?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
The aim of this study was to investigate whether participation in Family Wellness Warriors Initiative (FWWI), an Alaska Native program that addresses adverse life experiences, is associated with changes in health care utilisation. The study method was a propensity score-matched cohort analysis using retrospective electronic health record data from Southcentral Foundation, a tribal health care system, from 2012 to 2017. Ninety p\articipants in FWWI trainings were identified as the intervention cohort and were propensity matched with 90 people who participated in other emotional wellness-related interventions. The primary outcome was the number of total health system visits. Secondary outcomes included emergency department (ED) visits, substance-use visits and visits with somatisation potential. After adjustment for covariates, FWWI participants showed a 36% reduction in total system visits (incidence rate ratio 0.64, 95% CI 0.49–0.84) and a 70% reduction in substance use visits (incidence rate ratio 0.30, 95% CI 0.10–0.93) when compared to the control. FWWI participants showed a 40% reduction in ED visits (incidence rate ratio 0.60, 95%CI 0.35–1.02) when compared to the control that was borderline significant. No significant differences were found for visits with somatisation potential (incidence rate ratio 1.25, 95% CI 0.79–1.99).
Introduction
Adverse childhood experiences are associated with many negative adult health and health care utilisation outcomes, including cardiovascular illness, depression, suicide attempts, unhealthy substance use, obesity, lung disease, liver disease, cancer and medically unexplained symptoms such as pain or gastrointestinal problems[Citation1–Citation6]. Adverse experiences in adulthood can also negatively affect physical and mental health, and the effect of traumatic events throughout the lifetime can be cumulative and substantial [Citation7–Citation9]. For the purposes of this study, we will focus on adverse life experiences (ALEs), which can occur at any age. The population-level health burden of ALEs may be especially high in tribal communities, as Alaska Native and American Indian (ANAI) peoples have higher rates of adverse experiences than the general population, and have survived many traumas in recent history: epidemics, displacement from their traditional territories, punishment for speaking language or practicing culture, and family separation through forced attendance at boarding school [Citation10–Citation14]. Evidence indicates that health disparities can be driven by certain groups’ increased exposure to ALEs [Citation8,Citation9,Citation15].
An unanswered question is whether treating ALEs in adults can reverse the known negative health outcomes. Recommended treatments for ALEs are generally trauma-focused psychotherapies that reduce PTSD symptomology, improve self-esteem and build healthy emotional responses and interpersonal skills [Citation16–Citation19]. As these treatments target multiple mechanisms thought to drive ALE-related negative health outcomes-such as emotional distress, chronic stress, disrupted emotional awareness, limited interpersonal connections, and reduced self-efficacy-it is plausible that they may improve health outcomes[Citation3, Citation20–Citation25]. This possibility has not received much research attention: most studies of trauma-focused psychotherapies have focused on behavioural health outcomes such as PTSD symptomology, depression or anxiety [Citation26,Citation27].
In this study, we investigate whether an Alaska Native program to treat the emotional and interpersonal effects of ALEs can influence health care utilisation. Our primary outcome was total health system visits. Our secondary outcomes were substance use visits, emergency department visits and visits with somatisation potential. To our knowledge, this is the first propensity-matched study on the health care utilisation effects of treating ALEs. Additionally, as eliminating health disparities is a major national goal, and many groups experiencing health disparities have higher rates of ALEs, our study, conducted by a tribal organisation, could inform new approaches to addressing health disparities [Citation28].
Methods
Study type
A propensity score-matched cohort analysis using retrospective electronic health record data.
Setting and intervention
Southcentral Foundation (SCF) is a non-profit tribal health care organisation that is created, managed and owned by Alaska Native people. SCF serves over 65,000 Alaska Native and American Indian people and provides medical, behavioural, dental, traditional and residential services. SCF’s approach to health care is relationship-based and holistic.27 As a closed and comprehensive health care system, SCF offers a unique opportunity to investigate the physical health effects of programmes for emotional wellbeing.
