ABSTRACT
In the spring of 2020, the Alaska Native Tribal Health Consortium (ANTHC) designed and built a sanitizing treatment system to address shortages of filtering facepiece respirators (FFRs). The design criteria included sanitizing large numbers of FFRs, repeatedly achieving FFR fit test requirements, and deactivating enveloped respiratory viruses, such as SARS-CoV-2. The outcome was the Mobile Sanitizing Trailer (MST), a 20 by 8-foot modified trailer designed to process up to 1,000 FFRs during a standard heat cycle. This paper reports on the MST’s ability to: (1) sustain a target temperature, (2) produce tolerable conditions for FFRs as measured by fit factor and (3) successfully deactivate an infectious model virus. We found that the MST reliably and uniformly produced 75 degrees Celsius in the treatment chamber for the prescribed periods. Quantitative analysis showed that the FFRs achieved acceptable post-treatment fit factor even after 18, 60-minute heat cycles. Finally, the treated FFR materials had at least a log 3.0 reduction in viral RNA and no viable virus after 30, 60 or 90 minutes of heat treatment. As a sanitizing treatment during supply shortages, we found the MST a viable option for deactivation of virus and extending the usable life of FFRs.
Background
In late 2019, a novel coronavirus, SARS-CoV-2 the aetiological agent of coronavirus disease (COVID-19), spread worldwide. It was first detected in Alaska in March 2020. After initially being controlled, COVID19 cases began to increase in July 2020. By the end of 2020, the State Department of Health and Social Services reported 46,037 cases, 1035 hospitalisations [Citation1], and 245 deaths [Citation2], along with growing burden on the Alaska health system [Citation3]. COVID-19 is both a respiratory and inflammatory disease, with a significantly higher age-adjusted mortality (1.8-fold risk) in Alaska Native and American Indian populations [Citation4].
Throughout the first two years of the pandemic in Alaska, there were shortages of medical supplies including the disposable personal protective equipment (PPE) critical for hospitals and first responders. Of particular concern, was the shortage of N-95s, filtering face piece respirator (FFR) that met the National Institute for Occupational Safety and Health standard for filtering at least 95% of the airborne particles [Citation5].
The Alaska Native Medical Centre (ANMC) is a 173-bed hospital located in Anchorage, Alaska. It is the largest hospital serving Alaska Native and American Indian peoples in the USA. On a typical day, at ANMC, about 3000 FFRs are donned and discarded by medical staff. During the early months of
2020, the demand for FFRs increased, which resulted in shortages in Alaska and globally. The U.S. Centres for Disease Control (CDC), recognising that alternative strategies were needed to preserve limited supplies and provide protection for frontline health workers, developed new “crisis capacity” guidance allowing for the “reuse or decontamination” of FFRs [Citation6].
In March 2020, ANMC began implementing a reuse policy based on the CDC guidance, instructing staff to wear the same mask or FFR up to five times before disposal. This helped to extend use but with COVID-19 cases rising, there was a need for other strategies to help ensure that there would be adequate supply in the coming months.
In April 2020, the Alaska Native Tribal Health Consortium (ANTHC) assembled an interdisciplinary team including engineers, environmental health and safety professionals, skilled labourers, physicians, and nurses as a task force to develop methods for FFR decontamination. The goal was to design, build test, and operationalise a system that could meet five key criteria: (1) sanitise large volumes of FFRs, (2) utilise materials currently available in Alaska, (3) be scalable for use in rural hospitals, (4) repeatedly achieve the fit requirements for FFRs and (5) be effective at sanitising FFRs potentially contaminated with SARS-CoV-2.
At the time, the CDC “Crisis Capacity” guidance recognised three approaches for the decontamination of FFRs: (1) ultraviolet germicidal irradiation (UVGI), (2) vaporous hydrogen peroxide and (3) moist heat. The first approach, building a UVGI system, was not viable because the required lighting bulbs and ballasts were not available in Alaska. The second, vaporous hydrogen peroxide was in use at ANMC to sterilise medical equipment. There were, however, safety concerns for FFR decontamination related to vapours and the possibility of skin or respiratory reactions. The third approach using heat seemed achievable, scalable and the best option for meeting both the design criteria and the urgent time frame.
