ABSTRACT
Background
Respiratory infections are a major health problem in the Inuit population of Nunavik, province of Quebec, Canada.
Objectives
A study was undertaken to assess the burden of lower (LRTI) and upper respiratory tract infections (URTI) and otitis media (OM) and to explore some of their determinants including the pneumococcal conjugate vaccine (PCV) status.
Methods
The reference population includes children less than 5 years of age born in 1994–2010 and a sample of 825 children was selected for this study. Outpatient medical records were reviewed. Visits with a diagnosis of LRTI, URTI and OM were extracted. Univariate and multivariate statistical analyses were performed to identify predictors of disease risk.
Results
The average number of LRTI, URTI and OM episodes were, respectively, 2.6, 6.2 and 5.9 from birth up to the 5th birthday. Seasonal patterns were similar for URTI and OM, but was different for LRTI. Children who received the recommended 4 PCV doses had a lower LRTI and OM risk than unvaccinated children. There was a trend towards a lower OM risk associated with a mixed PCV10+ PCV13 schedule compared with PCV7.
Conclusion
Results suggest a lower LRTI and OM risk associated with PCV use in this high-risk population but respiratory disease risk remains high compared with the general population in Quebec.
Introduction
Respiratory infections and otitis media constitute a major public health problem in indigenous communities of Northern Canada [Citation1–Citation4]. The Nunavik is the most northerly region of the province of Quebec and 89% of its population is Inuit [Citation5]. The population (n ≈ 13,000 in 2016) is living in 14 villages scattered along Hudson Bay and Ungava Bay, with no roads between them or to the south. There is a community health centre offering primary care and immunisation services in each village. There are two regional hospitals offering secondary care services in the region, one in the Hudson Bay area (Kuujjuaq) and the other in the Ungava Bay area (Puvirnituq). Tertiary care services are provided by university hospitals situated in Montreal. Pneumococcal infections are particularly frequent in the Inuit population [Citation6,Citation7]. To reduce the burden of pneumococcal infections among children, the 7-valent pneumococcal conjugate vaccine (PCV7) was introduced in 2002; it was replaced by the 10-valent PCV (PCV10) in 2009, and then by the 13-valent PCV (PCV13) in 2011. In 2018, the vaccination schedule changed to 3 PCV10 infant doses followed by a PCV13 toddler dose. The rationale for this mixed schedule was based on several considerations: (i) PCV10 has been shown to provide cross-protection against invasive pneumococcal disease (IPD) caused by serotype 19A strains, (ii) one PCV13 dose in the second year of life has the capacity to maintain a herd effect against serotype 19A Streptococcus pneumoniae (Sp), (iii) PCV10 may be more effective than PCV13 to prevent otitis media, (iv) and, importantly, PCV10 has a lower purchase cost than PCV13 in Canada [Citation8]. PCVs are offered, respectively, at age 2, 4, 6 and 12 months, and the uptake is high. Since the beginning of the programme, more than 90% of children received the recommended number of doses [Citation9].
In 2007, a research program was launched to assess the burden of upper (URTI) and lower respiratory tract respiratory infections (LRTI) and otitis media (OM) in the children population of Nunavik born in 1994–2010. The first objective of the present analysis was to measure the frequency of outpatient visits and URTI, LRTI and OM episodes in a sample of children with a follow-up extending from birth up to the 5th birthday. The second objective was to explore the effect of some predictors of disease risk including gender, age, season, year of birth, and pneumococcal conjugate vaccine status.
Methods
The study protocol was approved by the Quebec University Hospital Research Ethics Committee, the Nunavik Public Health Directorate and by Medical Directors of the regional health centres (Inuulitsivik Health Centre and Ungava Tulattavik Health Centre).
Study population
The study population were children less than 5 years of age born between January 1st, 1994, and December 31st, 2010, who were registered by the public health services of Nunavik. The registration is initiated at birth or at the first visit for children born outside Nunavik. The list of registered children included: the child’s name and surname, medical record number, village of residence, gender and date of birth.