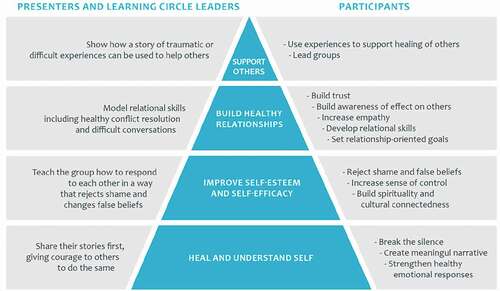
SCF’s Family Wellness Warriors Initiative (FWWI) trainings address ALEs as the root cause of family violence. FWWI provides intensive 5-day trainings which are grounded in Alaska Native values and methodologies and based on the theory that healing from ALEs is an essential step that must occur in order for participants to build resilience, self-efficacy and healthy relationships (). To heal ALEs, participants and peer leaders use storytelling to break the silence about harms experienced and to make sense of traumatic experiences, support each other, develop positive self-narratives and find commonalities with others. Participants work in peer-led groups to build self-esteem, develop relational skills and set positive goals for the future (). For a more detailed description of the FWWI program, see [Citation29] or [Citation19].
Treatment group
FWWI is a community program that advertises through diverse methods (ranging from fliers in public spaces to provider referrals) to potential participants in Anchorage and rural Alaska and does not require any kind of health care referral. To qualify for this study, participants needed to have completed an FWWI training between 10/1/2012 and 11/06/2016 and to have been empanelled in the SCF health care system at least 6 months before the training date. This resulted in 90 records. FWWI participants reported an average of 4.5 ALEs as measured by the Alaska screening tool [Citation30].
Comparison group
Comparison group participants needed to enrol in a non-FWWI emotional wellness-related intervention at SCF after 1 October 2012 and before 1 June 2016, and to have been empanelled as an SCF customer-owner for 6 months prior to the training. This resulted in 2273 cohort members, of which 90 were successfully matched to the treatment group. Matched comparison group participants reported an average of 4.6 adverse experiences as measured by the Alaska screening tool [Citation30]. Comparison group interventions were all behavioural health programs that required a health care referral, such as counselling or group therapy.
Health care utilisation time period
Several types of utilisation in the 6-month pre-period were measured in order to control for them as covariates. Four types of utilisation in the 6-month post-period, which occurred after a 3-month post-training transition period, were measured as outcomes.
Data sources
Training participation and Alaska screening tool information were pulled for FWWI participants from the FWWI program’s SQL server database. For the comparison group, intervention participation information and Alaska screening tool information were pulled from SCF electronic health records. For both groups, information about system utilisation and relevant diagnoses were pulled from both the Cerner and Tier electronic health records using a data abstraction tool designed by the study team.
Outcomes measurement
In collaboration with subject-matter expert team members (FWWI director, staff and participants; a psychiatrist; primary care providers; behavioural health providers), the following measurement definitions were adopted:
Primary outcome
Total system visits
All visits in the SCF system.
Secondary outcomes
Substance use visits
Visits at any SCF location with a diagnosis on the NYU ED algorithm drug and alcohol diagnosis list [Citation31].
Somatic visits
Visits at any SCF location on the somatisation potential list from Smith and colleagues: ill-defined symptoms and disorders in the musculoskeletal, nervous or gastrointestinal systems [Citation32].
Emergency department (ED) visits
Visits which had the location coded as the emergency department.
All diagnosis-based measurements of outcomes and covariates used taxonomies that incorporated both ICD-9 CM and ICD-10 CM codes.
Covariate measurement
Important covariates hypothesised to influence the selected outcomes were determined using stakeholder input.
