ABSTRACT
Information regarding medical evacuations in Greenland is sparse. This study provides an overview of incidence, costs, and diagnoses leading to medical evacuations in Greenland in 2018. This is a retrospective, observational study. Patients with a valid Danish civil personal registration number were included. Data were obtained by scrutinising the itinerary of the Greenland travel coordination office and the medical records. 481 patients were identified. Forty-nine patients were excluded. 432 patients were analysed. Two-thirds of the evacuations were carried out within Greenland. The overall incidence of evacuations was 7.7 evacuations per 1,000 inhabitants per year. This differed, however, between the five different health regions. The cost of a medical evacuation ranged from less than 4,800 US dollars to more than 50,000 US dollars per case. Pregnancy and childbirth accounted for the majority of evacuations in women (31.2%) while diseases within the circulatory system and digestive tract accounted for the majority of evacuations in men (39.8%). The costs of medical evacuations may be reduced when combining evacuations of more than one patient. This indicates that combining evacuations of multiple patients from one health region by applying mandatory use of a central coordinating service may be beneficial.
Introduction
Greenland is the largest Island in the world, spanning an area of 2,166,000 km2 with a population of 56,000 inhabitants [Citation1]. The majority of the population, 87% in total, lives in small or larger towns in Greenland. The remaining 13% live in small settlements with less than 500 inhabitants [Citation1].The vast distances combined with a population that is scattered over large areas pose considerable challenges to the delivery of health care. Greenland is divided into five health regions; each with a regional hospital and some health centres ().
Figure 1. An overview of Greenland and its health regions
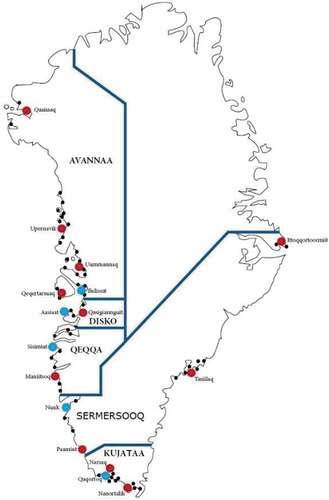
All healthcare in Greenland is tax-funded and free of charge for the citizens. Situated in the capital of Greenland, Nuuk, Queen Ingrid’s Hospital (QIH) is the most advanced hospital in Greenland and provides specialised diagnostic and therapeutic services for all of Greenland, such as advanced radiographic procedures as well as advanced surgical, medical, and psychiatric care. The regional hospitals facilitate primary care and hospitalisation as well as some elements of secondary care [Citation2,Citation3]. The vast majority of physicians working in Greenland are Danish. Of the very few physicians born in Greenland, almost all work at the QIH in Nuuk. Approximately 50% of the nurses employed in Greenland are of Greenlandic origin. The hospital in the capital of Greenland, Nuuk, provides the more advanced diagnostic and therapeutic interventions that cannot be carried out in the regional hospitals. Most settlements that do not have hospitals or health care clinics receive regular visits from a doctor and/or a nurse (2–4 times a year). The day-to-day health care in these small settlements is usually provided by a healthcare worker of Greenlandic origin who has training comparable to a nursing assistant or less. The written and spoken language at the hospitals is Danish while in the smaller settlements, Greenlandic is the language used. Patients whose required intervention exceeds the local capabilities may be evacuated to a more capable facility [Citation2]. In some instances, evacuation from a small settlement to a regional hospital will suffice, but patients whose treatment needs exceed those found locally may be evacuated to QIH for definitive treatment [Citation2,Citation3]. Despite the medical capabilities present at QIH in Nuuk, evacuation to a more advanced facility for further treatment may be necessary. In most instances, the tertiary hospital in Copenhagen, the capital of Denmark is the destination. However, as Iceland lies close to the eastern part of Greenland, in some instances, a medical evacuation is performed from East Greenland directly to Iceland. The process of evacuating a patient to offer more advanced medical interventions is complicated. A medical evacuation is usually requested by a physician or another healthcare worker on call at the location of departure. If a patient needs to be evacuated to QIH, the medical evacuation needs to be approved by a physician at the receiving hospital, the QIH. The period from deciding on a medical evacuation to the actual completion of the evacuation may vary according to the availability of the means of transport, limited daylight, the weather conditions, the large distances, the sparsely populated areas, and the limited infrastructure connecting towns, and the cost of the particular evacuation. Medical evacuations are usually carried out by either boat, helicopter, or fixed-wing aircraft [Citation3–5]. Due to rapidly changing weather conditions, during an urgent evacuation diversions