ABSTRACT
People living in rural Iceland have a higher rate of cardiovascular risk factors and healthcare utilisation compared to people in urban areas.
The aim of this qualitative study was to explore the experiences of people with coronary heart disease, living in rural Iceland regarding patient education, surveillance, and self-care support. The participants (N = 14, age 52‒79 years, 8 male), were interviewed 6 to 12 months after hospital discharge following a cardiac event (in 2018‒2019). Systematic text-condensation was used for analysis. The findings were categorised into three main themes: Education and support describes inadequate patient education and support from health-care professionals after discharge from hospitaland how the internet was the main information source supplemented with spouse’s and family support. Local healthcare services describe thelack of and importance of access to health-care professionals, stable services, and underutilisation of telemedicine and primary healthcare in the local area, and Self-care behaviour describes the lack of professional support with lifestyle changes and how the participants manage self-care as well as their attitudes towards the disease.
The results indicate that access to continuous healthcare services and person-centred support focusing on prevention strategies are widely impaired in rural areas in Iceland.
Introduction
Coronary heart disease (CHD) is a chronic condition and the leading cause of death globally (World Health Organization, n.d.) [Citation1] as well as the most common cause of premature death (<70 years) in Iceland [Citation2] and overall in Europe [Citation3]. The major causes of CHD are unpreventable factors such as age, gender, and heredity, alongside preventable factors such as smoking, diet, physical inactivity, and obesity.
In the Arctic, indigenous populations have been genetically protected from atherosclerosis [Citation4], but deviation in recent decades from traditional lifestyle and dietary practices and the influences of modern civilisation and urbanisation has caused an increase in CHD [Citation5]. The mortality rates due to CHD in Iceland have decreased considerably in recent years due to reduced risk factors, particularly smoking and unfavourable blood lipid levels [Citation6]. However, as in other European countries [Citation3], the CHD mortality rate is predicted to increase in the coming years due to the increased prevalence of diabetes and obesity [Citation7].
Myocardial infarction (MI) accounts for most of deaths caused by CHD [Citation3]. A large part of the Icelandic population lives in remote areas where long transport time makes it rare and difficult [Citation8] to reach the recommended 120 minute timeframe for the optimal treatment, percutaneous coronary intervention (PCI) [Citation9]. Following discharge from the hospital, comprehensive cardiac rehabilitation, an effective method to successful behavioural change [Citation10] using evidence-based methods (such as patient education and motivational interviewing), is also rarely available locally in rural Iceland. People in rural Iceland, where specialised health services are limited or lacking, have been shown to evaluate their health as worse than people living in the capital area where diverse specialised services are available [Citation11]. The mortality rates due to CHD have also been shown to be significantly higher among women living in rural Iceland than among women living in the capital area. Registered contacts with health care services due to CHD, the number of discharges from hospitals, and risk factor levels were also significantly higher in rural areas, especially among women [Citation12]. Similar findings have been reported in Australia [Citation13], Europe [Citation14,Citation15], and North America [Citation16], where regional differences in people’s health, risk factors, and mortality rates due to heart diseases have been noted. Also, in the northern areas of Sweden, rural inhabitants were more likely to have higher blood lipids and more central fat than people in urban areas of northern Sweden [Citation17].
The treatment of symptoms and the control of complications can reduce CHD mortality and recurrent events [Citation18]. However, despite clear clinical guidelines on treatment [Citation9] and secondary prevention of CHD [Citation10], research continues to show that most European patients with CHD do not reach the desired treatment goals or risk factor levels [Citation19,Citation20]. This may partly be explained by insufficient self-care, i.e. the process of maintaining health through health-promoting practices and managing illness [Citation21] but self-care has three key concepts according to Riegel et al., (2012) Citation21, i.e. self-care maintenance, self-care monitoring, and self-care management and is influenced by several factors including access to healthcare.
An important aspect of self-care management is deciding when to seek emergency treatment. Studies have demonstrated that delays in emergency treatment are affected by the time the patient takes to decide whether to contact healthcare services. However, good patient education can shorten that time [Citation22], making proper healthcare and patient education even more important in remote Arctic areas, such as rural Iceland, where travel time in acute situations is long [Citation8]. Effective self-care management begins by patient-education and involvement at the hospital, preferable with the family present. This can be a challenge for families living in rural areas far away from the hospitals. A qualitative study from Greenland on patient involvement described how the patients felt like guests in the foreign hospital environment and found it difficult to be far from home without relatives and friends during the time of illness [Citation23]. Returning home can be a challenge for people with complex chronic diseases living far from the hospital. Participants in rural areas experienced the feeling of isolation or being left alone in their recovery after MI according a study from Canada [Citation24] and a systematic review of qualitative meta-synthesis [Citation25] showed that individuals with chronic illness in rural areas experienced difficulties in accessing healthcare services due to weather and transport, while the provision of local services and social support helped to overcome these obstacles. Limited access to healthcare services in the local area can cause difficulties for people living in rural areas. Brundisini et.al (2013)Citation25, showed that feelings of vulnerability increased if health-care professionals were of limited availability and patients appreciated being able to form long-lasting, personal relationships with health-care professionals.
