Abstract
The purpose of this review is to explore how fitness for purpose can be defined for anaesthesiology graduates and to delineate the parameters of this concept for anaesthesiology. Newly qualified anaesthesiology graduates experience difficulties with the transition from trainee to specialist, with perceptions of unpreparedness especially in non-technical skills. This may be deleterious to the individual, the patient, colleagues and the workplace. It is possible that graduates may be deemed competent yet are unable to fulfil all their specialist roles. Fitness for purpose and its relationship with competence, expertise and excellence in anaesthesiology have been poorly defined in the literature. These concepts are not synonymous but provide a hierarchical framework for the development of a specialist from a beginner to an expert. The uncertainties surrounding competence are numerous, with generic competency frameworks not addressing all aspects unique to anaesthesiology. The applicability of such frameworks in areas outside which they were originally designed and, in particular, in anaesthesiology, is questionable and requires further investigation. Defining fitness for purpose in anaesthesiology will assist training departments, curriculum designers, assessors and regulators to produce specialists that are experts in their chosen field without any deficiencies and thus able to perform all their required roles.
Introduction
Anaesthesiology is a dynamic speciality with an ever-increasing scope of practice. For anaesthesiologists to function optimally as perioperative physicians, it is essential that graduates perform adequately in all their professional roles. The aim of this review is to explore how fitness for purpose can be defined for anaesthesiology graduates and to delineate the parameters of this concept.
Fitness for purpose in medicine
Fitness for purpose has been studied extensively in non-medical professions such as architecture and construction, business, consumerism and aviation. The Oxford English Dictionary (OED) defines it as ‘suitable for the intended use; fully capable of performing the required task’.Citation1 In legal terms, it may mean ‘appropriate, and of the necessary standard or quality, for its intended use or purpose’.Citation2 From a consumerism perspective, it implies that the product created is suitable for its intended purpose and possesses qualities that are ideal for its expected use, situation and customers. The newly qualified specialist as a ‘product’ would thus need to meet a suitable standard and be deemed appropriate for use by consumers to be considered fit for purpose. Any effective production process must take into account the expectations of society as well as of the system into which the product will be placed.
Several studies illustrate that new specialists across varying disciplines often feel unprepared for aspects of their roles as specialists.Citation3–5 Junior doctors have felt unprepared or have been assessed as such by their seniorsCitation6–15 with preparedness rates as low as 42%.Citation8 This also applies to postgraduate training, with perceptions of unpreparedness experienced by both traineesCitation16 and specialists.Citation5,Citation17 Studies of newly qualified specialists suggest that some are more deficient in generic non-technical skills (NTS), for example managementCitation5 or leadership,Citation18–21 compared with their technical abilities.Citation3,Citation4,Citation19,Citation20,Citation22,Citation23
As with newly qualified junior doctors,Citation24 recently graduated specialists who are less well equipped for their work roles have reported varying but higher degrees of anxiety, stress and burnout compared with their older or more experienced colleagues. This may culminate in decreased quality of patient care and diminished job satisfaction.Citation5,Citation19,Citation22,Citation25,Citation26 Such issues should be addressed to ensure practitioner well-being and quality patient care.
Defining fitness for purpose in anaesthesiology
A clear understanding of fitness for purpose is necessary to determine whether new anaesthesiologists are ready for independent practice. Related themes that arise from relevant literature can be grouped conceptually into two categories:
The good doctor;
Competence, expertise and excellence.
The good doctor
Since the original oath of Hippocrates, doctors have striven to adhere to its principles, despite its inevitable modernisation.Citation27,Citation28 The application of expert clinical knowledge and care that are scientifically sound forms a thread throughout the oath. However, the ‘art’ of medicine is strongly advocated as a virtue for all good clinicians. The multiple roles that good doctors fulfil has long been recognised.
In defining a good doctor, perspectives vary among patients, the profession and regulatory bodies.
Patients’ views
How patients prioritise doctors’ skills and attributes is inherent in their satisfaction with the healthcare system to which the doctors belong.Citation29 The European Task Force on patients’ evaluations of General Practice (EUROPEP) revealed that patients rate a doctor’s ‘humanness’ as the most important aspect of patient care, followed by ‘competence/accuracy’, ‘patient involvement in decisions’ and ‘time for care’.Citation29 Studies on patients’ views, including an African perspective,Citation30 highlight the concurrent desire for clinicians to be technically skilled,Citation31 adept at maintaining interpersonal relationships and communication,Citation31 and able to meet appropriate levels of competence.Citation29,Citation32,Citation33
Learners’ views
In a study addressing learners’ views, students emphasised that ‘humanism in medicine’ cannot be neglected by striving for academic excellence alone. The need for ‘relational intelligence’ was highlighted with the ‘good doctor’ embracing ongoing learning and the formation, nurturing and assessment of relationships with the patient, colleagues, learners, society and the profession.Citation34 Student views consistently rank non-technical skills (NTS) such as listening, compassion, informative communication, non-discrimination and empathy as prioritiesCitation35,Citation36 in good doctors.
