ABSTRACT
Aims 1) to describe the dental health goals and the single financial goal defined in 2008 with a new national caries strategy in Greenland (CSG) and the progress made during the subsequent 10-year period; 2) to describe the CSG initiatives; and 3) to report caries outcome data for 3-year-old children as well as 9-year-old children in 2012 and 2018; for 6-year-old children as well as 12-year-old children in 2015 and 2018 and for 15-year-old children in 2018, and to compare the data with the baseline data from 2008. Only 6 of the 20 dental health goals were close to being or were achieved over the 10-year period. The total cost of running PDHS-G increased by 4% from 2008 to 2018. The CSG strategy focused on predetermined visits/examinations, risk-related recalls, oral health promotion and predetermined fluoride and sealing policies. The percentage of children with a defs/DMFS = 0 increased by 8–18%, and the mean defs/DMFS decreased by 40–60% between 2008 and 2018 in all five age groups involved. To conclude, the goals defined in 2008 were generally not achieved (failure), but the caries status improved significantly from 2008 to 2018 in all age groups (success).
Introduction
The Public Dental Health Service in Denmark (PDHS-D) for children and adolescents that was introduced in 1972 by a government Act has been a success. In 1974, the percentage of 15-year-old children with a DMFS = 0 was 2.7% on a national level [Citation1], while in 2018 the corresponding figure was 63% [Citation2]. This in spite of the considerable inter-municipality variation in caries experience in Denmark which has been noted over the years [Citation3,Citation4].
Greenland is part of Denmark but has been self-governed since 2009. The Public Dental Health Service in Greenland (PDHS-G) for children has been very similar to its Danish counterpart. In 2007, the first author of the present paper was invited by the chief dental officer in Greenland at the time to help optimise the PDHS-G. Data showed that the prevalence and incidence of caries were high in Greenland, and that they had been for a number of years compared to the caries status in Denmark[Citation5], but also compared to caries data in the other countries in the circumpolar area[Citation6]. Even before 2008, the PDHS-G had modern equipment at its disposal in both towns and rural areas, and dental professionals visited at least once a year to conduct dental examinations and provide treatment in rural areas. One major problem, however, was recruiting dentists who were willing to work for longer than 3 months. In 2007, of the 34 dentists assigned to the dental service system, only four were native and the rest came from Denmark, other Scandinavian countries, or Germany.
The invitation from the chief dental officer was accepted and resulted in a workshop held in Nuuk in 2007 which was attended by representatives from the PDHS-G, by the first author and by the co-workers who were recognised as having developed the Nexö method together with the first author[Citation7]. The Nexö method is an effective non-operative caries treatment programme whose caries preventive principles were used in many clinics taken care of children all over Denmark and still are. At this meeting, goals for the prevalence of caries disease in children at specific ages were set for the following 10 years. The new national strategy, referred to as the Caries Strategy Greenland (CSG), was to be implemented on the 1 January 2008 throughout Greenland. The preventive part of the strategy relied on the most stable and native members of the dental staff, the dental hygienists. Furthermore, it was presumed that the CSG would not lead to increases in the annual costs of the Public Dental Health Service in Greenland after taking inflation into account.
The aim of this report is: 1) to describe the 20 dental health goals and the single financial goal to be achieved with the CSG between 2008 and 2018; 2) to describe the initiatives under the CSG; and 3) to report caries outcome data for 3-, 6-, 9-, 12-, and 15-year-old children in 2008 (baseline) and compare the data with corresponding data obtained in 2012 and 2018 (the 3- and 9-year-olds); in 2015 and 2018 (the 6-and 12-year-olds); and in 2018 (the 15-year-olds).
Materials and methods
A detailed description of the CSG was published in 2015[Citation8]. Thus, a summarised version is provided below:
In 2008, the dental staff in the PDHS-G included 34 dentists, of whom four were native, 21 full-time native dental hygienists, 53 native dental assistants/trained employees, 10 native dental technicians, and one chief dental officer (Danish). The corresponding figures in 2018 were: 31 dentists (of whom five were native), 23 native dental hygienists, 64 native dental assistants, nine native dental technicians, and one chief dental officer (Danish).