Few studies were found that describe the experiences of people with CHD in rural areas, despite the increasing disparities in CHD-mortality between urban and rural areas [Citation16] and little is known about the experience of people living with chronic diseases and their self-care in rural Iceland. Therefore, the aim of the study was to explore the experiences of people living with CHD in rural Iceland regarding patient education, surveillance, and self-care support.
Methods
This study utilised a descriptive qualitative method based on Giorgi’s descriptive phenomenology [Citation26], which is appropriate when the purpose is to obtain detailed descriptions of a phenomenon about which little is known [Citation27]. Semi-structured individual interviews with 14 CHD patients living in rural Iceland were conducted from 2018 to 2019. The research team comprised three registered nurses, all females. The first author (ThBJ) has extensive experience in primary care nursing in a remote area of East Iceland and the co-authors (BI & MHS) are experienced clinical nurses within cardiac care and patient education. The second author´s personal and clinical experiences are mainly from urban areas, while the third author´s experience is from both urban and rural areas. Both authors (BI & MHS) have substantial experience in qualitative research. In their clinical practice, the authors observed the sparse resources available to patients in rural Iceland, the lack of patient education and rehabilitation following discharge from the hospital and the lack of continuity in healthcare services which raised an interest in exploring the patients’ experiences.
Setting
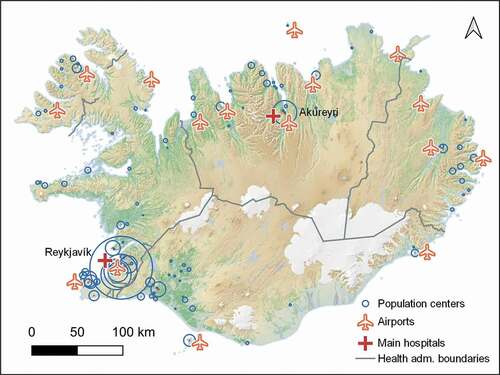
Iceland is a rural country with a population of 365,000 and its own language, Icelandic. The majority (63%) of the population lives in the Greater Reykjavík region in southwestern Iceland and about 5% live in Akureyri, the second largest urban district. Landspitali, – the National University Hospital in Reykjavík is the country’s only hospital performing specialised cardiac procedures, such as PCI and coronary artery bypass graft (CABG). Akureyri Hospital provides emergency services for the northern part of the country and is the air ambulance centre for Iceland. In emergency situations such as MI, people in a large part of the country depend on air ambulances. Comprehensive inpatient cardiac rehabilitation is offered in one rehabilitation centre in the Greater Reykjavík region and comprises physical training, patient education, lifestyle counselling, and psychosocial support. In addition, some centres offer general rehabilitation and outpatient cardiac rehabilitation, but mostly in urban areas.
Primary healthcare centres are in most villages in Iceland. However, some are sparsely staffed, and the role of health-care professionals is often quite broad, providing acute service, primary care and health promotion. In recent years, the optimisation of services and specialisation has led to the migration of health-care professionals to urban areas, resulting in increased travelling distances to specialised services for people living in rural Iceland. Hence, recent goals have been set to create a more structured and person-centred system with a suitable service level and increased implementation of telemedicine and ambulance transport [Citation28]. Over 95% of the Icelandic population has access to the Internet [Citation29], a fact that could ease the implementation of digital solutions and telemedicine and reduce the effect of long distances to hospitals and specialised healthcare services for half of the Icelandic population.
presents the distribution of towns and villages, health administration boundaries, primary airports, and the two main hospitals in Reykjavik and Akureyri.
Participants and recruitment
This is a sub-study of the quantitative study, “The Icelandic KRANS-study: Lifestyle, Risk Factors, and Self-Care of Individuals with Coronary Heart Disease” [Citation30]. The inclusion criteria for the KRANS-study were a hospital admission du to CHD, fluency in Icelandic (orally and written), the ability to answer questionnaires, and to be aged 18 to 79 years. A purposive sample was drawn from the KRANS-study, with the additional inclusion criteria of participants living 150 kilometres or more from either of the country’s two main hospitals in Reykjavik and Akureyri. Patient recruitment was continued until the data was considered sufficient to accomplish the study aim and saturation was reached. A total of 47 patients fulfilled the criteria, and 32 of them were sent invitations to participate. Of those, participants were selected by diversity in distributional location, gender, and age; 18 were contacted by phone, and 14 agreed to participate. None of the researchers knew the participants personally or professionally.
Data collection
The interview guide was constructed based on a review of the theoretical literature [Citation12–14,Citation25], clinical guidelines, the authors´ clinical experiences and pre-interviews with three individuals who lived with CHD in rural Iceland. Those pre-interviews yielded important information regarding the possible challenges in the daily lives of rural patients. Subsequently, the initial interview guide was discussed and further developed alongside a multi-professional team of researchers at the University of Akureyri. Data was collected from individuals in face-to-face semi-structured interviews with each participant from September 2018 to July 2019. Background and clinical variables were retrieved from the database of the KRANS-study[Citation30]. The main questions in the interview guide are presented in .
