Abstract
A Therapy Outcome Measure (TOM) is a practical tool for measuring outcomes of care, providing a quick and simple measure which can be used over time in a routine clinical setting. The TOM allows therapists to reflect on the dimensions of impairment, activity, participation, and well-being on an 11-point ordinal scale. Currently there are no therapy outcome measures for Inducible Laryngeal Obstruction (ILO) and Chronic Cough (CC). The purpose of this study was to develop two TOMs, one for ILO (TOM ILO) and one for CC (TOM CC), and to test the reliability and validity of each. Respiratory professionals working with patients with ILO and CC from eight UK locations received training in the use of TOM ILO and TOM CC. Face validity, inter-rater reliability and test-retest reliability were tested and analysed. TOM ILO and TOM CC both have strong face validity. The TOM ILO had strong intra-rater reliability and inter-rater reliability. The TOM CC had poor intra-rater but strong inter-rater reliability. TOM ILO and TOM CC have readily been adapted by those who received training. TOM ILO and TOM CC can now be used as a validated outcome measure.
Introduction
Inducible laryngeal obstruction (ILO) is an inappropriate, transient, and reversible narrowing of the laryngeal aperture in response to external triggers (Halvorsen et al., Citation2017). Several terms have been used to describe this including paradoxical vocal fold motion (PVFM) and vocal cord dysfunction (VCD), with ILO being a consensus term agreed by the European Respiratory Society, European Laryngological Society, and American College of Chest Physicians in 2017 (Christopher et al., Citation1983; Halvorsen et al., Citation2017; Kellman & Leopold, Citation1982). There is still a limited understanding of the pathophysiology, epidemiology, and aetiology of ILO (Haines et al., Citation2018). The prevalence of ILO is unknown but is more common in females with a broad age range (Haines et al., Citation2018; Petrov, Citation2019). Inducible laryngeal obstruction generally presents during inhalation and comes on suddenly with symptoms localised to the throat or upper chest (Haines et al., Citation2018; Halvorsen et al., Citation2017; Petrov, Citation2019). It occurs at the level of the glottis or supraglottis and leads to difficulty in breathing (Halvorsen et al., Citation2017). Individuals with ILO present across a variety of healthcare settings with differing levels of morbidity (Haines et al., Citation2018) which can lead to unnecessary medical treatment and increased healthcare utilisation (Abdelwahab et al., Citation2020; Tiotiu et al., Citation2018).
Cough is a protective reflex mechanism, which enables airway secretion clearance and prevents aspiration. Most cases of cough are acute or subacute and arise due to viral upper respiratory tract infections, usually lasting less than three weeks. However, when a cough persists for more than eight weeks it is defined as ‘chronic cough’ (Irwin et al., Citation2006). Such patients classically describe a dry irritable cough in response to environmental irritants (Hilton et al., Citation2013). Chronic cough represents hyperresponsiveness of the neuronal pathways involved in the cough reflex (Satia et al., Citation2017), and an impairment in descending inhibitory controls (Ando et al., Citation2016; Farrell et al., Citation2012), referred to as cough hypersensitivity syndrome (Morice et al., Citation2014). Chronic cough can remain refractory even to a systematic approach to management in approximately 20% of cases (Pratter & Abouzgheib, Citation2006). Persistent cough causes significant physical, psychological, and social morbidity. Many patients suffer from incontinence, vomiting and depression because of cough severity, thus negatively affecting quality of life (French et al., Citation1998).
The evidence base for ILO and CC is growing, but many aspects remain poorly understood (Haines et al., Citation2018; Patel et al., Citation2015). This makes it difficult for patients to explain all aspects of the disease. Progress has been made with guidelines published on laryngoscopy reporting procedures (Walsted et al., Citation2021), symptom-based questionnaires (Fowler et al., Citation2015; Pinto et al., Citation2016) and respiratory societies are acknowledging research priorities in this area (Halvorsen et al., Citation2017), but more is needed to increase clinician knowledge in this field.
The World Health Organisation (WHO) International Classification of Function, Disability, and Health (ICF) framework is a classification system for describing functioning and disability in relation to a health condition (World Health Organisation (WHO-ICF), Citation2001). It provides a common language and framework for describing the level of function of a person within their unique environment and has two parts ‘functioning and disability’ and ‘contextual factors’. It reinforces the importance of looking at the client as a whole and considering the individual’s lifestyle and personality. Patient questionnaires and symptom assessment scales are the two approaches used to assess and evaluate symptoms and functions.
Several symptom-based questionnaires that have been developed for respiratory or upper airway disorders are used in patients suspected with ILO and/or CC. Most focus on the impairment of body structure and function, but some include other factors, such as activity limitation, participation restriction, and contextual factors ().
Table 1. Respiratory and upper airway disorder questionnaires.
A health outcome can be defined as ‘a change in the health status of an individual group or population which is attributable to the planned intervention or series of interventions (World Health Organisation (WHO-ICF), Citation1998). Currently there are no therapy outcome measures for ILO and CC to allow us to evaluate changes over time and identify meaningful changes for the patient and the effect of interventions on the individual. Outcome measures are required to demonstrate the impact and value of therapy and services, identify areas of improvement and benchmark against other organisations, services, and standards.
The RCSLT has adopted Therapy Outcome Measures (TOMS) (Enderby et al., Citation2013) as its preferred outcome measurement tool. This is an outcome measure used by many rehabilitation professionals to measure and record the impact of their interventions, and based on the WHO-ICF (Citation2001). The TOM was initially developed by Professor Pamela Enderby in the 1980s and has been adapted over the years. Therapy Outcome Measures are administered following assessment/intervention of an individual by a healthcare professional. People are rated in relation to four domains: Impairment, Activity, Participation and Well-being. Well-being is not included within the WHO-ICF framework but is included within the TOM tool after reviewing goals of therapy. The therapist rates individuals using an 11-point ordinal scale with 6 defined points.
In this study we therefore aimed to develop TOMs for ILO and CC (TOM ILO and TOM CC). We have tested these for face validity, inter-rater reliability and test-retest reliability in a group of SLTs specialising in laryngeal dysfunction.
Materials and methods
Development of TOM ILO and TOM CC
The TOM ILO and TOM CC scales were adapted to reflect varying degrees of impairment, activity, participation and well-being of the ILO and CC population (Appendixes A and B). The ‘core’ TOM was initially formed by Pamela Enderby in the 1980s, but the wording has been altered for specific client groups. There are currently over 70 different TOMs that have been developed and published. These contain descriptors that have been developed by experts working in those areas and aim to improve inter-rater reliability.
