ABSTRACT
Little is known about self-rated health (SRH) of older people living in more remote and Arctic areas. Iceland is a high-income country with one of the lowest rates of income inequality in the world, which may influence SRH. The research aim was to study factors affecting SRH, in such a population living in Northern Iceland. Stratified random sample according to the place of residency, age and gender was used and data collected via face-to-face interviews. Inclusion criteria included community-dwelling adults ≥65 years of age. Response rate was 57.9% (N = 175), average age 74.2 (sd 6.3) years, range 65–92 years and 57% were men. The average number of diagnosed diseases was 1.5 (sd 1.3) and prescribed medications 3.0 (sd 1.7). SRH ranged from 5 (excellent) to 1 (bad), with an average of 3.26 (sd 1.0) and no difference between the place of residency. Lower SRH was independently explained by depressed mood (OR = 0.88, 95% CI = 0.80–0.96), higher body mass index (OR = 0.93, 95% CI = 0.87–0.99), number of prescribed medications (OR = 0.88, 95% CI = 0.78–1.00) and perception of inadequate income (OR = 0.45, 95% CI = 0.21–0.98). The results highlight the importance of physical and mental health promotion for general health and for ageing in place and significance of economic factors as predictors of SRH.
Introduction
The world population is getting older [Citation1], which has prompted concerns regarding the achievability of “ageing in place”, defined as “the ability to live in one’s own home and community safely, independently, and comfortably, regardless of age, income, or ability level” [Citation2]. In Iceland, ageing in place is generally favoured by older adults and policymakers [Citation3]. The ability to age in place in rural areas in arctic and cold climate has been associated with self-rated health (SRH) [Citation4] and access to health care in the community [Citation4–Citation6]. Therefore, enhanced understanding of factors that may affect the general health status of older individuals living in the high north is particularly important to enable those who choose to age in place to do so. Moreover, rural and arctic areas deserve attention as they may lack some of the ideal neighbourhood characteristics for active ageing [Citation7] and ageing in place [Citation8], such as age-friendly outdoor spaces and buildings, transportation, appropriate housing, opportunities for social participation and health services.
Self-rated health is considered a measure of general health status and is often used as a predictive measure of health outcomes [Citation9,Citation10]. Several socio-economic factors (SES) such as educational level [Citation11], cohabitation, income level [Citation4,Citation11,Citation12], and place of residency affect SRH in older people [Citation13]. Jylhä [Citation14] suggests that physical, mental, social and contextual factors influence SRH assessments and proposed a conceptual model of issues affecting the persons’ cognitive processes when assessing SRH. Illuminating the multidimensionality of the SRH concept and that the context where persons are living affect their SRH.
Focusing on older adults in arctic and/or rural areas, researchers have identified a collection of factors that may affect self-ratings of health. Generally, SRH declines with age [Citation15] and more medical conditions [Citation16]. When comparing two geographically different regions we saw that older women in Alaska and the contiguous US reported less SRH than men [Citation12], while older men in Australia reported worse SRH compared to women [Citation15]. Older people with higher income and education reported better SRH in a representative-stratified sample (N=2815) of older people in both densely populated urban areas and sparsely populated rural areas in South Finland [Citation11]. Studies from Australia and Canada [Citation15,Citation16] found that each additional medical diagnosis doubles the odds of worse SRH. Moreover, indicators of cognitive decline [Citation15,Citation16] and depressive symptoms have been reported as negative predictors of SRH [Citation10,Citation12,Citation15].
Studies have demonstrated health inequities between urban and rural populations [Citation13,Citation17]. Monnat and Pickett [Citation18] claimed that differences in SES explain health disparities between rural-urban residencies. Individuals with low SES experience worse health because they are less likely to have the necessary resources to adopt protective health strategies [Citation18]. Inupiaq Villages of Alaska are reported to provide a positive environment for ageing well [Citation19]. Choi et al. [Citation20] conducted a study in rural Texas by randomly selecting places with less than 10,000 inhabitants (N=757 older people). They found that health disparities according to degree of rurality within rural areas varied. Better SRH was found in areas adjacent to metropolitan areas, which is supported by results of a population-based study in Iceland as well [Citation21]. In that study, SRH was assessed among 5801 Icelandic individuals aged 18 to 79 years, where 3006 lived outside the capital area (CA) and 2795 in the CA. Residents outside the CA rated their health worse than those living in the CA and those furthest away from the CA were most likely to rate their health as poor [Citation21].