to other airports, delays, or cancellations may occasionally occur. Evacuating a patient is not without risks as the level of monitoring and the level of treatments available during the transport may decline [Citation6]. The decision to evacuate a patient must thus be based on balancing the need for more advanced treatment with the risks that a medical evacuation entails. Thus, the urgency of the medical evacuation should be clarified before transport [Citation3]. Apart from the mere healthcare-related considerations, another aspect to be considered is the cost of a medical evacuation [Citation3]. According to the financial proposal from 2018, patient transports and medical evacuations are budgeted at 6.4% of the total Greenlandic health care budget and thus represent a significant part of the Greenland health budget [Citation7]. The costs are not likely to be reduced in the future because there is an increasing demand for medical services and specialised treatment in Greenland [Citation2]. Few previous studies described the patients subjected to medical evacuation in the arctic. None of these studies investigated the conditions that apply to Greenland [Citation4]. The aim of this study was thus to describe the medical evacuations occurring in Greenland in 2018.
Methods
We performed a retrospective, observational study including all medical evacuations completed in Greenland in the year 2018.
Definitions
In this study, a medical evacuation was defined as an extraordinary flight to transfer a patient from one location to another. The international transfers were attributed as originating from Semersooq, even when patients might have begun their transfer journey from another region. Our study did not include patients evacuated by elective or planned scheduled transfers carried out in regular passenger flights.
Identification of patients
All patients evacuated in 2018 in Greenland were identified using the information provided by the health administration in Greenland. The information included the Civil Personal Registration number (CPR-number) which is a unique identifier of all patients [Citation8], the dates of the medical evacuation, and the initial diagnosis assigned to the patients. In case of invalid or incomplete CPR-number, the electronic billing system was used to identify the patients by checking names, site of departure, and location of destination with the medical records at the receiving destination. Medical evacuations cancelled before departure were not registered by the Greenlandic Health administration and thus do not appear in this study.
Inclusion and exclusion criteria
All patients who were either identified by a valid CPR number or who could be identified via information obtained from the electronic billing system were included. Tourists and other patients with no valid CPR number were excluded as were patients with no accessible medical records.
Data collection
The data collection was carried out by the authors HBP, BBP, MB, and MM by manual review of the medical records. One investigator (HSB) reviewed the medical records a second time to ensure the validity of the data. The itinerary provided by the Greenlandic Travel Coordination Service in all medical evacuations was used as the data source regarding location and time of departure and the initial diagnosis assigned to the patient. Further, this itinerary was used as the source of costs for each medical evacuation.When the time for initiating a medical evacuation was missing in the itinerary, we assumed that the timestamps in the medical records correlated with the actual time of ordering the medical evacuation. In case of a discrepancy between the electronic billing system and the medical records, the electronic billing system was used as a reference. The initial diagnosis for requesting an evacuation was categorised according to the ICD-10 classification system [Citation9].
Variables
We obtained information regarding age, sex, initial diagnosis, time of the decision to order a medical evacuation, the location of departure, and the time of admission at the receiving facility. We stratified patients according to sex, age, and ICD-10 diagnosis group. Medical evacuations were categorised according to the region of departure. The different types of medical evacuations were categorised as follows: Intra-regional medical evacuation, extra-regional medical evacuation (typically any medical evacuation with QIH as destination), and medical evacuation to another country. We registered the total cost of each medical evacuation. Furthermore, we registered the time that elapsed from deciding upon a medical evacuation to the evacuation had started. The evacuations were divided into three strata regarding departure: Medical evacuations carried out during the daytime (8 am-4 pm) on weekdays, evacuations carried out during evenings and night-time on weekdays (4 pm-8 am), and evacuations carried out on weekends and holidays (Friday 4 pm – Monday 8 am).