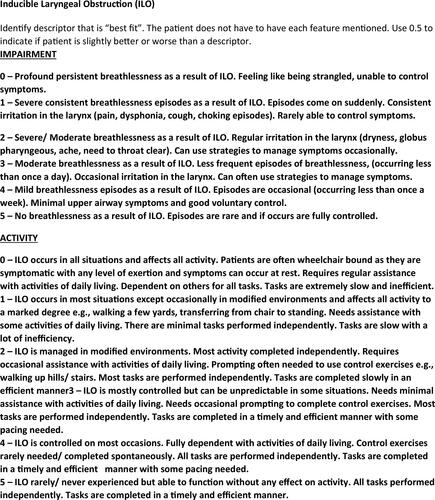
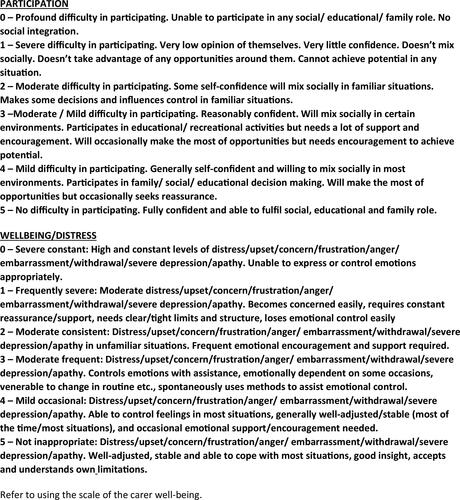
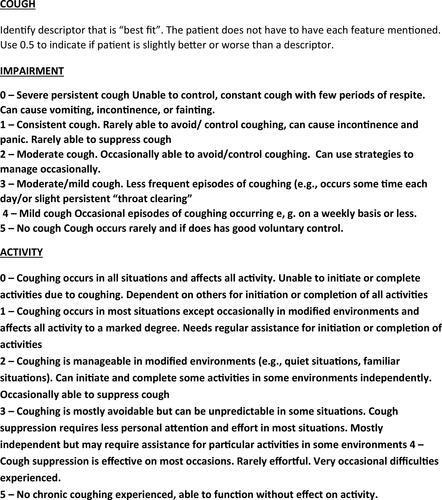
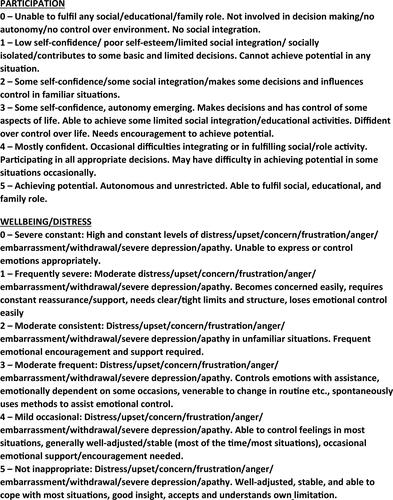
The TOM ILO and TOM CC were adapted by a specialist SLT (Siobhan Ludlow) in line with the RCSLT guidance and guided by TOMs developed for other disciplines ( and ). Siobhan Ludlow is a consultant SLT who has been working in the field of upper airways for over 10 years.
Figure 1. TOM ILO.
Figure 2. TOM CC.
The adapted TOMs were emailed to 10 specialist SLTs working with upper airway conditions including ILO and CC and responses were gathered from all 10 SLT professionals. Changes were made and the newly adapted scales were sent to Pamela Enderby and Alexandra John for review and to ensure that the scale were in line with the principles of TOMs.
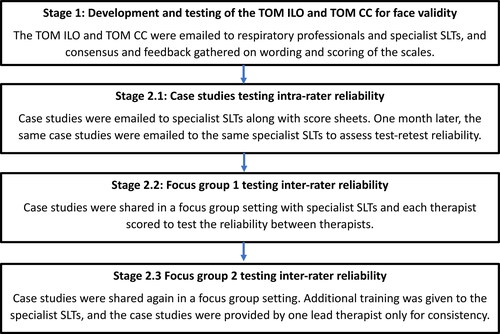
The iterative process of designing the measure and testing the validity and reliability was followed to produce a measure that functioned as intended ().
Sample and recruitment
Eligibility criteria
Inclusion criteria for patient recruits (stage 1)
Patient with a diagnosis of ILO or CC and undergoing speech and language therapy
Patients aged 17 and above
Inclusion criteria for professional recruits (stage 1, stage 2)
Medical professionals working in the NHS with respiratory patients
Medical professionals who understand ILO and CC (diagnosing and treating themselves or part of an MDT team who diagnose and treat) who can give a fair judgement on the relevance of TOMs domains.
Specialist SLTs who are working in upper airway or ENT services and regularly diagnosing and treating ILO and CC
Comprehension of English
Exclusion criteria for patient recruits (stage 1)
Patients with a diagnosis of ILO and/or CC that is being managed by other professionals and not currently appropriate for speech and language therapy.
Exclusion criteria for professional recruits (stage 1, stage 2)
Medical professionals who do not work within respiratory or the NHS.
Medical professionals who do not understand ILO or CC.
Speech and Language Therapists who do not work within respiratory or ENT and do not manage upper airway conditions.
Ethical and regulatory considerations
We sought advice from Manchester University NHS Foundation Trust (MFT) Research and Innovation (R&I) team and Professor Pam Enderby who stated that as there no identifiable data was involved, and outcome measurement is part of routine practice, there was no need for ethical approval for this project.
Statistical methods
The statistical methods chosen (Cohen’s Kappa co-efficient and Krippendorff alpha co-efficient) were decided on after advice and discussions with the MFT statisticians. Statistical analysis was performed in SPSS version 28.0.1.0
Recruitment
To test the TOM ILO and TOM CC for validity and reliability, a multidisciplinary group of respiratory professionals were recruited ( and ). Purposive sampling was used as these professionals are considered experts in the field of ILO and CC, have a deep understanding of the subject and a clear understanding of what needs to be measured.
Table 2. Professional groups.
Table 3. Professional groups geographical areas represented.
Stage 1: face validity
Once satisfied, the ILO and CC adapted TOMs were shared with the multi-professional groups by email to ensure all agreed with wording and scoring. Written feedback was returned by email. Feedback suggested that the TOM ILO and TOM CC had strong face validity and usability.
The ILO and CC adapted TOMs were trialled on 20 patients recruited from the Manchester SLTs to ensure that no further amendments needed to be made to wording or adaptive scales, then a reliability trial was completed.
Stage 2: reliability
Checking reliability is important as it represents the extent to which the adapted scale is understood consistently, and that the data collected is a correct representation. Intra-rater reliability refers to the consistency of the data recorded by one therapist over several trials. Inter-rater reliability is a measure of consistency used to evaluate the extent to which different professionals agree in their assessment decisions.