Anaesthesiologists’ views
In determining what constitutes a good anaesthesiologist, the opinions of anaesthesiologists themselves are invaluable. Components such as excellenceCitation37–41 and professionalismCitation42–45 have been explored; however, there remains a paucity of available literature on what anaesthesiologists believe a good or holistic practitioner should look like. Anaesthesiologists believe that their technical prowess alone is not sufficient and their NTS are important and need to be assessedCitation46 in order to prevent adverse outcomes.
Regulators’ views
Regulatory authorities provide practitioners with guidelines for good medical practice. These comprise rules of professional conduct and ethical principles against a country’s legal framework, to which all good doctors must adhere.Citation47,Citation48 Several specialist training and regulatory authorities have practice guidelines for specialists, which do not necessarily imply that specialists will be exceptional. They do, however, ensure that specialists at least meet a minimum standard deemed appropriate for that country to obtain licensure to practice.Citation49–51
Competence, expertise and excellence in anaesthesiology
In exploring whether the concept of fitness for purpose extends beyond just being a good doctor, it is important to describe terminologies that are sometimes used interchangeably.
Competence
Competence refers to ‘sufficiency of qualification; capacity to deal adequately with a subject’ and implies that a competent individual is sufficiently trained to manage his/her subject matter.Citation52 Various medical and educational definitions of competence exist with predominant features of the knowledge, skills, core values (attitudes) and behaviour that an individual should possess to perform the task for which he/she is trained.Citation53–55 Matveevskii, Moore and Samuels consider competence to be contextual, emphasising the role of the situation.Citation44 Competence comprises not only knowledge and skills, but a true understanding of work and the work environment with intuitive expert knowledge.Citation56,Citation57
Larsson suggests that providing an ‘all-encompassing’ definition of competence is difficult and that one should, rather, look at how it is used to better describe it.Citation56 Five dimensions of professional competence of anaesthesiologists are proposed:
Knowledge (theoretical)—encompassing a deeper approach to understanding rather than pure factual recall;Citation56
Skills (practical)—dependent on a ‘trained hand … a trained eye … and the ability to understand a situation in a holistic way’;Citation56
Anaesthetic non-technical skills (ANTS);Citation56
An understanding of the work being done—helping the patient and managing their physiology whilst leading the perioperative team and supporting the system;Citation56
Expert knowing that is intuitive in nature—having tacit knowledge that is primarily determined by knowing HOW rather than by knowing WHAT.Citation56
Expertise
An expert is ‘one whose special knowledge or skill causes him to be regarded as an authority; a specialist’.Citation58 Expertise is defined as ‘expert opinion or knowledge’ or ‘the quality or state of being an expert’.Citation59 Work experience alone may not be sufficient in becoming an expert, although it may contribute if it is reflective. Becoming an expert needs to include a context and process of learning and training within a given social role, thereby enabling one to become technically and non-technically adept. The expert makes use of fast thinking that is based on integrated tacit knowledge used subconsciously and without deliberation.Citation56,Citation60 Expert action is therefore spontaneous and frees up the individual to spend more time on tasks for which he/she has no expertise.Citation60
Excellence
Excellence is defined as ‘the possession chiefly of good qualities in an eminent or unusual degree; surpassing merit, skill, virtue, worth, etc.; … , eminence’.Citation61 In anaesthesiology, excellence implies transcending a minimum standard and is a goal towards which many aspire. Excellent anaesthesiologists are more than competent and effectively combine all their skillsCitation41 to become specialists that are exceptional rather than merely mediocre.
Glavin suggests that many tacit components of excellence have already formed part of the practice of anaesthesiology without explicit recognition.Citation41 He, like others,Citation37,Citation40 argues that several NTS may promote excellence in anaesthesiology, as these become more explicit and are effectively used in complex decision-making. However, many NTS have already been incorporated into competency frameworks, thereby implying their contribution to competence rather than to excellence. The question of what sets the excellent anaesthesiologist apart from the expert one thus arises.
Smith, Glavin and Greaves, in their UK-based Delphi-designed study of anaesthesiology experts, attempted to define excellence in anaesthesiology and considered possible ways to promote its practice in the discipline.Citation39 They suggested that excellence encompasses not only superior skills and knowledge, but also a group of personal attributes (personal qualities and personality functions) and their relationship within the work environment. The commonest distinguishing feature in their proposed definition was the continual desire to seek challenges and to learn from them, fostering an environment conducive to the pursuit of excellence.Citation39 However, this is what Larsson calls competence rather than excellence.Citation56 Smith and Greaves suggest that excellence may be defined as having an understanding of work,Citation40 although this again is what Larsson considers competence.Citation56 Smith proposes that excellence may be that elusive ‘something’ that binds all the components of a specialist together.Citation38 Defining the ‘something’ is difficult. It may refer to the way in which an excellent anaesthesiologist processes, integrates and incorporates the copious number of influences in a scenario to produce a favourable outcome. It may refer to an area of tacit knowledge that has not been fully elucidated, which allows one to have excellent results all the time. There remains, however, very little knowledge regarding markers or assessment of excellence to help embed it in anaesthesiology.