Approvals
All local legislation regarding data protection was respected. Ethical approval was obtained from the Greenlandic Health administration and the Greenlandic Ethics Committee (KVUG 2019–05).
Statistical analyses
Data were manually extracted from the medical records. Microsoft Excel 2016 (Microsoft Corp. Redmond, Washington, USA) and STATA 16.0 (StataCorp, College Station, Texas, USA) were used for statistical analyses. Data are presented as absolute numbers, percentages, median, and quartiles or range (where appropriate). A Chi-squared test (2 x 2 tables up to 2 × 5 tables) or a Kruskal-Wallis tests for equality of populations were applied to analyse for significant differences between groups. The level of significance was set at p < 0.05. The number of inhabitants in each region from 1 January 2018 was used to correlate the number of medical evacuations to the patient population (transports per 1,000 inhabitants) in each region [Citation10].
Results
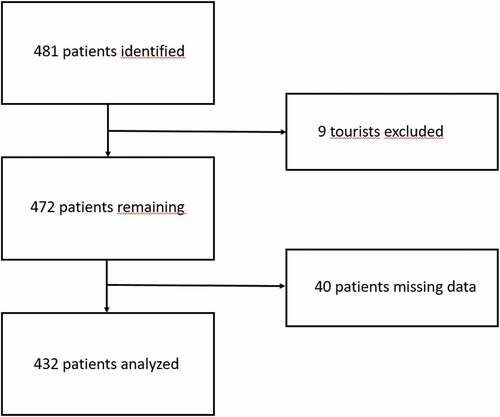
A total of 481 patients were identified using the list of medical evacuations provided by the travel coordination services. According to the criteria for exclusion (missing data, invalid CPR-number, no available medical records, or status as tourists), 49 patients were excluded. Thus, medical records from 432 patients were individually reviewed. For the flow chart, see .
In 53 cases, more than one patient was evacuated in one stroke. Forty-six evacuations were performed by having one medical crew accompany two patients, while seven evacuations of three or more patients were performed. Patients evacuated out of Semersooq accounted for the highest number of evacuations of multiple patients.
Distribution between health regions
The overall incidence of medical evacuations was 7.7 per 1,000 inhabitants per year. Overall, the incidence of medical evacuations within regions was lower (2.2 per 1,000 inhabitants per year) than the incidence of medical evacuations to QIH (5.5 per 1,000 inhabitants) (p < 0.00001). For details see .
Table 1. Overview of medical evacuations from each health region in Greenland in 2018
Distribution of diagnoses
Overall, the most frequent diagnoses assigned to patients evacuated were found within the ICD-10 classification chapters IX, Diseases of the circulatory system (15.5%), XI Diseases of the digestive system (18.1%), and XV Pregnancy, childbirth, and the puerperium (16%). In the age group 0–15 years, the most abundant reason for performing a medical evacuation was disease within the ICD-10 chapter XVI “Certain conditions originating in the perinatal period” (28%), whereas patients aged 16–29 years most predominantly were assigned a diagnosis within the ICD-10 chapter XV “Pregnancy, childbirth and the puerperium”. This diagnosis was assigned to 57.7%. In patients older than 55 years of age, diagnoses within the ICD-10 chapter IX “Diseases of the circulatory system” (28.1%) were the most frequent indication for evacuation. See for details.
Table 2. Distribution of diagnoses in evacuees in Greenland 2018 according to the WHO ICD-10 chapters
Evacuation by the time of day
The time from admission to deciding upon a medical evacuation was stratified into three strata: weekdays (8 am-4 pm), evenings and nights (4 pm-8 am), and weekends and holidays. The results are depicted in . The three groups did not differ significantly (Kruskal-Wallis test, p = 0.51).