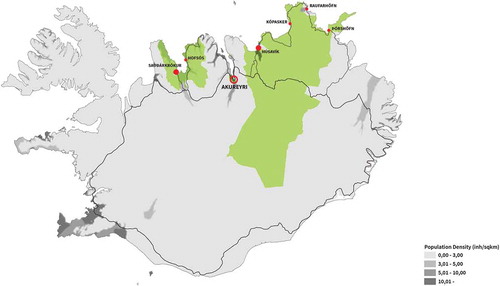
Iceland is a sparsely populated country where the CA is home to about two-thirds of the population and the remaining third lives mostly around the coastline; see . As in other Arctic countries, depopulation of rural municipalities, especially those furthest away from the CA, has occurred [Citation22]. This results in fewer people available for participation in social activities, local government and other services that municipalities provide. In the rural area furthest away from the CA, overall depopulation has been around 10–20% over the last 20 years [Citation22], and this area is included in our study. Moreover, a greater proportion of residents are ≥65 years in rural compared to urban areas in Iceland [Citation22]. According to population projections for the years 2016–2065, it is expected that in the year 2065, over 20% of all Icelanders will be ≥65 years, with the greatest increase in the oldest old group [Citation22].
Figure 1. The green areas represent the study´s rural areas, Akureyri the urban town is represented with the largest red circle. The bigger red points (Sauðárkrókur, Húsavík) represent the towns in both rural areas that were excluded from the study, the small red points represent the location of health clinics in rural areas. The grey colour indicates the population density with the darkest grey colour indicating the more dense areas
Iceland is an example of an ageing nation where the rural residents are facing challenges associated with ageing in arctic climate, and in areas with limited access to services that support their health and social participation. This study aims to examine factors potentially affecting SRH in two rural areas and an urban town in Northern Iceland. The chosen factors were those included in Jylhä’s [Citation14] model affecting SRH.
Materials and methods
Data were collected using a randomised cross-sectional, population-based design. Face-to-face interviews were conducted from September 2017 through January 2018.
Participants
The inclusion criteria were (a) being at least 65 years of age; (b) living in own home in the community; (c) capacity to communicate verbally; (d) competent to set up a time for a face-to-face interview. A stratified random sample from the national registry (N = 395) was taken. Postal codes were used to stratify, according to residency, age and gender. Of those, we could not reach 73 persons and 20 did not meet the inclusion criteria, because of cognitive impairment according to next of kin or that they had moved from the areas. That resulted in a total of 302 potential participants. At the time of random selection, the proportion of older men was 54.3% in the two rural areas and 46.0% in the urban town.
The geographical areas
Three distinct geographical areas were selected for the study, as they (a) represented parts of Iceland with understudied older populations; (b) fulfilled pre-determined definitions for urban/rural residency in Iceland [Citation23,Citation24]; (c) were located geographically close to the research base. The urban town (Akureyri) is the largest town in Iceland outside of the greater Reykjavik CA, with a university, secondary national hospital and diverse services. Although the population in the urban town is only around 19,000, it has a comprehensive urban infrastructure servicing the northern and eastern parts of Iceland, including cultural activities and strong presence of financial institutions. Of the urban inhabitants’ 14.6% were ≥65 years old. Inhabitants of the rural areas lived on farms, in other isolated houses or in small villages (≤200 inhabitants). Population of the two rural areas (see ) was approximately 4,000 and around 19% were ≥65 years. The urban town lies between the two rural areas and is separated geographically from them to the east and west by a fjord and a mountain range. Both rural areas have one town (not included in the study) with a primary health-care centre and a small basic hospital. Included in the rural area were small fishing villages, three in the east area and one in the west area, all had fewer than 200 inhabitants and a small primary health-care clinic that is open a few hours a week. Health care in Iceland is generally provided in health-care centres (national provided primary health care), where people can meet a health-care provider, such as a physician, a nurse, or a physiotherapist. The average travel distance to health-care services in the rural areas was over 20 km (12.5 miles), but the urban participants had to travel less than 5 km (3 miles) to access health care. In rural areas, the main roads are paved and kept open during the winter months. The smaller rural roads however are often not paved and are sometimes heavy with snow or ice during the winter months. In rural Iceland, public transportation is uncommon. A study on Northern Icelanders showed that 60% of 65–88 years old community-dwelling individuals drove their own car with the proportion lower for both women and participants over 75 years of age [Citation25].