Stage 2.1: case studies
Intra-rater reliability was tested by producing 20 case studies (Appendixes A and B) (10 ILO, 10 CC) which were shared with 10 specialist SLTs who were working within upper airway/ENT services and regularly seeing ILO and CC patients, along with score sheets (Appendixes E and F). All specialist SLTs were familiar with using TOMs for other disorders so no specific training was delivered at this time. Each therapist used the TOM ILO and TOM CC scales to rate the ILO and CC case studies. One month later, the therapists were asked to rate the same case studies again (without referring to their previous scoring 1st scores). This helped to measure if the adapted scale was consistent over time. Agreement was quantified for the TOM ILO and TOM CC scales using the Cohen’s Kappa co-efficient (k) (). Inter-rater reliability was also tested on this data using the Krippendorff alpha co-efficient ().
Table 4. Intra-rater reliability of TOMS ILO and TOMS CC using Cohen’s Kappa co-efficient.
Table 5. Inter-rater reliability of TOMS ILO and TOMS CC from case histories and focus groups using Krippendorff alpha co-efficient.
Stage 2.2: focus group 1
Inter-rater reliability was tested by inviting all specialist upper airway SLTs to attend a virtual focus group which was completed on Microsoft Teams. Some of these specialist SLTs (n = 6) were the same therapists that completed stage 2.1 (case studies). Each therapist who attended was asked to provide two case studies (1 ILO, 1 CC) and take turns to share their computer screen, whilst the other therapists rated the case studies using the adapted scales separately and without collusion ().
Stage 2.3: focus group 2
As the inter-rater reliability was poor on the first focus group. Further training was given to the specialist upper airway SLTs. This was completed online and involved more detailed explanation about TOMs and their use, including reminders about the scale (11-point), allowing scores between descriptors to be given (e.g. 1.5, 2.5), and use of more detailed case study descriptions. The lead therapist (Siobhan Ludlow-Consultant SLT) revised all case studies to keep consistency, and these were shared with the therapists before they attended the focus group. The therapists were able to ask any additional questions during the focus group and each therapist rated the case study using the adapted scales without collusion (Appendixes C and D).
Results
Most comments were supportive of the adapted measures with a few changes on wording including terminology of the varying levels of breathlessness on the TOM ILO, including independence level, pace and efficiency on the TOM ILO and including more detail on social ability on the TOM CC which were all made. The TOMS ILO showed ‘almost perfect’ intra-rater reliability with a Kappa (k) greater than 0.9 by each therapist. The TOMS CC co-efficient was less reliable with the highest percentage of therapists (50%) showing ‘fair’ intra-rater reliability with a Kappa (k) of between 0.21–0.40 ()
Where case studies were shared with 10 therapists via email twice (one month apart), the TOMS ILO showed a strong inter-rater reliability with a Krippendorff alpha co-efficient greater than 0.849. The TOMS CC showed moderate inter-rater reliability with a Krippendorff alpha co-efficient of 0.797 (). The TOMS ILO and TOMS CC on the first focus group showed poor inter-rater reliability with a Krippendorff alpha co-efficient of 0.614 (TOMS CC) and 0.612 (TOMS ILO). The TOMS ILO and TOMS CC on the second focus group showed strong inter-rater reliability with a Krippendorff alpha co-efficient of 0.892 (TOMS CC) and 0.881 (TOMS ILO).
Discussion
Therapy outcome measures provide quantifiable data and insights into a patient’s well-being, symptoms and functioning allowing therapists to track progress and make informed decisions about treatment approaches. The first iteration of the TOM ILO and TOM CC have been tested for face validity, intra-rater reliability and inter-rater reliability between specialist SLT’s. Initial findings suggest that both scales have strong face validity. The TOM ILO had strong intra-rater and inter-rater reliability. The TOM CC had poor intra-rater but strong inter-rater reliability. In previous reliability testing of TOM, the limitations of testing inter-rater reliability using patient case histories have been highlighted because information can be inadequate or reveal information in such a way as to prime judges (Enderby et al., Citation2013). Several of the specialist SLTs completed stage 2.1 (case studies), stage 2.2 (focus group 1) and stage 2.3 (focus group 2) therefore had seen the TOM ILO and TOM CC several times and may have had bias over those who were seeing the TOM ILO and TOM CC for the first time. Case histories are known to have difficulties in inter-rater reliability trials. However, they are resource efficient and allow presentation of data, using the full range of severities of conditions to test scoring systems. In preparing the case histories on the second focus group, more detail was given in the case histories and additional training given to the therapists prior to the focus group. The therapists were able to ask further questions if needed of the therapist presenting the case history.
The TOM CC poor intra-rater reliability could have been due to the nature of case histories and rating a second time without additional clinical information could cause bias. It has been reported that using the TOM in real life situations where professionals can explore patient-experiences and choose appropriate scores is easier than rating from case histories (John and Enderby Citation2000). Most therapists will see patients several times during their care therefore it is likely that the reliability in the clinic will be likely to be better than in this trial. All respiratory SLTs who were involved in this project felt positively towards these measures and realised the importance of collecting reliable data appropriate for their services to inform commissioning and service improvement. We are hopeful that the TOM ILO and TOM CC can now be used as validated outcome measure and can be published in future editions of TOMs book.
The effectiveness of any therapeutic intervention has many dimensions including clinical effectiveness of the intervention and the benefit felt by the patient as a direct result of having the intervention. Capturing the direct patient perspective on functional status, health related quality of life, symptoms, symptom burden, activity, participation and contextual impact complements therapy outcomes and provides a patient centred approach to care. There are several patient reported outcome measures (PROMs) used in chronic cough (Birring et al., Citation2003; French et al., Citation2002; Morice et al., Citation2011) but a specific ILO PROM is required in the future.
Conclusion
In conclusion, the TOM ILO and TOM CC scales have been shown to have strong reliability and validity. They can now be used for clinical and research purposes by therapists who have received the TOMs training. Future work is needed to develop and validate a patient reported outcome measure for ILO to be used alongside the TOMs.
Ethical statement
The author declares that as this is a discussion paper no ethical approval or informed consent is required for this manuscript.
Acknowledgements
Acknowledgement goes to the expert Speech and Language Therapists (SLTs) who were involved in various stages of the development and testing of the outcome measure. Rosamund Blaylock – clinical lead speech and language therapist, Leicestershire Partnership Trust. Jennifer Butler – highly specialist speech and language therapist, Newcastle upon Tyne Hospitals NHS Foundation Trust. Joanne Clayton – highly specialist speech and language therapist, Royal Liverpool, and Broadgreen University Hospitals NHS Foundation Trust. Karen Esposito – highly specialist speech and language therapist, Sheffield Teaching Hospitals NHS Foundation Trust. Fiona Gillies – highly specialist speech and language therapist, Whittington Hospital, London. Jemma Haines – chief AHP, Manchester University NHS Foundation Trust. Lydia Hart – senior specialist speech and language therapist, Frimley Health Foundation Trust. Hannah Lever – senior specialist speech and language therapist, Lancashire Chest Centre. Nicola Pargeter – principal speech and language therapist, University Hospitals Birmingham NHS Foundation Trust. Waseema Sarodia – specialist speech and language therapist, Manchester University NHS Foundation Trust. Julia Selby – consultant speech and language therapist, Royal Brompton Hospital. Claire Slinger – consultant speech and language therapist, Lancashire Chest Centre. Bethany Tidmarsh – senior specialist speech and language therapist, Manchester University NHS Foundation Trust. Emma Turner – highly specialist speech and language therapist, Guy’s Hospital, London. Special acknowledgment goes to Professor Pamela Enderby for sharing her knowledge and expertise and assisting in the development of the Therapy Outcome Measures (TOMs). The final document is the result of extensive consultation within and beyond the speech and language therapy profession with thanks to all those involved.