Table 1. Main questions in the interview guide
The interviews were conducted by all the authors, the first 10 by ThBJ, one by MHS, and three by BI. Interviews were conducted in Icelandic. The time and locations of the interviews were chosen by the participants, and all but three were conducted at their homes in privacy. Possible bias and pre-assumptions of the researchers were discussed, reflected on, and documented beforehand. After each interview, the interview guide was reviewed, and minor changes were made. Interviews were recorded digitally and transcribed verbatim. The average time of the interviews was 30 minutes (19‒53 minutes).
Data analysis
NVIVO’s 11 data processing software [Citation31] was used to structure and thematise the interview data; analytical models were configured in the MindNode mindmapping app [Citation32]. Data analysis was inductive and performed continually using systematic text condensation [Citation33] in the following four steps:
Total impression: From chaos to themes. In this step, the manuscripts were read thoroughly to gain a general first impression and find the whole meaning of the participants´ descriptions. Afterwards, the researchers reflected on possible preliminary themes.
Identifying and sorting meaning units: From themes to codes. In this step the researchers identified and organised text elements or units of meaning that could elucidate the research question. The units of meaning were identified, coded and sorted into themes.
Condensation: From code to meaning. In this step, the researchers systematically abstracted the meaning units, reduced the code groups to a few groups, and condensed the text, maintaining the participant´s original terminology as far as possible.
Synthesising: From condensation to descriptions and concepts. In this step, the data were reconceptualised, ensuring that the disconnected text elements still reflected the original context. Subsequently, the researchers adopted the role of a re-narrator, writing a story about the phenomenon grounded in the original data. The original transcripts were then read again to search for data that could challenge the researchers’ group conclusions [Citation33].
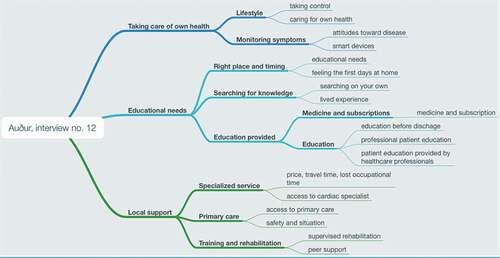
Examples of the analytical process can be seen in .
Table 2. The analytical process with examples
Throughout the interviews, reassurance and a proper understanding of meanings were discussed continually with the participants. An individual analytical model was developed for each interview (see example in ), followed by a complete analysis model with codes. Analysis was conducted simultaneously with the interviews but researchers took a good time to the analysis process and “lived with the data”. To establish an overview of data, the transcribed interviews were carefully read by all the researchers, a practice that was repeated throughout the analysis. All authors were active in the analytical process and discussed their preconceptions, codes and the analytical models as well as data saturation and the need for additions or changes in the interview guide. The results were reflected on and discussed during regular meetings among the research team as well as debriefed and discussed in a seminar with colleagues. The decision trail was carefully documented throughout the analysis.
Ethical considerations
This study fulfils the conditions of the Helsinki Declaration [Citation34] and was approved by the National Bioethics Committee in Iceland (VSN-18-116). Participants were given both oral and written information and signed a written consent form. Each participant was assigned a pseudonym that is used in the following description of the results.
Results
Fourteen individuals participated in the study. They lived in South Iceland (n = 2), West Iceland (n = 2), West Fjords (n = 2), North Iceland (n = 6), and East Iceland (n = 2). Their mean age was 67 years (SD 9.0). Ten of the participants had been admitted to the hospital for acute PCI at the time of enrolment in the KRANS-study, and four were admitted for elective PCI or CABG. A more detailed description of the participants is presented in .
Table 3. Characteristics of the participants
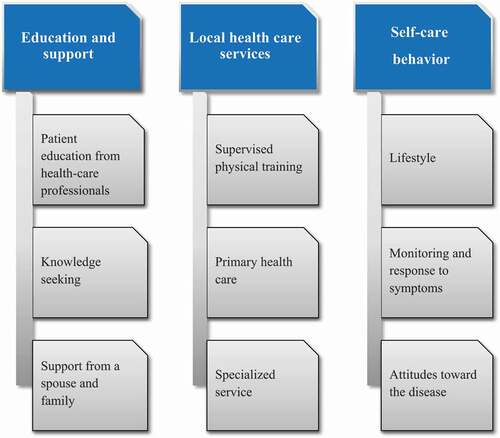
Data analysis of the interviews revealed three main themes and three subthemes that describe the patients’ experience of patient education, surveillance, and self-care support after hospitalisation for CHD. The three main themes were education and support, local health care services, and self-care behaviour. The main themes and subthemes are shown in .
Education and support
All the participants said they had received patient education before discharge but did not recall the content easily. Those who did not participate in cardiac rehabilitation reported limited patient education and instructions from health-care professionals following discharge from the hospital, and that this service was not available in their local areas. Patient education provided by health-care professionals, how participants sought CHD-related knowledge, and participants´ experiences of support from spouses and family are described in the three following subthemes.