Caries strategy Greenland, CSG
The first step was to upgrade the staff within the field of cariology. The CSG was based on the following four principlesCitation[8]: I) annual recording (using pre-coded registration forms) of the dental health status of children in Greenland; II) focus on goals to be achieved (see ); III) focus on visits and examinations at relevant dental ages (see ); and IV) a non-operative caries treatment programme (see ). Principles I, III and IV were primarily implemented by dental hygienists (see below). Operative treatments were performed by the dentists.
Table 1. Goals stated (GS) in 2008 and actual data (AD) in 2012, 2015 and 2018 in the different age groups.
Table 2. Overview of dental ages where CSG invites children/parents to the clinic. The clinical examinations are divided into a traditional clinical examination and extended clinical examination, the latter where radiographs were taken*. In addition, the table indicates what were done at the visits and clinical examinations and by whom.
Actual data I: recording dental health status
In implementing the CSG, a modified version of the Danish dental status recording system (SCOR) was implemented and became mandatory for recording the dental status on children in Greenland. The agreement was that the dental health status of each child should be recorded reaching the age of, 3, 6, 9, 12, and 15 years. The modified version which was to be used in Greenland was called GCOR. The caries recordings were made using 10 scores[Citation8]. Moreover, the GCOR recordings included the gingival status for reference teeth and deviations relevant for orthodontic treatment.
Actual data II: goals to be achieved
The first stated goal was that from 2012 and onwards ≥85% of children should, on reaching the age of 3, 6, 9, 12, and 15 years should have their dental status recorded in the GCOR system. The dental health goals (GS) in the years 2012–2018 are presented in and compared to the data from 2008. Another goal was that the total cost of running the PDHS-G after implementing the CSG should not exceed the 2008 level when adjusted for inflation.
Actual data III: focus on visits and examinations at relevant dental ages
presents the nine agreed times for when the motivation visits (toddlers) and the examinations of older children and adolescents up to the age of 15 should take place. Also, who was responsible for conducting the motivation visits and the examinations. In addition, the children were recalled to the clinic between the visits and examinations according to individual risk assessments. The risk indicators were inadequate oral hygiene, unhealthy diet, lack of compliance, and caries activity in the dentitions. For the permanent dentition, the emergence of molar teeth and orthodontic treatment was also included as risk indicators. For children who were classified as being at a high risk of developing caries, recalls were made after 4 months, while children with a moderate risk were recalled about 6 months after the examination. Low-risk children were not recalled to the clinic until the next predetermined visit ().
Actual data IV: the non-operative caries treatment programme
Dental health education and promotion
During the first visit (motivation visit) at the age of 8 months (), the child’s parents were informed about the structure and tasks of the dental health system for children in Greenland, that their child was born with healthy teeth, and that they (the parents) were responsible for keeping the child’s teeth healthy. A guide, in which the illustrations and photos were based on the Greenlandic environment and which was written in Greenlandic and in Danish, was discussed and handed out to the parents/child during this first visit. The guide covered relevant information regarding caries related to the nine predetermined visits and examinations presented in .
At each and every visit, both parents and children were trained in how to perform adequate plaque control twice a day using 1,450 ppm fluoridated toothpaste, while dietary advice was also provided. Furthermore, the visit included professional plaque removal, which was primarily performed by the dental hygienists who also evaluated the child’s caries risk and assessed whether the child could wait until the next predetermined examination or should be called in earlier (interim risk-related visits).
In addition, from the age of about 9 years, the child was considered able to assume responsibility for keeping his/her teeth healthy (). At the interim risk-related visits (), no general examination was performed, only specific caries problems were addressed.
Fluoride policy
The staff advised all parents to use 1,450 ppm fluoridated toothpaste when brushing their children’s teeth. Each child’s teeth should be brushed twice a day, from when the child’s first tooth emerged, the amount of toothpaste per day corresponding to the size of the nail on the child’s little finger. Furthermore, at the motivation visits, examinations and at the interim visits, fluoride varnish (Duraphat, 22,600 ppm F) or solutions (9,200 ppm F NaF solution) had to be applied on active, non-cavitated lesions and on surfaces at risk of lesion development[Citation9].
Sealing policy
All pits and fissures on permanent molar teeth should be preventively or therapeutically sealed when moisture control could be established[Citation10].
Settlements
It is important to emphasise that about 15% of children live in settlements which are remote communities (n = 60) with between 30 and 500 inhabitants, i.e. too few inhabitants for the settlement to be classified as a town. The intention, both before and during the CSG, was that children living in settlements would be seen by a dental hygienist/dentist once a year.