Designing study and instruments
A multi-disciplinary team of nurses, a physiotherapist, an occupational therapist, a physiologist, a psychologist and a bio-statistician conducted the study. The study team developed the protocol and selected instruments suitable for the relevant population. The standardised instruments have been evaluated for psychometric properties in older people. Self-rated health (SRH) was measured by the question “How would you rate your health?“ Response options were “Excellent, very good, good, fair and bad” scored from 1 to 5, higher score indicated better SRH. The question is regarded as a robust measure of health status [Citation12]. The Geriatric Depression Scale (GDS) is based on 30 questions scored 0 or 1 points, the points are added together to give the final score [Citation26], with higher scores indicating more depression [Citation27]. Mini-Mental State Examination (MMSE) assesses cognitive function as attention, orientation, memory and calculation [Citation28]. Scores range from 0 to 30, higher scores indicate better cognitive function and a score of <24 indicates increasing cognitive impairment. The SF-36 is a general measure of health-related quality of life [Citation29], has eight subscales, four in the physical component summary (PCS) and four in the mental component summary (MCS). Pain was assessed by the Bodily Pain SF-36 subscale (BP SF-36). The raw scores of selected SF-36 scales were transformed to norm-based scaled scores which range from zero to 100, higher scores reflect a better physical and mental health, and less pain [Citation29]. SF-36 is widely used and amply validated [Citation29].
Participants also answered questions about educational level, adequacy of income, living alone or not, access to health care, frequency of eating fruits and vegetables, physical activity, frequency of meeting other people and self-reported diagnosed diseases. Measurements included were blood pressure (taken twice with the second blood pressure value used in our analysis), height, weight and current medication use. Body Mass Index (BMI) was calculated based on the height and weight as kg/m2.
Data collection
Each participant received a letter with information regarding the study 2 weeks prior to a telephone interview where she/he was asked to participate in the study. At that stage, they accepted or declined participation. If they accepted, a face-to-face interview was scheduled. The face-to-face mode of administration was selected to optimise the participation rate and accuracy of responses among participants with any fine motor, hearing, vision, or minor communicative problems. Four research assistants (third year nursing students) were specifically trained to conduct all telephone calls, face-to-face interviews and standardised measurements. Participants were offered to meet the research assistants at the research centre, the nearest health-care centre or in their own homes. All rural participants chose to meet research assistants in their own homes, but that varied in the urban town where interviews were both conducted in participants’ homes and at the research centre.
Statistical analysis
Descriptive statistics were used to summarise the characteristics of the participant's age, gender, cohabitation, educational level, BMI, blood pressure, adequate income to fulfill own needs, number of diagnosed diseases, number of prescribed drugs, frequency of eating fruit and vegetables, physical activity, frequency of meeting other people, and access to health care. Mean, standard deviation and ranges were used to describe continuous variables, counts and proportions were used for categorical variables. All descriptive variables were compared between residencies using t-tests for continuous variables and chi-square tests for categorical variables.