Demographic measures of age, sex, marital status and Medicaid eligibility
Visit counts by location type, including total visit counts, primary care visit counts, urgent care visit counts, ED visit counts, speciality visit counts and inpatient visit counts;
Visits with an ICD self-inflicted injury code [Citation33]
Visits with a diagnosis on the HCUP chronic condition classifier list [Citation34]
Presence on chronic condition action lists
Number of behavioural health diagnoses [Citation35]
Charlson co-morbidity scores were calculated using 1) The Quan coding algorithm for pulling relevant diagnostic codes [Citation36] and 2) the original Charlson weights for weighing listed conditions. Look-back period was 1 year.
Alaska screening tool survey data included number of lifetime adverse experiences, anxiety and substance use [Citation30].
Statistical analysis
Propensity model
We used propensity matching to ensure the treatment and comparison groups were balanced on key covariates [Citation37]. Per [Citation38], we focused on covariates that were known by stakeholders or in the literature to influence the outcomes of interest, including demographics, Charlson score, behavioural health diagnoses and screenings and prior health care utilisation [Citation38].
Building the propensity model
The MatchIt R package was used to perform the propensity matching in R 3.3.2 [Citation39]. The logit option was used to build a logistic regression model, and the optimal matching option was used. Optimal matching minimises the average absolute distance across all matched pairs and matches without replacement [Citation39]. A 1 to 1 match was used because it resulted in the most balanced mean covariate values for the two groups. Evidence indicates 1 to 1 matching reduces bias in the estimate of treatment effect when compared to 1 to many matching [Citation40].
Evaluating balance
As recommended by Ho et al. [Citation41], we used standardised differences to evaluate the balance of the matched pairs across the means of the covariates [Citation41]. The standardised difference, which compares the mean of the treatment group with the mean of the comparison group, while adjusting for variability,, was calculated for each covariate.
Outcomes modelling
GEE-based negative binomial regression, with exchangeable correlation structure and empirical standard error estimates, was used to build a model for each outcome in SAS 9.2. The GEE approach accounted for the correlation between matched pairs [Citation42]. A negative binomial mean model was chosen because it handles over-dispersed count data [Citation43]. A separate model was built to predict each type of health care utilisation in the post-period. All models controlled for age, sex, Charlson score, Medicaid eligibility, count of behavioural health diagnoses, number of action lists a person qualified for, number of endorsed adverse experiences, and anxiety, trauma symptomology, and depression scores. Each model controlled for number of pre-visits of the same type as the predicted outcome. We chose to use a double-adjustment method, which follows propensity-matching with a regression model that controls for covariates, because this is recommended when there are covariates with a standardised difference greater than 10% after propensity matching and has been shown to dramatically reduce residual confounding bias [Citation44].
Results
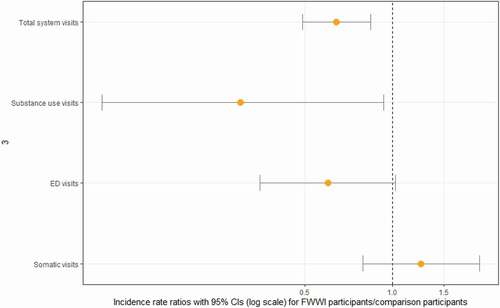
and show that when compared with the control group, FWWI participants had significantly lower post-training incidence rate ratios (predicted FWWI visits in 6 months/predicted comparison group visits in 6 months) for total system visits and substance use visits. The post-training incidence rate ratio for total system visits was 0.64 (95% CI 0.49–0.84), which is the equivalent of 36% fewer total system visits among FWWI participants when compared to control participants. The post-training incidence rate ratio for substance use visits was 0.30 (95% CI 0.10–0.93), which is the equivalent of 70% fewer substance use visits among FWWI participants when compared to control participants. FWWI participants had a lower post-training incidence rate ratio for ED visits when compared to the control group that was almost significant. The post-training incidence rate ratio for ED visits was 0.60 (95% CI 0.35–1.02), which is the equivalent of 40% fewer ED visits among the FWWI participants when compared to the control participants. The post-training incidence rate ratio for visits with somatisation potential was not significantly different between the two groups (1.09, 95% CI 0.72–1.64).