Competence, expertise and excellence are often used interchangeably when describing the process of attaining skills in specialist training; however, they are not synonymous but, rather, hierarchical. Competence can be seen as the minimum required to practise effectively, expertise as established capability with experience, and excellence as acknowledged superlative performance. Use of these terms often poses ambiguity, because of the various definitions of competence and its comparatives that exist in the literature, but it is important to remember that these concepts are distinctive.
Competence is the commonest term used when describing the training of specialists. As a threshold that all trainees must cross successfully, it requires further discussion to clarify not only the ambiguity associated with the term but also the ways in which training for competence has been approached, and various possible limitations of competency-based training.
Competency frameworks
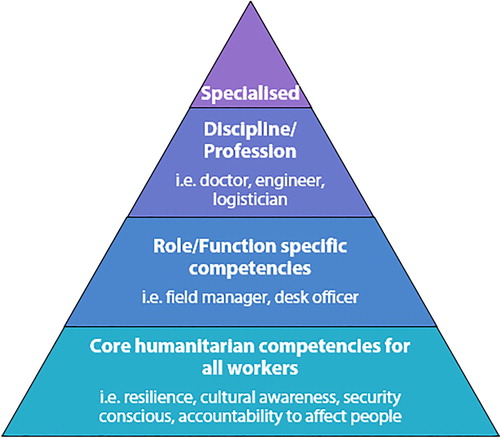
Competence is contextual in nature.Citation44 The competences of a worker become more specialised as his/her scope of practice narrows (see ).Citation54 A hierarchy of competences thus exists, and the core generic competences found in all doctors should be present in all specialists. Specialists, however, develop a new set of competences unique to that discipline that are deemed a minimum requirement to perform designated tasks.Citation54
Figure 1: The hierarchical nature of competency acquisition according to Walker and RussCitation54 (reproduced with permission).
Traditionally, competency was thought to be achieved after an appropriate, fixed contact time was spent in the relevant discipline, the so-called time-based or apprenticeship model. Recent insights have questioned the validity of this concept. All ‘products’ will not necessarily emerge from the process fully competent after a set time.Citation62 Trainees are exposed to different materials and assimilate information at different rates.Citation53 There is a move towards a competency-based training model, where individuals are trained and assessed in roles deemed appropriate for performance as independent practitioners. This outcomes-based approach considers assessment less subjective if concise, well-defined objectives are specified.Citation53
The Accreditation Council for Graduate Medical Education (ACGME) in the United States and the Royal College of Physicians and Surgeons of Canada oversee the training and teaching of their respective specialist trainees. Such oversight attempts to assure the public and medical community of the production of safe and competent practitioners. There has been a growing demand from all stakeholders for increased accountability of specialists resulting in organisations challenging their own standards and quality of training programmes to ensure that graduates remain fit for purpose. It was thus necessary to further formalise training with the goal of attaining minimum core technical and non-technical competences in a competency-based model. The ACGME, together with the American Board of Medical Specialties, established a set of six core competences upon which all their specialist training is based (see ).Citation53, Citation63, Citation64 Likewise, the Royal College of Physicians and Surgeons in Canada in 2005 created seven recently updated CanMEDS (Canadian Medical Education Directives for Specialists) competencesCitation65 (see ) for specialist training.
Table l: Core competences of medical specialists according to ACGME (Accreditation Council for Graduate Medical Education)Citation63 and CanMEDS (Canadian Medical Education Directives for Specialists)Citation65
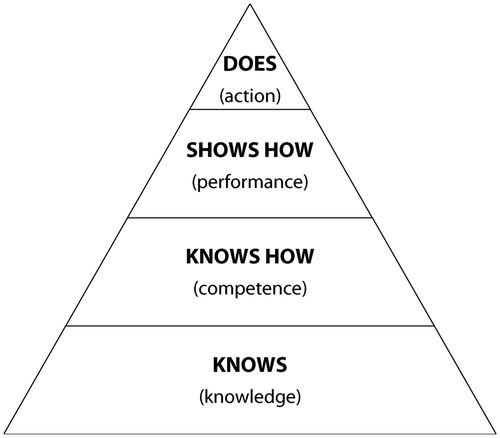
The ACGME and CanMEDS systems incorporate milestones considered as key components of a competent specialist. Achievement of these milestones is mandatory for trainees during their period of specialisation. Miller’s pyramid of clinical assessment (see ) suggests that cognitive processes are reflected by knowing and by asking why.Citation66 Assessing behavioural and psychomotor aspects of learning involves actual performance of a task, i.e. ‘shows how’ and ‘does’ (see ), and are more relevant to the application of knowledge after attaining competence.