Patient education from health-care professionals
All participants reported receiving some information about their treatment and what to expect before discharge from the hospital. However, they had trouble comprehending all the information they received. Many participants, especially those unaccompanied by a spouse or family member, also had considerable trouble remembering oral instructions. Written or visual information, such as that from videos, seemed to be better recalled. One patient said the following:
You get information and you may not be ready to receive it. You know, there is so much going on before an operation […] you are not quite ready to […] store information, it is like you forget it (Gunna, 69- year-old woman).
Participants expressed a need for further patient education from health-care professionals after discharge from the hospital, especially during the first days, which was not offered in their local area. Those who had attended cardiac rehabilitation (four of the participants), said that they had received all the information they needed, as well as personal support regarding lifestyle changes. They said this helped them to cope with the disease. Others said they lacked personal support and information about physical exercise:
I think everyone who has the opportunity to go to Reykjalundur [rehabilitation center] should go there […] it’s just you get this kind of education about everything […] both mental and physical (Petur, 65- year-old man).
Knowledge seeking
The participants said that the brochures they received at the hospital proved useful after they returned home, and afterwards, some also sought information from the Internet. The women reported more frequent use of the Internet than men for knowledge seeking, where Google was the most popular starting point of searches. Sigga, a 52-year-old woman said, “I just Google something”. However, Icelandic websites were also named. Some of the older participants did not have access to a computer or were not capable of using it: “I just got a new computer, but […] I can’t start it up because, you know, I don´t know how to” (Gudmundur, 73-year-old-man). Talking to other people who had had similar experiences and hearing their stories was said to be helpful, educational, and emotionally supportive. Kari, a 74-year-old man said, “I like to listen to those men who had this before like about 10 years ago and are doing well […] then you are calmer yourself”.
Support from a spouse and family
The presence of a spouse in the hospital was demonstrated to be very helpful in receiving and remembering information that proved valuable after returning home. Oddur, a 77-year-old man, described it as follows:
She joined me in the air ambulance and everything […] and observed what happened […] then she visited daily, that was very good […] she has just followed me through this all the way.
Spousal support after returning home was described as an important factor. The wives often helped or participated in information–seeking, and many managed their spouses’ medication. The married female participants described the support from their spouse as being that of a partner in lifestyle changes and pursuing outdoor activities.
Local healthcare services
Continuous service and personal contact with healthcare professionals at the local healthcare centre were highly valued. Those who did not attend cardiac rehabilitation reported a lack of patient education and opportunities for supervised physical training in their local areas. Additionally, access to specialised healthcare was considered deficient by some participants.
Primary healthcare
Unstable and discontinuous service and the frequent rotation of general practitioners at the local healthcare centre were often mentioned as disadvantages of the current healthcare system: “The doctors are replaced every two weeks” (Sigurjon, 57- year-old man). The participants repeatedly stated that the number of health-care professionals in the area was dwindling and travel time for seeking necessary healthcare had increased in recent years. They found it considerably important to have personal contact with a physician or a nurse in the local area who knew them, but this was rarely the case. Oddur, a 77- year-old man, said, “I always found it better to just meet the same one […] He knows you, rather than going to someone new and then you have to explain it, you see […] all over again”. Vala, a 79-year-old woman, said, “I feel it is bad that there is no nurse employed here […] it might have an impact to have a nurse here […] a nurse […] that is better than nothing”.
The participants rarely used primary healthcare to seek support with lifestyle changes. Adda a 74- year-old woman explained, “well, there is maybe this physician this week and another next week […] No I haven´t gone there […] I’m sure there is something missing there [in the service]”.
Supervised physical training
Most of the participants said they needed support and guidance with physical training after returning home. However, a lack of physiotherapists or referrals was common. During the interviews, some described having tough days after hospital discharge and experienced reduced physical and mental health. They described an unfulfilled and urgent need for supervised training. Jon, who had previously been in good health, was discharged from the hospital after an acute MI, feeling exhausted and disabled when returning home. He was referred, in the middle of the winter, to a physiotherapist far away from his hometown, whom he was unable to visit due to the distance. Later, he discovered a supervised physical exercise group in his hometown, in which he participated and was highly satisfied. He reported the following:
I got a piece of paper that I could read about what, what was available and of course all of it was located in town X and X but it was not specified what was available here […] if it had been here, I would definitely have gone […]. But one is not going to drive for […] many hours for an hour of rehab twice a week (Jon, 73-year-old man).
Most of the participants had at some point attended some kind of training or physiotherapy in or around their hometown, while others had travelled long distances. Women complained more often than men about not being referred to the rehabilitation they needed after returning home. Sigga asked for training in her local area but did not receive the appropriate referral:
I was a bit confused about what I should do. Went to the physical therapist and asked if I should do any physical therapy, no, no, no. You know it was like that […] I really didn´t know what to do, so I just cycled and did what I used to do before (Sigga, 52-year-old woman).
The four participants who attended inpatient cardiac rehabilitation were very satisfied with the program, support, and patient education they received. They highly recommended this because it had helped them to recover and maintain their health in daily life. Two of them had attended further outpatient cardiac training in their local areas which supported continuous improvements towards better health, and they received further support from staff and other attendees. Those who did not attend cardiac rehabilitation had either not been referred, even though they asked for it, or did not accept it because of the long travel distance from their homes. Farmers found it particularly difficult to attend cardiac rehabilitation because of the distance and absence from the farm.
