ABSTRACT
Multicenter case series has reported patients with hepatic injury following COVID-19 vaccination, which raised concern for the possibility of vaccine-induced liver dysfunction. We aimed to assess the impact of COVID-19 vaccination on liver function of pregnant women, who may be uniquely susceptible to vaccine-induced liver dysfunction. We conducted a retrospective cohort study at a tertiary hospital in Shanghai, China. Vaccine administration was obtained from the electronic vaccination record. Serum levels of alanine transaminase (ALT), aspartate transaminase (AST), total bile acid (TBA) and total bilirubin (TBIL) in early pregnancy were determined by enzymatic methods. Among the 7745 included pregnant women, 3832 (49.5%) received at least two doses of an inactivated vaccine. COVID-19 vaccination was significantly associated with higher levels of maternal serum TBA. Compared with unvaccinated pregnant women, the mean TBA levels increased by 0.17 μmol/L (β = 0.17, 95% CI, 0.04, 0.31) for women who had been vaccinated within 3 months before the date of conception. Moreover, COVID-19 vaccination was significantly associated with an increased risk of maternal hyperbileacidemia. The risk of hyperbileacidemia increased by 113% (RR = 2.13; 95% CI, 1.17-3.87) for pregnant women who had been vaccinated within 3 months before conception compared with unvaccinated pregnant women. However, when the interval from complete vaccination to conception was prolonged to more than 3 months, COVID-19 vaccination was not associated with serum TBA levels or maternal hyperbileacidemia. Our findings suggest that vaccination with inactivated COVID-19 vaccines more than 3 months before conception have no detrimental effects on maternal liver function in early pregnancy.
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has caused a major public health crisis since early 2020 [Citation1]. Vaccination is the most important method of pandemic control [Citation2]. As of June 1, 2022, more than 5 billion persons have been vaccinated with coronavirus disease 2019 (COVID-19) vaccines worldwide [Citation3]. Despite the high COVID-19 vaccination coverage, potential vaccine-induced adverse effects, especially for pregnant women who were excluded from the initial randomized controlled trials testing the safety and efficacy of COVID-19 vaccines, have not yet been fully characterized [Citation4].
The side effects related to COVID-19 vaccines are typically mild and usually resolve within 1–3 days after vaccination. These side effects include local adverse events (injection site pain, swelling and redness) and systemic reactions (fever, fatigue, headache and myalgia) [Citation5, Citation6]. In addition, COVID-19 vaccination has also been linked to the development of some autoimmune diseases, such as Graves’ disease, myocarditis and immune thrombocytopenic purpura [Citation7–14]. Recently, a multicenter case series reported 16 patients with hepatic injury following mRNA-based COVID-19 vaccination [Citation15]. Although the causality could not be proven, it raised concern for the possibility of vaccine-induced liver injury. However, no study has reported the effect of COVID-19 vaccination on liver function among pregnant women, who may be uniquely susceptible to vaccine-induced liver dysfunction.
In China, pregnant women are not recommended to receive COVID-19 vaccines. Using data from a retrospective cohort study of 7745 Chinese pregnant women, we examined the association of COVID-19 vaccination before conception with maternal liver function in early pregnancy. We hope our findings will add safety information related to COVID-19 vaccination for pregnant women or women who are trying to conceive.