Table 3. Medical evacuations in Greenland in 2018, divided in the time of departure and the cost. Time from admission to deciding upon an evacuation is presented as medians and quartiles
Destination of evacuated patients
In total, 377 evacuations were carried out within Greenland. The most common receiving facility was QIH in Nuuk with 270 Medical evacuations (62.5%). Of the patients evacuated within Greenland, 107 patients were transported to a facility within the same health region. A total of 55 patients were evacuated from a location in Greenland to another country. Forty-seven of these 55 patients (85.5%) were evacuated from QIH to hospitals in Iceland or Denmark. Only a few patients were evacuated directly from a regional facility to Iceland or Denmark.
Cost of medical evacuations
Although the number of evacuations did not differ throughout the days, the cost of a medical evacuation did differ according to the time of departure. The median cost of a medical evacuation was USD 4,700 (range USD 1,803–10,334). There was a wide span of cost, with some medical evacuations costing more than USD 50,000. The most expensive evacuations were carried out during evenings and nights or weekends. The less expensive medical evacuations (<USD 4,800) were primarily evacuations to QIH in Nuuk. The cost of combined medical evacuations also differed between the health regions. The most expensive transports were carried out in Semersoq. In all but one health region, the costs of combining medical evacuations resulted in a reduction in expenses per patient. See .
Table 4. Distribution of regional costs associated with medical evacuations. Costs are depicted as costs per transported patient and are reported for each patient transported singularly and patients transported in combination with other patients. Values are presented as means only as the value attributed to patients nos. 2 and 3 in combined transports were assigned to USD 0.00. The Chi-squared test (2 x 5 tables) was applied to test for differences between groups
Discussion
Main findings
In this study, we examined the medical evacuations of patients in Greenland in 2018. We found that nine out of ten medical evacuations took place within Greenland itself, the primary destination being the Queen Ingrid’s Hospital in Nuuk. We found that the incidence of evacuations differed between the five regions. The lowest number of evacuations were carried out within Semersooq which is the region that contains the most advanced hospital in Greenland. The overall incidence of evacuations per 1,000 inhabitants was significantly different among all regions in Greenland. The incidence of evacuations to Queen Ingrid´s Hospital in Nuuk from the Semersooq region was significantly smaller than the incidence of evacuations from the other four health regions. We believe this was the logical consequence of the large population living within Nuuk having Queen Ingrid´s Hospital as their primary care hospital. Thus, a secondary transport of patients in Semersooq was only indicated when the resources of the largest and most advanced hospital in Greenland were not sufficient and the patients thus were evacuated out of Greenland. The incidence of evacuations to QIH from the other four health regions in Greenland did not differ significantly. We found that patients with advanced treatment needs often were evacuated from other regions to QIH in Semersooq, before ultimately being evacuated to Denmark or other countries. This explains the higher number of medical evacuations from Semersooq to another country, compared to the other regions. The three most common causes of patient evacuation were cardiovascular disease (ICD-10 Chapter IX), diseases of the digestive tract (ICD-10 Chapter XI), and conditions related to pregnancy (ICD-10 Chapter XV). One-third of the evacuated female patients were diagnosed with conditions related to pregnancy and births. QIH in Nuuk is the only hospital in Greenland with facilities for handling preterm births and other complicated births [Citation11]. Thus, all women in whom preterm birth or other perinatal complications are expected are transferred to QIH approximately three weeks before term [Citation12].Among young men, the primary diagnosis indicating evacuations were related to trauma, other injuries, and poisoning. Previous research has shown that patients in this group have a high number of suicide attempts in Greenland and it appeared that a large amount of transported patients suffered from self-inflicted injuries [Citation13–15].The expenses related to the medical evacuations varied according to the time of the day that the evacuation was performed. Thus, evacuations carried out outside of the normal working hours (weekdays 8–16) were associated with higher costs. Medical evacuations can be regarded as a consequence of a mismatch between the need for treatment and the local resources available. Greenland’s large distances and dispersed scattering of the population across the vast area necessitates medical evacuations as an integral part of the national health service. Medical evacuations are also a result of a choice to offer specialised treatment at only one location in Greenland, thus applying the principle of bringing the patient to the treatment rather than treating the patient locally [Citation16]. We found that the overall incidence