Specialised services
One participant explained how the villagers´ safety was threatened by a recent reduction in ambulance services, in addition to the long distance to the hospital and unstable weather. Of the six female participants, four had experienced delays in acute treatment because they felt they had not been heard and that their symptoms had not been diagnosed soon enough in their local area. However, in emergency situations, all the other participants, had experienced efficient transport and care. Ari had experienced an MI far from the tertiary hospital but had experienced safe transportation and professionalism in his hometown. He said, “the service here, the emergency service is good. This system works splendidly” (Ari, 54-year-old man).
Some patients benefited from a follow-up by a cardiologist visiting their local area, but most had to travel long distances (to Landspitali or Akureyri) for specialised cardiac follow-up, causing unforeseen costs and travelling time. This proved especially burdensome for those with multiple illnesses as reimbursement from health insurance for travel expenses did not cover the cost. Sigga, 52-year-old woman, reported the following:
We only get [reimbursement] for two trips each year […]. Which is ridiculous of course. Especially if you get something like […] you know I only have two trips […] a year […] and I used them a while ago.
The men were generally more satisfied with their visits to cardiologists and the check-ups they received, but some of the women felt the visits were too short and would have preferred more time to talk. Gunna, 69-year-old woman, mentioned that she travelled a long distance to Reykjavík for a cardiac consultation that only took 10 minutes: “You don’t know beforehand which questions to ask […] but if the physician gives you time and talks to you, the discussions often raise questions”.
Self-care behaviour
All the participants were aware of the importance of a healthy lifestyle and had tried to improve their lifestyles. Professional support and help were said to be lacking locally, but family and friends were important source of support. The use of technology to communicate with healthcare services to compensate for long distances to specialised care and to monitor symptoms was uncommon among participants.
Lifestyle
Most participants were aware that changes in their lifestyles would be beneficial to their health, and all of them had tried to improve their lifestyles. Almost all participants believed that they took better care of their health after their cardiac incidents and claimed to be in better health than before. Behavioural changes were made mainly without professional help or supervision but were often accompanied or supported by family members. Participants described how behaviour changes were easier if all family members participated, and couples often changed their lifestyles together.
Those who had quit or were trying to quit smoking considered it the most important change for their health. They received support and information at the rehabilitation program, from the Internet, or from family and peers. The participants saw daily outdoor physical exercise as an integral part of improving their health, and many reported doing so regularly, preferably with a partner or others, by hiking, cycling, or golfing. Erna, a 58- year-old woman stated that daily exercise and work helped: “I can feel it when I go to the sheepfold in the mornings to feed and such. To walk, this motion […] it does a lot”.
Participants described their joint experiences of how nature was an important element in physical exercise and lifestyle improvement, and that was most often described as the benefit of living in the rural area: “We have such good walking trails here” (Adda, 74-year-old woman).
Several younger participants used mobile apps to get an overview of their daily exercise, and some even found it motivating. No one described the importance of fitness centres in improving lifestyle and health, but some said they used the swimming pools for exercise.
Symptom management and monitoring
Nearly all the participants had only occasional symptoms, such as shortness of breath during exercise, and did not see themselves as “patients”. Participants described the self-care methods they used to monitor the symptoms of their diseases and their physical health. All the participants had been prescribed a considerable amount of daily medication to treat the disease and symptoms. Most said they were quite confident in reacting to their symptoms and found it easy to take prescribed medication, while for others it was a new experience that took some time to get used to. Jon, a 73-year-old man, described it as follows: “Never had to take any medication before. […] Now there is a full cupboard”.
The use of technology for communication with healthcare professionals, such as cardiologists, was not common although two of them consulted their specialists by email. The regular use of a blood pressure monitor was quite common. Many participants described a lack of computer skills, and preferred face to face communication with a familiar health-care professional.
Attitudes towards the disease
Those who had participated in cardiac rehabilitation described how better lifestyle and being symptom- free increased their sense of security, despite long distances to the hospital. Participants also described how the experience of having a life-threatening disease and undergoing rehabilitation had led to a better life. Vidar, a 72- year-old man, said, “It’s ridiculous […] to say that a heart, this big heart attack has brought me such better control of my life”. The attitudes towards the disease were mixed among participants taking control or letting life continue as usual. Frames of mind were also augmented with a certain serenity: Erna, a 58-year-old woman, said, “I just somehow feel like this won’t happen again”. One participant said that the consequences of the disease had crossed his mind: “You might think that […] but I just decided that this is not in my hands” (Audur, 62-year-old woman).
Discussion
This study´s results describe the participants’ experiences of education, surveillance, and self-care support after CHD related hospitalisation. The results elucidate a gap between the recommended ESC guidelines on secondary prevention and rural CHD patients’ support to maintain health and perform effective self-care. In addition, the results provide insight into the opportunities and challenges that people face in rural areas in Iceland, and even elsewhere in the Arctic, where access to healthcare is limited due to long distances, weather, and organisational factors.