Disclosure statement
The author declares that this manuscript has not been submitted elsewhere. The author declares that there are no conflicts of interest.
Data availability statement
The author declares that there is no further supporting data available for this manuscript.
Additional information
Funding
References
- Abdelwahab, H., Aboelnass, A., Ayman, A., Elsaid, A., Farrag, N., & Hamad, A. (2020). Prevalence of inducible laryngeal obstruction among patients diagnosed as bronchial asthma. Advances in Respiratory Medicine, 88(2), 129–133. https://doi.org/10.5603/ARM.2020.0087
- Ando, A., Smallwood, D., McMahon, M., Irving, L., Mazzone, S. B., & Farrell, M. J. (2016). Neural correlates of cough hypersensitivity in humans: Evidence for central sensitisation and dysfunctional inhibitory control. Thorax, 71(4), 323–329. https://doi.org/10.1136/thoraxjnl-2015-207425
- Belafsky, P. C., Postma, C. H., & Koufman, J. A. (2002). Validity and reliability of the reflux symptom index (RSI). Journal of Voice, 16(2), 274–277. https://doi.org/10.1016/S0892-1997(02)00097-8
- Bestall, J. C., Paul, E. A., Garrod, R., Garnham, R., Jones, P. W., & Wedzicha, J. A. (1999). Usefulness of the Medical Research Council (MRC) dyspnea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax, 54(7), 581–586. https://doi.org/10.1136/thx.54.7.581
- Birring, S. S., Prudon, B., Carr, A. J., Singh, S. J., Morgan, M. D. L., & Pavord, I. D. (2003). Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire. Thorax, 58(4), 339–343. https://doi.org/10.1136/thorax.58.4.339
- Christopher, K. L., Wood, R. P., Eckert, R. C., Blager, F. B., Raney, R. A., & Souhrada, J. F. (1983). Vocal-cord dysfunction presenting as asthma. New England Journal of Medicine, 308(26), 1566–1570. https://doi.org/10.1056/NEJM198306303082605
- Deary, I., Wilson, J., Carding, P., & Mackenzie, K. (2003). VOISS: A patient-derived voice symptom scale. Journal of Psychometric Research, 54(5), 483–489.
- Enderby, P., John, A., & Petheram, B. (2013). Therapy outcome measures for rehabilitation professionals: Speech and language therapy, physiotherapy, occupational therapy. John Wiley & Sons.
- Farrell, M. J., Leonie, J. C., Chiapoco, D., Egan, G. F., & Mazzone, S. B. (2012). Neural correlates coding stimulus level and perception of capsaicin-evoked-urge-to-cough in humans. NeuroImage, 61(4), 1324–1335. https://doi.org/10.1016/j.neuroimage.2012.03.030
- Fowler, S. J., Thurston, A., Chesworth, B., Cheng, V., Constantinou, P., Vyas, A., Lillie, S., & Haines, J. (2015). The VCDQ – A questionnaire for symptom monitoring in vocal cord dysfunction. Clinical and Experimental Allergy, 45(9), 1406–1411. https://doi.org/10.1111/cea.12550
- French, C. L., Irwin, R. S., Curley, F. J., & Krikorian, C. J. (1998). Impact of chronic cough on quality of life. Archives of Internal Medicine, 158(15), 1657–1661. https://doi.org/10.1001/archinte.158.15.1657
- French, C. T., Irwin, R. S., Fletcher, K. E., & Adams, T. M. (2002). Evaluation of a cough-specific quality-of-life questionnaire. Chest, 121(4), 1123–1131. https://doi.org/10.1378/chest.121.4.1123
- Grammatopoulou, E., Skordilis, E., Georgoudis, G., Haniotou, A., Evangelodimou, A., Fildissis, G., Katsoulas, T., & Kalagiakos, P. (2014). Hyperventilation in asthma: A validation study of the Nijmegen Questionnaire-NQ. Journal of Asthma, 51(8), 839–846. https://doi.org/10.3109/02770903.2014.922190
- Haines, J., Hull, J. H., & Fowler, S. J. (2018). Clinical presentation, assessment, and management of inducible laryngeal obstruction. Current Opinion in Otolaryngology & Head and Neck Surgery, 26(3), 174–179. https://doi.org/10.1097/MOO.0000000000000452
- Halvorsen, T., Walsted, E. S., Bucca, C., Bush, A., Catarella, G., Friedrich, G., Herth, F. J. F., Hull, J. H., Jung, H., Maat, R., Nordang, L., Remacle, M., Rasmussen, N., Wilson, J. A., & Heimdal, J. (2017). Inducible laryngeal obstruction: An official joint European Respiratory Society and European Laryngological Society statement. European Respiratory Journal, 50, 1602221. https://doi.org/10.1183/13993003.02221-2016
- Hilton, E. C. Y., Baverel, P. G., Woodcock, A., Van Der Draff, P. H., & Smith, J. A. (2013). Pharmacodynamic modelling of cough responses to capsaicin inhalation calls into question the utility of the C5 end point. Journal of Allergy and Clinical Immunology, 132(4), 847–855.e5. https://doi.org/10.1016/j.jaci.2013.04.042
- Irwin, R. S., Baumann, M. H., Bolser, D. C., Boulet, L.-P., Braman, S. S., Brightling, C. E., Brown, K. K., Canning, B. J., Chang, A. B., Dicpinigaitis, P. V., Eccles, R., Glomb, W. B., Goldstein, L. B., Graham, L. M., Hargreave, F. E., Kvale, P. A., Lewis, S. Z., McCool, F. D., McCrory, D. C., & Tarlo, S. M. (2006). Diagnosis and management of cough executive summary. Chest, 129(1 Suppl), 1S–23S. https://doi.org/10.1378/chest.129.1_suppl.1S
- John, A., Enderby, P. (200). Reliability of speech and language therapists using therapy outcome measures. International Journal of Language & Communication Disorders, 35(2), 287–302.
