ABSTRACT
Deleterious effect of cold on overall mortality is well-established. We studied associations between the air temperature and the number f ambulance calls for asthma in Nur-Sultan, Kazakhstan – the second coldest capital in the world. Daily counts of ambulance calls for asthma in Nur-Sultan for the cold seasons (October-March) 2006–2010 were obtained from the Municipal Ambulance Station. Associations between the number of calls and mean and minimum apparent temperatures (average for lags 0–15) were studied using first-order Poisson auto-regression models controlling for wind speed and effects of month, year, weekends and holidays. Altogether, there were 7373 ambulance calls for asthma during the study period. An inverse association between minimum apparent temperature and the number of calls was observed for the age-group 60 years and older. A decrease of the minimum apparent temperature by 1°C was associated with an increase in the number of calls by 1.7% (95% CI: 0.1%-3.3%) across the whole temperature spectrum. No associations in other age groups were found. Our results suggest an inverse association between the average 15-day lag minimum apparent temperature and the number of ambulance calls during the cold season in Nur-Sultan, but this is limited to the oldest age-group.
Introduction
Earlier research has shown that climate, and specifically low temperatures, is an important independent determinant of health [Citation1]. Deleterious effect of cold on respiratory mortality is well-established: approximately a half of excess mortality during winter months is attributed to deaths from respiratory causes [Citation2]. Moreover, exposure to cold air is known to exacerbate chronic inflammatory airway diseases including asthma [Citation3]. More than two-thirds of Finnish adults with asthma report cold-related respiratory symptoms, the symptoms, but they start to emerge at relatively cold temperatures and with a temperature threshold increasing by age [Citation4]. In New Zealand, respiratory hospital admissions have been shown to be strongly associated with minimum temperatures during winter with the increase in hospitalisations when temperature falls below 8°C. As in the Finnish study, the greatest increase has been observed among the elders [Citation5]. Other studies have reported an increase in respiratory hospital admissions in cold days among children [Citation6], while other studies suggest that this association is limited only to adults [Citation7]. At the same time, Fitzgerald et al. have reported on a nearly 5% decrease in asthma admissions during cold spells in New York State with a decline being the strongest in the coldest regions [Citation8]. Winter and low latitude had a statistically significant association with the increased risk of asthma, especially in children and low-latitude areas in a recent meta-analysis [Citation9].
Thus, the results on the associations between cold temperature and asthma exacerbations vary between the settings and across age-groups warranting further research in different settings.
Most of the studies on the associations between climatic factors and asthma have been performed in high income countries with temperate or subtropical climate complicating generalisation of the findings and warranting replication of the results in other parts of the world, particularly in developing settings where low temperatures are not uncommon.
The capital of Kazakhstan – Nur-Sultan (Astana until 2019) – is located in the steppe region on the border between a humid continental and a semi-arid climate [Citation10]. Although located in Central Asia, the city has much in common with inland settings in the Arctic, particularly in Siberia. Winters are long and temperatures below –30°C are common. However, the size of the city is much greater (834000 in 2014) comparable to the Arctic settings making it a unique setting for exploring effects of climatic factors on various health outcomes [Citation11–13]. Information on respiratory health in Kazakhstan in international peer-reviewed literature is scarce. The only study on the prevalence of asthma we identified in Pubmed suggests that 1.9% of residents of Nur-Sultan had “doctor-diagnosed asthma” and 25.5% had wheezing symptoms in 2018 [Citation14].
The aim of this study is to assess associations between air temperature and daily counts of ambulance calls for asthma during cold season in Nur-Sultan, Kazakhstan – the coldest capital city in the European WHO region and the second coldest capital in the world.
Methods
This was an ecological study using aggregated data on daily counts of ambulance calls for doctor-diagnosed asthma during the cold seasons (from October 1 through March 31) 2006–2010. This six months period was selected to ensure comparability with other studies on the associations between climatic factors and health outcomes. Mean and minimum apparent temperatures were calculated using the formula AT = −2.653 + 0.994*T + 0.0153*DT2 where T is the mean or the minimum daily temperature, respectively, and DT is the dew point temperature [Citation15]. Apparent temperatures represent discomfort indices and are more appropriate for studies on the effects of cold since they combine the effect of temperature and humidity. However, we also repeated all analyses using mean and minimum daily temperatures. Data on temperature, humidity and wind speed were obtained from the Kazakhstani Hydrometerological Service (Kazhydromet). The meteorological station is located close to the geographical centre of the Nur-Sultan municipality; therefore, we assume that the data effectively represent the temperature in the city.