Additional workshops
Annual workshops, led by the first author and co-workers, were held for the dental staff from 2009 to 2012 and again in 2014. The main aims of the workshops were to continue the education of the staff in cariology, to calibrate (see below) the staff to the caries scoring systems they had to use and to update them on the interim results achieved under the CSG each year.
Calibration of caries recordings
The intra- and inter-reproducibility of the caries scoring system within the GCOR were measured, using photographs of the 10 caries scores. The entire staff participated in the tests at the workshops in 2010 and 2012. The Kappa values (surface level) for intra-reproducibility varied between 0.19 and 1.0 (mean 0.82, SD = 0.18), and the inter-reproducibility varied between 0.24 and 1.0 (mean 0.80, SD = 0.14).
GCOR scorings
The recording forms (see in reference 8) completed by hand by the dental hygienists/dentists every year in the clinics were submitted to IBM in Denmark for optical reading and the preparation of annual, standardised tables for each age cohort. Data were expressed at national level and at district level (n = 17), including both towns and settlements. For this paper, we concentrated on caries data.
Statistics
Outcomes (See ): The following outcomes were extracted in the period 2008 to 2018:
The number of submitted forms from the towns, including the settlements.
Percentage of children with a defs = 0, with >8 defs and the mean defs (3- and 6-year-old children)
Percentage of children with a DMFS = 0 with >4 DMFS and the mean DMFS (9-, 12- and 15-year-old children).
The mean number of extracted primary teeth (mentioned ex, in ) (3- and 6-year-old children) or permanent teeth (9-, 12-, and 15-year-old children mentioned Ex, in ).
The mean number of sealed surfaces for the 9-, 12-, and 15-year-olds. These figures have been extracted every year since 2012, and the medians for the age groups were presented for the subsequent 7 years.
In order to find out whether districts with many settlements (≥6, n = 5) influenced the caries burden both in the primary and in the permanent dentition, Chi-square analyses with Yates corrections were performed using the number of children in the districts with a defs = 0 or with a defs≥1 among the 6-year olds, and with a DMFS = 0 or a DMFS≥ 1 among the 15-year olds. Data from 2018 were used.
Concerning the mean defs/DMFS, F-tests Welch’s ANOVA and Post Hoc tests were made to compare 2008 versus 2012/2015 versus 2018 for the different age groups. In addition, the 95% confidence intervals are presented.
Information about the composition of the dental staff and the cost of running the PDHS-G in 2008 and in 2018 was obtained from the chief dentist. The annual inflation was based on figures from Statistics Greenland [http://bank.stat.gl/pxweb/da/Greenland/Greenland__PR/PRXPRISV.px/table/tableViewLayout1/?rxid=23994775-2d03-4c60-bb4a-0d26acaa6740].
Results
shows the dental health goals defined in 2008 (lines SG 2008) and what was actually achieved (lines AD) in 2012 for the 3- and 9-year-olds; in 2015 for the 6- and 12-year olds and in 2018 for the 15-year-olds, the years in which the designated goals had to be evaluated. Finally, for all age groups, data were also shown for 2018 in order to identify trends.
First, the outcomes defs = 0%/DMFS = 0 increased between 8% (9-year olds in 2008 = 57% to 65% in 2015; column 4, row 4) and 17% (15-year olds in 2008 = 14% to 31% in 2018; column 4, row 6) in the years of evaluation. An additional 13% increase in the percentage of children with a DMFS = 0 was seen in 2018 for the 9-year olds (79% versus 65%; column 4, row 4) compared to 2012 and about 10% for the 12-year olds in 2018 compared to 2015 (55% versus 44%; column 4, row 5).
For the 3-year-old children the data were very close to that stated in the goals apart from the number of recorded 3-year-olds. For this age group, the goal was that >85% of the 3-year olds in 2012 should have had their dental status recorded, but this figure was only 75%, increasing to 78% in 2018 (column 2, row 2). The goal of having >80% of children with a defs = 0 was close to having been achieved (76% in 2012 and 78% in 2018, column 3, row 2).
For the 6-year-old children, we were close to achieving the following goals in 2015 with about >90% recorded registration formulas (85%, column 2, row 3) and 50% of children with a defs = 0 (49.5%, column 3, row 3), but we were a long way from achieving the goal that <5% of children had a defs>8 (column 5, row 3). The actual figure in 2015 was 24.3% of the children, and it was similar in 2018.