SARS-CoV-2 is one of the group of viruses that can be deactivated by exposure to moderate temperatures. A study by Heimbuch et al. found that 99.9% of a model H1N1, was inactivated when FFRs were heated to a temperature of 60°C for 15–30 minutes [Citation7]. Darnell et al. found that heat treatment for 45 minutes at 75°C resulted in complete inactivation of SARS-CoV [Citation8]. Price et al. was able to preserve the respiratory efficiency of FFRs for up to 20 cycles, using a temperature of 70°C for 30 minutes, indicating that FFRs could sustain repeated heating at these temperatures [Citation9].
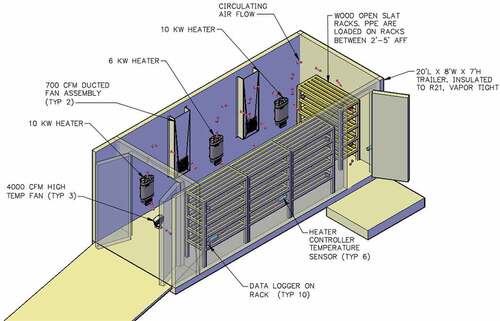
ANTHC was proposing a novel design () and there were no published articles describing test results using large-scale dry heat treatment units. The CDC crisis capacity strategy allows reuse of the same FFR up to five times. The goal for the ANTHC was to develop an approach that would allow the FFRs to be sanitised up to ten times if necessary. Both virological and FFR fit testing were considered necessary to demonstrate the effectiveness of the process and to earn the confidence of health care workers in the clinical setting.
Construction of the MST began on 9 April 2020 and involved the retrofit of a 6 × 2 metre utility trailer. The trailer was durable, mobile and could accommodate enough shelf space to process 1000 masks per run cycle. Specifications included high temperature insulation, stainless steel walls, sauna grade stainless steel heaters and fans, and heat-resistant electronics. Wood shelving was used instead of steel to preserve electrostatic charge, an inherent feature used to improve the filtration properties of N-95 respirators [Citation10]. The MST was operational at ANMC on 23 April 2020 ().
The next steps were to (1) demonstrate that the MST could achieve and sustain a 75°C target temperature; (2) that the FFRs could tolerate repeated heat treatments in this unit; and 3) the heat treatments could deactivate the model viruses.
Methods
Testing MST ability to achieve prescribed temperatures
The MST operations experiment involved testing the unit to reliably and uniformly achieve target temperature and duration. Based on the Darnell et al. paper, 75°C was selected as the target operational temperature for a 60-min cycle [Citation8]. The MST utilised programmable controls and six temperature sensors that were actively monitored throughout the process. Packaging the FFRs for repeated use involved placing each FFR into an individual paper bag, labelled for return to the same user. This was done to emulate the method used in clinical applications, one user per FFR to reduce the risk of pathogen transmission between medical staff. Temperature measurements in the MST were collected in three ways: using electronic sensors for the ambient temperatures inside the MST, using heat activated temperature labels adhered to the outside of each bag, and electronic data loggers to record the temperatures inside the paper bags. Relative humidity in the MST was also measured using electronic data loggers. The MST heating proceeded as follows: temperatures were increased until the sensors averaged 49°C. Heating was then paused for 10 minutes to allow temperatures to equalise throughout the enclosure. This was done again at 60°C and then the temperature was ramped up to the operational temperature of 75°C. The heat cycle was then initiated based on the prescribed time period.