The daily counts of ambulance calls for asthma were used as dependent variables. The data were obtained from the Municipal Ambulance Station. Diagnosis of asthma by ambulance doctor was based on a prior diagnosis of asthma and physical exam finding of wheezing or improvement with short-acting beta agonist.
An exploratory analysis using the countfit estimation function in Stata software revealed that the Poisson distribution provided the best fit for the data [Citation16]. In addition, analysis of autocorrelations and partial autocorrelations of dependent variables showed the first-order autocorrelation. Robust standard errors were used to account for heterogeneity [Citation16]. We also modelled curvilinear relationships between temperature and outcomes by fitting cubic splines with knots spaced every 5°C using uvrs function in Stata [Citation17] and searched for a threshold value for the temperature using ”hockey-stick” models [Citation17]. However, the most parsimonious model describing relationship between the temperature and the number of calls was linear across the whole temperature spectrum during the study period. Thus, first-order autoregressive Poisson regression was used to assess the effect of temperature on daily counts of calls. The effect of cold on health outcomes [Citation1,Citation18], including asthma [Citation19], can be delayed for up to two weeks, so we used average temperature values for lags 0–15 days. Also, wind speed with 0 lag was included in the models as a continuous variable. Months, years and public holidays were included in the models as binary variables.
All analyses were performed using the Stata 10.0 software (Stata Corp., TX, USA).
Results
Mean daily temperature varied between −36.2°C to 18.4°C during the study period. The corresponding numbers for minimum temperature were −39.7°C and 12.8°C. Altogether, there were 7373 ambulance calls for asthma during the study period. The number of calls across independent variables is presented in . Out of them, 51.3% were among men. The daily counts of ambulance calls for asthma varied between 0 and 21 with the median of 8 calls per day. Calculation of average temperatures for lag 0–15 days resulted in reduction in the number of days included in the analyses and in the overall number of cases to 7355.
Table 1. Background characteristics of the study population and average values for air temperatures during the cold seasons 2006–2010 in Nur-Sultan, Kazakhstan
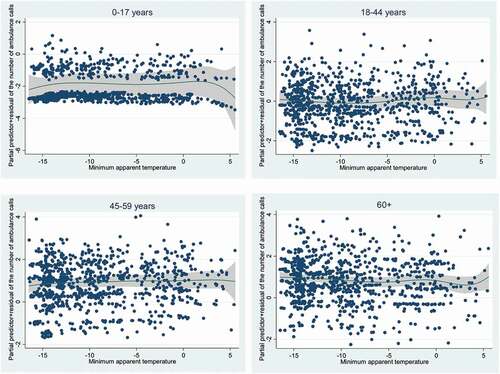
Associations between the number of calls and either mean or minimum temperatures did not reach the level of statistical significance (). Significant association between the temperature and the number of calls was observed only for the oldest age-group: the number of calls increased on average by 1.7% (95% CI: 0.1–3.3) for each 1°C decrease in minimum apparent temperature in multivariable autoregressive models (). Results of regression modelling were also presented graphically in .
Table 2. Association between mean- and minimum temperature and daily counts of ambulance calls for asthma during the cold seasons 2006–2010 in Nur-Sultan, Kazakhstan
Table 3. Association between mean- and minimum apparent temperature and daily counts of ambulance calls for asthma during the cold seasons 2006–2010 in Nur-Sultan, Kazakhstan
Discussion
This is to the best of our knowledge the first study from Central Asia on the association between air temperature and asthma exacerbations. We found an inverse association between temperature and ambulance calls for asthma in the cold season, but only among the oldest age-group.
The main strength of the study is that we included all served ambulance calls during cold seasons from 2006 to 2010. There in only one ambulance station in the city and the use of all calls in the city in the given period minimises both random error and selection bias. Relatively large sample size provides an opportunity to assess relatively small variations in the number of ambulance calls across the whole range of temperatures.
Our results are in line with the consensus that elderly are the most vulnerable to the effects of cold [Citation1]. Cold temperatures and low humidity were shown to be associated with respiratory infections in Finland [Citation20]. Cooling of the air to 10°C during exercise and to −17°C during resting is associated with bronchospasm in asthmatic subjects which may partly explain our findings [Citation21]. However, it has been suggested that it is facial cooling but not breathing of cold air induces bronchoconstriction [Citation22]. Cooling of bronchi by cold air slows ciliary movement and induces local inflammatory responses [Citation23]. Thus, an infectious pathway of asthma exacerbations associated with cold temperatures cannot be excluded.