Ordinal logistic regression was used to evaluate the association between SRH as a three-level ordinal variable and the independent variables used in Jylhä’s [Citation14] model. Due to few participants reporting SRH as either “excellent” or “bad” (8 and 6 participants, respectively), the SRH was categorised into three levels, “excellent” and “very good” were combined into a single category, the response “good” was its own category and “fair” and ”bad” the third. The independent variables were cognitive function (MMSE), bodily sensation (BP SF-36, BMI, age, number of prescribed medications), mental sensation (GDS) and social-economic status (living alone or not, educational level, adequate income, urban/rural residency, access to health care). Multiple imputation by chained equations was used to handle missing data.
Ethical approval
The National Bioethics Committee (VSNb2016060007/03.01) approved the study and reported it to the Data Protection Authorities. Written informed consent was obtained from all participants.
Results
Participants
Out of 302 invited to participate, 175 (57.9%) agreed. People who declined to participate did not differ significantly from the study sample according to age (p = 0.77) and residency (p = 0.55). But, more women declined to participate compared to men (p = 0.01). The most common reason for declining was “too busy” and that the person felt that she/he had participated in many studies recently.
Characteristics of participants
Characteristics of the sample are shown in . The age range was from 65 to 92 years with 15 individuals, ≥85 years. Residents in the urban town had more years of education and more people had completed university degrees than in rural areas. People in rural areas used less prescribed medications compared to urban residents (). Of all participants, 46 (26.3%) said that they did not use any prescribed medications and 5 (2.8%) used ≥10 prescribed medications. On average, the sample reported 1.5 diagnosed diseases. Although the BMI was on average around 28 kg/m2, the range was from 19.2 to 56.3 kg/m2 and around 69% of the sample had BMI less than 30 kg/m2. Both mean values for Systolic and Diastolic Blood Pressures were in the range recommended [Citation30].
Table 1. Demographic characteristics of participants, number of diagnosed diseases and prescribed medications, body mass index (BMI), systolic and diastolic blood pressure and access to health care according to residency
Eating fruits or vegetables daily was reported by 70% of the sample and 38.9% reported to conduct physical activity 3 days or more per week, in a way that they perspired and were short of breath, with no significant difference between urban/rural residents. Urban people met (daily/weekly) their children or relatives more often than rural people (p = 0.02), but there was not a significant difference between urban/rural residents in how often they met their neighbours or friends or how often they talked with family or friends on the telephone or using the internet. Majority of the participants used some form of health-care service within the last 6 months, with an encounter with a physician (60%), a nurse (30%) a physiotherapist (26%) or an occupational therapist (2%), with no significant difference between the place of residency. Access to health care was rated as “good or rather good” by 83.4%. When the variable access to health care was divided into “good, rather good and neutral access” and “not good and bad access”, a chi-square test showed that people living in rural areas rated access to health care better compared to urban residents (p = 0.02).
Standardised measures
No difference was found between the place of residency in any of the measures based on standardised instruments, except for the sensation of pain (). The average score on the MMSE was around 27 (), 50 participants (28.6%) scored <27 and 19 (11%) <24. Increased age was correlated with lower MMSE (r = −.213, p=0.005), people with a university degree had higher MMSE scores compared to the other two educational groups (p=0.03).
Table 2. Scoring of self-rated health (SRH), the Mini-Mental State Examination (MMSE), the Geriatric Depression Scale (GDS) and three scales from the SF-36
Self-rated health
Scores of SRH were similar for rural and urban older people (). Eight people (4.6%) rated their health as excellent, 35 (20%) as very good, 84 (48%) as good, 42 (24%) as fair and 6 rated their health as bad (3.4%). Gender, educational level, place of residency, cohabiting or not, BMI ≤30 or >30 and access to health care were not significantly related to SRH. Participants who reported to have adequate income had higher SRH scores than those who reported not to have adequate income (p = 0.001). Level of SRH decreased with increased age (p = 0.007). People that scored 24–30 on the MMSE, compared to 19–23, had better self-rated health (p < 0.001). Those that rated their SRH as fair or bad were less physically active compared to people with, good, very good and excellent SRH (p = 0.02).
