ABSTRACT
The Northern Finland Birth Cohort 1986 is a large population-based birth cohort, which aims to promote health and wellbeing of the population. In this paper, we systematically review the psychiatric research performed in the cohort until today, i.e. at the age of 32 years of the cohort (2018). We conducted a systematic literature search using the databases of PubMed and Scopus and complemented it with a manual search. We found a total of 94 articles, which were classified as examining ADHD, emotional and behavioural problems, psychosis risk or other studies relating to psychiatric subjects. The articles are mainly based on two large comprehensive follow-up studies of the cohort and several substudies. The studies have often used also nationwide register data. The studies have found several early predictors for the aforementioned psychiatric outcomes, such as problems at pregnancy and birth, family factors in childhood, physical inactivity and substance use in adolescence. There are also novel findings relating to brain imaging and cognition, for instance regarding familial risk of psychosis in relation to resting state functional MRI. The Northern Finland Birth Cohort 1986 has been utilised frequently in psychiatric research and future data collections are likely to lead to new scientifically important findings.
Abbreviations: attention deficit hyperactivity disorder (ADHD); magnetic resonance imaging (MRI)
Introduction
Birth cohort studies were originally designed to study early health outcomes, but already the earliest birth cohorts, started in the 1940s, have also studied later outcomes, including psychiatric problems and diagnoses. Birth cohort studies have been useful for instance when looking into early antecedents of childhood/adolescent [Citation1,Citation2] or adult psychiatric outcomes [Citation3,Citation4].
The Northern Finland Birth Cohorts (NFBC) 1966 and 1986 are two large population-based birth cohorts that aim to promote the health and wellbeing of the population. The NFBCs are among the oldest and most studied birth cohorts in the world and especially in the circumpolar region. The data have been collected since the antenatal period from health records, questionnaires and clinical examinations up to today. The older birth cohort, the NFBC1966, includes all people with an expected date of birth in 1966 in Northern Finland, whereas the younger birth cohort, the NFBC1986, includes those with an expected date of birth between 1 July 1985 and 30 June 1986. The two birth cohorts have been studied extensively with over 1,000 peer-reviewed publications in various fields of health sciences (http://www.oulu.fi/nfbc).
The focus in the NFBC1986 has been on children’s psychiatric health from the beginning. The studies have especially focused on attention deficit hyperactivity disorder (ADHD), emotional and behavioural problems and psychosis risk from childhood to adult age. In this paper, we systematically review the psychiatric research performed in the NFBC1986 until 2018, i.e. at the age of 32 years of the cohort.
Methods
Literature search
We conducted a systematic literature search using PubMed (Medline) and Scopus (Elsevier) databases in May 2018. The main search criteria were “Northern Finland Birth Cohort 1986” OR “Northern Finland Birth Cohort 1985–1986”. We also checked all publications of two authors who were involved in most of the early psychiatric studies of the cohort (“Northern Finland Birth Cohort” AND (“Moilanen I” OR “Taanila A”)). Additionally, we searched manually for articles from the extensive publication list maintained by the NFBC cohorts (http://www.oulu.fi/nfbc) and reviewed reference lists of the accepted articles from the literature search. Articles published after the systematic search were manually added to the review. Abstracts of the articles were checked by two authors and the final inclusion was done by consensus between the authors. The two inclusion criteria were that the study included data from the NFBC1986 and examined any psychiatric or psychological subject.
Sample
The NFBC1986 is based on 9,362 pregnant women and their 9,479 live-born babies in Northern Finland (former provinces of Oulu and Lapland), with an expected date of birth between 1 July 1985 and 30 June 1986. The live-births in this study represent 99% of all births in the region [Citation5]. The NFBC1986 is a genetically homogeneous population, including approximately 99.9% Caucasian people and 0.1% with Sami origin. The area is located between latitudes 65–70 degrees north. The overall study design has been approved and is under the review of the Ethical Committee of the Northern Ostrobothnia Hospital District, Finland.
The original articles of this literature review are largely based on two comprehensive data collections of the whole cohort, one in childhood (8 years) and one in adolescence (15–16 years), and on subsamples collected in childhood and early adulthood. Register data and earlier collected data of the NFBC1986 have also been utilised in the studies.
The 8 year follow-up was conducted in the spring of the children’s first school year (either 1993 or 1994), and the 15–16 year follow-up between April 2001 and February 2002. The former included questionnaires to parents and teachers and the latter to adolescents and their parents.
Other follow-ups including various questionnaires, interviews, cognitive tests and brain imaging have been performed for selected subsamples. Adolescents with ADHD symptoms and controls have been investigated at ages 16–18 years [Citation6] and 21–25 years [Citation7]. The Oulu Back Study, which also included psychiatric measures, was conducted when adolescents were 18 years old [Citation8]. Those with psychosis risk based on parental psychosis or prodromal symptoms at age 15–16 years were invited to the Oulu Brain and Mind Study I at age 21–25 years [Citation9]. At age 25–27 years, children who were born to mothers who were smoking during pregnancy and their controls were invited to the Oulu Brain and Mind Study II [Citation10]. There has also been a small sub-study for single-parent and reconstructed families, when children were 9 years old [Citation11].
Measures of psychiatric symptoms
The data collections with time points, sample sizes and used psychiatric measures are summarised in . Measures relating to ADHD, emotional and behavioural problems and psychosis risk and methods in cognition and brain imaging studies are presented briefly below.
ADHD symptoms
ADHD-related symptoms were measured with a teacher rated Rutter B2 (RB2) scale in childhood [Citation12], and with Strengths and Weaknesses of ADHD symptoms and Normal Behaviors (SWAN) questionnaire in adolescence and in early adulthood [Citation13]. The RB2 scale includes 26 items, 3 of which are considered to measure hyperactivity. The Rutter items were scored from 0 to 2 (0 = does not fit, 1 = fits partly, 2 = fits well). In the SWAN questionnaire parents rate their children into a 7-point statement scale for 18 items, of which nine measure inattentive and nine hyperactive-impulsive symptoms. Some studies have used the Youth Self-Report (YSR) subscale of attention problems [Citation14]. In the YSR questionnaire, adolescents rate themselves for how true (scale from 0–2) each item is now or was within the past six months. In addition, diagnostic interviews (Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version, K-SADS-PL [Citation15]) were conducted in the ADHD sub-study at age 16–18 years [Citation6].