- Kellman, R. M., & Leopold, D. A. (1982). Paradoxical vocal cord motion: An important cause of stridor. Laryngoscope, 92(1), 58–60. https://doi.org/10.1288/00005537-198201000-00012
- Morice, A. H., Faruqi, S., Wright, C. E., Thompson, R., & Bland, J. M. (2011). Cough hypersensitivity syndrome: A distinct clinical entity. Lung, 189(1), 73–79. https://doi.org/10.1007/s00408-010-9272-1
- Morice, A. H., Millqvist, E., Belvisi, M. G., Bieksiene, K., Birring, S. S., Chung, K. F., Dal Negro, R. W., Dicpinigaitis, P., Kantar, A., McGarvey, L. P., Pacheco, A., Sakalauskas, R., & Smith, J. A. (2014). Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. European Respiratory Journal, 44(5), 1132–1148. https://doi.org/10.1183/09031936.00218613
- Olin, J., Shaffer, M., Nauman, E., Durso, C., Fan, E., Staudenmayer, H., Christopher, K., & Gartner-Schmidt, J. (2022). Development, and validation of the exercise-induced laryngeal obstruction dyspnea index. Journal of Allergy and Clinical Immunology, 1437–1444. https://doi.org/10.1016/j.jaci.2021.09.027
- Patel, R, Venediktov, R, Schooling, T, Wang, B. (2015). Evidence-Based Systematic Review: Effects of Speech-Language Pathology Treatment for Individuals With Paradoxical Vocal Fold Motion. American Journal of Speech-Language Pathology, 24, 566–584.
- Petrov, A. (2019). Vocal cord dysfunction: The spectrum across the ages. Immunology and Allergy Clinics of North America, 39(4), 547–560. https://doi.org/10.1016/j.iac.2019.07.008
- Pinto, L. H., Aun, M. V., Cukier-Blaj, S., Stelmach, R., Cukier, A., Kalil, J., Agondi, R. C., & Giavina-Bianchi, P. (2016). Vocal cord dysfunction diagnosis may be improved by a screening checklist. Allergology International, 65(2), 180–185. https://doi.org/10.1016/j.alit.2015.11.001
- Pratter, M. R., & Abouzgheib, W. (2006). Make the cough go away. Chest, 129(5), 1121–1122. https://doi.org/10.1378/chest.129.5.1121
- Rosen, C. A., Lee, A. S., Osborne, J., Zullo, T., & Murry, T. (2004). Development and validation of the Voice Handicap Index-10. Laryngoscope, 114(9), 1549–1556. https://doi.org/10.1097/00005537-200409000-00009
- Satia, I., Tsamandouras, N., Holt, K., Badri, H., Woodhead, M., Ogungbenro, K., Felton, T. W., O’Byrne, P. M., Fowler, S. J., & Smith, J. A. (2017). Capsaicin-evoked cough responses in asthmatic patients: Evidence for airway neuronal dysfunction. Journal of Allergy and Clinical Immunology, 139(3), 771–779.e10. https://doi.org/10.1016/j.jaci.2016.04.045
- Schatz, M., Meltzer, E. O., Nathan, R., Derebery, J. M., Mintz, M., Stanford, R. H., Dalal, A. A., Silvey, M. J., & Kosinski, M. (2010). Psychometric validation of the rhinitis control assessment test: A brief patient – Completed instrument for validating rhinitis symptoms. Annals of Allergy Asthma and Immunology, 104(2), 118–124.
- Sedeh, F. B., Von Bülow, A., Backer, V., Bødtger, U., Petersen, U. S., Vest, S., Hull, J., & Porsbjerg, C. (2018). Breathing pattern assessment tool as a new screening tool to identify dysfunctional breathing. European Respiratory Journal, Conference abstract therefore no specific pages. 52(62).
- Tiotiu, A., Plavec, D., Novakova, S., Mihaicuta, S., Novalova, P., Labor, M., & Bikov, A. (2018). Current opinions for the management of asthma associated with ear, nose, and throat co-morbidities. European Respiratory Review, 27(150), 180056. https://doi.org/10.1183/16000617.0056-2018
- Traister, R. S., Fajt, M. L., Landsittel, D., & Petrov, A. A. (2013). A novel scoring system to distinguish vocal cord dysfunction from asthma. Journal of Allergy and Clinical Immunology in Practice, 2(1), 65–69.
- Vertigan, A. E., Bone, S. L., & Gibson, P. G. (2014). Development and validation of the Newcastle laryngeal hypersensitivity questionnaire. Cough (London, England), 10(1), 1. https://doi.org/10.1186/1745-9974-10-1
- Walsted, E. S., Famokunwa, B., Andersen, L., Rubak, S. L., Buchvald, F., Pedersen, L., Dodd, J., Backer, V., Nielsen, K. G., Getzin, A., & Hull, J. H. (2021). Characteristics, and impact of exercise-induced laryngeal obstruction: An international perspective. ERJ Open Research, 7(2), 00195–02021. https://doi.org/10.1183/23120541.00195-2021
- Wen, S., Wang, S., Niu, S., Zhang, M., Shi, C., Qiu, Z., Xu, X., & Yu, L. (2020). Sensitivity and specificity of combination of Hull airway reflux questionnaire and gastroesophageal reflux disease questionnaire in identifying patients with gastroesophageal reflux-induced chronic cough. Annals of Translational Medicine, 8(23), 1564. https://doi.org/10.21037/atm-20-3236
- Williams, M. T., Lewthwaite, H., Paquet, C., Johnston, K., Olsson, M., Belo, L. F., Pitta, F., Morelot-Panzini, C., & Ekström, M. (2021). Dyspnea-12, and multi-dimensional dyspnea profile: Systematic review of use and properties. Journal of Pain and Symptom Management, 63(1), e75–e87. https://doi.org/10.1016/j.jpainsymman.2021.06.023
- World Health Organisation (WHO-ICF). (1998). International classification of functioning, disability and health promotion glossary. World Health Organisation.
- World Health Organisation (WHO-ICF). (2001). International classification of functioning, disability and health. World Health Organisation.
- Ye, J., Nouraie, M., Holguin, F., & Gillespie, A. (2017). The ability of a patient-symptom questionnaire to differentiate PVFMD from asthma. Journal of Voice, 31(3), 382 e1–382 e8. https://doi.org/10.1016/j.jvoice.2016.08.013
- Yorke, J., Swigris, J., Russell, A.-M., Moosavi, S. H., Ng Man Kwong, G., Longshaw, M., & Jones, P. W. (2010). Dyspnea-12 is a valid and reliable measure of breathlessness in patients with interstitial lung disease. Chest, 139(1), 159–164. https://doi.org/10.1378/chest.10-0693
Appendix A.
ILO case studies V1
Appendix B.
Chronic cough case studies V1
Appendix C.
ILO case histories V2
77 y/o Female. Retired. Lives with husband
PMHx: Asthma (well controlled on ICS), reflux, IBS, OA
Respiratory investigations: in keeping with asthma. No recent exacerbations.