For the 9-year olds we were a long way from achieving the goal of 80% of children with a DMFS = 0 in 2012 (65%, column 4, row 4), but we came close in 2018 (78.6%, column 4, row 4). The goal of <5% of children having a DMF>4 was achieved in 2018. We also came close to achieving the goal that no children aged nine should have any permanent teeth extracted (mean = 0.04, last column, row 4).
For the 12- and 15-year-old children, we were a long way from achieving any of the goals stated back in 2008. For example, that <5% of 12- and 15-year olds should have a DMFS = 0. The actual figures were two to four times higher (column 6, rows 5 and 6) ().
Concerning sealants, the median for the 9-year-old children in the 2012–2018 period was 3.69 sealed surfaces. The corresponding figures for 12- and 15-year olds were 7.09 and 8.58, respectively.
Internal analyses disclosed that in districts with many settlements (≥6), among the 6-year-old children in 2018 there was a significantly lower percentage with a defs = 0 compared to districts with few settlements (Chi-square 19.4309; df = 1, p < 0.0001). This was also true for the 15-year olds in 2018 (Chi-square 13.8651; df = 1, p = 0.002).
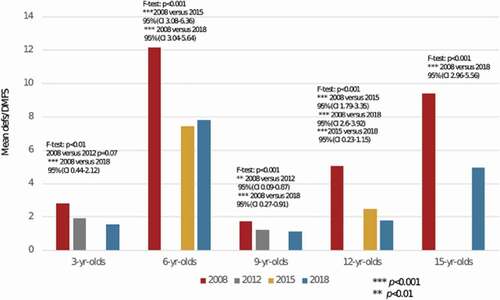
illustrates the mean defs/DMFS of the children in different years as well as in the different age groups. The p values from the F- and post hoc tests, as well as the 95% CI, are presented in the figure.
In general, the mean defs/DMFS decreased by 30–60% from 2008 to 2018 in the five age groups. For the 3-year-olds, the mean defs in 2012 (1.81) did not differ significantly from 2008 (2.82) (p = 0.07), while the mean defs in 2018 (1.54) differed significantly from 2008. The 95% confidence interval ranged between 0.44 and 2.12, thus a rather low lower bound. This was also the case for the 95% confidence interval for the 9-year-old children: 95% CI 0.09–0.87/95% CI 0.27–0.91 (), and there was even a significant decrease in mean DMFS from 2008 (1.72) to 2012 (1.24) and from 2008 to 2018 (1.13). For the other age groups, the CI 95% lower bounds were ≥1.79, indicating that the levels reached in mean defs/DMFS (7.4, 7.8 for the 6-year-olds, 2.5, 1.8 for the 12-year-olds, and 5.0 for the 15-year-olds) are of significant clinical relevance compared to the data from 2008.
Total cost of running the PDHS-G in 2008 and in 2018
Analyses disclosed () that the total cost of running the PDHS-G in 2018, after taking inflation into account.
Table 3. Costs in mill Danish crown in 2008 adjusted for inflation and the actual costs in 2018 for running the public dental health service in Greenland.
Discussion
Greenland
Greenland is the world’s largest island. Between 2008 and 2018, the population totalled approx. 56,000 people. About 15% of the population lived in settlements, 20% of the population was below 15 years of age, and the annual birth cohort was approx. 800.
The dental care system pre-2008
In 2007, when CSG was being planned, there was a very high caries experience among the Greenlandic population, there was a politically supported and reasonably funded national dental health service system with free dental care for children and adolescents up to the age of 15 years, and there were up-to-date and well-equipped dental clinics distributed across the 17 Greenlandic districts.
The Public Dental Health Service in Greenland for children has always been school-based. In 2007, as now, the staff comprised stable and skilled native dental hygienists, skilled as well as unskilled dental assistants, and dentists who were usually short-term locum dentists from Denmark. The dentists managed the staff and dealt mainly with operative treatment. In 2007, the time for a child’s first visit to the dental clinic as well as recalls, oral health promotion, fluoride and sealing policies were all decided locally in the 17 districts. Recordings of dental status, including caries recorded according to the GCOR at that time, were made regularly until 1996 all over Greenland, and very irregularly between 1996 and 2008. Due to a high level of dental disease, interventions such as extractions were common treatment measures for both children and adolescents. Furthermore, restorative – as opposed to preventive – dental care was dominant. These measures had resulted in a marginal improvement in the caries experience among adolescents in Greenland, i.e. the mean DMFS index for 15-year olds was 10.6 in 1996, 10.0 in 2002 [Citation5] and 9.4 in 2008 ().