The results, as described by the participants, are in concordance with the “Middle Range Theory of Self-care in Chronic Illness” [Citation21] and its three main components: Self-care maintenance, self-care monitoring, and self-care management. Maintaining health is a behaviour that involves maintaining mental and physical stability to limit the disease progress symptoms. The participants in this study demonstrated self-care maintenance by implementing lifestyle changes, such as consuming healthier foods and quitting smoking, and adhering to their medication regimen. However, to do so efficiently, they needed further contact, support, and instructions from health-care professionals. The education they needed was for example instructions on how to exercise safely after discharge, and dietary information. Monitoring in Riegel´s self-care theory [Citation21] refers to how patients monitor their health, listen to their body, and assess symptoms. The participants monitored their health for example by observing blood pressure and heart rate, but they lacked contacts to local health-care professionals to get reassurance on how they were doing in their self-care monitoring. Finally, management involves decision-making on how to respond to symptoms. Here, again, the participants reported need for more knowledge on when to seek assistance.
One of the changes that the participants saw as most urgent in the healthcare service was a better continuity of care at local healthcare centres, and the results show the underutilisation of the primary healthcare, digital solutions and telemedicine. Clinical guidelines [Citation10] on secondary prevention assume that primary healthcare guides cardiac patients and their relatives in the first weeks following returning home after a cardiac event, provides support, repeats important information, and refers the patients to appropriate resources. This study´s results show a lack of continuity of care and referral to appropriate resources. This is consistent with findings from a qualitative study of people with CHD in Norway [Citation35], which showed that patients were not receiving adequate instructions and information on how to integrate health information, and, as demonstrated in our study, needed help to facilitate connections to community resources, such as supervised physical training and guidance on lifestyle changes. Although all the participants in this study had received patient education before hospital discharge, they needed more knowledge and professional support, especially during their first days at home, which was not available in their local areas. This indicates that the enhancement of patient education is needed for the effective self-care of individuals in rural Iceland. The lack of rehabilitation referrals and resources in large areas of the country is consistent with the results of the Euroaspire IV and V studies [Citation19,Citation20], where it was demonstrated that clinical guidelines were not sufficiently followed and patients were not provided with referrals to rehabilitation and necessary information. The resources used by the participants in this study to change their lifestyles included support from family and friends and good access to pristine nature, which was preferred to the use of fitness centres. This information could prove valuable in developing follow-up and rehabilitation programs for people in rural areas in Iceland.
According to this study´s results, a patient’s sense of security, and consequently, the ability to manage self-care, may be influenced by access to health-care professionals and safe and reliable emergency services to hasten hospital admission. This is in accordance with the assumptions of Riegel et.al (2012) [Citation21] that self-care is affected by access to healthcare. The participants expressed a sense of security when transport was seen as safe, roads were passable, and if they had easy and stable access to health-care professionals. This is supported by Brundisini et. al (2013) [Citation25], who found that a feeling of vulnerability increases if healthcare professionals are of limited availability, and that patients appreciate being able to form long-lasting, personal relationships with professionals who know them. This is also consistent with studies that have shown that people with chronic disease in rural areas experience barriers in accessing healthcare that can be overcome with the help of long-distance healthcare services or telemedicine [Citation36], with professionals who live in their areas [Citation25], and with improvements such as interdisciplinary teamwork [Citation37]. A study from Northern Iceland showed that solid primary healthcare, good local elderly care, and reliable emergency services were fundamental for living in rural areas, as well as some freedom in healthcare choices [Citation38].
The participants in this study requested professional and personal support from someone familiar with their disease situations. This highlights the need for building bridges between specialised professionals, often situated in tertiary hospitals, and rural primary health-care professionals. Support from family and friends was of great importance to patients, which highlighted the importance of family-centred interventions. Participants had the opportunity for regular cardiology consultation, but this service was rarely provided in the local area, and the journey was considered expensive and time-consuming. People with newly-diagnosed CHD often want to receive patient education face to face [Citation39], from health-care professionals specialising in cardiac care who can individualise education following discharge [Citation40].
Implications for practice, policy and future research
The results of this study provide valuable input in healthcare policy-making in rural Arctic areas regarding the secondary prevention of CHD and providing support to CHD patients to implement self-care. The development of CHD risk factors and mortality rates have been unfavourable in the Arctic and rural areas in recent years, compared to urban areas [Citation16].
Recently, Health Policy: A Policy for Iceland’s Health Care until 2030 discussed schemes in which long-distance healthcare services could be implemented in Iceland [Citation28]. Prior studies have shown promising results on how to achieve risk goals through motivational interviews and solution-focused approaches [Citation41,Citation42]. Interdisciplinary, nurse-led teamwork has also yielded good results [Citation43]. Therefore, in rural Arctic areas, it could be effective to train and strengthen healthcare professionals to apply these methods and establish interdisciplinary teams, supported by expert professionals in urban areas connected through telemedicine. In this way, knowledge about the prevention and treatment of chronic disease will gradually be transferred from university hospitals to professionals in rural areas simultaneously so that patients may contact the professionals in the local area, and thus receive better and more targeted services.