Referred to SLT from Asthma clinic
Reports sx which feels separate to asthma over the past few years – feels like throat closing when people spray aerosols/cleaning the house. Can happen with/without cough. Initially felt like ‘going to die’ but very transient, resolves after a few minutes when ‘calms down,’ tends to sit, breathe through
Happening approximately weekly
No benefit if takes salbutamol
Voice feels ‘different’ – lower pitch, hoarse
No dysphagia
Avoids all aerosol triggers, nothing in the house anymore. Worries about being symptomatic in shops, i.e. avoids perfume aisle etc.
Questioning whether related to stress – husband having memory clinic/dementia investigations
As happened a few times now, acknowledges not life threatening but just wants diagnosis/explanation of what is going on
Laryngoscopy = unable to trigger typical symptoms but, in absence of respiratory concern, to treat empirically for ILO
60 y/o Female. Retired nurse. Lives with husband
PMHx: Fibromyalgia, Sjorgrens. No respiratory diagnoses.
Respiratory investigations = no evidence of lower airways disease
Referred to SLT from Allergy clinic
Long-standing history of? anaphylaxis to multiple drugs but no evidence of allergy on formal testing and so Allergy clinic keen for MDT discussions and SLT input.
Traumatic episode following COVID jab – throat tightness, SOB, stridor. Ended up ventilated in ICU.
Since then, has been experiencing similar symptoms ‘out of the blue’ and in response to environmental triggers and stress. Taking up to x10 epi-pens a day, with little effect.
Baseline mild inspiratory wheeze (chest clear)
Seeing psychology for trauma post-ICU
Debilitating currently – scared to leave the house. Convinced having spontaneous episodes of anaphylaxis and reliant on adrenalin. Huge impact on quality of life.
Strained voice quality
Swallowing feels ‘tight’
No reflux/rhinitis concerns
Laryngoscopy = significant tension at baseline with clear ILO even before provocation. For SLT.
28 y/o Female. Student
PMHx: severe asthma (on Benralizumab), anxiety.
Respiratory investigations: asthma since childhood. Previously difficult to manage with recurrent exacerbations, but now well controlled on biologic.
Referred to SLT by Severe Asthma service
Has recently been experiencing episodes of throat closure – taking excessive amounts of salbutamol as a result but no benefit. Associated palpitations, worsen anxiety.
Triggers: aerosols, stress – overthinking/overinterpreting of symptoms ‘hyperaware’ of any laryngeal sensations now
Very anxious as has had bad asthma attacks in the past – frightened.
Impacting quality of life – happened once on night out and distressed/embarrassed/friend called ambulance as they thought it was asthma. Makes her wants to avoid some social settings.
No dysphonia/dysphagia/reflux/rhinitis concerns
Laryngoscopy = structurally and functionally normal at baseline. Intermittent vocal cord adduction on provocation with aerosols. Triggered typical sx. For SLT therapy alongside normal asthma management.
58 y/o Male. Stopped working as result of sx. Difficult social situation at home
PMHx: anxiety/depression, HTN, reflux, nil other significant
Respiratory investigations: no evidence of lower airways disease.? BPD but no self-reported SOB concerns
Referred to SLT from local Allergy Clinic
Multiple calls for ambulances, A&E attendance due to throat tightness and subjective feeling of swelling/tingling
Allergy testing – normal. Have written multiple letters encouraging him not to carry an epi-pen
Bounced between services; Resp/Gastro/Allergy/ENT and hard to engage
Patient convinced allergic to multiple foods and avoiding++, therefore difficult for him to consider differential diagnoses. Open to stress/anxiety impact on overall sx however.
Previous ENT scope in A&E = no laryngeal oedema
Very dysphonic (mod-severe rough, strained)
Eating and drinking normally aside from avoidance behaviours
Laryngoscopy = intermittent ILO at baseline. Declined provocation. For SLT input with ongoing liaison with allergy team.
48 y/o Female. Not working (own choice). Lives with partner
PMHx: TBM, obesity, chronic pain
Respiratory investigations: bronch for TBM diagnosis. Otherwise no lower airways disease. Encouraged to lose weight.
Referred to SLT by Physio as did not feel sx entirely explained by TBM. Managing ACT advice well and no recent chest infections.
Barking cough secondary to TBM but can find when cough++ that throat ‘shuts off’ and ‘can’t get any air in’ – lasts seconds but partner can get worried
Patient not distressed but wants to know how to manage these episodes when they happen (few times a month). Googled ILO/VCD, sounds like what she is experiencing.
Episodes always start with cough and if can’t settle can get throat closure
Triggers: exertion, unaware of any other
Musculoskeletal pain secondary to coughing – no cardiac concerns for upper chest pain
Laryngoscopy = no concerns at baseline. Circumferential tension, generalised oedema (likely die to BMI). Provocation with exertion = ++cough which progressed to ILO. For SLT therapy.
35 y/o Nurse. Off sick as A&E nurse currently. Lives with partner
PMHx: nil significant past medical history. Generally fit and well.
Respiratory investigations: thoroughly investigated and normal CXR/HRCT/PFTs
Never used to have any problems but over the last 12 month has struggled to breathe around cleaning fluids at work, i.e. ChlorClean
Experiences throat tightness, chest tightness wheeze – became unmanageable at work and colleagues advised her to get it investigated. Currently signed off as result.
Has trialled inhalers but no benefit
Low mood since being signed off from work, keen to go back as financial concerns
Acknowledges stress at work but contextual
Laryngoscopy = evident baseline tension but no structural concerns. Provocation with cleaning products resulted in usual symptoms and intermittent ILO. For SLT therapy.
46 y/o Mail. Works in IT. Lives alone
PMHx: Asthma (on ICS), reflux, fusion of cervical spine with associated chronic pain
Respiratory investigations: mild asthma as per investigations and reversibility testing
Referred to SLT by asthma nurses
Adherent to ICS and no change to asthma management plan indicated
Patient reporting episodes of SOB and throat tightness +/- wheeze which are unresponsive to inhalers or previous courses of OCS. Can differentiate well between upper and lower airway sx.
Laryngeal sx mainly happen on exertion but can also be when talking fast
Taking excessive amounts of salbutamol as doesn’t know what else to do
Feels like these sx caused the breakdown of his relationship as they frightened partner
Wants to get back into exercise but feels limited because of his symptoms
Laryngoscopy = no structural/functional concerns at baseline. On provocation with exertion, evidence of BPD and ILO. For SLT and Physio treatment.
55 y/o Female. Works as a teacher (currently on sick leave). Lives with parents
PMHx: anxiety, IBS, migraines
Respiratory investigations: NAD
Referred to SLT by local Allergy clinic
Following investigations, allergy clinic did not feel any true allergic response. Possible spontaneous angioedema of the lips and urticaria. Referred to psychology team.