of evacuations differed significantly between the five different regions in Greenland. The lower incidence in the region of Semersooq can be explained by the fact that a large proportion of the population is situated in Nuuk. Thus, there is no need for a medical evacuation across the borders of the health region for patients falling ill in that particular health region, and a simple, intra-regional transport can be performed. There was no difference in time from admission to the local health clinic or hospital to the decision to evacuate was made, regardless of the time of day or the day of the week. An individualised audit of the medical records included in our study, however, indicated that some patients were evacuated quicker than other patients. We found that particularly in Semersooq, patients who had been scheduled for a less urgent medical evacuation could be transported sooner than originally planned, should another, more urgent transport of a new patient become necessary. In these instances, two patients or more could be transported in one stroke as the vehicle used for transportation, and the medical personnel accompanying the more acutely ill patient could perform double duty. This pooling of patients was facilitated by the senior regional physician or by the travel coordination service. We believe that this approach may have led to a reduction of costs in many cases. The calculated costs of the evacuations ranged from zero (an evacuation of a patient that by coincidence could travel with another patient) to more than 50,000 USD. Consistent with other studies, an evacuation during the day was less costly than an evacuation during the weekend or the night [Citation4]. Medical evacuations covering large distances carried a higher cost than medical evacuations covering shorter distances. First of all, medical evacuations covering long distances require a greater amount of fuel, and second, more airports may be required to open in case of sudden weather changes necessitating deviations en route.
Other studies
A Norwegian study reported that the most frequent diagnoses eliciting an evacuation were neurological and cardiological diseases that exceeded the capabilities available at the referring hospital or health clinic [Citation17]. In a study from the remote parts of Alaska, trauma or respiratory diseases were the main reasons for health clinics to evacuate the patients [Citation18]. In Europe, in Poland, the evacuees from remote health clinics or minor hospitals were shown to be primarily trauma patients [Citation19]. A mutual trait for the patients evacuated in our study and the three studies mentioned above was that the severity of illness exceeded the capabilities available at the evacuating centre. A Canadian study by McDonnell et al suggested that reductions in the need for evacuation could be attained with initiatives to increase the local capabilities. This could be done by increasing the educational level of the health care workers in remote places, by implementing better recruitment of local workforces, and by increasing the availability of more advanced equipment [Citation20]. However, this is not always a simple solution as several barriers to adequate health care in remote regions have previously been identified: The mere physical geography with the need for long travelling distances is one. Healthcare staff shortages have been identified as another factor affecting patient access to health care services. Cultural and language differences have also been addressed, as the healthcare practitioner´s lack of knowledge about minority and indigenous populations was identified as an important barrier, even to the brink of discrimination related to legacies of colonialism. Finally, systemic factors in the form of fragmented management of health services, lack of communication between management and staff, and lack of funding for the healthcare system were identified [Citation3]. A reduction in the need for evacuations may be achieved with increasing telemedical possibilities. A study from Greenland concluded that the number of evacuations could be reduced by implementing optimal telemedical consultations between the peripheral health clinics and the larger centres [Citation21]. The same findings were reported in a study on traumas of the upper extremity [Citation22]. The cost-effectiveness of telemedical solutions has been investigated and found to be acceptable when properly implemented [Citation23].
Based on the reviews of the medical records of the patients in our study, an impression was created that the establishment of basic guidelines for deciding and initiating an evacuation in some instances could have reduced the costs of evacuations. We found that in these cases central coordination of the evacuations increased the rational use of the resources. Thus, in some cases, the medical evacuations included two or more patients with a subsequent reduction in the total costs. These measures may be pursued by coordinating the evacuations, a task that is presently being facilitated by either the travel coordination in Nuuk or the local physician. Although it is difficult to establish uniform guidelines for all regions, due to different terrain and weather conditions, central coordination of all medical evacuations might result in better coordination within and outside a region.