Further research is needed on self-care of cardiac patients living in the Arctic, and how it is affected by their special environmental situation. Also, more intervention studies are needed to explore how e-health and telemedicine can possibly be used to improve patient education and support self-care in the Arctic.
Methodological considerations
To increase the study’s validity and reliability, the analysis was based on a systematic method that was carefully followed, and the decision trail documented throughout the research process. The different personal and clinical backgrounds of the research team can be seen as another strength of the study. This helped increase the reflexivity of the results, as different versions of the phenomenon were perceived and interpreted from different angles and acknowledgement of preconceptions. Another strength of the study lies in the demographic variation of the sample, as it includes males and females equally of various ages and from diverse parts of rural Iceland.
The limitations of the study could lie in the chosen method since it does not assume repetitive interviews, which could give deeper information and reinforce the synthesis of the themes. Instead, reassurance and understanding of the meaning of information were discussed continually with the participants in each interview.
Conclusion
Access to continuous healthcare, person-centred patient education and support focusing on prevention strategies is greatly impaired in rural areas in Iceland. In particular, according to the participants, improved process of referrals to available rehabilitation resources, lower travel-costs to specialist services, improved and continuous access to local health-care professionals, and access to individual patient education and rehabilitation are needed. Personal follow-up and patient education with a patient-centred and family-focused approach could be improved for rural inhabitants of Iceland.
Additional information
The study was funded by the Icelandic Regional Development Institute, the Icelandic Nurses’ Association Research Fund, and the University of Akureyri Research Fund.
Acknowledgments
We would like to acknowledge all the people who were willing to participate in this study and share their experiences.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- World Health Organization, W. (n.d.). Cardiovascular diseases. [cited 2021 Nov 9. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
- Andersen K, Aspelund T, Gudmundsson EF, et al. [Five decades of coronary artery disease in Iceland. Data from the Icelandic Heart Association]. Laeknabladid. 2017;103(10):411–13.
- Timmis A, Townsend N, Gale CP, et al. European society of cardiology: cardiovascular disease statistics 2019. Eur Heart J. 2020;41(1):12–85.
- Bjerregaard P, Kue Young T, Dewailly E, et al. Indigenous health in the Arctic: an overview of the circumpolar inuit population. Public Health. 2004;32:390–395.
- Burtseva TE, Uvarova TE, Tomsky MI, et al. The health of populations living in the indigenous minority settlements of northern Yakutia. Int J Circumpolar Health. 2014;73(1):25758.
- Aspelund T, Gudnason V, Magnusdottir BT, et al. Analysing the large decline in coronary heart disease mortality in the icelandic population aged 25-74 between the years 1981 and 2006. PLoS ONE. 2010;5(11):e13957.
- Thorolfsdottir RB, Aspelund T, Capewell S, et al. Population assessment of future trajectories in coronary heart disease mortality. PloS One. 2014;9(1):e85800.
- Sigmundsson Þ, Arnarson D, and Magnússon V, et al. Transportation time and quality of treatment among patients with STEMI in rural areas of Iceland Laeknabladid . 2016;102(1 doi:https://doi.org/10.17992/lbl.2016.01.59 Accessed05 09 2021).http://www.laeknabladid.is/tolublod/2016/01/nr/5696
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39(2):119–177.
- Piepoli MF, Hoes AW, Agewall S, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representati. Eur Heart J. 2016;37(29):2315–2381.
- Haraldsdóttir S, Valdimarsdóttir UA, Guðmundsson S. Poorer self-rated health in residential areas with limited healthcare supply. Scand J Public Health. 2014;42(3):310–318.
- Haraldsdottir S, Gudmundsson S, Thorgeirsson G, et al. Regional differences in mortality, hospital discharges and primary care contacts for cardiovascular disease. Scand J Public Health. 2017;45(3):260–268.
- Alston L, Allender S, Peterson K, et al. Rural inequalities in the Australian burden of ischaemic heart disease: a systematic review. Heart Lung Circ. 2017;26(2):122–133.
- Hoffmann R, Borsboom G, Saez M, et al. Social differences in avoidable mortality between small areas of 15 European cities: an ecological study. Int J Health Geogr. 2014;13(1):8.
- Stang A, Stang M. An inter-state comparison of cardiovascular risk factors in Germany: towards an explanation of high ischemic heart disease mortality in Saxony-Anhalt. Dtsch Arztebl Int. 2014;111(31–32):530–536.
- Virani SS, Alonso A, Aparicio HJ, et al. heart disease and stroke statistics—2021 update. Circulation. 2021;143(8). doi:https://doi.org/10.1161/CIR.0000000000000950
- Lindroth M, Lundqvist R, Lilja M, et al. Cardiovascular risk factors differ between rural and urban Sweden: the 2009 Northern Sweden MONICA cohort. BMC Public Health. 2014;14(1):825.
- De Bacquer D, De Smedt D, Kotseva K, et al. Incidence of cardiovascular events in patients with stabilized coronary heart disease: the EUROASPIRE IV follow-up study. Eur J Epidemiol. 2019;34(3):247–258.