Emotional and behavioural problems
Emotional (or internalising) and behavioural (or externalising) problems were measured in childhood with Rutter A2 (RA2) and RB2 scales, and in adolescence and early adulthood with the YSR [Citation16]. The NFBC studies used a modified parent rated RA2 scale with five emotional and four behavioural items. In the RB2 scale, there are four items measuring emotional problems and six behavioural problems. The version of the YSR questionnaire used included 30 items for emotional problems and 29 items for behavioural problems. These have been analysed continuously or using different cut-offs. Some studies also included register data, such as diagnoses of depression and criminal records.
Psychosis risk
Vulnerability to psychosis in the NFBC1986 was defined as having either prodromal symptoms or familial risk (FR) based on parental psychoses. The register-based information about the individual’s later-life psychosis was formed by utilising the Care Register for Health Care (previously known as the Finnish Hospital Discharge Register), Finnish outpatient registers, Finnish Centre for Pensions, and the registers of the National Social Insurance Institute [Citation17]. In adolescence, prodromal symptoms of psychosis were assessed using the PROD-screen (a screen for prodromal symptoms of psychosis), which has 21 items, of which 12 items specifically target psychotic-like experiences [Citation18]. In the Oulu Brain and Mind Study I, prodromal symptoms were also assessed using the Structured Interview for Prodromal Syndromes (SIPS) [Citation19]. Psychosis was also studied using register diagnoses and in sub-studies using interviews.
Cognition
Cognitive studies so far fare based on the ADHD sub-study and on the Oulu Brain and Mind Study I, which included subsamples for ADHD and psychosis risk research [Citation9]. The ADHD sub-study included the Wechsler Adult Intelligence Scale–Revised (WAIS–R) measuring working memory, the Conners’ Continuous Performance Test (CPT) measuring response inhibition and state regulation, and the Attention Network Task (ANT) measuring interference control [Citation20,Citation21]. Oulu Brain and Mind Study I included an extensive battery of cognitive tests, which have been studied separately, such as response initiation, vocabulary and matrix reasoning, or as one overall cognitive score [Citation10,Citation22–Citation24].
Neuroimaging
The neuroimaging studies reported so far are based on the Oulu Brain and Mind study I [Citation9], where participants underwent magnetic resonance imaging (MRI) scanning with the GE Signa 1.5 T scanner at Oulu University Hospital. Brain function was assessed with face-task blood oxygen level dependent (BOLD) functional MRI (fMRI) and resting state BOLD fMRI [Citation25,Citation26]. Grey-matter volume was assessed from T1-weighted structural scans. White-matter microstructure properties were assessed with diffusion tensor imaging (DTI) [Citation27]. The analyses of the neuroimaging data were carried out with FMRIB Software Library (FSL).
Results
Our systematic search found 314 articles in Scopus and 135 in PubMed. After removing duplicates, the number of articles was 341. We found 94 original articles related to psychiatry, of which 11 were found through the manual search. The included articles are listed in the Supplement , with references, sample sizes, a short summary of psychiatric methods used and comments. The main findings of these articles are summarised below in the following categories: ADHD, emotional and behavioural problems, psychosis risk and other studies.
Table 1. Statistically significant findings of risk factors for ADHD symptoms or diagnosis in the Northern Finland Birth Cohort 1986
ADHD
A total of 33 articles focused on ADHD, which was studied either by different ADHD symptoms in childhood or adolescence or by diagnosis assessed in the ADHD sub-study. At the age of 8 years, 9.5% of children had hyperactive problems assessed with the RB2 scale [Citation28]. At the age of 15–16 years, parents reported boys more often having problems than girls in the SWAN scale, but in the YSR attention scale, girls themselves reported as having more problems [Citation29]. Based on the SWAN screen and diagnostic interviews, the estimated prevalence of persistent ADHD diagnosis in childhood and adolescence was 6.7%, the prevalence of ADHD only in childhood was 12.6% and only in adolescence 8.5% [Citation6].
Risk factors for ADHD
presents the studied risk factors for ADHD. In many studies, maternal smoking has been associated with ADHD [Citation30–Citation32]. Also, other pregnancy related factors, such as maternal thyroid dysfunction [Citation33], prenatal exposure to synthetic glucocorticoids [Citation34], maternal adiposity prior to pregnancy [Citation35] and increased placental size [Citation36] have been associated with later ADHD symptoms.
Some studies have evaluated different developmental factors as risk factors for ADHD; intellectual disability of a child associated with hyperactivity problems in childhood [Citation28], and mixed-handedness has been associated with ADHD symptoms, both in childhood and adolescence [Citation37]. Executive functioning, state regulation and social risk factors have been associated with ADHD symptoms in adolescence [Citation21]. Scholastic impairment in childhood has been associated with comorbid diagnoses of behavioural problems and ADHD in adolescence [Citation38]. Also, major depression or oppositional defiant disorder by the age of 13 years, has been associated with persistent ADHD diagnosis in adolescence [Citation39].
The type of the family affected ADHD symptoms in adolescence, so that a divorced or reconstructed family increased the score of the ADHD scale among boys, and a reconstructed family increased reported YSR attention problems among boys and girls [Citation29]. Also having any hospital-treated injuries was associated with hyperactive symptoms in childhood and with ADHD symptoms and diagnosis in adolescence [Citation40]. In genetic studies, it has been found that the allelic variants of the dopamine β-hydroxylase gene are associated with ADHD symptoms in adolescence [Citation41].
Associating factors with ADHD
ADHD symptoms have also been linked to factors measured at the same time or at a later point in time. For example, childhood ADHD symptoms have been associated with scholastic impairment in reading, writing and mathematics [Citation42]. Also, childhood inattention-hyperactivity symptoms have been associated with adolescent obesity and physical inactivity [Citation43].
In adolescence, ADHD symptoms increased the frequency of the executive function deficits [Citation20] and were associated with various psychosocial well-being factors [Citation44]. Also, ADHD symptoms were associated with prodromal symptoms for psychosis in adolescence [Citation40] and affected substantially on crime [Citation45].