CSG strategy from 2008 to 2018
The structure of the CSG differs in certain aspects from the strategy that was in place up until 2008. For example, the CSG offered a first visit to the clinic when the child was 8-month old followed by eight other predetermined visits up until the child reached the age of 15 (). These specific dental ages were selected according to the possibility of initiating dental health education and promotion before the development of caries on susceptible surfaces [Citation11,Citation12]. Between the predetermined visits, the parents/children were also offered non-operative care according to individual needs. The interventions (broadly speaking the non-operative care) used are described in under the heading “What to do”.
In addition, the CSG was based on predetermined fluoride and sealant policies. Fluoridated toothpaste with 1,450 ppm F was recommended for all children, the amount not exceeding the size of the nail of the child’s little finger per day[Citation13]. Furthermore, local application of 2% NaF liquid (9,200 ppm F) or Duraphat (22,600 ppm F) was to be applied on all initial lesions and placed on surfaces at risk[Citation9]. This type of systematic approach to the local application of fluoride was not used in the service prior to 2008.
CSG – goals and outcomes
The effect of the CSG was tested at the population level in a practice-based setup as opposed to a trial with randomised allocation to test and control groups. The goals set in CSG 2008–2018 were motivated by what had been achieved by the Public Dental Health Service for Children and Adolescents in Denmark over an extended period of time.
To begin with, it is important to emphasise that the intra- and inter-examiner reproducibility of the caries scoring system, which was tested twice during the 10-year period, was found to be substantial or perfect[Citation14]. Thus, the collected caries data obtained in the present study are reliable. The reason for deciding on the goal that >85% of all relevant age cohorts should have their dental status recorded was that the data is more valid if it is based on the majority of an age cohort. The lowest figure in this study was 75% for the 15-year-old children. As the birth cohort in Greenland is approx. 800 a year, it corresponds to >600 children in the different age groups having had their dental status recorded in this study.
There is no doubt that there has been a significant improvement in caries prevalence and caries severity in all five age groups involved in the evaluation. It was also interesting to note that there is a trend towards a continued reduction in caries incidence over the 10-year period, and thus most of the figures are better in 2018 than in 2012 or 2015. Look, for example, at the 9- and 12-year-olds, where the DMFS>4 goal of <5.0% of the children (, column 6, rows 4 and 5) has decreased from 9.0% in 2012 to 3.0% in 2018 for the nine-year-olds, and from 16.5% in 2015 to 10.8% in 2018 for the 12-year-olds. The high values of lower bounds in the confidence intervals obtained among the 6-, 12- and 15-year olds () indicate that the obtained results are of clinical relevance[Citation15].
Why were the goals not achieved?
Due to the very high caries experience in the Greenlandic population, adding artificial fluoride to the water supply on a national scale would be a more effective way of controlling the caries situation. Only recently, Iheozor‐Ejiofor et al. [Citation16] published a Cochrane review, which concluded that “water fluoridation led to a 15% increase in children with no decay in their baby teeth and a 14% increase in children with no decay in their permanent teeth. These results are based predominantly on old studies and may not be applicable today”. However, there was and still is no central water supply system in Greenland, and it was finally concluded in 2005 that such a community-based approach was not feasible in Greenland[Citation5]. Instead, the Home Rule Cabinet in Greenland decided in 2005, on the recommendation of WHO [Citation17], to implement salt fluoridation throughout Greenland. Thus, the influence of salt fluoridation was a factor that had to be taken into account when we assessed the goals. The first author actually initiated a systematic review in order to identify at what level salt fluoridation could contribute to a reduction in caries, and found a median preventive fraction of 45% reduction in caries experience in adolescents after using fluoridated salt. The reliability of the data was poor due to the fact that no randomised clinical trial had been undertaken[Citation18]. Fluoridated salt (220 ppm F) should already have been available by 2008, but finally became available in shops in Greenland from 2010. However, it was not embraced by the general population because it was too expensive compared to non-fluoridated salt. In fact, very few packs of fluoridated salt were sold. Thus, without some caries-reducing benefit from the fluoridated salt [Citation18,Citation19], the goals set in 2007 for the age cohorts which were to be achieved in 2012, 2015 and 2018 () were too optimistic. From 2019, and following this evaluation of the CSG, the (new) chief dental officer in Greenland has decided to support the CSG with fluoride rinsing programmes on a national level for children aged 6 to 15 years. A Cochrane review has stated that a significant reduction in caries will be seen as a result of fluoride rinsing programmes, even when using fluoridated toothpaste[Citation20].