An ordinal logistic regression model with SHR as the outcome revealed that a lower BMI, fewer GDS points, less use of medications and having adequate income increased the odds of better SRH. Having adequate income more than doubled the odds of having better SRH. All odds-ratios and associated confidence intervals are presented in . Lower age showed a trend to increase SRH.
Table 3. Independent association between eleven explanatory factors and the odds of higher ratings of health (SRH)a, based on logistic regression analysis
Discussion
This study contributes significantly to the spare literature on ageing in rural Arctic areas. We found that community-dwelling older people rated their health as good with little differences between the place of residency. As other studies report [Citation16] both physical, mental and socio-economic factors affected SRH. Here, adequate income more than doubled the odds of having better SRH, highlighting the importance of economic factors as predictors of SRH. Cohen et al. [Citation12] claim that rural older community-dwelling adults in US report generally lower SRH. However, if the county is a high-income county, urban older people rate their health worse. Iceland is a high-income country with the seventh highest GDP per capita in the world [Citation31] and has one of the lowest rates of income and health-related inequality in the world based on the United Nations Development Program [Citation32]. That may explain the lack of urban vs rural difference in SRH and illuminates the importance of socio-economic factors for SRH.
Our study supports the robust results [Citation4,Citation15] that depression increases the likelihood of worse SRH. Jylhä [Citation14] suggests that assessment of SRH is more influenced by mental health in older people than other indicators of health. Here, increased cognitive impairment or lower scoring of MMSE with age was associated with greater depression but did not increase the likelihood of poorer SRH. Depressive symptoms are common in Iceland and most common among people with low income [Citation33]. It is estimated that direct and indirect cost related to mental health problems is around 4.9% of Iceland´s GDP [Citation34], suggesting an area for improvement for policymakers for the future. Use of less prescribed medications increased SRH and rural participants used less medications although found to have more pain, which is confirmed in other studies [Citation35].
SRH declined with age, as is found in other studies [Citation15]. The average rating of SRH was 3.26 for all participants which is comparable to 3.15 (±0.96) (scale 1–5) that Choi et al. [Citation20] report. Most rated their health as good (48%) and around 25% as excellent or very good. This is slightly higher than a previous study among older Icelandic people found, where 18% rate their health as excellent or very good [Citation4]. In a US-based study [Citation36], 46% of 4411 older people assessed their SRH as excellent or very good. Wilson et al. [Citation37] report that 63.3% of 578 older people in England rate their health in the top two categories. In the third category, they use the word “fair” where we and the other aforementioned studies use “good” which might explain the difference.
When the variable access to health care was dichotomised, rural people reported better access compared to urban people. The explanation could be that geographical distance to a health-care centre is generally less than an hour drive, making the geographical distance to health-care centres less of a barrier. In the small health clinics, health-care practitioners work on a regular basis and might know their clients personally, as previous Icelandic study report [Citation5]. In the urban town, there has been a shortage of physicians in primary health care and long waiting periods for an appointment. Similar findings are reported from Alaska where rural people were less likely to miss their annual medical check-up, although older people in Alaska were generally more likely to miss their annual medical check-up compared to older people in the lower 48 states of the US [Citation12]. In addition, Iceland was ranked as number two out of 195 countries based on health-care access and quality index based on mortality from causes amenable to personal health [Citation38]. However, in Iceland, there is an uneven distribution of health-care professionals and most specialists’ services are conducted in the CA [Citation3]. It is reported that among all Icelanders some cannot afford health-care services, with little or no urban to rural difference [Citation39]. Moreover, the country is sparsely populated, especially in the rural areas we are studying (), which we would expect to hamper health-care access.
Limitations and strengths
The self-selection of people’s residency prohibits any causal conclusions to be drawn from the results presented. The relatively small sample limits how many variables could be included into the regression model. However, the sample size is reasonable compared to the population studied. The sample is drawn from relatively large understudied areas, some of the most remote areas in Iceland. The strengths of the study are that it used a random sample that should well represent the areas studied. However, some declined to participate due to limited time and we can expect that more frail or disabled people are more likely to decline to participate.