Diagnosis of ADHD in adolescence was associated with comorbidity with various psychiatric disorders and family environment related factors [Citation46], and increased suicidal ideation and deliberate self-harm [Citation47]. Comorbidity of ADHD and disruptive behavioural disorder were associated with more severe symptoms of conduct disorder [Citation48] and psychiatric hospitalisation [Citation49]. Young adults with past ADHD showed some differences in brain white matter [Citation50] and had structural and functional deficits in caudate associated with abnormal working memory function compared to healthy controls [Citation7].
Emotional and behavioural problems
There were a total of 38 published articles studying emotional and behavioural problems. Of the cohort members, 14.3% scored above the cut-off point for signs of probable psychiatric disturbance (i.e. having significant emotional and behavioural problems in the RB2 total scale) in childhood [Citation51]. Marked gender differences were found in emotional and behavioural problems in children and adolescents; the proportion of scoring above the cut-off point was higher for boys (19.8%) than for girls (8.7%). Behavioural problems (9.2%; boys 14.0% and girls 4.1%) were more common than emotional problems (4.1%; boys 4.3% and girls 3.9%) among children [Citation51]. In adolescence, girls had more emotional and behavioural problems than boys [Citation52]. Comparison between individuals of the NFBC1986 at the age of 15–16 years and Greek adolescents aged 18 years showed that Finnish boys scored lower than Greek boys on 10 of the 11 YSR subscales, especially in the anxious/depressed scale, and that Finnish girls scored higher than Greek girls on the somatic complaints and delinquent behaviour scales [Citation53].
Risk or associating factors for emotional problems in childhood and adolescence
presents the risk and associating factors for emotional and behavioural problems. Regarding emotional problems, female gender [Citation54], single-parent family [Citation51], problems in motor functions and learning difficulties [Citation55], multi-site musculoskeletal pain [Citation8] and physical inactivity [Citation56] were common factors associated with more severe emotional problems. In addition, use of cannabis and alcohol in adolescence in females predicted later inpatient hospital diagnoses of emotional disorders (e.g. depression), but similar results were not seen in males [Citation16]. One study found that prenatal glucocorticoid treatment did not predict emotional problems in childhood, but it was related to a total RB2 problem score [Citation34].
Table 2. Statistically significant findings of risk factors for emotional and behavioural problems in the Northern Finland Birth Cohort 1986
Risk or associating factors for behavioural problems in childhood and adolescence
Several factors have been examined in relation to behavioural problems among children and adolescents (see ). Risk factors associated with behavioural problems were prenatal (e.g. smoking/drinking while pregnant, low birth weight), family related (e.g. teenage mother, single parent) and environmental/socioeconomic factors (e.g. economic exclusion, material deprivation) [e.g. Citation57,Citation58]. Recently, several studies have looked accumulation of early risk factors to various outcomes in adolescence and adulthood, such as psychosocial problems [Citation57], school functioning [Citation59], substance use [Citation60,Citation61] and criminality [Citation62,Citation63]. As to the prenatal risk factors, the size of the placenta was associated with antisocial behaviour [Citation36]. Maternal smoking during pregnancy was related to behavioural problems both in childhood and in adolescence in both genders [Citation64]. The relationship between maternal smoking during pregnancy and pain in adolescence was mediated by childhood and adolescent behavioural problems [Citation64]. It has also been shown that female gender and paternal psychiatric hospitalisation are related to disruptive behaviour disorders without ADHD in adolescence [Citation49].
Some specific child characteristics were associated with behavioural problems: behavioural problems were more common among children with intellectual disability [Citation28] and also learning difficulties were associated with behavioural problems in childhood [Citation54]. Psychologically distant interaction with the father was associated with behavioural problems at school in a sub-study based on single parent and reconstructed families [Citation11].
Effects of emotional and behavioural problems on other factors
Emotional and behavioural problems have been reported to associate with multi-site musculoskeletal pains in adolescence [Citation65]. Behavioural problems in adolescence were also associated with low back pain [Citation66]. Furthermore, both genders with behavioural problems in adolescence were less likely to report high overall academic performance and plans of continuing into higher education [Citation67]. Conduct disorder symptoms and inattention-hyperactivity in childhood increased the risk for obesity and physical inactivity in adolescence [Citation43]. When emotional problems were considered as risk factors for different outcomes, children with emotional problems were more prone to withdrawal in adolescence [Citation68]. Each YSR subscale was strongly associated with concurrent self-reported life satisfaction in adolescence [Citation68]. In the adjusted models including substance use, family patterns, place of residence, family occupational level, parental alcohol use and parental psychiatric disorder, behavioural problems in childhood and adolescence predicted later violent crimes or offences against property in both males and females [Citation16]. Further, in general, behavioural problems in childhood, but not emotional problems, were associated with smoking, alcohol use, and the use of other substances in adolescence [Citation16]. NFBC1986 has also been a part of CARTA consortium; the consortium study found no causal association between smoking heaviness and depression or anxiety [Citation69].
Psychosis risk
In total, there were 27 studies on psychosis risk, most of these studies explored either prodromal symptoms or clinical risk (CR), some looked also psychotic diagnoses. There were 177 cases with known psychosis (based on registers) in the sample until age of 27 years, the cumulative incidence of all psychoses was 1.9% [Citation17].
Familial risk
Parental psychosis was a significant predictor of offspring’s psychosis [Citation17]. FR for psychosis has been investigated in relation to brain function and structure in eight previous studies. summarises group differences between FR participants and controls in the fMRI studies and one structural MRI study.
Figure 2. Summary of group differences between familial risk (FR) for psychosis and controls in functional and structural MRI studies in the Northern Finland Birth Cohort 1986. Blue represents decreased fMRI/MRI signal in FR (vs. controls) and red represents an increase in fMRI/MRI signal in FR (vs. controls)
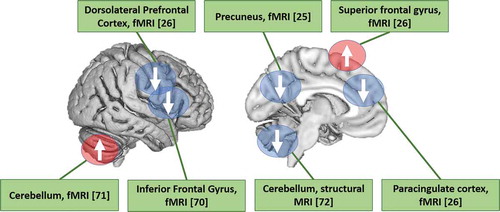
Three studies investigating FR participants and controls explored functional connectivity in different brain networks using resting state fMRI. The studies found that FR participants (vs. controls) demonstrated decreased default mode network activation [Citation23], lower central executive network activation [Citation70] and increased activation in the cerebellum [Citation71]. In a study of face-processing, fMRI activation to dynamic happy and fearful faces (relative to control stimulus) were compared between FR and controls [Citation26]. The authors found group differences in activation in the prefrontal cortex (PFC) and decreased connectivity between the amygdala and the PFC in the FR group (vs. controls).