Another reason for not achieving the goals was probably because the CSG guidelines were not strictly followed. In connection with the annual workshops, internal analyses of dental records were performed in order to illustrate the degree to which the dental staff had been able to meet the requirements of the CSG. One review showed that the recall frequency for the 3-year olds was about two compared to the suggested three times (motivation visits, ). A second review disclosed also only a marginal use of local applications of Duraphat/2% NaF solution for controlling active caries lesions in the permanent dentition.
An important aspect of the CSG was that all occlusal surfaces including the susceptible buccal and palatal pits and fissures on permanent molar teeth should be sealed. Thus, a total of eight surfaces were to be sealed on 9-year olds and 16 surfaces on, e.g., 15-year olds. It seems that about 50% (mean 3.80 surfaces) of the surfaces which are prone to caries were sealed in 2012 among the nine-year-olds[Citation8], and the same level was sealed during the 2008–2018 period on the 9-, 12- and 15-year olds (means 3.69, 7.09 and 8.56, respectively). Thus, it is tempting to believe that even better data concerning the prevalence of caries among the Greenlandic child population can be obtained if all the above-mentioned surfaces are sealed in future generations.
The interim evaluation report [Citation8] about CSG in 2012 – i.e. 4 years after the CSG was implemented – showed that the caries experience in children in the settlements was higher than in towns. The analyses in the present report indicate that this trend is continuing. This may be related to the fact that the dental personnel only have the resources at their disposal to visit the settlements once a year, and therefore do not maintain as close contact with these populations as with the towns. The results from the settlements had a negative impact on the overall achievement. The question of how to improve the implementation of the CSG in the settlements has been discussed at each annual meeting, but the results show that there is still room for improvement. The fluoride rinsing programmes will probably reduce the incidence of caries, also for children living in settlements[Citation20].
For adults, the dental healthcare available in Greenland has for a long time primarily focused on pain relief and treating symptoms. However, since 2013 the PDHS-G has opened up for the possibility that well motivated 16–20-year olds could also receive dental care. These initiatives could explain why the cost of running the PDHS-G has increased slightly from 2008 to 2018.
A relevant question is: Can some of the experience from the present study be used in other parts of the Arctic region and with a positive effect? Our data shows that native, skilled and motivated dental hygienists and dental assistants, corresponding to dental nurses, can promote dental health successfully in Greenland under suboptimal conditions for controlling dental caries. Thus, it might also be possible for local dental hygienists/dental nurses in other circumpolar areas to improve the caries situation locally. Further, motivation visits in the first three years of a child’s life aimed at providing information on good oral habits to the parents in Greenland also seem to promote dental health successfully. Thus, in this study, we were faced with the fact that about 50% of the 6-year olds had a defs = 0 in 2015 and 2018 versus 25% in 2008. This also meant that fewer teeth were extracted due to caries in the 6-year olds in 2015 and 2018 versus 2008. This eventually reduced the need for orthodontic treatment. Information about healthy diet, breastfeeding guidelines and instructions on how to brush teeth with fluoridated toothpaste is essential in order for parents to be able to prevent their children from suffering dental caries. In Greenland, the staff in the Public Dental Health Service performed this work, but some information could be provided to parents in connection with the growth and vaccine programmes which the individual counties are using for their child populations.
In conclusion, the present results show that a systematic approach to non-operative caries management performed in close collaboration with highly motivated dental staff and researchers can successfully improve the dental health status of children and adolescents in a country facing great structural challenges, high caries prevalence and which lacks natural fluoride in its water supply. The cost of running the PDHS-G increased by 4% from 2008 to 2018; some of this 4% increase can be explained by the new tasks (e.g. some 16–20-year olds are included in the PDHS-G) being performed by the PDHS-G, while the remainder probably can be attributed to the CSG.