- Kotseva K, Bacquer D, De, Backer G, et al. Lifestyle and risk factor management in people at high risk of cardiovascular disease. A report from the European Society of Cardiology European Action on Secondary and Primary Prevention by Intervention to Reduce Events (EUROASPIRE) IV cross-sectional su. Eur J Prev Cardiol. 2016;23(18):2007–2018.
- Kotseva K, De Backer G, De Bacquer D, et al., Investigators*, on behalf of the E. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–835.
- Riegel B, Jaarsma T, Strömberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012;35(3):194–204.
- Farquharson B, Abhyankar P, Smith K, et al. Reducing delay in patients with acute coronary syndrome and other time-critical conditions: a systematic review to identify the behaviour change techniques associated with effective interventions Cardiac risk factors and prevention. Heart. 2019;6:975.
- Seibæk L. Patient involvement in Greenland hospital-care: a qualitative study of the patient perspective. Int J Circumpolar Health. 2021;80(1):1971377.
- Lowe E, Banner D, Estefan A, et al. Being uncertain: rural-living cardiac patients’ experience of seeking health care. Qual Health Res. 2021;10497323211005432. doi:https://doi.org/10.1177/10497323211005431
- Brundisini F, Giacomini M, and Dejean D, et al. (2013 Accessed02 09 2019). Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. In Ontario Health Technology Assessment Series, (Vol. 13, Issue 15). http://www.hqontario.ca/en/mas/mas_ohtas_mn.html
- Wertz FJ, Giorgi A. The descriptive phenomenological method in psychology: a modified Husserlian approach. Pittsburgh, PA: Duquesne University Press, 233 pp, 978-0-8207-0418-0, $25.00 (paper). Journal of Phenomenological Psychology. 2009;41(2):269–276.
- Brinkmann S, and Kvale S. Interviews: learning the craft of qualitative research interviewing. 3.Edition ed. Los Angeles: SAGE; 2015.
- the Icelandic Ministry of Health. (n.d.). Health policy A policy for Iceland’s health services until 2030 Government of Iceland Ministry of Health. [cited 2021 Apr 5, https://www.government.is/library/01-Ministries/Ministry-of-HealTh/PDF-skjol/Heilbrigdisstefna_english.pdf
- Statistics Iceland. (n.d.). ICT usage by individuals. [cited 2020 Nov 22. https://statice.is/statistics/business-sectors/science-and-technology/ict-usage-by-individuals
- University of Akureyri. (n.d.). Lifestyles, risk factor management and self-care of individuals with coronary heart disease (The KRANS-study). [cited 2019 Dec 14]. https://www.unak.is/is/rannsoknir/rannsoknir-vid-ha/The-KRANS-study
- NVIVO.Qualitative Data Analysis Software. (n.d.). [cited 2020 Nov 21. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- MindNode. (n.d.). [cited 2021 Mar 4. https://mindnode.com
- Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40(8):795–805.
- World Medical Association. World Medical Association Declaration of Helsinki. JAMA. 2013;310(20): 2191.
- Valaker I, Norekvål TM, Råholm M-B, et al., Investigators, on behalf of the C. Continuity of care after percutaneous coronary intervention: the patient’s perspective across secondary and primary care settings. Eur J Cardiovasc Nurs. 2017;16(5):444–452.
- Ruiz-Pérez I, Bastos Á, Serrano-Ripoll MJ, et al. Effectiveness of interventions to improve cardiovascular healthcare in rural areas: a systematic literature review of clinical trials. Prev Med. 2019;119:132–144.
- Jaarsma T, Brons M, Kraai I, et al. Components of heart failure management in home care; a literature review. Eur J Cardiovasc Nurs. 2013;12(3):230–241.
- Gustafsdottir SS, Fenger K, Halldorsdottir S, et al. Social justice, access and quality of healthcare in an age of austerity: users’ perspective from rural Iceland. Int J Circumpolar Health. 2017;76(1):1347476.
- Ingadottir B, Blondal K, Jaarsma T, et al. Perceptions about traditional and novel methods to learn about postoperative pain management: a qualitative study. J Adv Nurs. 2016;72(11):2672–2683.
- Svavarsdóttir MH, Sigurdardottir AK, Steinsbekk A. What is a good educator? A qualitative study on the perspective of individuals with coronary heart disease. Eur J Cardiovasc Nurs. 2016;15(7):513–521.
- Bosselmann L, Fangauf SV, Herbeck Belnap B, et al. Blended collaborative care in the secondary prevention of coronary heart disease improves risk factor control: results of a randomised feasibility study. Eur J Cardiovasc Nurs. 2019;147451511988006. DOI:https://doi.org/10.1177/1474515119880062
- Wood D, Kotseva K, Connolly S, et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: a paired, cluster-randomised controlled trial. Lancet. 2008;371(9629):1999–2012.
- Connolly SB, Kotseva K, Jennings C, et al. Outcomes of an integrated community-based nurse-led cardiovascular disease prevention programme. Heart. 2017;103(11):840–847.