Association between brain grey matter volume and psychosis risk was investigated using voxel-based morphometry in FSL to map regional grey-matter volumes in FR participants, CR participants that had prodromal syndrome according to the SIPS, participants with both FR and CR, and controls [Citation72]. Individuals with both FR and CR showed lower cerebellar grey-matter volume when compared to controls and no other group differences were found. In one recent study, it was found that the lowest connectivity in the face-processing network was observed in a group with high polygenic risk score for schizophrenia [Citation73].
Brain structure in FR individuals was also investigated using brain diffusion measures (DTI) in two studies. No differences were discovered in whole-brain central white matter regions in any DTI measures between FR participants and controls [Citation27]. Body mass index (BMI) associated with lower integrity of white matter in several brain areas, whereas an opposite pattern was detected in the control group [Citation74]. Furthermore, there was a group-by-BMI interaction (FR vs. controls) in the above white matter microstructural measures.
Somatic health and risk for psychosis
Besides the above reported findings on the effects of BMI, the associations of other physical measures, as well as different blood markers, with psychosis risk have also been studied in the NFBC1986. Physical inactivity in adolescence was shown to be associated with first-onset psychosis during a 4-year follow-up period after adjusting for several confounders [Citation75]. At the same age, no co-occurrence was reported for other cardiometabolic risk factors, including glucose and lipid metabolism, and first-onset psychosis [Citation76]. In addition, no association was found between cardiometabolic risk factors and FR [Citation77].
Levels of circulating inflammatory marker C-reactive protein (CRP) were associated with schizophrenia by the age of 27 years [Citation78]. Finally, parental somatic illness in childhood may also increase psychosis risk in the offspring. The effect was emphasised in the accumulation of illnesses, as well as in some specific diagnostic groups [Citation79].
Adolescence substance use and risk for psychosis
Adolescence substance use was studied in relation to prodromal symptoms and the incidence of psychosis in four studies [Citation80–Citation83]. The information on substance use was collected using postal questionnaires and during the cohort study in adolescence, whereas diagnoses of psychoses were based on register data.
Adolescents who had tried cannabis (5.6% of the sample) had higher scores of prodromal symptoms of psychosis compared to those who had not used cannabis. There was also a dose-dependent effect showing increase in prodromal symptoms as a function of cannabis use [Citation80]. In follow-up until the age of 30 years, the risk of psychosis was higher in individuals who had used cannabis in adolescence even when adjusted with prodromal symptoms, also with a dose-dependent effect showing an increased incidence of psychosis among those with the most frequent cannabis use [Citation81].
In addition to cannabis use, heavy smoking (i.e. 10 or more cigarettes a day) in adolescence was independently associated with an increased risk of psychosis by the age of 30 years also with a dose-dependent effect [Citation82]. During the same follow-up period, the use of inhalants was associated with incident psychosis even after controlling for baseline psychotic experiences and substance use, among others [Citation83].
Other studies in psychosis risk
Difficulty in making contact with others, as measured by sub-score of the PROD-screen in adolescence, was associated with an elevated risk of psychosis during the following years, but not with other psychiatric disorders [Citation84]. Neuropsychological functioning of individuals at CR and FR for psychosis was assessed in three studies in the Oulu Brain and Mind Study I. A study using 19 cognitive variables reported that individuals with psychosis performed worse in fine motor skills when compared with at-risk groups [Citation22]. In another study, the at-risk groups outperformed the psychosis group in semantic fluency response initiation [Citation23]. Neither of these studies found differences between the at-risk groups and controls. A study investigating cognitive performance and two candidate dopamine receptor D2 polymorphisms, namely rs6277 and rs1800497, found an association between poorer cognitive performance and minor allele rs1800497 in those at FR, but not in those at CR, suggesting different cognitive phenotypes in different risk groups for psychosis [Citation24]. The statistically significant risk factors for psychosis are summarised in .
Table 3. Statistically significant findings of risk factors for psychosis in the Northern Finland Birth Cohort 1986
Other work
The first psychiatric article in the NFBC1986 reported that 1.5% of the cohort members’ mothers used psychotropic drugs during pregnancy [Citation85]. Maternal advanced age, multiparity, overweight, smoking, alcohol use, and low social class increased and failure to ensure contraception decreased the regular use of psychotropic drugs during pregnancy.
Of the adolescents, about 30% reported loneliness [Citation86], which was associated with deliberate self-harm [Citation87] and a dislike of school [Citation88]. More girls (10%) than boys (7%) were alexithymic in adolescence. Mother’s low level of education, a broken childhood home, and living in a rural area were associated with higher alexithymia [Citation89]. In an fMRI study of subsample of 104 young adults, early traumas were associated with deviant brain response to fearful faces and weaker performance in fearful facial expression recognition [Citation90].
Discussion
Main results
So far there have been 94 studies on different psychiatric topics in the NFBC1986. The studies have identified associated factors, brain imaging findings and cognitive deficits in relation to ADHD, emotional and behavioural problems and psychosis risk. The studies have revealed several early risk factors for these mental health problems. For instance: maternal smoking during pregnancy has been linked with ADHD and behavioural problems; social problems with ADHD, emotional problems and psychosis risk; low physical activity and substance use with emotional and behavioural problems and psychosis risk; and single family with ADHD and emotional and behavioural problems. Several brain regions were associated with FR of psychosis in the NFBC1986. Specifically, the brain imaging data suggest that FR relates to alterations in the default mode network, central executive network, cerebellum and PFC.
Significance of the NFBC1986 findings
The early studies focused mainly on ADHD and other childhood mental health problems, but during recent years there has been an increase in studies, especially in psychosis risk research. The ADHD studies got a lot of attention as for instance the top journal in the field of child and adolescent psychiatry, the Journal of the American Academy of Child and Adolescent Psychiatry, published several NFBC1986 studies in a special issue in 2007.