Figure 2: Original pyramid of clinical assessment by Miller.Citation66
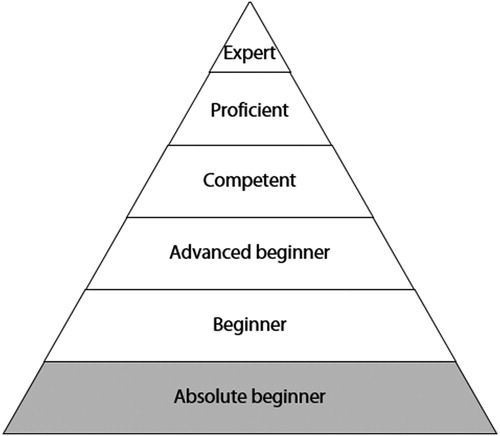
The Dreyfus five-stage model of skill acquisition describes how a beginner can progress through a period of training to become competent, proficient and ultimately an expert.Citation44,Citation53,Citation67 This was expanded by Park (see ) to include the absolute beginner stage.Citation67 According to Eraut, the early and mid-stages involve situational understanding of pattern recognition.Citation58 The latter stages of ‘proficiency’ and ‘expertise’ consist of tacit knowledge acquisition and work understanding during the course of training in various clinical scenarios, a concept shared by others.Citation44,Citation57 This pinnacle of expertise (see )Citation67 originally described by Dreyfus and DreyfusCitation60 must be attained at specialist graduation when one is granted licensure.
Figure 3: Modified Dreyfus model.Citation67
Core competences of an anaesthesiologist deemed a minimum requirement by patients, peers and training institutions can be broadly classified as technical and non-technical. Technical skills (knowledge and practical components of anaesthesiology practice) are generally well taught and emphasised in most postgraduate training programmes. However, the less taught but increasingly important NTS of anaesthesiology practice (attitudes, behaviours, attributes) have been considered ‘softer’ components and not emphasised as much during training.Citation68 Suggested reasons for this de-emphasis are that NTS are harder to teach and/or assess and form part of the so-called ‘hidden curriculum’, implying that they are learned from mentors and role-models rather than through formal teaching. If specialist anaesthesiologists are to become experts who are fit for purpose in every aspect of their practice, then the focus of teaching, training and assessment should balance technical with non-technical skills to avoid any deficits at graduation.
Limitations of competency frameworks and competency-based training
Context specificity
The ACGME and CanMEDS outcomes-based competency frameworks have been adopted by anaesthesiology regulators within the US and Canada respectively. Both frameworks’ component milestones establish the mandatory minimum for their anaesthesiologists. The practitioner who achieves these milestones is deemed competent. However, these milestones may be only contextually applicable since the frameworks were designed for these specific countries. Educators design training programmes according to the outcomes deemed appropriate for a specific set of needs. In high-income countries (HIC) it may be appropriate to focus on the needs of the individual consumer; however, in resource-poor low- and middle-income countries (LMIC), the needs of a nation may be prioritised over those of the individual. Training of anaesthesiologists needs to consider this, together with considerations of national demographics, education levels, ethnic groups and cultural practices of communities. North American models and milestones may not necessarily be applicable to other countries with their unique needs that drive production of anaesthesiologists.
Validity for anaesthesiology
Anaesthesia is a dynamic discipline and unique in some respects, as it involves integration of advanced technology, critical safety and complex tasks, and may, in certain scenarios, have a lot more in common with aviation than with other medical disciplines.Citation40 Interactions with patients are shorter and less complex but more intense than in other disciplines.Citation42 Competence in anaesthesiology cannot necessarily be assessed by means of attaining generic milestonesCitation40 suitable for all specialists. Milestones should be evaluated to include aspects unique to anaesthesiology before adoption.
Content and context
Learning in anaesthesiology requires the acquisition of technical and NTS. Unlike technical skills, NTS cannot be as easily subdivided into milestone components, and are therefore formally taught or learned less readily. Similarly, NTS cannot be assessed using the same tools as for technical skillsCitation69 or be assessed out of their relevant contexts. The importance of NTS is, however, clear as indicated by patients’ opinions.Citation29–33
Competency frameworks assume that competence is reached upon attainment of all individual milestones. The assumption that the individual is able to perform a task if he/she can perform the components of the task is not necessarily correct. Competences may be interdependent, and this may be missed by separating complex ones into individual components.Citation40,Citation70 Competences involving complex tasks that interrogate the integration of skills, especially if non-technical in nature (e.g. decision-making), cannot always be reduced to single tasks or to questions in an exam.Citation71 Since this is a dynamic process, they may be poorly assessed by current means.Citation71 Many of the competences are considered to be ‘meta-competences’ or highly complex competences that can be applied to several activities.Citation70 The reductionist nature of the milestones approach thus places anaesthesiologists at risk of merely being proficient in individual core components in their own work environment with their own patients according to their own assessors and standards. The possibility exists that one may be creating only parts of a whole productCitation62 and that these ‘competences in context’Citation72 do not always ensure that anaesthesiologists will become experts.
Ultimately, anaesthesiologists do not all work in the same environment, preferring either the public or private sectors, or an urban or rural setting. This may result in differing emphasis on particular competences (e.g. management of healthcare funders for the private practitioner); however, it is imperative that all specialist anaesthesiologists graduate with all the core competences that are necessary for independent practice irrespective of their subsequent placement.