Table 1. Post-training incidence rate ratios for visits for FWWI participants when compared to comparison participants
Discussion
Using a propensity-matched comparison group, we investigated changes in health care utilisation after participation in the FWWI training, which addresses the emotional effects of ALEs. We found that after completing the FWWI program, participants had significantly fewer total and substance use visits when compared to comparison group participants. FWWI participants had fewer ED visits when compared to the comparison group, and this difference was borderline significant. We did not find a significant difference in visits with somatisation potential.
Emergency department (ED) visits
ED visits are expensive and often preventable [Citation45]. There is some evidence that more frequent ED visits can be associated with lower self-efficacy and coping skills as well as increased anxiety [Citation46–Citation50]. SCF internal data analyses have shown that as anxiety, depression and trauma symptomology increase, so do ED visits, even when controlling for other aspects of health. As internal FWWI evaluations show increased self-efficacy and reduced anxiety, depression and trauma symptomology among participants, this may be the mechanism through which the training reduces ED utilisation. FWWI focus group participants described a reduction in anxiety and distress as a result of processing their trauma and understanding it was not their fault, and an increased sense of control over their lives as a result of better understanding their emotions, seeing others with similar experiences making positive changes and building coping skills during trainings [Citation19]. These are all potential mechanisms that could reduce ED utilisation, and our findings are in line with behavioural health studies that indicate that 1) a person must process traumatic memories and build a coherent narrative in order to replace harmful thought patterns and contain experiences [Citation51,Citation52] 2) connecting with others can normalise experiences and reduce distress [Citation16,Citation53] and 3) coping skills can be learned and functioning improved using similar group exercises [Citation16,Citation18].
Reducing unnecessary ED visits is recognised as an important policy goal due to the potential for significant cost savings [Citation54]. A brief review of the literature indicates that many programs to reduce ED utilisation focus on primary care access, case management support and chronic conditions self-management education [Citation45,Citation48,Citation54]. Our study findings indicate another potential avenue: by addressing ALE-related distress and low self-efficacy. Felitti and colleagues found that non-stigmatising screening for ACEs was associated with fewer ED visits the following year [Citation55]. Otherwise, we could not find work on adverse experiences, trauma or PTSD that cited ED visit count changes as an outcome, or studies on reducing ED visits that focused on helping people to heal from adverse experiences. As such, this is an innovative finding.
Total system visits
Multiple studies have shown associations between higher overall health care utilisation and histories of trauma and abuse [Citation56,Citation57]. Our study indicates that directly addressing a history of traumatic experiences can reduce this higher utilisation. The potential mechanism is likely the same as proposed for ED visits: a reduction in anxiety, depression, and trauma symptomology, and an increase in self-efficacy, as shown by FWWI evaluations [Citation19]. This proposed mechanism is supported by the documented association between anxiety, depression and higher health care utilisation [Citation58].
Substance use visits
The relationship between adverse life experiences and substance use is well documented and has been explained through the self-medication model, which posits that persons experiencing PTSD attempt to cope with their distress by taking substances such as alcohol or drugs [Citation55,Citation59–Citation61]. In internal focus groups, multiple FWWI participants described previous substance use driven by ALE-related distress, and then noted that through FWWI they were able to resolve much of that distress, as well as develop healthy coping skills that replaced substance use. Yet, many substance use treatment programs do not directly address trauma histories, and participants suffering from PTSD often have worse treatment outcomes [Citation62]. Programs that do treat both have found that for those with trauma symptomology, reducing PTSD symptoms is more effective than health education in treating substance use [Citation63]. As such, there is recognised need for more trauma-informed approaches to substance use treatment [Citation62–Citation64]. Our study supports these findings and shows that when participants were able to address their trauma and build coping skills, substance-use health care visits decreased.