Materials and methods
Study participants
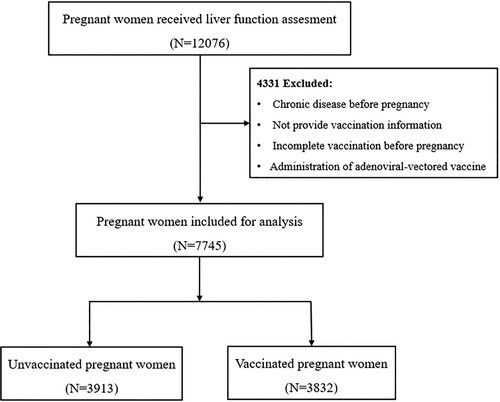
This retrospective cohort study was conducted at the Shanghai First Maternity and Infant Hospital, which is one of the largest prenatal health care providers in China, with more than 25000 deliveries per year. Participants were pregnant women who were registered at the hospital’s department of obstetrics from September 2021 to January 2022. The flowchart of participant enrolment is shown in . Briefly, 12076 singleton pregnant women who received liver function assessments in early pregnancy were screened for eligibility. We excluded 4331 pregnant women with chronic disease before pregnancy, women who did not provide vaccination information, women who did not complete vaccination before pregnancy and women who received adenoviral-vectored vaccines. Ethics approval was obtained from the Ethics Committee of the Shanghai First Maternity and Infant Hospital.
Exposure
Vaccine administration data were collected from each participating woman’s electronic vaccination record. These data included the vaccine type and manufacturer, number of vaccine doses and date of vaccination. In China, the most commonly used COVID-19 vaccines are inactivated virus vaccines. Therefore, we focused on inactivated COVID-19 vaccines. Participating pregnant women were categorized as exposed if they received at least two doses of an inactivated vaccine before conception. Since pregnant women are not recommended to receive COVID-19 vaccines in China, no unvaccinated participating pregnant women received the vaccine after conception.
Assessment of covariates
Demographic characteristics regarding maternal age (MA), body weight and height before pregnancy, and reproductive history, such as maternal parity (nulliparous or multiparous), abortion history (yes or no) and mode of conception (conceived naturally or conceived through the use of artificial reproductive technology), were extracted from the hospital’s electronic medical record system. Gestational age (GA) at the time of the liver function assessment was calculated from the last menstrual period to the date of the liver function assessment. Prepregnancy body mass index (BMI) was calculated as weight (kg) divided by body height in metres squared (m2) and was classified into three categories: underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.9 kg/m2), and overweight or obese (BMI ≥ 25.0 kg/m2).
Outcomes
The main outcome of interest was maternal liver function, which was assessed by measuring serum levels of alanine transaminase (ALT), aspartate transaminase (AST), total bile acid (TBA) and total bilirubin (TBIL) during early pregnancy. The laboratory reference ranges of ALT, AST, TBA and TBIL were 1–40 U/L, 2–40 U/L, 0–10 μmol/L and 0-17.1 μmol/L, respectively. The diagnostic standards for hyperbileacidemia were serum levels of TBA higher than 10 μmol/L.
Statistical analysis
According to their vaccination status, all participating pregnant women were categorized into vaccinated and unvaccinated groups. The general characteristics of the two groups are presented as percentages (%) and were compared using the chi-square test. Continuous serum ALT, AST, TBA and TBIL are depicted as the mean ± SD and were compared between the two groups using the two-sample t test.
We first conducted multiple linear regression models to assess the associations of COVID-19 vaccination with serum levels of ALT, AST, TBA and TBIL. In linear regression models, vaccination status (yes/no) was fitted as an independent variable, whereas each liver function parameter was fitted as a dependent variable. We considered GA at the time of the liver function assessment, MA, parity, mode of conception, abortion history and prepregnancy BMI as potential confounders. Given one study observed that the binding and neutralizing antibodies declined over time 3 months after receiving two doses of an inactivated virus vaccine [Citation16], based on the time intervals from complete vaccination to the date of conception, vaccinated participants were further divided into two subgroups: ≤ 3 months and > 3 months since vaccination. We then estimated the association between the time intervals and each liver function parameter with the unvaccinated group serving as a reference.
We subsequently performed multivariable log-binomial regression analysis to estimate the relative risk (RR) and 95% CI for the associations of COVID-19 vaccination with a dichotomous outcome: maternal hyperbileacidemia. We adjusted for the same confounders as those in linear regression analysis. In log-binomial regression analysis, the association between the time intervals from complete vaccination to the date of conception and the risk of maternal hyperbileacidemia was also estimated with the unvaccinated group serving as the reference.