Measuring competence in anaesthesiology
The ACGME and CanMEDS models are two of the currently accepted and accredited competency frameworks used, despite their potential limitations for anaesthesiology. Determining whether a trainee has attained clinical competence has been more achievable with traditional tools of assessment.Citation62 However, the non-technical bouquet of social, cognitive and personal skills is often missed, which subsequently led to the development of the anaesthetists’ non-technical skills (ANTS) rating scale in Scotland (see ).Citation73
Table 2: Components of the anaesthetists’ non-technical skills (ANTS) systemCitation73
Based on crew-resource management in the aviation industry, a hierarchical behaviour marker system and rating scale was devised to assess NTS unique to anaesthetists comprising four main categories (see ).Citation73 Each category comprises several elements with behavioural identifiers against which the individual could be rated. This model has limitations since it may not be appropriate in its entirety to particular scenarios, institutions or cultures, and has thus been modified by some,Citation74 requiring validation and reliability testing. The search for universally relevant tools for assessing NTS in anaesthesiology has been ongoing and has given rise to the consideration of simulation.Citation62 Simulation in anaesthesiology is growing in popularity, in part because it allows assessment of both technical and NTS simultaneously, as well as the ability to standardise scenarios, which is ideal for assessment. It also allows debriefing to take place, an important component of trainee instruction and learning that enables the trainee to modify his/her future behaviour(s). Attempts have already been made to combine milestones with simulation, but the latter requires validation.Citation62 Simulation has been used predominantly as a teaching rather than as an assessment toolCitation62 and its validity and reliability in summative testing has not been established, thus requiring further investigation. The cost of simulation, especially in LMIC where resources are limited, may be prohibitive.
Figure 4: The CanMEDS (Canadian Medical Education Directives for Specialists) Roles. Copyright © 2015, Royal College of Physicians and Surgeons of Canada. http://rcpsc.medical.org/canmeds. Reproduced with permission.
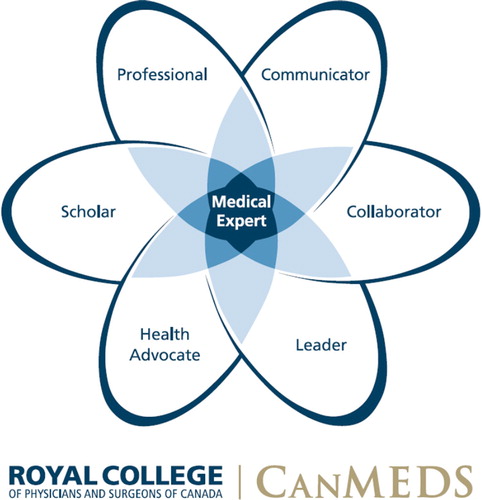
Smith and Greaves regard competence as an unfortunate term implying that the individual is completely capable of performing the whole task, which is not always the case.Citation40 Regulatory authorities using competency frameworks do not always state explicitly that practitioners meeting the criteria to obtain licensure are ‘competent’ but this is often inferred. Unpacking specialist roles or meta-competences into their components on which the individual is assessed does not imply that the overall role can be performed. This can result in a ‘component-competent’ specialist who, unfortunately, is incompetent in the overall task required.Citation40 Competence in this context thus implies only that the individual has sufficient skill to perform components of a task. Larsson, however, suggests that by appreciating the context of the task, by having an understanding of the work and its environment and by combining them with intuitive knowledge,Citation56 the individual evolves beyond the traditional understanding of competence. The evolution from competency to proficiency and beyond, as described by Dreyfus and Dreyfus,Citation60 results in the creation of the expert who can apply multiple competences to complex tasks in any context in anaesthesia without having to stop and deliberate (intuitive knowledge). If frameworks such as CanMEDS have medical expertise at the core of all their roles (see )Citation65 then those passing their assessments should be considered experts, as suggested by Dreyfus and DreyfusCitation60 (see ),Citation67 rather than ‘competent’ since competence forms part of expertise. According to CanMEDS, the definition of the Medical Expert is a physician who ‘integrates all of the CanMEDS roles, applying medical knowledge, clinical skills and professional values in their provision of high-quality and safe patient-centred care. It is the central physician role in the CanMEDS framework and defines the physician’s clinical scope of practice.’Citation65
It is important to note that despite the progression of a practitioner from competent to expert, NTS may still be deficient. We suggest that an anaesthesiologist who is fit for purpose is an expert without any deficiencies in either technical or non-technical skills.
Excellence however, surpasses fitness for purpose. What constitutes excellence in a specialist deemed fit for purpose requires further research. It may encompass an indication of the manner in which a specialist practises, or the ability to practise exceptionally well all the time. It may also relate to superlative patient outcomes, or the ability to innovate. As suggested by Miller,Citation75 excellence may make use of creativity, vision and leadership to explore uncharted waters and to surpass preconceived boundaries.
Conclusion
Fitness for purpose and its relationship with competence, expertise and excellence in anaesthesiology have been elusive concepts and poorly defined in the literature. Rather than being considered synonymous, they provide a hierarchical framework for the development of a specialist from a beginner to an eventual expert. The uncertainties surrounding competence are plentiful, with current generic competency frameworks perhaps not addressing all aspects of competence (e.g. NTS). Their applicability for the South African context, and validity for anaesthesiology, is questionable. These need to be explored before these frameworks can be used in environments outside North America. Since deficits in NTS exist in some graduates, these anaesthesiology experts are not currently fit for purpose despite qualifications citing licensure for practise. In order to protect both patients and practitioners, further exploration into fitness for purpose in anaesthesiology should be considered. Once fitness for purpose is attained by every graduate, then anaesthesiologists should set their sights on excellence, not only for maximal benefit of their patients but in pursuit of attaining their maximal human potential.