Testing treated FFRs for fit factor
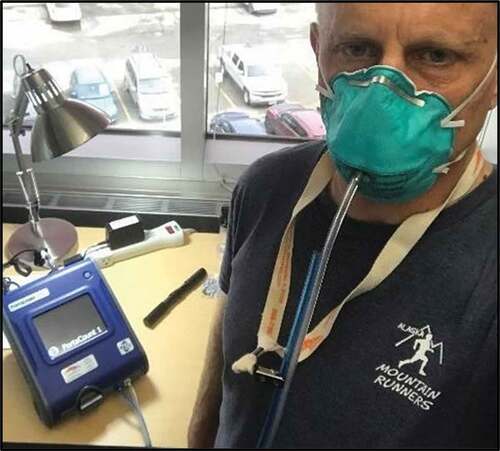
Testing the resilience of FFRs to the treatment process involved repeat heating and then measurement of fit factor using three models of medical N-95 FFRs. Testing was done in mid-June of 2020. The aim was to test the FFRs until fit test failure. To determine fit factor, ANTHC performed a series of quantitative tests using a TSI PortaCount Respirator Fit Tester, model 8038 (see ). The PortaCount uses an
Occupational Safety and Health Agency (OSHA) approved method to quantitatively fit test a respirator [Citation11]. This allowed the evaluator to assess the filtration properties of the respirator and limit ambiguities from the process, which is partially intended to assess the ability of the wearer to properly don the respirator.
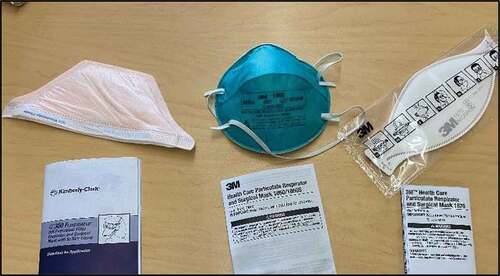
The method uses an ambient aerosol condensation nuclei counter. A fit factor is calculated by dividing the outside particle concentration by the particle concentration inside the respirator [Citation12]. When using the PortaCount on respirators with less than 99% efficiency (e.g. an N95 respirator with 95% efficiency), PortaCount uses the “N95 Companion” mode. In this mode, the maximum fit factor that can be reported is 200. Anything above 200 is reported as “200+” [Citation13]. Two tests were performed on each respirator type, the first on a new respirator, which was used as the baseline measurement, and the second on a respirator, that had been heat-treated. The FFR models included those commonly used in the ANMC hospital: the Kimberlee Clark – K300 Fluid Shield, 3 M 1860 Health Care Particulate Respirator and Surgical Mask, and 3 M 1870 Health Care Particulate Respirator and Surgical mask (see ). A total of 18 heat cycles and 18 fit tests were completed before the leased PortaCount instrument had to be returned.
Testing treated FFR materials for viral inactivation
The virology experiment involved the model virus, inoculated respirator samples from four types of FFRs, heat treatment in the MST for different timeframes, and analysis for infectious virus and residual viral RNA. Heat inactivation of enveloped RNA viruses like SARS-CoV-2, had been widely used for decades. To analyse the effects on an authentic infectious RNA virus inoculated into different FFR materials, we employed influenza virus A/WSN/33 (H1N1) (WSN), a well-established model respiratory virus used at the University of Alaska Anchorage, Biosafety Level 2 (BSL2) Bortz Laboratory [Citation14]. Like animal coronaviruses, influenza viruses exhibit similar heat deactivation profiles as SARS-CoV-2, but
WSN lacks human infectivity, according to data reported in peer-reviewed literature and preprints [Citation15,Citation16]. For this reason, handling of WSN does not require the Biosafety Level 3 (BSl-3) precautions, required for microbes that can cause serious or acute disease through inhalation. For example, avian, human H3N2, and human H1N1 influenza A viruses and influenza B virus are deactivated after heat treatment at
55.6°C (132.1°F) for 30 minutes, with evidence of inactivation for shorter times and at higher temperatures [Citation17–20].