Conclusions
The study contributes to knowledge of the health of older community-dwelling people living in Arctic areas in Northern Iceland; a sample that is not well studied, and like other Arctic areas often ignored from studies. Although participants generally rated their health status as rather good, they represent a population which is likely to experience declining health and may, therefore, be particularly vulnerable to negative effects of climate changes. Yet, the relatively high SRH of the sample may reflect a resilient population with the capacity needed to age in place. The study highlights the importance of promotion of physical and mental health as well as small health-care centres in rural areas. It stresses the importance of the distribution of health-care services in rural and remote areas to increase the accessibility of services for vulnerable groups such as older people. Knowledge of SRH and its explanatory factors should be used for further research on ageing in place including focus on social participation, social support and access to health care. This knowledge should also be considered by health policymakers to enable older people who want to age in place to do so.
Acknowledgements
The authors thank all the study participants and the research assistants performed data collection.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Beard JR, Officer A, de Carvalho IA, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–2154. doi:10.1016/S0140-6736(15)00516-4.
- Centers for Disease Control and Prevention [CDC]. 2014. Healthy places terminology. [cited 2019 Oct 17]. Available from: https://www.cdc.gov/healthyplaces/terminology.htm
- Sigurgeirsdottir S, Waagfjord J, Maresso A. Iceland: health system review. Health Syst Transit. 2014;16:1–8.
- Arnadottir SA, Gunnarsdottir ED, Stenlund H, et al. Determinants of self-rated health in old age: a population-based, cross-sectional study using the international classification of functioning. BMC Public Health. 2011;11(1):670.
- Gustafsdottir SS, Fenger K, Halldorsdottir S, et al. Social justice access and quality of healthcare in an age of austerity users perspective from rural Iceland. Int J Circumpolar Health. 2017;76:1347476.
- Huot S, Ho H, Ko A, et al. Identifying barriers to healthcare delivery and access in the Circumpolar North: important insights for health professionals. Int J Circumpolar Health. 2019;78:1571385.
- World Health Organization. Global age-friendly cities: a guide. Geneva: World Health Organization; 2007. Available from: https://www.who.int/ageing/publications/Global_age_friendly_cities_Guide_English.pdf
- Cramm JM, Van Dijk HM, Nieboer AP. The creation of age-friendly environments is especially important to frail older people. Ageing Soc. 2018;38:700–720.
- Chireh B, D’Arcy C. Pain and self-rated health among middle-aged and older Canadians: an analysis of the Canadian community health survey-healthy aging. BMC Public Health. 2018;18:1006–1011.
- Rohrer JE, Arif A, Denison MS, et al. Overall self-rated health as an outcome indicator in primary care. J Eval Clin Pract. 2007;13:882–888.
- Nummela OP, Sulander TT, Heinonen HS, et al. Self-rated health and indicators of SES among the ageing in three types of communities. Scand J Public Health. 2007;35:39–47.
- Cohen SA, Talamas AX, Sabik N. Disparities in social determinants of health outcomes and behaviours between older adults in Alaska and the contiguous US evidence from a national survey. Int J Circumpolar Health. 2018;78:1–7.
- Cohen SA, Cook SK, Sando TA, et al. What aspects of rural life contribute to rural‐urban health disparities in older adults? Evidence from a national survey. J Rural Health. 2018;34:293–303.
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316.
- French DJ, Sargent-Cox K, Luszcz MA. Correlates of subjective health across the aging lifespan. J Aging Health. 2012;24:1449–1469.
- Meng X, D’Arcy C. Determinants of self-rated health among Canadian seniors over time: a longitudinal population-based study. Soc Indic Res. 2016;126:1343–1353.
- Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37:455–463.
- Monnat SM, Pickett BC. Rural/urban differences in self-rated health: examining the roles of county size and metropolitan adjacency. Health Place. 2011;17:311–319.
- Smith J, Easton PS, Saylor BL. Inupiaq elders study: aspects of aging among male and female elders. Int J Circumpolar Health. 2009;68:182–196.