As a sensitivity analysis to address the confounding effects of liver dysfunction in a previous pregnancy, we replicated all linear regression models restricted to nulliparous pregnant women. Another sensitivity analysis was conducted to ensure that the observed associations were not confounded by the mode of conception by replicating linear regression models to participating women who conceived naturally. In a third sensitivity analysis, we replicated regression models restricted to participants with no prior history of abortion. All statistical analyses were performed using R statistical software version 3.2.3 (R Project for Statistical Computing), and a 2-sided P < 0.05 was considered significant.
Results
Demographic characteristics of the participants
After exclusion, 7745 pregnant women were included in the final analysis. As shown in Table S1, there was no significant difference in MA, parity, prepregnancy BMI or mode of conception between the included and excluded subjects. However, the prevalence of abortion was slightly higher in the included subjects than in the excluded subjects (24.2% vs. 21.9%, P = 0.004). The general characteristics of the included subjects are summarized in . Of the 7745 included pregnant women, 3832 (49.5%) completed vaccination before conception (1636 completed vaccination within 3 months of conception, and 2196 completed vaccination before 3 months of conception), while 3913 (50.5%) did not receive any COVID-19 vaccine before their liver function assessment. The vaccinated and unvaccinated groups did not differ in MA or prepregnancy BMI. However, compared with the unvaccinated pregnant women, the vaccinated pregnant women were more likely to be multiparous and less likely to have a prior abortion history or conceive through the use of ART.
Table 1. General characteristics of the participating pregnant women.
Distribution of serum levels of ALS, AST, TBIL and TBA
Serum levels of ALT, AST, TBIL and TBA were measured and compared between the vaccinated and unvaccinated groups (). The mean (± SD) ALS, AST, TBA and TBIL levels of the 7745 participating pregnant women were 19.13 ± 18.54 µmol/L, 19.61 ± 8.39 µmol/L, 2.26 ± 2.27 U/L and 9.27 ± 3.49 U/L, respectively.
Table 2. Distribution of serum ALT, AST, TBA and TBIL in early pregnancy.
Analyses of the differences in serum liver function parameters between the two groups showed that serum levels of ALT (18.59 vs. 19.66, P = 0.011) and AST (19.37 vs. 19.84, P = 0.012) were significantly lower in vaccinated pregnant women than in vaccinated pregnant women. In contrast, serum levels of TBA (2.33 vs. 2.20, P = 0.022) and TBIL (9.42 vs. 9.13, P < 0.001) were significantly higher in vaccinated pregnant women than in vaccinated pregnant women.
Association of COVID-19 vaccination with serum levels of ALS, AST, TBIL and TBA
The adjusted associations of COVID-19 vaccination with serum levels of ALT, AST, TBA and TBIL are presented in . We found that COVID-19 vaccination was not significantly associated with serum levels of ALT, AST or TBIL. COVID-19 vaccination was significantly associated with higher levels of serum TBA. Compared with unvaccinated pregnant women, pregnant women who had been vaccinated within 3 months before the date of conception showed an increase in the mean TBA level of 0.17 U/L (β = 0.17, 95% CI, 0.04, 0.31). However, when the time interval from complete vaccination to the date of conception was prolonged to more than 3 months, COVID-19 vaccination was not associated with serum levels of TBA.
Table 3. Effect estimates (95% CI) of serum ALT, AST, TBA and TBIL levels associated with COVID-19 vaccination before conception.
Sensitivity analysis
In the sensitivity analysis, when restricting the analysis to nulliparous pregnant women, the associations of COVID-19 vaccination with TBA were similar to those observed in all participating pregnant women (Table S2). Further limiting the analysis to pregnant women who conceived naturally yielded generally similar findings (Table S3). In addition, compared with the main results, the observed associations did not change significantly when limiting the analysis to pregnant women with no prior history of abortion (Table S4).