This experiment tested heat deactivation of FFR materials using a consistent temperature of 75°C, for either 30, 60 or 90 minutes. Samples of the sectioned FFR materials were inoculated with influenza virus
WSN. The test materials were from four FFR models: 1) 3 M 1870 Health Care Particulate Respirator and Surgical Mask 2) Kimberlee Clark – K300 Fluid Shield, 3) 3 M 1860 Health Care Particulate Respirator and Surgical Mask, and 4) 3 M 8200 Industrial Particulate Respirator. Three different materials were prepared from each FFR, including the strap, the metal used on the nose bridge, and the filter fabric. These components were cut into approximately 1 cm2 pieces, placed on sterile 12-well tissue culture treated plates and UV-sterilised for 10 minutes. Each well was treated with 250 µL of phosphate-buffered saline (PBS) to help maintain a constant pH, and inoculated with a 10 µL aliquot of influenza A/WSN/33 (H1N1) virus containing 5 × 104 infectious units (I.U.) total. The plates were then incubated at room temperature for 15 minutes before drawing the resulting supernatant liquid and wrapping the plates with parafilm sealant to maintain sterility during transport to the MST. WSN inocula were derived from aliquots of a stock WSN titre of 5 × 103 I.U./µL (5x106 I.U./mL, a titre corresponding to a typical high-titre respiratory droplet with titre calculated by 10-fold serial limiting dilution assay (LDA) in 96-well plates (concentration range of 10°–10− [Citation8]). In LDA, I.U. of samples diluted in 50 µL of OptiMEM (Gibco) were quantified by 1-h inoculation of cells in 250ul PBS at 37°C in a 5% CO2 sterile humidified tissue culture incubator, replaced with complete growth medium (DMEM, 10% FBS, supplemented with antibiotics), and growth for 1 day, on monolayers of human lung adenocarcinoma cells (A549). The titre of WSN in inocula and experiments, measured in I.U., was back-calculated by visualisation of cytopathic effect (C.P.E.) and immunoflourescent quantification of WSN nucleoprotein (NP) infectious centres labelled using monoclonal antibody AA5H (ThermoFisher Scientific), as described previously [Citation14]. To calculate I.U., immunofluorescent infectious centres were enumerated in duplicate for N = 8 tenfold serial dilutions of the input inoculum, and back calculated to quantify original inoculum titre (dividing the average number of immunofluorescent infectious centres by 10−N, where N is the serial dilution step).
To serve as non-heat treated controls, a set of virus-positive and virus-negative plates were incubated at room temperature for one-hour post-inoculation, and then stored at −80°C. Inoculated samples for heat treatment were sealed in gas-permeable sterile flasks and packed into a Styrofoam carrying case for transport to the MST, about a ½ hour drive from the lab.
Prior to loading any samples, the MST was heated to 38°C for at least a half hour to minimise any spatial temperature variation. The prepared sample plates (see ) were then transferred into individual brown paper bags to mimic the procedure used for treatment of FFRs. The temperature sensitive labels were placed on the exterior of each bag as an indicator of the maximum temperature achieved, and the temperature and humidity data loggers (also in brown paper bags) were placed adjacent to the sample bags to provide environmental data for each test zone (see ). Finally, the door was closed and the treatment cycle initiated.
After treatment, a waiting period of 24 hours was applied at ambient temperatures to mimic the time required to return FFRs to clinical staff. This procedure was applied for inoculated and uninoculated samples. Performance of the analyses to detect both residual virus RNA and infectious (surviving) virus used established methods, as described in detail previously [Citation14]. Briefly, these included: (1) LDA for measuring infectious influenza virus as described above, (2) reverse transcription polymerase chain reaction (RT-PCR) to detect viral RNA by measuring influenza M gene, using a standardised protocol validated in the Bortz lab at UAA [Citation14] as follows: total RNA was purified using RNeasy Viral RNA/DNA kit
(Qiagen) eluted in 50ul ddH2O, and preserved at −80°C. Normalised RNA aliquots (5 µl, or 1/10th of the
RNA sample) were analysed in duplicate by qRT-PCR using Superscript III One-Step (ThermoFisher), on a BioRad CXF96 PCR machine to determine threshold cycle (Ct). Primers binding sites in influenza M gene were: Fwd(+25) AGATGAGTCTTCTAACCGAGGTCG, Rev(−124) TGCAAAAACATCTTCAAGTCTCTG, with Probe(+64) 6-FAM-TCAGGCCCCCTCAAAGCCGA-BHQ-1 (IDT, Coralville, IA). Ct values were averaged and statistically analysed in comparison to negative and positive control inocula by two-tailed Student t-test for significance. Difference in viral RNA quantity between untreated (0’ timepoint) and treated samples was estimated by measured as 2−del.Ct fold change that is 2-to-the power of the difference in PCR cycles.