Acknowledgements
The authors would like to thank Dr Santosh Pershad and Professor Adrian Bosenberg for their assistance.
Disclosure statement
No conflict of interest was reported by the authors.
ORCID
Nicola Kalafatis http://orcid.org/0000-0002-1675-1963
Thomas Sommerville http://orcid.org/0000-0003-4556-8962
Pragasan Dean Gopalan http://orcid.org/0000-0002-3816-1171
References
- Oxford English Dictionary. ‘Fit for purpose’. Oxford University Press. Available from: http://www.oed.com/view/Entry/70747?redirectedFrom=fit+for+purpose#eid130154137
- Translegal English Dictionary. Available from: https://www.translegal.com/legal-english-dictionary/fit-for-purpose
- Morrow G, Illing J, Redfern N, et al. Are specialist registrars fully prepared for the role of consultant? Clin Teach. 2009;6:87–90. doi: 10.1111/j.1743-498X.2009.00272.x
- Morrow G, Burford B, Redfern N, et al. Does specialty training prepare doctors for senior roles? A questionnaire study of new UK consultants. Postgrad Med J. 2012;88(1044):558–65. doi: 10.1136/postgradmedj-2011-130460
- Beckett M, Hulbert D, Brown R. The new consultant survey 2005. Emerg Med J. 2006;23(6):461–3. doi: 10.1136/emj.2005.030726
- Green-Thompson LP, McInerney P, Manning DM, et al. Reflections of students graduating from a transforming medical curriculum in South Africa: a qualitative study. BMC Med Educ. 2012;12(1):49–57. https://doi.org/10.1186/1472-6920-12-49
- Peterlini M, Tiberio I, Saadeh A. Anxiety and depression in the first year of medical residency training. Med Educ. 2002;36:66–72. doi: 10.1046/j.1365-2923.2002.01104.x
- Cave J, Goldacre M, Lambert T, et al. Newly qualified doctors’ views about whether their medical school had trained them well: questionnaire surveys. BMC Med Educ. 2007;7:38–43. https://doi.org/10.1186/1472-6920-7-38
- Goldacre MJ, Taylor K, Lambert TW. Views of junior doctors about whether their medical school prepared them well for work: questionnaire surveys. BMC Med Educ. 2010;10:78–87. https://doi.org/10.1186/1472-6920-10-78
- Tallentire VR, Smith SE, Skinner J, et al. The preparedness of UK graduates in acute care: a systematic literature review. Postgrad Med J. 2012;88(1041):365–71. doi: 10.1136/postgradmedj-2011-130232
- Tallentire VR, Smith SE, Wylde K, et al. Are medical graduates ready to face the challenges of Foundation training? Postgrad Med J. 2011;87(1031):590–5. doi: 10.1136/pgmj.2010.115659
- Morrow G, Johnson N, Burford B, et al. Preparedness for practice: the perceptions of medical graduates and clinical teams. Med Teach. 2012;34(2):123–35. doi: 10.3109/0142159X.2012.643260
- Ochsmann EB, Zier U, Drexler H, et al. Well prepared for work? Junior doctors’ self-assessment after medical education. BMC Med Educ. 2011;11:99–108. https://doi.org/10.1186/1472-6920-11-99
- Evans DE, Roberts CM. Preparation for practice: how can medical schools better prepare PRHOs? Med Teac. 2006;28(6):549–52. doi: 10.1080/01421590600628399
- Matheson C. How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgrad Med J. 2009;85(1009):582–9. doi: 10.1136/pgmj.2008.071639
- Blumenthal D, Gokhale M, Campbell EG, et al. Preparedness for clinical practice: reports of graduating residents at academic health centers. JAMA. 2001;286(9):1027–34. doi: 10.1001/jama.286.9.1027
- Amin HJ, Singhal N, Cole G. Validating objectives and training in Canadian paediatrics residency training programmes. Med Teach. 2011;33(3):e131–44. doi: 10.3109/0142159X.2011.542525
- Rama-Maceiras P, Parente S, Kranke P. Job satisfaction, stress and burnout in anaesthesia: relevant topics for anaesthesiologists and healthcare managers? Eur J Anaesthesiol. 2012;29(7):311–9. doi: 10.1097/EJA.0b013e328352816d
- Dijkstra IS, Pols J, Remmelts P, et al. Preparedness for practice: a systematic cross-specialty evaluation of the alignment between postgraduate medical education and independent practice. Med Teach. 2015;37(2):153–61. doi: 10.3109/0142159X.2014.929646
- Higgins R, Gallen D, Whiteman S. Meeting the non-clinical education and training needs of new consultants. Postgrad Med J. 2005;81(958):519–23. doi: 10.1136/pgmj.2004.028902
- McKinstry B, Macnicol M, Elliot K, et al. The transition from learner to provider/teacher: the learning needs of new orthopaedic consultants. BMC Med Educ. 2005;5(1):17–23. https://doi.org/10.1186/1472-6920-5-17
- Westerman M, Teunissen PW, Fokkema JP, et al. The transition to hospital consultant and the influence of preparedness, social support, and perception: a structural equation modelling approach. Med Teach. 2013;35(4):320–7. doi: 10.3109/0142159X.2012.735381
- Lieberman L, Hilliard RI. How well do paediatric residency programmes prepare residents for clinical practice and their future careers? Med Educ. 2006;40(6):539–46. doi: 10.1111/j.1365-2929.2006.02479.x
- Van Hamel C, Jenner LE. Prepared for practice? A national survey of UK foundation doctors and their supervisors. Med Teac. 2015;37(2):181–8. doi: 10.3109/0142159X.2014.947929
- Westerman M, Teunissen PW, Jørgensen RL, et al. The transition to hospital consultant: Denmark and the Netherlands compared on preparedness for practice, perceived intensity and contextual factors. Med Teac. 2013;35(6):481–9. doi: 10.3109/0142159X.2013.774332
- Rama-Maceiras P, Jokinen J, Kranke P. Stress and burnout in anaesthesia: a real world problem? Curr Opin Anaesthesiol. 2015;28(2):151–8. doi: 10.1097/ACO.0000000000000169
- Edelstein L. The Hippocratic oath: text, translation and interpretation. Ann Arbor: University Microfilms International; 1973.
