D, Kowalkowski V, Kang S, et al. Systematic review and meta-analyses of randomized controlled trials examining tinnitus management. Laryngoscope. 2011;121:1555–1564.
- Hesser H, Weise C, Zetterqvist Westin V, et al. A systematic review and meta-analysis of randomized controlled trials of cognitive-behavioral therapy for tinnitus distress. Clin Psych Rev. 2011;31:545–553.
- Sindhusake D, Mitchell P, Newall P, et al. Prevalence and characteristics of tinnitus in older adults: the blue Mountains Hearing Study. Int J Audiol. 2003;42:289–294.
- Zarenoe R, Ledin T. Quality of life in patients with tinnitus and sensorineural hearing loss. B-ENT. 2014;10:41–51.
- Newman CW, Jacobson GP, Spitzer JB. Development of the Tinnitus Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1996;122:143–148.
- Newman CW, Sandridge SA, Jacobson G. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol. 1998;9:153–160.
- Hiller W, Goebel G. When tinnitus loudness and annoyance are discrepant: audiological characteristics and psychological profile. Audiol Neurotol. 2007; 12:391–400.
- Andersson G. Tinnitus loudness matchings in relation to annoyance and grading of severity. Auris Nasus Larynx. 2003;30:129–133.
- Cima RF, Crombez G, Vlaeyen JW. Catastrophizing and fear of tinnitus predict quality of life in patients with chronic tinnitus. Ear Hear. 2011;32:634–641.
- Erlandsson SI, Hallberg LR-M. Prediction of quality of life in patients with tinnitus. Br J Audiol. 2000; 34:11–20.
- Malouff JM, Schutte NS, Zucker LA. Tinnitus-related distress: a review of recent findings. Curr Psychiatry Rep. 2011;13:31–36.
- Stephens SDG, Hallam RS, Jakes SC. Tinnitus: a management model. Clin Otolaryngol Allied Sci. 1986;11:227–238.
- Coles RRA, Hallam RS. Tinnitus and its management. Br Med Bull. 1987;43:983–998.
- Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005; 48:1204–1235.
- Myers PJ, Griest S, Kaelin C, et al. Development of a progressive audiologic tinnitus management program for veterans with tinnitus. J Rehabil Res Dev. 2014;51:609–622.
- Tyler R, editor. Tinnitus treatments. Clinical protocols. New York: Thieme; 2006.
- Gander PE, Hoare DJ, Collins L, et al. Tinnitus referral pathways within the national health service in England: a survey of their perceived effectiveness among audiology staff. BMC Health Serv Res. 2011;11:162.
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry. 2005; 186:11–17.
- Andersson G, Rask-Andersen H. Self-reported hearing problems after surgery for vestibular schwannoma (acoustic neuroma). J Audiol Med. 2002;11:25–34.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67: 361–370.
- Baguley DM, Andersson G. Factor analysis of the Tinnitus Handicap Inventory. Am J Audiol. 2003; 12:31–34.
- Andersson G, Kaldo V. Cognitive-behavioral therapy with applied relaxation. In: Tyler RS, editor. Tinnitus treatment clinical protocols. New York: Thieme; 2006. p. 96–115.
- Newman CW, Sandridge SA, Bolek L. Development and psychometric adequacy of the screening version of the Tinnitus Handicap Inventory. Otol Neurotol. 2008;29:276–281.
- Zöger S, Svedlund J, Holgers KM. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. 2004;47:282–288.
- Martinez Devesa P, Waddell A, Perera R, et al. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2010;(9):CD005233.
- Cima RF, Maes IH, Joore MA, et al. Specialised treatment based on cognitive behaviour therapy versus usual care for tinnitus: a randomised controlled trial. Lancet. 2012;379:1951–1959.
- Hesser H, Weise C, Rief W, et al. The effect of waiting: a meta-analysis of wait-list control groups in trials for tinnitus distress. J Psychosom Res. 2011; 70:378–384.
- Andersson G, Vretblad P, Larsen H-C, et al. Longitudinal follow-up of tinnitus complaints. Arch Otolaryngol Head Neck Surg. 2001;127:175–179.
- Maes IH, Cima RF, Anteunis LJ, et al. Cost-effectiveness of specialized treatment based on cognitive behavioral therapy versus usual care for tinnitus. Otol Neurotol. 2014;35:787–795.