There has been significant international collaboration in the NFBC1986, as two-thirds of the studies (63 out of 94) included international co-authors from, for instance, Imperial College London, University of Cambridge, University of California Los Angeles, and University of Michigan. NFBC1986 has been also part of the Nordic ADHD network [Citation30,Citation31,Citation35,Citation42]. The number of psychiatric studies in the NFBC1986 has increased rapidly during the last years, as 69 of 94 studies (73%) were published in 2010 or later. The current research is extremely active, as 21 studies were published 2017–2018.
Comparison to other birth cohort studies
There are several birth cohorts worldwide. The other birth cohorts in circumpolar region include e.g. the Finnish nationwide register-based birth cohorts (children born 1987 and 1997) [Citation91], the Uppsala Birth Cohort Multigeneration Study (UBCoS, 1915–1929) [Citation92], and the Norwegian Mother and Child Cohort Study (MoBa, 1999–2009) [Citation93]. The first aboriginal birth cohort has started in Canada with a focus on causes of fat gain [Citation94]; however there are no birth cohorts in the area yet focusing also on mental health issues. Future birth cohort studies in the north should also focus on mental health of indigenous population. So far, the only studies on mental health in these populations are from Australia [Citation95].
There have been several other birth cohorts, which have been investigating factors related to psychosis. A review of antecedents of schizophrenia in birth cohorts found 11 birth cohorts from 7 countries [Citation3]. The Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort is one of the largest of the younger birth cohorts (children born in the early 1990s). The studies in relation to psychosis and depression have been recently reviewed [Citation2].
Regarding cannabis use, smoking and the risk for psychosis, the NFBC1986 results are in line with the findings in the ALSPAC cohort, where they were associated with both depression and psychotic episodes [Citation2]. Interestingly, in the NFBC1986 the prevalence estimates are very high when compared to other samples, both in ADHD [Citation6] and in psychoses [Citation17]. The high prevalence estimates enable to investigate these disorders diversely in the NFBC1986.
When we compare the NFBC1986 with the older birth cohort NFBC1966, the younger cohort includes more high-quality registers and the childhood and adolescence follow-up include substantially more mental health related data than the older cohort. The older birth cohort has been studied especially for adult schizophrenia [Citation4], while the research in the younger birth cohort has been more varied.
Based on our experience on the birth cohorts, the future cohorts should start early, e.g. include information already on mental well-being of mothers during pregnancy and have large enough sample size with frequent follow-ups with good participation rates. These are not easily achieved goals; the challenges in general and especially in indigenous populations relate, e.g. to locating participants, to the maintenance between follow-up waves and to cross-cultural differences between the researchers and the cohort participants [Citation96].
Strengths and limitations
The strengths of birth cohort samples in general, and also of the NFBC1986, include the prospective design and large number of population-based age-matched comparison subjects for those with mental health problems. This design provides unique possibilities to analyse causal relationships, such as the effect of risk factors during pregnancy and delivery on later risk of illness; the studies have also collected a large number of potential covariates, which have been included in statistical models. Good participation rate, homogeneous population and possibility to utilise register data have been the major advantages to conduct birth cohort research in the Northern Finland. There have only been two large data collections in the NFBC1986. However, the participation in these two follow-ups has been very good, approximately 90% of teachers and 88% of parents participated when children were 8 years, and 76% of adolescents and 72% of parents when children were 15–16 years. When compared to other population-based studies, it can be noted that the NFBC1986 is genetically and culturally highly homogeneous. A major benefit in the NFBC1986 is also the possibility to utilise large nationwide health registers. Linking the cohort data to register data enables researchers to study various outcomes, such as hospital care, relatively easily and with low attrition. The NFBC1986 studies utilising cognitive and brain imaging data differ from most of the other studies on these topics, as in those studies cases are often collected from clinical samples and from one treatment setting, and controls are not included or are of strictly selected volunteers.
Conclusions
The studies in the NFBC1986 have found several early predictors for different psychiatric outcomes. There are also several interesting findings related to brain imaging and cognition. The next large follow-up of the NFBC1986 will begin in 2019. This follow-up will include some of the same topics as before, but also new instruments relating, for instance, to empathy, temperament, anxiety and depression. The current review can be used to learn about the work done in the NFBC1986 until today. The data is available for future research on request (see: http://www.oulu.fi/nfbc). The NFBC1986 has been utilised frequently in psychiatric research and future data collections are likely to lead to new scientifically important findings.
Supplemental Material
Download MS Word (50.1 KB)Acknowledgments
We would like to acknowledge all the participants in this study and the researchers who collected the data.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed here
Additional information
Funding
References
- Thompson L, Kemp J, Wilson P, et al. What have birth cohort studies asked about genetic, pre- and perinatal exposures and child and adolescent onset mental health outcomes? a systematic review. Eur Child Adolesc Psychiatry. 2010;19(1):1–14.
- Niarchou M, Zammit S, Lewis G. The Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort as a resource for studying psychopathology in childhood and adolescence: a summary of findings for depression and psychosis. Soc Psychiatry Psychiatr Epidemiol. 2015;50(7):1017–1027.
- Welham J, Isohanni M, Jones P, et al. The antecedents of schizophrenia: a revsiew of birth cohort studies. Schizophr Bull. 2009;35(3):603–623.
- Jääskeläinen E, Haapea M, Rautio N, et al. Twenty years of schizophrenia research in the Northern Finland Birth Cohort 1966: a systematic review. Schizophr Res Treatment. 2015;2015:524875.
- Järvelin MR, Hartikainen-Sorri AL, Rantakallio P. Labour induction policy in hospitals of different levels of specialisation. Br J Obstet Gynaecol. 1993;100(4):310–315.
- Smalley SL, McGough JJ, Moilanen IK, et al. Prevalence and psychiatric comorbidity of attention-deficit/hyperactivity disorder in an adolescent Finnish population. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1575–1583.
- Roman-Urrestarazu A, Lindholm P, Moilanen I, et al. Brain structural deficits and working memory fMRI dysfunction in young adults who were diagnosed with ADHD in adolescence. Eur Child Adolesc Psychiatry. 2016;25(5):529–538.