Visits with somatisation potential
Visits driven by somatic or medically unexplained symptoms are known to drive a high proportion of primary care visits, to be difficult to treat biomedically and to frequently be associated with a history of abuse or trauma [Citation2,Citation65,Citation66]. These visits can be difficult to distinguish through diagnosis codes, and we utilised a taxonomy that identifies visits with somatisation potential [Citation32]. We did not see a significant difference in incidence of visits with somatisation potential between FWWI and the comparison group. It is not clear whether the training did not reduce somatic visits or whether our outcome taxonomy, which included all diagnoses in the nervous system, gastrointestinal system, musculoskeletal system and ill-defined complaints, was overly broad. Additionally, the classifier was developed on persons with higher utilisation levels, and our cohort included persons with normal utilisation levels. Finally, SCF primary care providers noted using diagnoses related to stress or pain for some somatic visits but because these diagnoses are not included in the Smith classifier any changes in stress or pain-related visits would not have been captured in this study.
Limitations
Given the study’s observational design, there may be unidentified confounders that were not adjusted for in the model. The diagnosis taxonomy for visits with somatisation potential may have been overly broad and not captured change in visits with medically unexplained symptoms. The diagnosis taxonomy for substance use visits is a widely used measurement system and is likely more accurate, but it is possible some substance use visits were missed.
FWWI is a community-based program that does not require a referral through a healthcare system. FWWI often attracts participants who prefer a non-medical approach to emotional wellness. The comparison pool participated in emotional wellness programs that require a health care referral, such as counselling, group therapy or other behavioural health programs. Most importantly, both groups’ participants showed the desire to make a change in their life by seeking out and participating in an emotional wellness program. While the full comparison pool was fairly different from the treatment group (notably, the comparison pool had more behavioural health diagnoses but fewer ALEs and lower health care utilisation), the propensity matching process was able to select the members of the comparison group who were similar to FWWI participants (and result in similar average behavioural health diagnoses, ALEs and prior health care utilisation between the groups). While it is not clear if this study’s results would apply to all those utilising SCF’s various behavioural health programs (especially those with more behavioural health diagnoses), there are many people with multiple ALEs who prefer community-based programming and do not seek formal behavioural health services.
Conclusion
To our knowledge, this is the first propensity-score matched study of the health care utilisation effects of a psychosocial intervention to address adverse lifetime experiences. Our study, conducted in a closed health care system, shows that an Alaska Native program that helps adults heal from past adverse experiences can significantly reduce total health system visits and substance use visits. ED visits also showed a borderline significant reduction. Findings indicate promise for community programs that heal ALEs as a tool to address health disparities.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5):389–8.
- Drossman DA, Talley NJ, Leserman J, et al. Sexual and physical abuse and gastrointestinal illness: review and recommendations. Ann Intern Med. 1995;123(10):782–794.
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14(4):245–258.
- Hamby, S. L. The spectrum of victimization and the implications for health. In K. A. Kendall-Tackett editor, Application and practice in health psychology. Health consequences of abuse in the family: A clinical guide for evidence-based practice (p. 7–27). American Psychological Association, Washington, DC; 2004.
- Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060.
- Lanius RA, Vermetten E, Pain C. The impact of early life trauma on health and disease. Cambridge, UK: Cambridge UP; 2010.
- McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44.
- Seeman TE, Crimmins E, Huang MH, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004;58(10):1985–1997.
- Thoits PA. Stress and health: major findings and policy implications. J Health Soc Behav. 2010;51(Suppl):S41–53.
- Brave Heart MYH. Oyate Ptayela: rebuilding the Lakota Nation through addressing historical trauma among Lakota parents. Journal of Human Behavior in the Social Environment. 1999;2(1–2):109–126.
- Duran E, Duran B. Native American postcolonial psychology. Albany, NY: State University of New York (SUNY) Press; 1995. p. 227.