Strengths and limitations
One of the major strengths of this study is the low number of unidentified patients being excluded. This is facilitated by the unique civil personal registration number, the CPR-number, which enables the identification of all patients residing in Greenland and Denmark [Citation8]. Another strength of the study is the validation process in collecting data. All data were manually reviewed twice to ensure the optimal quality of data. Among the limitations in this study are chance findings of very few patients evacuated that did not appear on the official list of evacuated patients. This indicates that not all patients had been registered by or reported to the coordinating offices of medical evacuations. This was the case with a few patients from the region of Tasiilaq. This region lies in the very eastern part of Greenland and it is possible that some evacuations were made to Reykjavik, Iceland. From Tasiilaq, the nearest advanced medical facility is situated in Reykjavik, Iceland, and not in Nuuk. Despite the use of the CPR number to identify patients, some patients were not included in this study due to inaccessible medical records. Patients with missing data were primarily from Tasiilaq, as another medical record system may have been used in this particular region opening the possibility that some data from Tasiilaq were inadequate. Another limitation in this study was that we only investigated the physical properties and the costs of the evacuations. This study did not aim to investigate whether evacuations from remote health care clinics were caused by variations in the staffing of the smaller clinics or whether evacuations were indicated as a cause of other barriers to acceptable primary healthcare as alluded to above.
Conclusion
This study provides an overview of the medical evacuations in Greenland in 2018. The most common indication for evacuations were diseases related to the digestive tract. While in the majority of patients, evacuation to the Queen Ingrid´s Hospital in Nuuk sufficed, some patients required further evacuation to Denmark or other countries for additional treatment. The median cost of the evacuations was approximately 5000 USD; the more expensive evacuations taking place outside normal working hours. We identified a possibility for reducing the costs of medical evacuation when combining transports of more than one patient, primarily when performing evacuations out of Greenland. However, the more costly evacuations outside normal working hours may be a result of patients presenting with acute conditions of a severity that does not allow for combined transports. Thus, the costs per evacuated patient may be higher. We suggest that further studies focusing on improved cooperation within the individual health regions may improve future planning and execution of the medical evacuations.
Author contributions
Study design: All authors
Collection of data: HBP, BP, MB, MM.
Drafting of the manuscript: HBP, BP, SM.
Critical reviewing of data: All authors.
Critical revision of the manuscript: All authors.
Approval of manuscript before submission: All authors.
Geolocation information
This research was carried out in Greenland.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Anonymized data are available directly from the corresponding author ([email protected]) on reasonable request. No data deposition has been carried out.
Additional information
Funding
References
- Facts about Greenland. [ cited 2021 June 27]. Available from: https://naalakkersuisut.gl/en/About-government-of-greenland/About-Greenland/Facts-about-Greenland
- Niclasen B, Mulvad G. Health care and health care delivery in Greenland. Int J Circumpolar Health. 2010;69:437–10.
- Huot S, Ho H, Ko A, et al. Identifying barriers to healthcare delivery and access in the Circumpolar North: important insights for health professionals. Int J Circumpolar Health. 2019;78(1):1571385.
- Gunnarsson B, Jensen NS, Garði TI, et al. Air ambulance and hospital services for critically ill and injured in Greenland, Iceland and the Faroe Islands: how can we improve? Int J Circumpolar Health. 2015 June10;74:25697. PMID: 26066019; PMCID: PMC4463496.
- Bjerregaard P, Mulvad G, Olsen J. Studying health in Greenland: obligations and challenges. Int J Circumpolar Health. 2003 Mar;62(1):5–16. PMID: 12725338.
- McGuire NM. Monitoring in the field. Br J Anaesth. 2006;97:46–56.