Association of COVID-19 vaccination with risk of maternal hyperbileacidemia
Given that linear regression analysis demonstrated that COVID-19 vaccination was associated with higher serum levels of TBA, we sought to examine the associations of COVID-19 vaccination with the risk of maternal hyperbileacidemia. As shown in , COVID-19 vaccination was associated with an increased risk of maternal hyperbileacidemia. In the adjusted model, compared with unvaccinated pregnant women, women who had been vaccinated within 3 months before the date of conception had a risk of maternal hyperbileacidemia that increased by 113% (RR = 2.13; 95% CI, 1.17, 3.87). However, when the time interval from complete vaccination to the date of conception was prolonged to more than 3 months, COVID-19 vaccination was not significantly associated with maternal hyperbileacidemia.
Table 4. Relative risk of maternal hyperbileacidemia associated with COVID-19 vaccination before pregnancy.
Discussion
The most intuitive expected toxicity of COVID-19 vaccines is related to immune activation. Therefore, the side effects are usually mild and self-limiting, and very few serious adverse events are reported [Citation17]. In this cohort of 7745 Chinese pregnant women, we provided a comprehensive assessment of the effect of COVID-19 vaccination on maternal liver function in early pregnancy. We found that pregnant women who had been vaccinated within 3 months before the date of conception had higher serum TBA levels than those who had not been vaccinated. In addition, we found that COVID-19 vaccination within 3 months before the date of conception was associated with an increased risk of maternal hyperbileacidemia. Since higher serum TBA is considered to be an indicator of hepatobiliary impairment or disease [Citation18], our findings might suggest the possibility of COVID-19 vaccine-induced liver injury.
Although rare, evidence of liver injury related to COVID-19 vaccination has emerged recently. In a multicenter case series, Shroff H et al. reported 16 patients with liver injury following mRNA-based COVID-19 vaccination. Of the 16 patients, 13 demonstrated a hepatocellular pattern of liver injury [Citation15]. In another study, Dumortier J reported a case of a liver transplant recipient who presented mild liver injury after the first dose of an mRNA vaccine. In addition to liver injury, a growing number of case reports reporting individuals who developed autoimmune hepatitis following mRNA-based COVID-19 vaccination have begun to emerge, and molecular mimicry is supposed to be the potential mechanism underlying vaccine-induced autoimmune conditions [Citation19–26].
Our study is the first to examine the association of COVID-19 vaccination before conception with liver function among pregnant women. We observed higher levels of serum TBA and an increased risk of maternal hyperbileacidemia in association with COVID-19 vaccination within 3 months before the date of conception. The observed association of COVID-19 vaccination with serum TBA was consistent with a recent study conducted by Liu et al. With 11 healthy adult volunteers, they observed significantly elevated serum levels of TBA at Day 7 after the first dose of an inactivated COVID-19 vaccine [Citation27].
The mechanisms through which inactivated vaccines impact liver function have not been elucidated. Similar to SARS-CoV-2 infection, vaccinated with mRNA COVID-19 vaccines could also trigger autoimmune responses through cross-reactivity with host cells [Citation28], which may induce liver injury with autoimmune features. In addition, one study observed an enrichment of T cells in different areas of the liver that were reactive to mRNA COVID-19 vaccine [Citation29]. The activation of intrahepatic T cells may lead to immune-mediated liver injury [Citation30]. Although inactivated vaccines have lower immunogenicity than mRNA vaccines [Citation31], they may trigger similar immune and autoimmune responses. We hypothesized that the alterations in maternal liver function might be attributed to inactivated vaccine-induced immune and autoimmune responses, especially the responses within 3 months after receiving two-dose inactivated vaccines.
Considering that the estimated increase in serum TBA is relatively small (0.17 U/L), the clinical relevance of the present findings merits further discussion. Our findings do not intend to discourage health care providers from prescribing inactivated COVID-19 vaccines to women who are trying to conceive. In contrast, we raise awareness about the potential adverse effects of COVID-19 vaccination on liver function among pregnant women and suggest that COVID-19 vaccination should be performed more than 3 months before the date of conception.