- Manson SM, Beals J, Klein SA, et al. Social epidemiology of trauma among 2 American Indian reservation populations. Am J Public Health. 2005;95(5):851–859.
- Napoleon H, Madsen EC (1991). Yuuyaraq: the way of the human being: with commentary: University of Alaska, Fairbanks, College of Rural Alaska, Center for Cross-Cultural Studies.
- Sarche M, Spicer P. Poverty and health disparities for American Indian and Alaska Native children: current knowledge and future prospects. Ann N Y Acad Sci. 2008;1136:126–136. Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2567901/
- Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. Am Sociological Rev. 1995;60:104–125.
- Cloitre M, Koenen KC, Cohen LR, et al. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol. 2002;70(5):1067.
- Ford JD, Russo E. Trauma-focused, present-centered, emotional self-regulation approach to integrated treatment for posttraumatic stress and addiction: Trauma Adaptive Recovery Group Education and Therapy (TARGET). Am J Psychother. 2006;60(4):335–355. Available from: http://lib-ezproxy.tamu.edu:2048/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=23723421&site=ehost-live
- Kinniburgh KJ, Blaustein M, Spinazzola J, et al. Attachment, self-regulation, and competency. Psychiatric Annals. 2005;35:424–430.
- Ray L, Outten B, Andrews P, et al. Disrupting the intergenerational transmission of trauma: a conceptual model for the family wellness warriors initiative. Journal of Health Disparities Research and Practice. 2019;12(2):40–71.
- Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106(1):29–39.
- Danese A, Moffitt TE, Harrington H, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163(12):1135–1143. Available from: https://doi.org/http://dx.doi.org/10.1001/archpediatrics.2009.214
- Dong M, Dube SR, Felitti VJ, et al. Adverse childhood experiences and self-reported liver disease: new insights into the causal pathway. Arch Intern Med. 2003;163(16):1949–1956.
- Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease adverse childhood experiences study. Circulation. 2004;110(13):1761–1766.
- Edwards VJ, Anda RF, Felitti VJ, et al. (2004). Adverse childhood experiences and health-related quality of life as an adult.
- Luby JL, Barch D, Whalen D, et al. Association between early life adversity and risk for poor emotional and physical health in adolescence: A putative mechanistic neurodevelopmental pathway. JAMA Pediatr. 2017;171(12):1168–1175. Available from: https://doi.org/http://dx.doi.org/10.1001/jamapediatrics.2017.3009
- Hoge CW, Chard KM. A window into the evolution of trauma-focused psychotherapies for posttraumatic stress disorder. Jama. 2018;319(4):343–345. Available from: http://ezproxy.library.tamu.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=mdc&AN=29362777&site=ehost-live
- Niknejad B, Bolier R, Henderson CR Jr, et al. Association between psychological interventions and chronic pain outcomes in older adults: A systematic review and meta-analysis. JAMA Intern Med. 2018;178:830, Available from
- Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(Suppl1):S149–S155. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222512/
- Gottlieb K, Outten B. Family Wellness Warriors. Fam Community Health. 2011;34(3):235–241.
- DHSS A (2011). Alaska screening tool. Available from: http://dhss.alaska.gov/dbh/Documents/Resources/pdf/AST_2011.pdf
- Ballard DW, Price M, Fung V, et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48(1):58–63.
- Smith RC, Gardiner JC, Armatti S, et al. Screening for high utilizing somatizing patients using a prediction rule derived from the management information system of an HMO: a preliminary study. Med Care. 2001;39(9):968–978.
- CDC. (2015). ICD injury matrices. Available from https://www.cdc.gov/nchs/injury/injury_matrices.htm
- AHRQ. (2018). Agency for healthcare research and quality healthcare cost and utilization project. Chronic condition indicator (CCI). Available from www.hcup-us.ahrq.gov/tools_software.jsp
- Dillard DA, Avey JP, Robinson RF, et al. Demographic, clinical, and service utilization factors associated with suicide‐related visits among Alaska Native and American Indian adults. Suicide Life-Threatening Behav. 2017;47(1):27–37.