- Grønlands Selvstyre. Forslag til Finanslov 2018. [Online]. [ cited 2021 June 27]. Available from: https://naalakkersuisut.gl/~/media/Nanoq/Files/Attached%20Files/Finans/DK/Finanslov/2018/FL2018%20%20med%20sidetal%20linket%20indholdsfortegnelse%20og%20underskrift%20%20DK.pdf
- Schmidt M, Pedersen L, Sørensen H. The danish civil registration system as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549.
- WHO. International statistical classification of diseases and related health problems 10th revision. [ cited 2021 June 27]. Available from: https://icd.who.int/browse10/2016/en.
- Statistics Greenland: municipalities of Greenland 2018. [ cited 2021 June 27]. Available from: http://www.stat.gl/publ/da/BE/201901/pdf/Gr%C3%B8nlands%20befolkning%202019.pdf
- Pregnancy and Childbirth in Greenland. [ cited 2021 June 27]. Available from: https://www.norden.org/en/info-norden/pregnancy-and-childbirth-greenland
- Vilalta A, Troeger KA. Disparities in emergency transport of women with a preterm labor diagnosis in urban vs rural areas in the US. Clinicoecon Outcomes Res. 2020;12:327–332.
- Björkstén KS, Bjerregaard P, Kripke DF. Suicides in the midnight sun–a study of seasonality in suicides in West Greenland. Psychiatry Res. 2005 Feb28;133(2–3):205–213. PMID: 15740996.
- Bolliger L, Gulis G. The tragedy of becoming tired of living: youth and young adults’ suicide in Greenland and Denmark. Int J Soc Psychiatry. 2018 June;64(4):389–395. Epub 2018 Apr 10. PMID: 29633920.
- Sargeant H, Forsyth R, Pitman A. The epidemiology of suicide in young men in greenland: a systematic review. Int J Environ Res Public Health. 2018 Nov1;15(11):2442. PMID: 30388882; PMCID: PMC6266058.
- Aaen-Larsen B. Health care in the circumpolar world: Greenland. Int J Circumpolar Health. 2004;63(Suppl 2):49–53. PMID: 15736622.
- Zakariassen E, Østerås Ø, Nystøyl DS, et al. Loss of life years due to unavailable helicopter emergency medical service: a single base study from a rural area of Norway. Scand J Prim Health Care. 2019;37:233–241.
- Rice B, Wood J, Britton C, et al. Medevac utilization and patient characteristics in Rural Alaska 2010 to 2018. Air Med J. 2020 Sept-Oct;39(5):393–398. Epub 2020 Jun 19. PMID: 33012479.
- Rzońca P, Gałązkowski R, Wójcik-Fatla A, et al. Missions of the helicopter emergency medical service in rural and urban areas in Poland - a comparative retrospective analysis. Ann Agric Environ Med. 2019 June17;26(2):355–360. Epub 2019 Apr 19. PMID: 31232071.
- McDonnell L, Lavoie JG, Healy G, et al. Non-clinical determinants of Medevacs in Nunavut: perspectives from northern health service providers and decision-makers. Int J Circumpolar Health. 2019 Dec;78(1):1571384. PMID: 30724715; PMCID: PMC6366434.
- Penninga L, Lorentzen AK, Davis C, et al. Series for acute medical emergencies in Greenland: a model for austere environments. Telemed J E Health. 2020 Aug;26(8):1066–1070. Epub 2019 Dec 4. PMID: 31804895.
- Tripod M, Tait M, Bracey J, et al. The use of telemedicine decreases unnecessary hand trauma transfers. Hand (N Y). 2020 May;15(3):422–427. Epub 2018 Nov 12. PMID: 30417694; PMCID: PMC7225886.
- Natafgi N, Shane DM, Ullrich F, et al. Using tele-emergency to avoid patient transfers in rural emergency departments: an assessment of costs and benefits. J Telemed Telecare. 2018 Apr;24(3):193–201. Epub 2017 Mar 7. PMID: 29278984.