- Shewan A, Shewan A. University of St A, library, Shewan C. Greek hero cults and ideas of immortality. The Gifford lectures delivered in the University of St. Andrews in the year 1920. By Lewis Richard Farnell. Oxford: Clarendon Press; 1921. p. 434. 18s. 1921.
- Wensing M, Jung H, Mainz J, et al. A systematic review of the literature on patient priorities for general practice care. Part 1: description of the research domain. Soc Sci Med. 1998;47(10):1573–88. doi: 10.1016/S0277-9536(98)00222-6
- Pfeiffer A, Noden B, Walker Z, et al. General population and medical student perceptions of good and bad doctors in Mozambique. Educ Health (Abingdon, England). 2011;24(1):387–98.
- Martin S. What is a good doctor? Patient perspective. Am J Obstet Gynecol. 1998;178(4):752–4. doi: 10.1016/S0002-9378(98)70486-7
- Hurwitz B, Vass A. What’s a good doctor, and how can you make one? By marrying the applied scientist to the medical humanist. BMJ: Brit Med J. 2002;325(7366):667–8. doi: 10.1136/bmj.325.7366.667
- Coulter A. Patients’ views of the good doctor: doctors have to earn patients’ trust. BMJ: Brit Med J. 2002;325(7366):668–9. doi: 10.1136/bmj.325.7366.668
- Rutberg PC, King B, Gaufberg E, et al. Do medical students’ narrative representations of ‘the good doctor’ change over time? Comparing humanism essays from a national contest in 1999 and 2013. Acad Med. 2017;92(4):537–43. doi: 10.1097/ACM.0000000000001531
- Maudsley G, Williams EM, Taylor DC. Junior medical students’ notions of a ‘good doctor’ and related expectations: a mixed methods study. Med Educ. 2007;41(5):476–86. doi: 10.1111/j.1365-2929.2007.02729.x
- García-Huidobro D, Núñez F, Vargas P, et al. Undergraduate medical students’ expectative of their desired profile as medical doctors. Rev Med De Chile. 2006;134(8):947–54. doi: 10.4067/S0034-98872006000800001
- Larsson J, Holmstrom IK. How excellent anaesthetists perform in the operating theatre: a qualitative study on non-technical skills. Br J Anaesth. 2013;110(1):115–21. doi: 10.1093/bja/aes359
- Smith A. In search of excellence in anesthesiology. Anesthesiology. 2009;110:4–5. doi: 10.1097/ALN.0b013e318190b263
- Smith AF, Glavin R, Greaves JD. Defining excellence in anaesthesia: the role of personal qualities and practice environment. Br J Anaesth. 2011;106(1):38–43. doi: 10.1093/bja/aeq308
- Smith AF, Greaves JD. Beyond competence: defining and promoting excellence in anaesthesia. Anaesthesia. 2010;65(2):184–91. doi: 10.1111/j.1365-2044.2009.06162.x
- Glavin RJ. Excellence in anesthesiology. Anesthesiology. 2009;110:201–3.