- Choi JY, Reiter EM, Theodori GL. The impact of rurality community attachment and community involvement on health among rural Texans. J Rural Soc Sci. 2015;30(1):1–24.
- Haraldsdóttir S, Gudmundsson S. Poorer self-rated health in residential areas with limited healthcare supply. Scand J Public Health. 2014;42:310–318.
- Statistics Iceland. [cited 2019 May 31]. Available from: https://statice.is/statistics/population/inhabitants/
- OECD. Definition of Functional Urban Areas (FUA) for the OECD metropolitan database 2013. Available from: https://www.oecd.org/cfe/regional-policy/Definition-of-Functional-Urban-Areas-for-the-OECD-metropolitan-database.pdf.
- Marshall JU. The structure of urban systems. Toronto: University of Toronto Press; 1989.
- Arnadottir SA, Gunnarsdottir ED, Stenlund H, et al. Participation frequency and perceived participation restrictions at older age: applying the International Classification of Functioning, Disability and Health (ICF) framework. Disabil Rehabil. 2011;33:2208–2216.
- Yesavage J, Brink TL, Rose TL, et al. Development and validation of a Geriatric Depression Screening Scale: a preliminary report. J Psychiatr Res. 1983;17:37–49.
- Valdimarsdóttir M, Jónsson JE, Einarsdóttir S, et al. Validation of an Icelandic version of the Geriatric Depression Scale (GDS). (Mat á þunglyndi aldraðra: Þunglyndismat fyrir aldraða – íslensk gerð Geriatric Depression Scale (GDS). Icelandic Med J. 2000;86:344–348.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psych Res. 1975;12:89–98.
- Ware JE. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25:3130–3139.
- American Diabetes Association. 9. Cardiovascular disease and risk management: standards of medical care in diabetes—2018. Diabetes Care. 2018;41:S8–S104.
- OECD Data. OECD (2019), Gross domestic product (GDP) (indicator); 2019. [cited 2019 May 31. Available from: https://data.oecd.org/gdp/gross-domestic-product-gdp.htm. OECD, Gross domestic product (GDP) (indicator). doi: 10.1787/dc2f7aec-en.
- Murray C, Lim SS. Measuring the health-related sustainable developmental goals in 188 counties: a baseline analysis from the global burden of disease study 2015. Lancet. 2016;388:1813–1850.
- Statistics Iceland. [cited 2019 May 31]. Available from: https://px.hagstofa.is/pxen/pxweb/en/Samfelag/Samfelag__heilbrigdismal__heilsufarsrannsokn__heilsufar/HER02210.px/table/tableViewLayout1/?rxid=c414dcad-78ff-4e66-bcce-f3cc21dcd95e
- OECD/EU. Health at a glance. Europe 2018. State of health in the EU cycle. Paris: OECD Publishing; 2018.
- Sigurdardottir AK, Arnadottir SA, Gunnarsdottir ED Socioeconomic status and differences in medication use among older people according to ATC categories and urban–rural residency. Scand J Public Health. 2013;41:311–317.
- Willa DB, Hubbard RA, Crane PK, et al. Longitudinal associations between self-rated health and performance-based physical function in a population-based cohort of older adults. PLoS One. 2014;9:e111761.
- Wilson JJ, Blackburn NE, O’Reilly R, et al. Association of objective sedentary behaviour and self-rated health in English older adults. BMC Res Notes. 2019;12:1–6.
- Barber RM, Fullman N, Sorensen RJD, et al. Health care access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: a novel analysis from the global burden of disease study 2015. Lancet. 2017;390:231.
- Statistics Iceland. [cited 2019 May 31]. Available from: https://px.hagstofa.is/pxen/pxweb/en/Samfelag/Samfelag__heilbrigdismal__heilsufarsrannsokn__heilbrigdisthjonusta/HER03001.px/table/tableViewLayout1/?rxid=0e5a0bf6-52f5-44cf-a647-f95fffdabc2a