All post-treatment analyses were conducted under clean lab (BSL-2) conditions.
Results
Testing MST ability to achieve prescribed temperature
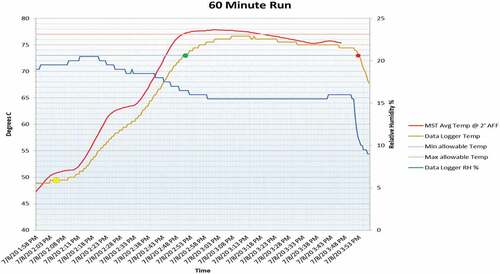
Test operation of the MST was performed on 8–9 July 2020. On 8 July, the 60-min cycle was performed. The conditions were rainy with ambient temperatures between 12 and 13.8 degrees Celsius. The 30- and 90-min cycles were run on 9th July. The weather was cloudy with ambient temperatures between 13.8 and 18.8 degrees Celsius. Inside the MST, the target temperature (75°C) was achieved for each of the three periods. However, the data loggers indicated that the periods at target temperature inside the paper bags were different. For the 60-min run, temperatures were plus or minus 2 degrees of 75°C for a total of 61 minutes, one minute over the goal. For the 30-min test, the data logger recorded temperatures ± minus 2°C for 23 minutes. For the 90-min test, the data logger was within ± 2 degrees of 75°C for 84 minutes. The humidity was uncontrolled but monitored during each cycle. Relative humidity varied from 13% to 23%, dropping as the temperature inside the MST rose. The graph below () shows the compiled data for the 60-min test run. The red line shows the rise of average temperature during ramp up and then levelling off for the 60-min run time. The brown line shows the data logger temperature profile (inside bag) with the dots indicating ± 2 degrees period. The blue line represents percent relative humidity.
Testing treated FFRs for fit factor
The FFRs tested for fit check using the PortaCount instrument went through a total 18 heat cycles in the MST. All of the baseline (new untreated) respirators achieved a maximum real-time fit factor of 200 + . The MST treated respirators also achieved a maximum real-time fit factor of 200+ for each of the tested cycles, demonstrating not just the resilience of the FFRs to repeated heating, but also that there was no measurable effect on fit factor.
Testing treated FFR materials for viral inactivation
We subsequently tested the unit’s ability to heat-inactivate infectious virus in filter materials ().
Figure 8. FFR cloth samples (M1-M4, x-axis) were inoculated with 5 × 104 infectious units (I.U.) (see Methods) of influenza A/WSN/33 (H1N1) virus (WSN Titre, y-axis) and heat treated at 75°C for 0, 30, 60, or 90 minutes followed by 24 hr. at ambient room temperature, and recovered in PBS. Control samples were inoculated for the indicated times, and then left untreated for 24 hours at ambient room temperature. WSN titres were analysed by limiting dilution assay on A549 cells (I.U.). FFR types included 3 M 1870 (M1), KC 46827 (M2), 3 M 1860S (M3), and 3 M 8200 (M4). WSN virus was inactivated in all samples treated with heat for 30, 60 and 90 minutes.
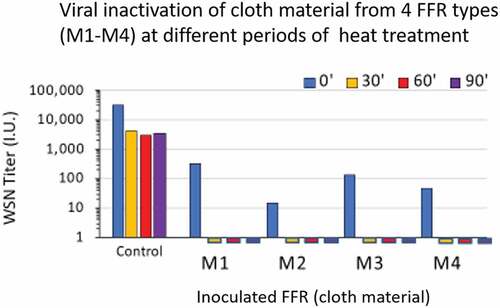
The FFS materials tested included 3 M 1870 (labelled M1 in ), KC 46827 (labelled M2), 3 M 1860s (labelled M3), or 3 M 8200 (labelled M4), using infectious influenza virus WSN as a model enveloped respiratory virus. FFS mask materials were inoculated with a titre of 5 × 104 infectious units (I.U.) of WSN virus and heat treated for 0’, 30’, 60’, or 90’, then held for 24 hours at ambient room temperature, and recovered in phosphate buffered saline for quantification of virus titre (). After 30, 60 or 90 minutes of heating at 75°C, the infectious WSN virus was completely inactivated in all four filter (cloth) materials. A period of 23 minutes was also sufficient to inactivate infectious WSN virus. In fact, all heat periods longer than 23 minutes achieved complete viral inactivation.