Bearing certain limitations, our results should be interpreted with caution. First, although the sample size is quite large (N = 7745), our study is an observational study and the existence of residual confounders may not be ruled out. Second, due to the retrospective design of the present study, we could not assess the antibody levels of each participant. However, no participant had ever been infected with SARS-CoV-2 before the date of their liver function assessment, and therefore, no participant in the unvaccinated group developed natural antibodies. Third, all vaccinated pregnant women received inactivated COVID-19 vaccines, and we could not compare the effect of different types of COVID-19 vaccines on maternal liver function. Fourth, all participating pregnant women were from one of the largest cities in China, and most participants were of Han ethnicity, which may limit the generalizability of our findings.
Our study provides the first evidence that vaccination with inactivated COVID-19 vaccines more than 3 months before conception does not result in any detrimental effects on maternal liver function in early pregnancy. Our findings may contribute to the mounting evidence that supports the safety of COVID-19 vaccination in pregnant women or women who are trying to conceive.
Authors contributions
The study was designed by LPJ and YZ. Acquisition, analysis, or interpretation of data were done by LPJ and YZ. Drafting of the manuscript was done by YZ and YBZ. Statistical analysis was done by YZ and YBZ. YZ, YBZ, YCZ, ZYZ, YJZ, MYL and XS provided administrative, technical and material support. LPJ obtained the funding and had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. All authors contributed to the reviewing and approved the final version.
Supplemental Material
Download MS Word (22.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Tsang HF, Chan LWC, Cho WCS, et al. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther. 2021;19(7):877–888.
- Viana J, van Dorp CH, Nunes A, et al. Controlling the pandemic during the SARS-CoV-2 vaccination rollout. Nat Commun. 2021;12(1):3674.
- Lim CH, Ryu J, Choi Y, et al. Understanding global PM2.5 concentrations and their drivers in recent decades (1998-2016). Environ Int. 2020;144:106011.
- Meo SA, Bukhari IA, Akram J, et al. COVID-19 vaccines: comparison of biological, pharmacological characteristics and adverse effects of pfizer/BioNTech and moderna vaccines. Eur Rev Med Pharmacol Sci. 2021 Feb;25(3):1663–1669.
- Riad A, Pokorna A, Attia S, et al. Prevalence of COVID-19 vaccine side effects among healthcare workers in the Czech republic. J Clin Med. 2021 Apr 1;10(7).
- Al Khames Aga QA, Alkhaffaf WH, Hatem TH, et al. Safety of COVID-19 vaccines. J Med Virol 2021;93(12):6588–6594.
- Hines A, Shen JG, Olazagasti C, et al. Immune thrombocytopenic purpura and acute liver injury after COVID-19 vaccine. BMJ Case Rep. 2021 Jul 30;14(7).
- Jawed M, Khalid A, Rubin M, et al. Acute immune thrombocytopenia (ITP) following COVID-19 vaccination in a patient With previously stable ITP. Open Forum Infect Dis. 2021;8(7):ofab343.
- Schimmel J, Alba EL, Chen A, et al. Letter to the editor: thyroiditis and thyrotoxicosis after the SARS-CoV-2 mRNA Vaccine. Thyroid. 2021;31(9):1440.
- Chee YJ, Liew H, Hoi WH, et al. SARS-CoV-2 mRNA vaccination and graves’ disease: a report of 12 cases and review of the literature. J Clin Endocrinol Metab. 2022;107(6):e2324–e2330.
- Bostan H, Ucan B, Kizilgul M, et al. Relapsed and newly diagnosed graves’ disease due to immunization against COVID-19: A case series and review of the literature. J Autoimmun 2022;128:102809.