No hospital admissions but GP prescribed epi-pen (infrequent use) – now stopped by Allergy team.
Very aware of own symptoms; lists, constantly looking for ‘allergens’ (i.e. convinced allergic to onions so will avoid completely).
Reporting instances where food/cooking smells cause her SOB, wheeze and throat tightness. No cough. When symptomatic ‘can’t get air in or out’ but can settle in 30–45 mins if focuses on breathing. Can sometimes lose voice completely.
Now avoids eating out or socialising with friends. Potential to become quite isolated.
Feels like can’t eat in staff room/around pupils and currently – not confident to go back to work until resolved/knows what is going on and how to manage it.
Laryngoscopy: baseline circumferential tension, increased on phonation. Evidence of ILO on exposure to cooking spices. For SLT therapy and ongoing Psychology for anxiety.
83 y/o Male. Retired. Lives with wife
PMHx: HTN, bilateral hip replacements, Crohn’s (managed on biologics)
Respiratory investigations: normal CXR, HRCT, PFTs
No SOB/sputum concerns
Reports long-standing dry, laryngeal cough which worsened post COVID. Can cough to the point of choking which can be frightening (happens approx. once a week). Has also fallen over a few times as result and ended up in A&E. Self-rated 8/10 but variable.
Referred to SLT from Consultant Cough clinic
Typically episodes of choking/throat tightness always start with cough
Intermittent reflux – started on treatment
No rhinitis/PND concerns
No dysphagia and voice quality WNL for patient
Triggers: strong smells, i.e. candles/incense at daughters house. Can sometimes happen ‘out of the blue’
Laryngoscopy = signs of reflux. Otherwise structurally and functionally normal at baseline. Provocation with scents = immediate cough++ which progressed to ILO. For SLT treatment.
19 y/o Female. Student. Lives with parents
PMHx: severe asthma (on Omalizumab), rhinitis, polyps
Respiratory investigations: PFTS, HRCT in line with severe asthma diagnosis
No sputum burden or recent infections
Referred to SLT by Severe Asthma service
Patient reporting when having a ‘bad day’ with asthma, throat can feel tight and ‘harder to breath in.’ Only occasional GP previously prescribed rescue pack for this but didn’t improve sx. Confused as to why people keep saying it’s her asthma when she clearly feels the tightness in her throat.
Not overly concerned, life-long asthmatic and knows how to manage symptoms but feels throat has become tighter, more uncomfortable in the past few years and wants to know why.
No specific triggers
No reflux, ENT removed polyps, takes nasal spray daily for rhinitis
Good adherence with medications/inhaler hygiene etc.
Laryngoscopy = no structural concerns but held very tight at baseline. Unable to trigger typical episode but ‘simulated’ how it feels – demonstrated stridor and paradoxical closure. For SLT treatment based on history alongside usual asthma treatment.
Appendix D.
Chronic cough case histories V2
82 y/o Male – retired. No previous occupational exposures. Lives at home with son
PMHx: chronic neck and back pain, nil else
Generally fit and well.
Respiratory investigations: CT thorax, PFTs = NAD
Referred to SLT from Consultant Cough clinic
Reporting intermittent dry laryngeal cough since 2019. No apparent precipitating event/trigger.
No secondary benefit to cough from Gabapentin for neck/back pain
No concerns re: reflux (managed on PPIs)/rhinitis/PND/localised pain/dysphagia/dysphonia/SOB
Cough mainly characterised by globus, chronic throat clearing – ‘annoying’ but ‘just gets on with it’
Not limiting day-to-day activities just irritating
Self-rated 5/10
Laryngoscopy = mild A-P squeeze on phonation otherwise NAD. SLT therapy for globus, hypersensitivity.
59 y/o Female – works in admin. Lives at home with husband
PMHx: Mild bronchiectasis, mild emphysema, EDAC, Fibromyalgia, memory investigations
Respiratory investigations: HRCT as above, PFTs = normal, No sputum concerns on bronch
No recent chest infections
Sx out of proportion for respiratory disease
Referred to SLT from Consultant Cough clinic
No secondary impact to cough from Gabapentin/Amitriptyline/Fentanyl patches for chronic pain
Dry cough, constant last 18 month – finding it difficult to manage in context of COVID. Avoiding social situations. Frustrated, tearful in consultation.
No specific triggers but worse when talking. Self-rated 9/10.
Denies chest focused sx and no recent infections
No dysphonia/dysphagia/reflux/rhinitis/PND/SOB concerns
Laryngoscopy = No structural/functional concerns. For SLT therapy.
49 y/o Female – works as healthcare assistant. Lives with husband
PMHx: recurrent tonsillitis and ear infections, breast cancer (1996, 2018) with ongoing reconstructive surgeries, skin cancer (2019) tx with radiotherapy, now discharged.
Respiratory investigations: A/w full PFTs, normal HRCT thorax. Pt denies any chest-focused sx or SOB. No mucus or chest infections.
Referred to SLT from Consultant Cough clinic
Dry, laryngeal cough (before Breast Ca in 1990s). Variable throughout the year. No pattern. Self-rated 8/10.
Much better on holiday – husband even thought about moving abroad as patient exasperated with it.
Would like to try and avoid antitussives and trial SLT first.
Triggers to cough = temperature change, talking, lying flat, strong smells
Initially cough improved ‘a bit’ with the addition of PPIs, no overt reflux
A lot of health related stress previously but very pragmatic, level-headed. Not limiting activities but can feel embarrassed.
No rhinitis/PND/dysphagia
Previous ENT surgery to widen R nostril. This side now more uncomfortable due to radiotherapy in this area for previous skin cancer.
Voice can feel ‘croaky’ when cough is bad, can lose easily.
Laryngoscopy = No structural/functional concerns at baseline. A-P and L-M squeeze on phonation. For SLT therapy.
78 y/o Female – retired. Lives with husband
PMHx: Asthma (stable on low-dose ICS), GERD, ex-smoker (stopped 25 years ago)
Respiratory investigations: no change to PFTs, peak flows. No asthma concerns. HRCT = in keeping with mild asthma.
Reports intermittent ‘choking’ laryngeal cough for the past 3 years. Self-rated 6/10.
Predominantly dry but can feel more productive in the mornings
Referred to SLT from Consultant Cough clinic
Previous adverse reaction to Morphone so declined antitussives
Triggers = exertion, smells, laughing, talking
Subjectively feels no change to asthma, no SOB concerns. Rarely uses salbutamol.
No benefit to cough with changes to inhalers/PPIs/OCS
Feels occasionally things can go ‘wrong way’ because cough at meal times (but describes as normal irritative cough interrupting meals when trying to talk to husband at same time). Can find this upsetting when out with friends. No dysphagia concerns. No hx of infections.