However, contrary to the findings from many other studies, we have not observed associations between temperature and asthma exacerbations among children, young-, and middle-aged adults [Citation3,Citation6,Citation7,Citation24]. The absence of association for younger age groups in this study is highly likely to be due to limited statistical power. One may also speculate that parents of children in Nur-Sultan may be less likely to rely on ambulance services and instead transport their children to emergency departments using personal vehicles. Another potential explanation is that children can stay at home instead of going to schools or kindergartens during days with low temperatures. This reduces exposure to cold and may prevent asthma symptoms.
Similarly, cold temperatures were not associated with either cardiovascular or cerebrovascular mortality in Nur-Sultan [Citation25]. In Europe, the effect of cold is known to be less pronounced in locations with lower average temperatures [Citation15]. Given that Nur-Sultan is the coldest capital in the European WHO region one may expect less pronounced effects of cold on health outcomes than in other European settings. This hypothesis is further supported by the findings from Yakutsk, North-Eastern Russia, where winter temperatures during cold season are even more extreme than in Nur-Sultan. Both settings have low humidity suggesting that our results should be generalised with due caution to areas with less continental climates and with higher winter temperatures. Donaldson et al found no association between air temperature and mortality with the exception for some increase in the number of deaths from respiratory causes [Citation23]. Nur-Sultan is a rapidly developing capital of the oil rich Kazakhstan, where adaptive capacities to harsh climatic conditions are in place with well-established warning system, modern housing, central heating arrangement with the indoor temperature kept between 20 and 24°C in most of the apartments and good public transport infrastructure. A culture of putting fur or feather cloths and hats when going outdoors in winter was proposed as one of the explanations of limited associations between cold and health outcomes in Yakutsk [Citation23], which is also relevant for our setting.
Nevertheless, the results should be interpreted with caution taking into consideration potential limitations of the study. As a dependent value we used the number of asthma exacerbation diagnoses set by the medical doctor who served the ambulance call and visited the patient leaving a chance for misclassification bias. However, even if this is the case, measurement bias is unlikely to vary across the temperatures and thus can be considered as non-differential. Non-differential bias is associated with less precision and wider confidence intervals. Another limitation of the study is lack of data about asthma characteristics given heterogeneity of the condition. The effects of temperature extremes are likely to be more pronounced among the most vulnerable groups. This corresponds with our results suggesting that the effect of temperature on asthma exacerbation in Nur-Sultan is restricted to the oldest age-group. At the same time the only results that reached the level of statistical significance were obtained in the largest age-group. Therefore, this association should be interpreted with caution. Individual data were not available for this study, so we could not test the hypothesis on variations of the effects of temperature on the outcome across socio-economic strata or asthma types.
Air pollution, particularly levels of NO2 and SO2 during winter season, was also shown to be associated with the risk of exacerbations of asthma [Citation26] but not in all studies [Citation27]. Nevertheless, a recent systematic review and meta-analysis has demonstrated clear association between the number of alsthma-related ambulance dispatches and NO2 [Citation28]. We did not have access to the data on pollutants in Nur-Sultan during study period, therefore the confounding effect of air pollution cannot be excluded. Given that this is an ecological study with limitations by design [Citation29] further research should be performed on an individual level and directed at studying the factors behind the observed association for further development of strategies directed at mitigation of the effects of cold on population health in urban settings of Central Asia.
Conclusions
In agreement with the findings from other settings, the results suggest an inverse association between the average 15-day lag minimum apparent temperature and the number of ambulance calls during the cold season but in Nur-Sultan this effect seems to be restricted to the oldest age-group.
Acknowledgments
This publication has been developed within the WHO/BMUB project on protecting health from the climate change in Europe, coordinated by Dr. Bettina Menne, WHO Regional Office for Europe. The authors are grateful for the financial support received from Germany.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Young TK, Mäkinen TM. The health of Arctic populations: does cold matter? Am J Hum Biol. 2010;22(1):129–6.
- Keatinge WR. Winter mortality and its causes. Int J Circumpol Health. 2002;61(4):292–299.
- Ellis EF. Asthma in childhood. J Allergy Clin Immunol. 1983;72(5):526–539.
- Harju T, Mäkinen T, Näyhä S, et al. Cold-related respiratory symptoms in the general population. Clin Respir J. 2010;4(3):176–185.
- Gosai A, Salinger J, Dirks K. Climate and respiratory disease in Auckland, New Zealand. Aust NZ J Public Health. 2009;33(6):521–526.