- Auvinen J, Eskola PJ, Ohtonen HR, et al. Long-term adolescent multi-site musculoskeletal pain is associated with psychological distress and anxiety. J Psychosom Res. 2017;93:28–32.
- Veijola J, Mäki P, Jääskeläinen E, et al. Young people at risk for psychosis: case finding and sample characteristics of the Oulu Brain and Mind Study. Early Interv Psychiatry. 2013;7(2):146–154.
- Ramsay H, Barnett JH, Murray GK, et al. Smoking in pregnancy, adolescent mental health and cognitive performance in young adult offspring: results from a matched sample within a Finnish cohort. BMC Psychiatry. 2016;16(1):430.
- Taanila A, Laitinen E, Moilanen I, et al. Effects of family interaction on the child’s behavior in single-parent or reconstructed families. Fam Process. 2002;41(4):693–708.
- Rutter M. A children’s behaviour questionnaire for completion by teachers. J Child Psychol Psychiatry. 1967;8:1–18.
- Swanson JM, Schuck S, Porter MM, et al. Categorical and dimensional definitions and evaluations of symptoms of ADHD: history of the SNAP and the SWAN rating scales. Int J Educ Psychol Assess. 2012;10(1):51–70.
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington (VT): University of Vermont, Research Center for Children, Youth & Families; 2001.
- Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988.
- Miettunen J, Murray GK, Jones PB, et al. Longitudinal associations between childhood and adulthood externalizing and internalizing psychopathology and adolescent substance use. Psychol Med. 2014;44(8):1727–1738.
- Filatova S, Marttila R, Koivumaa-Honkanen H, et al. A comparison of the cumulative incidence and early risk factors for psychotic disorder in young adults in the Northern Finland Birth Cohorts 1966 and 1986. Epidemiol Psychiatr Sci. 2017;26(3):314–324.
- Heinimaa M, Salokangas RK, Ristkari T, et al. PROD-screen - a screen for prodromal symptoms of psychosis. Int J Methods Psychiatr Res. 2003;12(2):92–104.
- McGlashan T, Miller TJ, Scott WW, et al. Structured interview for prodromal sydromes – version for present prodromal syndromes, Version 3.0, New Haven (CT): PRIME Research Clinic, Yale School of Medicine; 2001.
- Loo SK, Humphrey LA, Tapio T, et al. Executive functioning among Finnish adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1594–1604.
- Forssman L, Bohlin G, Lundervold AJ, et al. Independent contributions of cognitive functioning and social risk factors to symptoms of ADHD in two Nordic populations-based cohorts. Dev Neuropsychol. 2009;34(6):721–735.
- Mukkala S, Ilonen T, Nordström T, et al. Different vulnerability indicators for psychosis and their neuropsychological characteristics in the Northern Finland 1986 Birth Cohort. J Clin Exp Neuropsychol. 2011;33(4):385–394.
- Mukkala S, Ilonen T, Koskela J, et al. Response initiation in young adults at risk for psychosis in the Northern Finland 1986 Birth Cohort. Cogn Neuropsychiatry. 2014;19(3):226–240.
- Ramsay H, Barnett JH, Miettunen J, et al. Association between dopamine receptor D2 (DRD2) variations rs6277 and rs1800497 and cognitive performance according to risk type for psychosis: a nested case control study in a Finnish population sample. PLoS One. 2015;10(6):e0127602.
- Jukuri T, Kiviniemi V, Nikkinen J, et al. Default mode network in young people with familial risk for psychosis - the Oulu Brain and Mind study. Schizophr Res. 2013;143(2–3):239–245.
- Pulkkinen J, Nikkinen J, Kiviniemi V, et al. Functional mapping of dynamic happy and fearful facial expressions in young adults with familial risk for psychosis - Oulu Brain and Mind Study. Schizophr Res. 2015;164(1–3):242–249.
- Koivukangas J, Björnholm L, Tervonen O, et al. White matter structure in young adults with familial risk for psychosis - the Oulu Brain and mind study. Psychiatry Res. 2015;233(3):388–393.
- Taanila A, Ebeling H, Heikura U, et al. Behavioural problems of 8-year-old children with and without intellectual disability. J Pediatr Neurol. 2003;1:15–24.
- Hurtig T, Taanila A, Ebeling H, et al. Attention and behavioural problems of Finnish adolescents may be related to the family environment. Eur Child Adolesc Psychiatry. 2005;14(8):471–478.
- Obel C, Linnet KM, Henriksen TB, et al. Smoking during pregnancy and hyperactivity-inattention in the offspring - comparing results from three Nordic cohorts. Int J Epidemiol. 2009;38(3):698–705.
- Rodriguez A, Olsen J, Kotimaa AJ, et al. Is prenatal alcohol exposure related to inattention and hyperactivity symptoms in children? disentangling the effects of social adversity. J Child Psychol Psychiatry. 2009;50:1073–1083.
- Kotimaa AJ, Moilanen I, Taanila A, et al. Maternal smoking and hyperactivity in 8-year-old children. J Am Acad Child Adolesc Psychiatry. 2003;42(7):826–833.
- Päkkilä F, Männistö T, Pouta A, et al. The impact of gestational thyroid hormone concentrations on ADHD symptoms of the child. J Clin Endocrinol Metab. 2014;99(1):E1–8.
- Khalife N, Glover V, Taanila A, et al. Prenatal glucocorticoid treatment and later mental health in children and adolescents. PLoS One. 2013;8(11):e81394.
- Rodriguez A, Miettunen J, Brink Henriksen T, et al. Maternal adiposity prior to pregnancy is associated with ADHD symptoms in offspring: evidence from three prospective pregnancy cohorts. Int J Obes. 2008;32:550–557.
- Khalife N, Glover V, Hartikainen AL, et al. Placental size is associated with mental health in children and adolescents. PLoS One. 2012;7(7):e40534.
- Rodriguez A, Kaakinen M, Moilanen I, et al. Mixed-handedness is linked to mental health problems in children and adolescents. Pediatrics. 2010;125(2):e340–348.
- Nordström T, Hurtig T, Rodriguez A, et al. Different risk factors between disruptive behavior disorders and ADHD in Northern Finland Birth Cohort 1986. J Atten Disord. 2014;21(11):904–912.