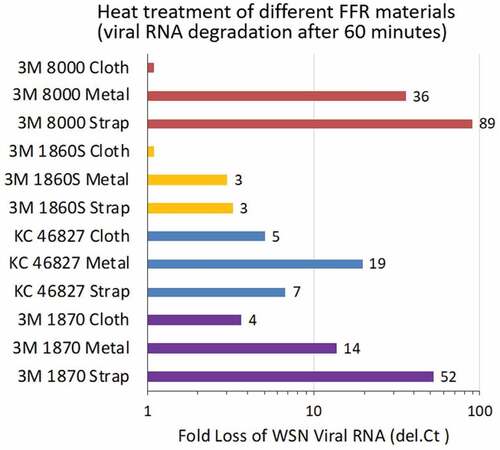
To understand how virus infectivity was degraded, we also analysed residual viral RNA on different FFR materials after 60 minutes of heat treatment at 75°C. The 3 M 8200 and the 3 M 1860 filter material retained viral RNA, and other cloth/filter materials exhibited greater than eightfold degradation of intact viral RNA as measured by quantitative RT-PCR (); range of fold RNA reduction, 3–89). Viral RNA was significantly degraded in all FFR materials (metal nose clip, strap) other than the filter fabric of two of the materials. No infectious virus was recovered from any cloth/filter material.
Figure 9. FFR materials (y-axis) were inoculated with 5 × 104 infectious units (I.U.) of influenza A/WSN/33 (H1N1) virus, and left untreated for 24 hr., or heat treated at 75°C for 60 minutes followed by 24 hr. at ambient room temperature. RNA was recovered and residual WSN viral RNA was measured by quantitative Spackman M-probe RT-PCR in comparison to control (0’, untreated) for each FFR material; fold (log base 2del.Ct) difference in PCR cycle threshold value (number of cycles difference between 0’ untreated and treated for each material yields delta Ct, 2del.Ctn displayed on, x-axis), corresponding to 2 n loss of WSN viral RNA signal.
Discussion
Testing MST ability to achieve prescribed temperature
As measured by the temperature sensors, the MST was successful at maintaining inside temperatures of
75°C for 30, 60 and 90 minutes. However, the data loggers inside the paper bags achieved 75°C for 28, 61, and 84 minutes. This may reflect the variation in temperature sensor readings, thermal inertia of the data loggers, or the insulation properties of the paper bags. Despite variability in temperature/periods inside the bags, time at temperatures where viral deactivation can occur was actually longer. The MST warm-up period provided heating safety factor. Note: some studies show evidence of viral deactivation at temperatures as low as 60°C [Citation7]. A standing question is the ability of the MST to achieve temperature parameters in different seasons and outdoor temperatures. On the test days, the temperatures outside the MST averaged about 15 degrees Celsius (59 degrees Fahrenheit). The system is heavily insulated and designed for use in cold and subzero conditions. Evaluation of MST performance under winter conditions is a topic for future study.
Testing treated FFRs for fit factor
After 18 cycles of heating, there was no measurable effect on fit factor in tested N-95 FFRs. The materials including fabric, fasteners, and straps demonstrated resilience to repeated heating. However, the testing did not include medical staff actually wearing these FFRs during work. The FFRs were only donned for testing. The performance with repeat heating and the added impact from transfers, donning, doffing and normal wear is a subject for further study. Future testing should consider using the evaluation NIOSH uses when approving respirators (42 CFR 84).