Data collection
For logistical and budgetary reasons, the collection of data on outpatient visits was performed for a stratified (year of birth and village) random sample of births from 1994 to 2005 in the 14 villages (Phase 1 of the study), and for all births from 2006 to 2010 in the 3 largest villages representing 46% of the total population (Phase 2 of the study). Medical records were reviewed on-site by a team of 3 specially-trained graduate students working under the close supervision of one of the authors (JBL) and digital copies of relevant visits were made. Diagnoses reported by nurses (mainly) or physicians were classified and coded into 3 broad categories by one of the authors (JBL): upper respiratory tract infection (including any infection of the nose and nasal passages, paranasal sinuses, the pharynx, and the portion of the larynx above the vocal folds), lower respiratory tract infection (including any infection of the larynx, trachea, bronchi, lungs and pleura) and any type of otitis media. LRTI with URTI was coded as LRTI, whereas OM was coded as a separate entity. Successive visits for a same diagnostic category within a 28-day interval were considered as a single episode. Copies of immunisation cards of all children in the reference population were obtained from the primary health care centres. The information collected included type and date of all PCVs administered up to the 5th birthday. The analysis was restricted to children with a medical follow-up extending from birth up to their 5th birthday. Children who died or emigrated out of the region before their 5th birthday were excluded.
Statistical analyses
Rates of visits and episodes were computed by person-years of observation. Cumulative rates by the 5th birthday were calculated with the number of individuals at risk in the denominator. Univariate analyses of rates were computed by gender, age, year of birth and village using the whole dataset. The analysis of disease rates by calendar month was restricted to events during the years 1999–2010 during which the study population was homogeneous according to its age distribution. Mean numbers of episodes in different categories were compared using Poisson regression models. The existence of a trend in rates over time was tested using a linear regression model. Risks of first episodes from birth up to the 5th birthday in different immunisation status categories (hazard ratios) were compared using multivariate Cox regression models adjusting for potential confounders: gender (2 categories), age (continuous variable), season (4 categories), month of birth (4 categories) and village of residence (3 categories). Hazard proportionality assumption was tested using time varying variables and Schoenfeld’s method for independence between residuals and time [Citation9]. Statistical significance was set for p values < 0.05 (bilateral tests).
Results
A total of 825 children were included in the analysis. The sample represented about 16% of the 5 166 children born in the Nunavik region in the period 1994–2010. There were 404 children born in 1994–2005 (Phase 1) and 421 born in 2006–2010 (Phase 2). The distribution of study children by village and year of birth is provided in the Supplementary Table 1.
The overall frequency of LRTI, URTI and OM visits and episodes in the sample of 825 children is shown in . There were only two children without any visit for one of these conditions. The mean number of visits per episode was 1.9 for LRTI, 1.4 for URTI and 1.6 for OM. URTI and OM were particularly frequent with an average of 6.2 and 5.9 episodes per child, respectively, against 2.6 episodes for LRTI. There was no clear pattern according the place of residence and variations in rates could be explained by small numbers (details are provided in Supplementary Table 2).
Table 1. Frequency of visits and episodes of lower tract respiratory infection (LRTI), upper tract respiratory infection (URTI) and otitis media (OM) in a sample of 825 children born in the Nunavik region of Quebec, in 1994–2010, with a follow-up to their 5th birthday.
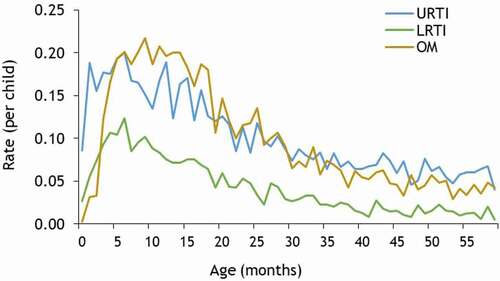
There were 435 girls and 390 boys in the study population but gender was not associated with a difference in the frequency of visits or episodes for the three conditions. The frequency rates of episodes by age in months is presented in . Both LRTI and URTI rates peaked at the age of 6 months whereas the OM rate peaked around the age of 12 months. These three conditions were less frequent in children 3 to 4 years of age than in younger ages.
Figure 1. Frequency rate of episodes of lower tract respiratory infection (LRTI), upper tract respiratory infection (URTI) and otitis media (OM) by age (in months), in a sample of 825 children born in the Nunavik region of Quebec, in 1994–2010, with a follow-up to their 5th birthday.
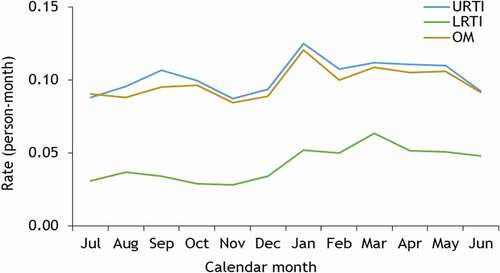
There was a seasonal variation in disease rates as shown in . URTI and OM had a very similar pattern with lower rates during the summer and fall, and a winter peak in January. For LRTI, the peak was observed in March.