Presbyphonic sounding voice but no patient concerns
Reflux managed on PPIs, variable PND sx
Laryngoscopy = evidence of PND – requested Avamys via GP. Otherwise no structural/functional concerns. For SLT therapy.
53 y/o Female – full time mum, 2 young children. Lives with partner
PMHx: IBS, Fibromyalgia, ME,? mild asthma, previous Breast Ca – now discharged, neuralgia, endometriosis
Respiratory investigations: HRCT thorax = mild bronchiectasis. A/w full PFTs. Referred to Physio to trial ACT +/- hypertonic saline. Consideration for bronch if no change.
Cough started around same time as COVID ∼2019
Denies any sputum burden and cough always feels dry, localises to larynx++. Self-rated 8/10.
Reports? chest infections but no current evidence – just describes increased periods of dry cough
Working diagnosis = combination of lower + upper airway symptoms (?upper > lower)
Referred to SLT from Consultant Cough clinic
No benefit to cough with antibiotics/OCS/ICS – coughs more trying to use her Fostair.
Describes generalised laryngeal irritation, globus, no pain
No specific triggers, random
Can get chest ‘heaviness’ but? musculoskeletal as constant coughing
Reflux well controlled on PPIs
No dysphagia/dysphonia/rhinitis/PND concerns
Feels ‘going round in circles’, frustrated, cough aggravates Fibro, ME, ‘exhausted.’ Low mood. Doesn’t really go out much because of cough. Sleeping in separate room to partner.
Laryngoscopy = normal larynx but difficult to establish LHS/CRC as refused procedure unless lidocaine spray used. Likely LHS/CRC component based on history but advised complete Resp investigations +/- bronch first then re-refer SLT.
63 y/o Female – retired. Lives alone, husband recently passed away
PMHx: HTN, otherwise fit and well.
Long-standing cough, variably dry/productive; ‘as long as I can remember’. Self-rated 6/10.
Respiratory investigations = HRCT, PFTs normal. Bronch: raised neutrophils and eosinophils.
Treated with Azithromycin, resolved productive component of cough. Ongoing dry, irritative.
Referred to SLT from Consultant Cough clinic
Cough localised to throat/upper chest. Generalised irritation, feels like ‘flap in throat catches’ and causes cough
No specific triggers
No reflux/localised pain/dysphonia/dysphagia
Had FESS with ENT in 2020 – ongoing PND despite Dymista
As a result of cough staying at home a lot. Worried people will think she has COVID. Referred to local services for anxiety support/management.
Laryngoscopy = rhinitis and PND. Requested CNS review of nasal treatment and technique. SLT for hypersensitivity.
68 y/o Male – retired. No previous occupational exposures. Lives with wife
PMHx: previous hiatus hernia, reflux (managed on PPIs + Gaviscon), IBS
Respiratory investigations: HRCT thorax, PFTs = NAD. No lower airways concerns.
Reported some exertional breathlessness but resp/cardiac investigations normal and attributed to deconditioning.
Cough started prior to surgery for hiatus hernia (2018) when reflux was really bad
Can cough until retching but doesn’t happen that often any more
Referred to SLT from Consultant Cough clinic
On 5 mg MST BD – tolerating. Would ideally like to stop this in future.
Initially sought referral as wife concerned, but not overly bothered himself. Self-rated 4/10.
Intermittent throat-focused cough and throat clearing++
Triggers: none specific, worse with masks
Reflux now well controlled.? PND but nasal sprays gave him nosebleeds so stopped.
No dysphagia/dysphonia concerns
Laryngoscopy = LHS/CRC. No concerns. For SLT therapy.
48 y/o Female – off sick because of cough. Lives alone
PMHx: reflux, rhinitis, OA, spinal stenosis, restless legs
Respiratory investigations: ground glass changes? after bad infection approx. 5 years ago. No other concerns. PFTs, auscultation normal. No evidence asthma.
Denies SOB/sputum
Cough started 2019 after a bad virus/infection. Dry, laryngeal.
Can cough until dizzy/vomits, feels like about to pass out but no actual cough syncope. Very distressed. Self-rated 10/10. Currently not working as result.
Referred to SLT from Consultant Cough clinic
No response to antitussives – frustrated, just wants ‘magic pill’
Triggers: environmental smells, stress/anxiety, smoke, cold air, spicy foods
Limiting daily activities as very anxious about people looking at her when symptomatic
Referred for local anxiety management
No reflux concerns
Voice – moderately strained. No dysphagia.
Rhinitis feels well managed on Dymista.
Laryngoscopy = structurally and functionally normal at baseline but evidently sensitive. Significant A-P and L-M squeeze on phonation. For SLT therapy.
55 y/o Female. Works as nurse. Lives with husband
PMHx: nasal polyps, nil other significant
Reports low-level irritation in larynx +/- cough. Unsure of duration. Dry, Self-rated 2/10.
Respiratory investigations = normal CXR, HRCT, PFTs
No response to sx with previous trials of ICS, PPIs
Referred to SLT from Consultant Cough clinic
Could not tolerate antitussives – woozy, nauseous. Unable to work as a nurse with side effects so discontinued.
No SOB/dysphonia/dysphagia/localised pain/reflux
Ran out of Beconase and didn’t renew prescription – ongoing PND
Frequent throat clearing and finds it ‘annoying.’ Not really much impact on QoL – more aware of it in quiet environments, i.e. theatre
Laryngoscopy = rhinitis, advised restart nasal spray. Mild circumferential tension. No structural or functional concerns. For SLT therapy.
52 y/o Male. Works in IT. Lives with wife
PMHx: cataracts, T2DM
Respiratory investigations; normal PFTs, CXR, HRCT. No lower airways concerns.
Laryngeal cough for approximately 15 years. Self-rated 5/10.
Referred to SLT from Consultant cough clinic
Currently 10 mg MST BD – tolerating
SOB but felt due to BPD as avoids taking deep breath due to cough – feels he breathes differently to compensate. For consideration of Physio after SLT.
Feels globus and secretions in throat which often triggers cough. Otherwise, no exacerbating factors. Feels less confident – cough makes him feels self-conscious, especially at work.
Swallowing feels more ‘effortful’ but more in keeping with laryngeal tension than dysphagia
No chest infections
Voice feels ‘gravelly’
No reflux/rhinitis/PND
Laryngoscopy = PND – for nasal spray via GP. Moderate circumferential tension (likely die to posture/BPD). No structural/functional concerns. For SLT therapy
Appendix E.
TOM ILO score sheet
Therapy outcome measure instructions and scoring sheet
You have been provided with 10 case studies to rate using the TOMs ILO. Please refer to the descriptors when rating the case studies
Thank you!
Appendix F.
TOM CC score sheet
Therapy outcome measure instructions and scoring sheet
You have been provided with 10 case studies to rate using the TOMs COUGH. Please refer to the descriptors when rating the case studies
Thank you!