Acknowledgments
The authors gratefully acknowledge all staff members of the Public Dental Health Service in Greenland for their commitment and enthusiastic persistence in the implementation of the Caries Strategy Greenland, CSG.
We also acknowledge the former head of Agency for Health and Prevention, Kalaallit Nunaat, chief dentist Dr Frank Senderowitz who initiated CSG and significantly contributed to the success of the program with his continuing care for the dental health in Greenland. His successors, chief dentist Dr Olina Hansen and chief dentist Lone Mahnfeldt, are acknowledged for their contribution of data concerning staff and economy. Former chief dental officer in Nexö municipality, Denmark, Dr Christian ME Christiansen, and former dentist in Nexö municipality, Dr Jette Christiansen, both associated with the Dental School of Copenhagen, are acknowledged for their significant contribution to CSG, for their great enthusiasm in the ongoing process of optimizing the program in close collaboration with the dental staff, and for their significant contribution at the annual workshops.
Disclosure statement
No potential conflict of interest was reported by the authors.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Friis-Hasché E. Child oral health care in Denmark. Copenhagen: Copenhagen University Press; 1994.
- Danish National Board Health. Available from: http://sundhedsstyrelsen.dk/da/sundhed/tandpleje/tandsundhed/boern-0-18- aar/15-aarige
- Ekstrand KR, Christiansen MEC, Qvist V. The influence of different variables on the inter-municipality variation in caries experience in Danish adolescents. Caries Res. 2003;37(2):130–9.
- Ekstrand KR, Christiansen ME, Qvist V, et al. Factors associated with inter-municipality differences in dental caries experience among Danish adolescents. An ecological study. Community Dentistry and Oral Epidemiology. 2010;38(1):29–42.
- Petersen PE, Bøge Christensen L. Dental health status and development trends among children and adolescents in Greenland. Int J Circumpolar Health. 2006;65:35–44.
- Gorbatova MA, Gorbatova LN, Grjibovski AM. Dental caries experience among 15-year-old adolescents in north-west Russia. Int J Circumpolar Health. 2011;70:232–235.
- Ekstrand KR, Christiansen ME. Outcomes of a non-operative caries treatment programme for children and adolescents. Caries Res. 2005;39:455–467.
- Ekstrand KR, Qvist V. The impact of a national caries strategy in Greenland after 4 years. Int J Paediatr Dent. 2015;25:255–266.
- Fejerskov O, Thylstrup A, Larsen MJ. Rational use of fluids in caries prevention. A concept based on possible cariostatic mechanisms. Acta Odontol Scand. 1981;39:241–249.
- Splieth CH, Ekstrand KR, Alkilzy M, et al. Sealants in dentistry; outcomes of the ORCA Saturday afternoon symposium 2007. Caries Res. 2010;44:3–13.
- Carvalho JC, Ekstrand KR, Thylstrup A. Dental plaque and caries on occlusal surfaces of first permanent molars in relation to stage of eruption. J Dent Res. 1989;68:773–779.
- Ekstrand KR. How to maintain sound teeth: an individualized population strategy for children and adolescents. In: Meyer-Lueckel H, Paris S, Ekstrand KR, editors. Caries management – science and clinical practice. New York: Thieme; 2013. p. 306–310.
- Bruun C, Thylstrup A. Dentifrice usage among Danish children. J Dent Res. 1988;67:1114–1117.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174.
- Petrie A, Sabin C. Medical Statistics at a glance. 3rd ed. West Sussex, UK: Willey Blackwell; 2009.
- Iheozor‐Ejiofor Z, Worthington HV, Walsh T, et al. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2015;(6). Art. No.: CD010856. DOI:https://doi.org/10.1002/14651858.CD010856.pub2.
- Marthaler TM, Petersen PE. Salt fluoridation–an alternative in automatic prevention of dental caries. Int Dent J. 2005;55:351–358.
- Bakhshandeh A, Derawi B, Twetman S, et al. Effekten og virkningsmekanismen af saltfluoridering på caries: en oversigts artikel. Tandlægebladet. 2008;112:784–794. English abstract.
- Meyer-Lueckle H, Satzinger T, Kielbassa AM. Caries prevalence among 6-16-year-old students in Jamaica 12 years after the introduction of salt fluoridation. Caries Res. 2002;36:170–173.
- Marinho VC, Chong LY, Worthington HV, et al. Fluoride mouthrinses for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2016;29:7(jul):CD002284.