Figure 2. Frequency rate of episodes of lower tract respiratory infection (LRTI), upper tract respiratory infection (URTI) and otitis media (OM) by calendar month, in a sample of 825 children born in the Nunavik region of Quebec, in 1994–2010, with a follow-up to their 5th birthday and observed during the years 1999–2010.
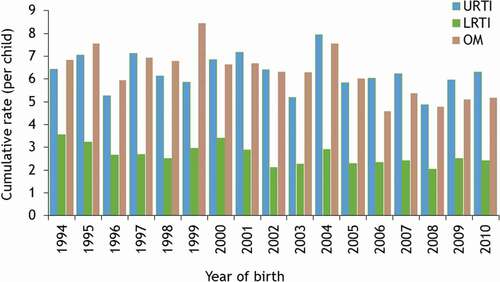
Cumulative frequencies of episodes by the 5th birthday according to the year of birth are shown in . There were statistically-significant negative linear trends over the successive birth cohorts for LRTI (regression coefficient = −0.058; p = 0.004) and for OM (regression coefficient = −0.147; p = 0.002) but this was not significant for URTI (regression coefficient = −0.038; p = 0.341).
Figure 3. Cumulative frequency rate of episodes of lower tract respiratory infection (LRTI), upper tract respiratory infection (URTI) and otitis media (OM) by year of birth, in a sample of 825 children born in the Nunavik region of Quebec, in 1994–2010, with a follow-up to their 5th birthday.
In the total sample, there were 167 unvaccinated children, mostly belonging to cohorts not eligible to receive the PCV7 (born before May 1997). The majority of children who received one (n = 54), two (n = 36) or three PCV (n = 11) doses were eligible to the PCV7 catch-up program for children more than 3 months of age. There were 557 children who received the recommended 4 doses. The number of children who received PCV7 only (1 to 4 doses) was 446, 33 received PCV10 only, 18 PCV13 only, and 161 received different vaccines, including 71 who received PCV10 followed by PCV13 (details in Supplementary Table 3).
A comparison of the mean number of episodes by immunisation status was performed for the children living in the 3 villages selected for both phases and born from 1994 to 2010 in order to control potential variations in rates between villages. Unvaccinated children born in May 1997 and after and who were eligible to receive a PCV were excluded as they may have been protected by the herd effect generated by vaccinated children. As shown in , children who received the recommended four PCV doses tended to have a lesser number of disease episodes than unvaccinated children. Relative differences were, respectively, 22% for LRTI (rate ratio = 0.78; p = 0.001), 7% for URTI (rate ratio = 0.93; p = 0.16) and 20% for OM (rate ratio = 0.80; p < 0.001).
Table 2. Mean number (per child) of episodes of lower tract respiratory infection (LRTI), upper tract respiratory infection (URTI) and otitis media (OM), according to immunisation status, in a sample of 572 children born in 3 villages in the Nunavik region of Quebec, in 1994–2010, with a follow-up to their 5th birthday.
Results of multivariate Cox regression models among children in the 3 largest villages showed a reduced risk of first episode among children who received at least one PCV dose compared to unvaccinated children with hazard ratios values, respectively, of 0.64 for LRTI (p = 0.01), 0.78 for URTI (p = 0.08) and 0.73 for OM (p = 0.05) (details in Supplementary Table 4 to 6).
An exploratory analysis was conducted to compare outcomes among 293 children who received PCV7 only and 71 children vaccinated with PCV10 followed by PCV13 in the 3 largest villages. The average number of LRTI episodes per child was 3.1 in the PCV7 group and 3.0 in the PCV10+ PCV13 group. The corresponding figures were 6.0 vs 6.1 for LRTI and 5.8 vs 5.3 for OM (details in Supplementary Table 7). Using a multivariate Cox model and the PCV7 group as the reference, hazard ratios for first episodes associated with a mixed schedule were, respectively, 0.85 (p = 0.50) for LRTI, 1.15 (p = −0.47) for URTI and 0.91 (p = 0.65) for OM (details in Supplementary Table 8 to 10).