- Edelstein SB, Stevenson JM, Broad K. Teaching professionalism during anesthesiology training. J Clin Anesth. 2005;17(5):392–8. doi: 10.1016/j.jclinane.2004.10.006
- Kearney RA. Defining professionalism in anaesthesiology. Med Educ. 2005;39(8):769–76. doi: 10.1111/j.1365-2929.2005.02233.x
- Matveevskii A, Moore DL, Samuels PJ. Competency and professionalism in medicine. Clin Teach. 2012;9:75–9. doi: 10.1111/j.1743-498X.2012.00539.x
- McKenna J, Rosen HD. Competency-based professionalism in anesthesiology: continuing professional development. Can J Anaesth. 2012;59(9):889–908. doi: 10.1007/s12630-012-9747-z
- Gaba D. What makes a ‘good’ anesthesiologist? Anesthesiology 2004;101:1061–3. doi: 10.1097/00000542-200411000-00003
- Health Professions Council of South Africa. Available from: http://www.hpcsa.co.za/Conduct/Ethics
- General Medical Council. Available from: https://www.gmc-uk.org/guidance/10058.asp
- Anaesthetists TRCo. The Good Anaesthetist. Standards of practice for career grade anaesthetists 2010. Available from: https://www.aagbi.org/sites/default/files/good_anaesthetist_2010.pdf
- Dobson G, Chong M, Chow L, et al. Guidelines to the practice of anesthesia – revised edition 2017. Can J Anaesth. 2017;64(1):65–91. doi: 10.1007/s12630-016-0749-0
- Anaesthesiologists SASo. South African society of anaesthesiologists. SASA practice guidelines 2013. 2012 Revision. S Afr JAnaesth Analg. 2013;19(1):S1–S42.
- The Oxford English Dictionary-’competence‘. Oxford University Press; [10]. Available from: http://www.oed.com/view/Entry/37567?redirectedFrom=competence
- Ebert T, Fox C. Competency-based education in anesthesiology. Anesthesiology. 2014;120:24–31. doi: 10.1097/ALN.0000000000000039
- Walker P, Russ C. Fit for purpose: the role of modern professionalism in evolving the humanitarian endeavour. Int Rev Red Cross. 2011;93(884):1193–210. doi: 10.1017/S1816383112000276
- Becke K, Johr M. Etiquette, competence, and professionalism: the profile of the ‘ideal pediatric anesthesiologist’. Paediatr Anaesth. 2017;27(2):116–7. doi: 10.1111/pan.13096
- Larsson J. Monitoring the anaesthetist in the operating theatre – professional competence and patient safety. Anaesthesia. 2017;72 Suppl 1:76–83. doi: 10.1111/anae.13743
- Sandberg J. Understanding human competence at work: an interpretative approach. Acad Manage J. 2000;43(1):9–25.
- Eraut M. Expert and expertise: meanings and perspectives. Lear Health Soc Care. 2005;4:173–9. doi: 10.1111/j.1473-6861.2005.00102.x
- The Oxford English Dictionary-’expertise‘. Oxford University Press. Available from: http://www.oed.com/view/Entry/66556?redirectedFrom=expertise
- Dreyfus H, Dreyfus S. Mind over machine: the power of human intuition and expertise in the era of the computer. New York: The Free Press; 1986.
- The Oxford English Dictionary-’excellence’. Oxford University Press. Available from: http://www.oed.com/view/Entry/65701?redirectedFrom=excellence#eid
- Chin M, Lagasse RS. Assessment of competence: developing trends and ethical considerations. Curr Opin Anaesthesiol. 2017;30(2):236–41. doi: 10.1097/ACO.0000000000000431
- Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29(7):648–54. doi: 10.1080/01421590701392903
- Mainiero M, Lourenco A. The ACGME core competencies: changing the way we educate and evaluate residents. Med Health Rhode Isl. 2011;94(6):164–7.
- Frank J, Snell L, Sherbino Jea, editors. The draft CanMEDS 2015 physician competency framework-eeries IV. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2015. 2015 March.
- Miller G. The Assessment of clinical skills/competence/performance. Acad Med. 1990;65(9):S63–S7. doi: 10.1097/00001888-199009000-00045
- Park J. Proposal for a modified dreyfus and miller model with simplified competency level descriptions for performing self-rated surveys. J Educ Eval Health Prof. 2015;12:54–7. http://doi.org/10.3352/jeehp.2015.12.54
- UK education ‘will not be fit for purpose’ [Article]. Institution of chemical engineers; 2014 [18]. Available: http://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=97450690&site=ehost-live
- Holmboe ES, Ward DS, Reznick RK, et al. Faculty development in assessment: the missing link in competency-based medical education. Acad Med. 2011;86(4):460–7. doi: 10.1097/ACM.0b013e31820cb2a7
- Leung W-C. Learning in practice. BMJ. 2002;325:693–6. doi: 10.1136/bmj.325.7366.693
- Patel BS, Feerick A. Will competency assessment improve the training and skills of the trainee anaesthetist? Anaesthesia. 2002;57:711–2. doi: 10.1046/j.1365-2044.2002.27092.x
- Snell LS, Frank JR. Competencies, the tea bag model, and the end of time. Med Teach. 2010;32(8):629–30. doi: 10.3109/0142159X.2010.500707
- Patey R, Flin R, Fletcher G, et al. Developing a taxonomy of anesthetists’ nontechnical skills (ANTS). 2005. In: Advances in patient safety: from research to implementation (Vol 4: Programs, tools and products) [Internet]. Agency for healthcare research and quality (US); [325–36].
- Jepsen RMHG, Spanager L, Lyk-Jensen HT, et al. Customisation of an instrument to assess anaesthesiologists’ non-technical skills. Int J Med Educ. 2015;6:17–25. doi: 10.5116/ijme.54be.8f08
- Miller R. The Pursuit of excellence. Anesthesiology. 2009;110(4):714–20. doi: 10.1097/ALN.0b013e31819c72f9