- Hurtig T, Ebeling H, Taanila A, et al. ADHD symptoms and subtypes: relationship between childhood and adolescent symptoms. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1605–1613.
- Hurtig TM, Taanila A, Veijola J, et al. Associations between psychotic-like symptoms and inattention/hyperactivity symptoms. Soc Psychiatry Psychiatr Epidemiol. 2011;46(1):17–27.
- Nyman ES, Ogdie MN, Loukola A, et al. ADHD candidate gene study in a population-based birth cohort: association with DBH and DRD2. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1614–1621.
- Rodriguez A, Järvelin M-R, Obel C, et al. Do inattention and hyperactivity symptoms equal scholastic impairment? Evidence from three European cohorts. BMC Public Health. 2007;7:327.
- Khalife N, Kantomaa M, Glover V, et al. Childhood attention-deficit/hyperactivity disorder symptoms are risk factors for obesity and physical inactivity in adolescence. J Am Acad Child Adolesc Psychiatry. 2014;53(4):425–436.
- Taanila AM, Hurtig TM, Miettunen J, et al. Association between ADHD symptoms and adolescents’ psychosocial well-being: a study of the Northern Finland Birth Cohort 1986. Int J Circumpolar Health. 2009;68(2):133–144.
- Savolainen J, Hurtig T, Ebeling H, et al. Attention deficit hyperactivity disorder (ADHD) and criminal behaviour: the role of adolescent marginalization. Eur J Criminol. 2010;7(6):442–459.
- Hurtig T, Ebeling H, Taanila A, et al. ADHD and comorbid disorders in relation to family environment and symptom severity. Eur Child Adolesc Psychiatry. 2007;16(6):362–369.
- Hurtig T, Taanila A, Moilanen I, et al. Suicidal and self-harm behaviour associated with adolescent attention deficit hyperactivity disorder – a study in the Northern Finland Birth Cohort 1986. Nord J Psychiatry. 2012;66(5):320–328.
- Nordström T, Ebeling H, Hurtig T, et al. Comorbidity of disruptive behavioral disorders and attention-deficit hyperactivity disorder – indicator of severity in problematic behavior? Nord J Psychiatry. 2013;67(4):240–248.
- Nordström T, Hurtig T, Moilanen I, et al. Disruptive behaviour disorder with and without attention deficit hyperactivity disorder is a risk of psychiatric hospitalization. Acta Paediatr. 2013;102(11):1100–1103.
- Bode MK, Lindholm P, Kiviniemi V, et al. DTI abnormalities in adults with past history of attention deficit hyperactivity disorder: a tract-based spatial statistics study. Acta Radiol. 2015;56(8):990–996.
- Taanila A, Ebeling H, Kotimaa A, et al. Is a large family a protective factor against behavioural and emotional problems at the age of 8 years? Acta Paediatr. 2004;93(4):508–517.
- Heikkala E, Remes J, Paananen M, et al. Accumulation of lifestyle and psychosocial problems and persistence of adverse lifestyle over two-year follow-up among Finnish adolescents. BMC Public Health. 2014;14:542.
- Kapi A, Veltsista A, Sovio U, et al. Comparison of self-reported emotional and behavioural problems in adolescents from Greece and Finland. Acta Paediatr. 2007;96(8):1174–1179.
- Patwardhan I, Mason WA, Savolainen J, et al. Childhood cumulative contextual risk and depression diagnosis among young adults: the mediating roles of adolescent alcohol use and perceived social support. J Adolesc. 2017;60:16–26.
- Taanila A, Yliherva A, Kaakinen M, et al. An epidemiological study on Finnish school-aged children with learning difficulties and behavioural problems. Int J Circumpolar Health. 2011;70(1):59–71.
- Kantomaa MT, Tammelin TH, Ebeling HE, et al. Emotional and behavioral problems in relation to physical activity in youth. Med Sci Sports Exerc. 2008;40(10):1749–1756.
- Parra GR, Smith GL, Mason WA, et al. Tests of linear and nonlinear relations between cumulative contextual risk at birth and psychosocial problems during adolescence. J Adolesc. 2017;60:64–73.
- Loftipour S, Ferguson E, Leonard G, et al. Maternal cigarette smoking during pregnancy predicts drug use via externalizing behavior in two community-based samples of adolescents. Addiction. 2014;109:1718–1729.
- January SA, Mason WA, Savolainen J, et al. Longitudinal pathways from cumulative contextual risk at birth to school functioning in adolescence: analysis of mediation effects and gender moderation. J Youth Adolesc. 2017;46(1):180–196.
- Mason WA, January SA, Chmelka MB, et al. Cumulative contextual risk at birth in relation to adolescent substance use, conduct problems, and risky sex: general and specific predictive associations in a Finnish birth cohort. Addict Behav. 2016;58:161–166.
- Mason WA, Patwardhan I, Smith GL, et al. Cumulative contextual risk at birth and adolescent substance initiation: peer mediation tests. Drug Alcohol Depend. 2017;177:291–298.
- Savolainen J, Eisman A, Mason WA, et al. Socioeconomic disadvantage and psychological deficits: pathways from early cumulative risk to late-adolescent criminal conviction. J Adolesc. 2018;65:16–24.
- Solomon SJ, Savolainen J, Mason WA, et al. Does educational marginalization mediate the path from childhood cumulative risk to criminal offending? J Dev Life Course Criminol. 2017;3(3):326–346.
- Määttä AJ, Paananen M, Marttila R, et al. Maternal smoking during pregnancy is associated with offspring’s musculoskeletal pain in adolescence: structural equation modeling. Nicotine Tob Res. 2017;19(7):797–803.
- Paananen MV, Auvinen JP, Taimela SP, et al. Psychosocial, mechanical, and metabolic factors in adolescents’ musculoskeletal pain in multiple locations: a cross-sectional study. Eur J Pain. 2010;14(4):395–401.
- Mikkonen P, Heikkala E, Paananen M, et al. Accumulation of psychosocial and lifestyle factors and risk of low back pain in adolescence: a cohort study. Eur Spine J. 2016;25(2):635–642.
- Kantomaa MT, Tammelin TH, Demakakos P, et al. Physical activity, emotional and behavioural problems, maternal education and self-reported educational performance of adolescents. Health Educ Res. 2010;25(2):368–379.