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139.
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55.
- Brookhart MA, Schneeweiss S, Rothman KJ, et al. Variable selection for propensity score models. Am J Epidemiol. 2006;163(12):1149–1156.
- Stuart EA, King G, Imai K, et al. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28.
- Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172(9):1092–1097.
- Ho DE, Imai K, King G, et al. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007;15(3):199–236.
- Hardin JW, Hilbe JM. Generalized estimating equations. Chapman and Hall (US): CRC press; 2012.
- Hilbe JM. Negative binomial regression. New York (NY): Cambridge University Press; 2011.
- Nguyen T-L, Collins GS, Spence J, et al. Double-adjustment in propensity score matching analysis: choosing a threshold for considering residual imbalance. BMC Med Res Methodol. 2017;17:78. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5408373/
- Kellermann AL. Nonurgent emergency department visits: meeting an unmet need. Jama. 1994;271(24):1953–1954. Available from: https://doi.org/http://dx.doi.org/10.1001/jama.1994.03510480077038
- Adams RJ, Smith BJ, Ruffin RE. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax. 2000;55(7):566–573.
- Joyner J, Moore AR, Mount DL, et al. Emergency department patients self-report higher patient inertia, hopelessness, and harmful lifestyle choices than community counterparts. J Clin Hypertens (Greenwich). 2012;14(12):828–835.
- Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–1223.
- Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emer Med J. 2001;18(6):430–434.
- Wasilewski Y, Clark NM, Evans D, et al. Factors associated with emergency department visits by children with asthma: implications for health education. Am J Public Health. 1996;86(10):1410–1415.
- Rauch S, Foa E. Emotional processing theory (EPT) and exposure therapy for PTSD. J Contemp Psychotherapy. 2006;36(2):61–65.
- Wigren J. Narrative completion in the treatment of trauma. Psychotherapy: Theory, Research, Practice, Training. 1994;31(3):415.
- Cook A, Spinazzola J, Ford J, et al. Complex trauma. Psychiatric Annals. 2005;35(5):390–398.
- Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44(3):717–729.
- Felitti VJ, Anda RF. The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: implications for healthcare. In Lanius, Ruth A., Eric Vermetten, and Clare Pain, editors. The impact of early life trauma on health and disease: The hidden epidemic. Cambridge (UK): Cambridge UP; 2010. p. 77–87.
- Alexander RW, Aaron LA, Alberts KR, et al. Sexual and physical abuse in women with fibromyalgia: association with outpatient health care utilization and pain medication usage. Arthritis Rheumatol. 1998;11(2):102–115.
- Koss MP, Koss PG, Woodruff WJ. Deleterious effects of criminal victimization on women’s health and medical utilization. Arch Intern Med. 1991;151(2):342–347.
- Simon G, Ormel J, VonKorff M, et al. Health care costs associated with depressive and anxiety disorders in primary care. Am J Psychiatry. 1995;152(3):352.
- Dube SR, Anda RF, Felitti VJ, et al. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27(5):713–725.
- Dube SR, Felitti VJ, Dong M, et al. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564–572.
- Khantzian EJ. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harv Rev Psychiatry. 1997;4(5):231–244. Available from: https://doi.org/https://doi.org/10.3109/10673229709030550
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addict Behav. 1998;23(6):785–795.
- Hien DA, Jiang H, Campbell AN, et al. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. Am J Psychiatry. 2009;167(1):95–101.
- Brown PJ, Stout RL, Gannon-Rowley J. 15Substance Use disorder-PTSD Comorbidity: patients’ perceptions of symptom interplay and treatment issues. J Subst Abuse Treat. 1998;15(5):445–448.
- Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59 Suppl 20:15–21.
- Leserman J, Li Z, Drossman D, et al. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychol Med. 1998;28(2):417–425.