- Jafarzadeh A, Nemati M, Jafarzadeh S, et al. Thyroid dysfunction following vaccination with COVID-19 vaccines: a basic review of the preliminary evidence. J Endocrinol Invest. 2022;26:1–29.
- Vera-Lastra O, Ordinola Navarro A, Cruz Domiguez MP, et al. Two cases of graves’ disease following SARS-CoV-2 vaccination: An autoimmune/inflammatory syndrome induced by adjuvants. Thyroid. 2021;31(9):1436–1439.
- Zettinig G, Krebs M. Two further cases of graves’ disease following SARS-Cov-2 vaccination. J Endocrinol Invest 2022;45(1):227–228.
- Shroff H, Satapathy SK, Crawford JM, et al. Liver injury following SARS-CoV-2 vaccination: A multicenter case series. J Hepatol 2022;76(1):211–214.
- Zhao W, Chen W, Li J, et al. Status of humoral and cellular immune responses within 12 months following CoronaVac vaccination against COVID-19. mBio. 2022;13(3):e0018122.
- Dumortier J. Liver injury after mRNA-based SARS-CoV-2 vaccination in a liver transplant recipient. Clin Res Hepatol Gastroenterol. 2022;46(1):101743.
- Luo L, Aubrecht J, Li D, et al. Assessment of serum bile acid profiles as biomarkers of liver injury and liver disease in humans. PLoS One. 2018;13(3):e0193824.
- Zhou T, Fronhoffs F, Dold L, et al. New-onset autoimmune hepatitis following mRNA COVID-19 vaccination in a 36-year-old woman with primary sclerosing cholangitis - should we be more vigilant? J Hepatol 2022;76(1):218–220.
- Vuille-Lessard E, Montani M, Bosch J, et al. Autoimmune hepatitis triggered by SARS-CoV-2 vaccination. J Autoimmun 2021;123:102710.
- Zin Tun GS, Gleeson D, Al-Joudeh A, et al. Immune-mediated hepatitis with the moderna vaccine, no longer a coincidence but confirmed. J Hepatol 2022;76(3):747–749.
- Tan CK, Wong YJ, Wang LM, et al. Autoimmune hepatitis following COVID-19 vaccination: true causality or mere association? J Hepatol 2021;75(5):1250–1252.
- Rela M, Jothimani D, Vij M, et al. Auto-immune hepatitis following COVID vaccination. J Autoimmun 2021;123:102688.
- Palla P, Vergadis C, Sakellariou S, et al. Letter to the editor: autoimmune hepatitis after COVID-19 vaccination: A rare adverse effect? Hepatol. 2022;75(2):489–490.
- McShane C, Kiat C, Rigby J, et al. The mRNA COVID-19 vaccine - A rare trigger of autoimmune hepatitis? J Hepatol 2021;75(5):1252–1254.
- Londono MC, Gratacos-Gines J, Saez-Penataro J. Another case of autoimmune hepatitis after SARS-CoV-2 vaccination - still casualty? J Hepatol 2021;75(5):1248–1249.
- Liu J, Wang J, Xu J, et al. Comprehensive investigations revealed consistent pathophysiological alterations after vaccination with COVID-19 vaccines. Cell Discov. 2021 Oct 26;7(1):99.
- Liu Y, Sawalha AH, Lu Q. COVID-19 and autoimmune diseases. Curr Opin Rheumatol. 2021;33(2):155–162.
- Boettler T, Csernalabics B, Salie H, et al. SARS-CoV-2 vaccination can elicit a CD8 T-cell dominant hepatitis. J Hepatol. 2022;77(3):653–659.
- Adams DH, Hubscher SG. Systemic viral infections and collateral damage in the liver. Am J Pathol 2006;168(4):1057–1059.
- Mukhopadhyay L, Yadav PD, Gupta N, et al. Comparison of the immunogenicity & protective efficacy of various SARS-CoV-2 vaccine candidates in non-human primates. Indian J Med Res. 2021 Jan & Feb;153(1 & 2):93–114.