- Xu Z, Huang C, Hu W, et al. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med. 2013;70(10):730–735.
- Abe T, Tokuda Y, Ohde S, et al. The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emerg Med. 2009;27(2):153–159.
- Fitzgerald E, Pantea C, Lin S. Cold spells and the risk of hospitalization for asthma: New York, USA 1991-2006. Lung. 2014;192(6):947–954.
- Cong X, Xu X, Zhang Y, et al. Temperature drop and the risk of asthma: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2017;24(28):22535–22546.
- Peel MC, Finlayson B, McMahon TA. Updated world map of the Köppen-Geiger climate classification. Hydrol Earth Syst Sci. 2007;11(5):1633–1644.
- Grjibovski AM, Nurgaliyeva N, Kosbayeva A, et al. Effect of high temperatures on daily counts of mortality from diseases of circulatory system in Astana, Kazakhstan. Medicina (Lithiania). 2012;48:640–646.
- Grjibovski AM, Kozhakhmetova G, Kosbayeva A, et al. Associations between air temperature and daily suicide counts in Astana, Kazakhstan. Medicina (Lithuania). 2013;49:379–385.
- Grjibovski AM, Kosbayeva A, Menne B. The effect of ambient air temperature and precipitation on monthly counts of salmonellosis in four regions of Kazakhstan, Central Asia, in 2000-2010. Epidemiol Infect. 2014;142(3):608–615.
- Nugmanova D, Sokolova L, Feshchenko Y, et al. The prevalence, burden and risk factors associated with bronchial asthma in commonwealth of independent states countries (Ukraine, Kazakhstan and Azerbaijan): results of the CORE study. BMC Pulm Med. 2018;18(1):110.
- Analitis A, Katsouyanni K, Biggeri A, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168(12):1397–1408.
- Long S, Freese J. Regression models for categorical dependent variables using Stata. Texas, USA: Stata Corp; 2006. p. 527.
- Royston P, Sauerbrei W. Multivariable modelling with cubic regression splines: a principled approach. Stat J. 2007;7:45‑70.
- Yang J, Ou C-Q, Ding Y, et al. Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environ Health. 2012;11(1):1–9.
- Zhang Y, Peng L, Kan H, et al. Effects of meteorological factors on daily hospital admissions for asthma in adults: a time-series analysis. PLoS One. 2014 14;9(7):e102475.
- Mäkinen TM, Juvonen R, Jokelainen J, et al. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir Med. 2009;103(3):456–462.
- Eschenbacher WL, Moore TB, Lorenzen TJ, et al. Pulmonary responses of asthmatic and normal subjects to different temperature and humidity conditions in an environmental chamber. Lung. 1992;170(1):51–62.
- Koskela H, Tukiainen H. Facial cooling but not breathing of cold air induces bronchoconstriction: a study in asthmatic and healthy subjects. Eur Respir J. 1995;8(12):2088–2093.
- Donaldson GC, Ermakov SP, Komarov YM, et al. Cold related mortalities and protection against cold in Yakutsk, Eastern Siberia: observation and interview study. BMJ. 1998;317(7164):978–982.
- Mireku N, Wang Y, Ager J, et al. Changes in weather and the effects on pediatric asthma exacerbations. Ann Allergy Asthma Immunol. 2009;103:220–224.
- Grjibovski AM, Nurgaliyeva N, Kosbayeva A, et al. No association between temperature and deaths from cardiovascular and cerebrovascular diseases during the cold season in Astana, Kazakhstan – the second coldest capital in the world. Int J Circumpol Health. 2012;71(1):19769.
- Kim S, Kim Y, Lee MR, et al. Winter season temperature drops and sulfur dioxide levels effect on exacerbation of refractory asthma in South Korea: a time-trend controlled case-crossover study using Soonchunhyang asthma cohort data. J Asthma. 2012;49(7):679–687.
- Toshikazu A, Tokuda A, Ohde S, et al. The relationship of short-term air pollution and weather to ED visits for asthma in Japan. Am J Emergency Med. 2009;27(2):153–159.
- Sangkharat K, Fisher P, Thomas GN, et al. The impact of air pollutants on ambulance dispatches: a systematic review and meta-analysis of acute effects. Environ Pollut. 2019;254(Pt A):112769.
- Kholmatova KK, Grjibovski AM, Kholmatova KK, et al. Ecological studies in medicine and public health. Ekologiya Cheloveka (Human Ecology). 2016;9:57–64.