Discussion
To our knowledge, this is the first study aiming to assess the burden of respiratory infections and otitis media seen in outpatient clinics in the paediatric Inuit population of Canada. For budgetary and logistical reasons, the study was restricted to a sample 825 children representing 16% of all children born in 1994–2010 in the Nunavik region of Quebec. The power of the study to identify statistically significant differences and trends of low magnitude is thus limited. The study population include only children with available records up to their 5th birthday. Children who died or emigrated outside the region before their 5th birthday were excluded from analyses. Crude diagnostic categories were used as misclassification between subcategories (i.e. bronchiolitis vs pneumonia; acute OM vs chronic OM vs OM with effusion) is a recognised issue. These are limitations.
Results show a persistent high risk of respiratory infections and otitis media in the paediatric Inuit population of the Nunavik experiencing unfavourable living conditions: a climate dominated by long and cold winters, inadequate and crowded housing, poor diet, poor accessibility to drinking water and specialised health services, low level of education and income, high rate of unemployment, high rate of smoking, alcohol and illicit drug dependence [Citation10–Citation12]. The incidence of invasive pneumococcal infections in the Nunavik population is 5 to 10 times higher than in the general population of Quebec [Citation6]. We do not have precise statistics on the frequency of medical visits for respiratory infections in the population of Quebec living in the Southern part of the province but results of a study on physician claims to the universal provincial health insurance for otitis media are available [Citation13]. In this study, the cumulative rate of visits from birth to the 5th birthday during the period 2005–2007 was 395 per 100 children. Assuming as in the present study that there were 1.6 visits for each OM episode, the mean number of OM episode per child would be 2.5, which is more than two times lower than in the Nunavik with 5.9 episodes per child.
An interesting observation was the very similar seasonal pattern between URTI and OM but not for LRTI pointing to aetiological similarities and differences. Viruses play an important role in the aetiology of URTI and any URTI may trigger an acute otitis media involving a bacterial infection [Citation14]. Bronchiolitis, a common LRTI in young children, is mainly caused by the Syncytial Respiratory Virus not frequently found in OM, whereas pneumonia may be caused by a large variety of viruses and bacteria [Citation15]. There is a paucity of data regarding the organisms
that trigger and cause OM in Inuit children. Some degree of diagnostic misclassification between URTI and OM may also have contributed to their seasonal similarity.
An objective of the study was to explore the association between pneumococcal vaccine status and disease risk. Compared to unvaccinated children, those who received the recommended 4 PCV doses had a statistically lower mean number of LRTI and OM episodes in univariate analyses (). The difference was not statistically significant for URTI which are mainly caused by viruses [Citation14]. In multivariate analyses (Supplementary Tables 4 and 6), the risk of first LRTI episode was 36% lower among vaccinated children than among unvaccinated children (any regimen) and the relative difference was 27% for OM. These results have to be interpret carefully as there may be a cohort effect and a progressive improvement in health associated with other time-dependent factors. Pneumococcal conjugate vaccines may have contributed to the decline in disease risk, however, especially for LRTI and OM. The incidence of invasive pneumococcal disease among children less than 5 years of age in the Nunavik decreased from 350 per 100 000 person-years in 2000–2001, before any PCV use, to 212/100 000 in 2010–2016, a 39% difference [Citation7]. Assuming that 30% of all pneumonia are caused by Streptococcus pneumonia [Citation16] and that 60% of acute respiratory infections in children are pneumonia [Citation17], a 39% decrease in pneumococcal infection risk would translate into a 7% decrease in the incidence of all-cause LRTI.
The current immunisation schedule in the Nunavik is three PCV10 infant doses followed by a PCV13 toddler booster dose. Although not many children in the study received a mixed regimen consisting of PCV10 followed by PCV13 (n = 71), there was no indication of an increased disease risk compared with those who received PCV7 only, and there was a trend towards a lower risk for OM (Supplementary Tables 7 and 10). These results are in line with observations in Australia and Sweden. In an observational study among Indigenous Australian children, those vaccinated with PCV10 has less suppurative OM than those vaccinated with PCV7 [Citation18]. A time-series analysis conducted in Sweden on administrative records showed that the introduction of PCVs was followed by a decrease in the frequency of medical visits for otitis, myringotomy, and ventilation tube insertions in children and the decrease was more marked in counties that used PCV10 than in those that opted for PCV13 [Citation19].
In conclusion, there was a weak time-trend towards a lower incidence of LRTI, URTI and OM among Inuit children in the Nunavik region and the sequential use of different PCVs may have contributed to this. The disease risk, however, remains much higher than in the Quebec population of other regions.
Registration
ClinicalTrials.gov registration number: NCT01694329
Supplemental Material
Download MS Word (30.5 KB)Acknowledgments
The authors thank all the health professionals in Nunavik who participated in data collection.