- Honkanen M, Määttä H, Hurtig T, et al. Teachers’ assessments of children’s mental problems with respect to adolescents’ subsequent self-reported mental health. J Adolesc Health. 2014;54(1):81–87.
- Taylor AE, Fluharty ME, Bjørngaard JH, et al. Investigating the possible causal association of smoking with depression and anxiety using Mendelian randomisation meta-analysis: the CARTA consortium. BMJ Open. 2014;4(10):e006141.
- Jukuri T, Kiviniemi V, Nikkinen J, et al. Central executive network in young people with familial risk for psychosis - the Oulu Brain and Mind Study. Schizophr Res. 2015;161(2–3):177–183.
- Jukuri T, Kiviniemi V, Nikkinen J, et al. Cerebellar activity in young people with familial risk for psychosis - The Oulu Brain and Mind Study. Schizophr Res. 2015;169(1–3):46–53.
- Roman-Urrestarazu A, Murray GK, Barnes A, et al. Brain structure in different psychosis risk groups in the Northern Finland 1986 Birth Cohort. Schizophr Res. 2014;153(1–3):143–149.
- Lieslehto J, Kiviniemi VJ, Nordström T, et al. Polygenic risk score for schizophrenia and face-processing network in young adulthood. Schizophr Bull. 2018 Oct 3;1–11. DOI:10.1093/schbul/sby139.
- Koivukangas J, Björnholm L, Tervonen O, et al. Body mass index and brain white matter structure in young adults at risk for psychosis - The Oulu Brain and Mind Study. Psychiatry Res. 2016;254:169–176.
- Koivukangas J, Tammelin T, Kaakinen M, et al. Physical activity and fitness in adolescents at risk for psychosis within the Northern Finland 1986 Birth Cohort. Schizophr Res. 2010;116(2–3):152–158.
- Koponen H, Vuononvirta J, Mäki P, et al. No difference in insulin resistance and lipid levels between controls and adolescent subjects who later develop psychosis. Schizophr Res. 2008;104(1–3):31–35.
- Koponen H, Mäki P, Halonen H, et al. Insulin resistance and lipid levels in adolescents with familial risk for psychosis. Acta Psychiatr Scand. 2008;117(5):337–341.
- Metcalf SA, Jones PB, Nordstrom T, et al. Serum C-reactive protein in adolescence and risk of schizophrenia in adulthood: a prospective birth cohort study. Brain Behav Immun. 2017;59:253–259.
- Räsänen S, Niemelä M, Nordström T, et al. Parental hospital-treated somatic illnesses and psychosis of the offspring – the Northern Finland Birth Cohort 1986 study. Early Interv Psychiatry. 2017 Aug 25;1–7. DOI:10.1111/eip.12479.
- Miettunen J, Törmänen S, Murray GK, et al. Association of cannabis use with prodromal symptoms of psychosis in adolescence. Br J Psychiatry. 2008;192:470–471.
- Mustonen A, Niemelä S, Nordström T, et al. Adolescent cannabis use, baseline prodromal symptoms and the risk of psychosis. Br J Psychiatry. 2018;212(4):227–233.
- Mustonen A, Ahokas T, Nordström T, et al. Smokin` hot: adolescent smoking and the risk of psychosis. Acta Psychiatr Scand. 2018;138(1):5–14.
- Mustonen A, Niemelä S, McGrath JJ, et al. Adolescent inhalant use and psychosis risk – a prospective longitudinal study. Schizophr Res. 2018;201:360–366.
- Mäki P, Koskela S, Murray GK, et al. Difficulty in making contact with others and social withdrawal as early signs of psychosis in adolescents – the Northern Finland Birth Cohort 1986. Eur Psychiatry. 2014;29(6):345–351.
- Larivaara P, Hartikainen AL, Rantakallio P. Use of psychotropic drugs and pregnancy outcome. J Clin Epidemiol. 1996;49(11):1309–1313.
- Rönkä AR, Rautio A, Koiranen M, et al. Experience of loneliness among adolescent girls and boys: Northern Finland Birth Cohort 1986 study. J Youth Stud. 2014;17:183–203.
- Rönkä AR, Taanila A, Koiranen M, et al. Associations of deliberate self-harm with loneliness, self-rated health and life satisfaction in adolescence: Northern Finland Birth Cohort 1986 study. Int J Circumpolar Health. 2013;72:21085.
- Rönkä AR, Sunnari V, Rautio A, et al. Associations between school liking, loneliness and social relations among adolescents: Northern Finland Birth Cohort 1986 study. Int J Adolesc Youth. 2017;22:93–106.
- Joukamaa M, Taanila A, Miettunen J, et al. Epidemiology of alexithymia among adolescents. J Psychosom Res. 2007;63(4):373–376.
- Lieslehto J, Kiviniemi V, Mäki P, et al. Early adversity and brain response to faces in young adulthood. Hum Brain Mapp. 2017;38(9):4470–4478.
- Gyllenberg D, Marttila M, Sund R, et al. Temporal changes in the incidence of treated psychiatric and neurodevelopmental disorders during adolescence: an analysis of two national Finnish birth cohorts. Lancet Psychiatry. 2018;5:227–236.
- MacCabe JH, Koupil I, Leon DA. Lifetime reproductive output over two generations in patients with psychosis and their unaffected siblings: the Uppsala 1915–1929 Birth Cohort Multigenerational Study. Psychol Med. 2009 Oct;39(10):1667–1676.
- Magnus P, Birke C, Vejrup K, et al. Cohort profile update: the Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol. 2016 Apr;45(2):382–388.
- Wahi G, Wilson J, Miller R, et al. Aboriginal birth cohort (ABC): a prospective cohort study of early life determinants of adiposity and associated risk factors among aboriginal people in Canada. BMC Public Health. 2013;13:608.
- Jamieson LM, Paradies YC, Gunthorpe W, et al. Oral health and social and emotional well-being in a birth cohort of aboriginal Australian young adults. BMC Public Health. 2011;11:656.
- Lawrance M, Sayers SM, Singh GR. Challenges and strategies for cohort retention and data collection in an indigenous population: Australian aboriginal birth cohort. BMC Med Res Methodol. 2014;14:31.