Disclosure statement
Philippe De Wals has received research grants and reimbursements of travel expenses from vaccine manufacturers including the GSK Group of Companies, Novartis, Pfizer and Sanofi Pasteur. The other authors have no potential conflict of interests to report.
Supplementary materials
Supplemental data for this article can be accessed here
Additional information
Funding
References
- MacMillan HI, MacMillan AB, Offord DR, et al. Aboriginal health. CAMJ. 1996;155:1569–6.
- He H, Xiao L, Torrie JE, et al. Disparities in infant hospitalizations in indigenous and non-indigenous populations in Quebec, Canada. CMAJ. 2017;189:E739–46.
- Ayukawa H, Bruneau S, Proulx JF, et al. Otitis media and hearing loss among 12-16-year-old Inuit of Inukjuak, Quebec, Canada. Int J Circumpolar Health. 2004;63(Suppl 2):312–314. .
- Dallaire F, E D, Vzina C, et al. Portrait of outpatient visits and hospitalizations for acute infections in Nunavik preschool children. Can J Public Health. 2006;97:362–368.
- Aboriginal Population Profile. Census. Statistics Canada; 2016. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/abpopprof/details/page.cfm?Lang=E&Geo1=AB&Code1=2016C1005084&Data=Count&SearchText=Nunavik&SearchType=Begins&B1=All&GeoLevel=PR&GeoCode=2016C1005084&SEX_ID=1&AGE_ID=1&RESGEO_ID=1
- Degani N, Navarro C, Deeks SL, et al. Invasive bacterial diseases in Northern Canada. Emerg Infect Dis. 2008;14:34–40.
- LeMeur JB, Lefebvre B, Proulx JF, et al. Limited impact of pneumococcal vaccines on invasive pneumococcal disease in Nunavik (Quebec). Can J Public Health. 2019;110:36–43.
- Comité sur l’immunisation du Québec. Scientific advisory on the optimal schedule for childhood immunization against pneumococcal disease in Québec. Quebec city (QC): Institut national de Santé publique du Québec; 2017. Available from: https://www.inspq.qc.ca/sites/default/files/publications/2379_opinion_optimal_schedule_childhood_immunization_pneumococcal_disease.pdf
- Cléophat JE, Le Meur JB, Proulx JF, et al. Uptake of pneumococcal vaccines in the Nordic region of Nunavik, province of Quebec, Canada. Can J Public Health. 2014;105:e268–72.
- First Nations and Inuit health indicators. Ottawa (ON): Government of Canada. Available from: https://health-infobase.canada.ca/fnih/
- Fortin M, Bélanger RE, Boucher O, et al. Temporal trends of alcohol and drug use among Inuit of Northern Quebec. Can Int J Circumpolar Health. 2015;4:e29146. .
- Climate, Nunaviké Wikipedia; 2020. Available from: https://en.wikipedia.org/wiki/Nunavik#Climate
- De Wals P, Carbon M, Sévin E, et al. Reduced physician claims for otitis media after implementation of pneumococcal conjugate vaccine program in the province of Quebec, Canada. Pediatr Infect Dis J. 2009;28:e271–5.
- Nokso-Koivisto J, Marom T, Chonmaitree T. Importance of viruses in acute otitis media. Curr Opin Pediatr. 2015;27:110–115.
- Moore HC, de Klerk N, Keil AD, et al. Use of data linkage to investigate the aetiology of acute lower respiratory infection hospitalisations in children. J Paediatr Child Health. 2012 Jun;48(6):520–528.
- Morrow A, De Wals P, Petit G, et al. The burden of pneumococcal disease in the Canadian population before routine use of the seven-valent pneumococcal conjugate vaccine. Can J Infect Dis Med Microbiol. 2007;18:121–127.
- Anderson G, Deceuninck G, Zhou Z, et al. Hospitalisation for lower respiratory tract infection in children in the province of Quebec, Canada, before and during the pneumococcal conjugate vaccine era. Epidemiol Infect. 2017;145:2770–2776.
- Leach AJ, Wigger C, Andrews R, et al. Otitis media in children vaccinated during consecutive 7-valent or 10-valent pneumococcal conjugate vaccination schedules. BMC Pediatr. 2014;14:200.
- Gisselsson-Solen M. Trends in otitis media incidence after conjugate pneumococcal vaccination; A national observational study. Pediatr Infect Dis J. 2017;36:1027–1031.