Testing treated FFR materials for viral inactivation
In this experiment, we also tested the efficacy of the MST for deactivation of infectious virus. The effectiveness generally of heat treatment on single-stranded RNA viruses is well established. Avian, human H3N2, and human H1N1 influenza A viruses and influenza B virus are deactivated after heat treatment at 55.6°C (132.1°F) for 30 minutes, with evidence of inactivation for shorter times and at higher temperatures [Citation17,Citation20]. Influenza A virus WSN was used as a surrogate virus because it mimics the general biophysical characteristics for heat inactivation of an enveloped RNA virus. It should be noted that no infectious virus was recovered from any cloth/filter material in this study, suggesting that heat treatment was highly effective at inactivating enveloped RNA viruses, including the surrogate WSN virus and as reported in the peer-reviewed literature and preprints, coronaviruses including SARS-CoV-2 [Citation15,Citation16]. The test where samples inside paper bags were heated at 75°C for 23 minutes (plus ramp-up time) demonstrated that even the shortest heating test period in the MST was sufficient to inactivate infectious WSN virus. A topic for further study is effectiveness against other pathogens, and testing of other types of personal protective equipment (caps, gowns, gloves, etc.) also vulnerable to supply shortages.
Conclusion
Overall, the MST functioned as intended, reliably generating the temperatures needed and resulting in FFRs that were free of infectious virus and capable of repeatedly meeting fit requirements.
Decontamination of FFRs is only a crisis capacity strategy but the MST is a resource that can be utilised at ANMC in the event of future shortages. The capacity is adequate to meet the daily needs of the hospital, and the design would accommodate scaling down for smaller hospitals or clinics. In addition to the targeted use of the MST for viral deactivation, and requirements for use in only crisis capacity situations, the limitations to the MST include construction and operational cost. The material cost was almost $60,000.00 and it required many hours of labour to design and construct. However, this may not be as significant given the high costs of standard hospital equipment and the premium placed on FFRs and other PPE during shortages. Consideration, however, should be given to the operational costs, which include labour for one operator, assistants to help with loading and unloading, and the cost for fuelling and renting or purchasing a diesel generator. Counted among the benefits, the ability to provide FFRs that are virus free and the peace of mind this provides to hospital staff knowing that their FFR were sanitised between shifts. In conclusion, we recognise that sterilisation as opposed to sanitising as a method is preferable. However, given the situation at hand and the need for a local solution, dry heat treatment combined with sanitising protocols can provide the Alaska Native Medical Centre with an effective approach to extend FFR supply in a crisis capacity situation.
Availability of Data and Material
Data was generated at the Alaska Native Tribal Health Consortium, Division of Environmental Health and Engineering, and at the University Alaska Anchorage, Bortz Laboratory. The findings are available from the corresponding author on request.
Consent to participate
A recommendation for Dr. Ella Lovejoy to participate in this paper was provided by the Tanana Chiefs Conference, Research and Study Subcommittee on 19 May 2021.
Consent for publication
This manuscript was reviewed and approved for publication by the Alaska Native Tribal Health Consortium, Research Review Committee at their 4 May 2021 meeting.
Ethics approval
This manuscript was reviewed and approved by the Alaska Native Tribal Health Consortium, Research Review Committee at their 4 May 2021 meeting.
Acknowledgments
We would like to acknowledge the ANTHC staff that contributed to the design, construction and testing of the MST. Bailey Gamble, Martin Wortman, Mike Findley, George Wallin, Marchquis Pulliam, Noel Mapili, James Anderson, Dave Reed, Joy Britt, Bailey Richards, Chris Fish, Jason Rutman, Gunnar Hodgson, Kolt Garvey, Amanda Setiawan, Luke George, Martin Wortman, David Beveridge, ShawnTakak, Daniel Andrews, Sonny Vinberg, Brian Berube, Andrew Lean, Vannessa Nunnery, and Ida Norton.Thank you for making this project possible! The UAA Laboratory team extends special thanks to Vera Soloview and Dr. Jason Burkhead (UAA).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Frick A, Watkins A. Summary of COVID-19 Hospitalizations — Alaska, January 1 through December 31, 2020, Alaska Department of Health and Social Services Bulletin No. 1, 2021 Jan 29 2021. http://www.epi.alaska.gov/bulletins/docs/b2021_01.pdf
- Toomey M, Tompkins M. Summary of COVID-19 Deaths — Alaska, January 1 through December 31, 2020. Bulletin No. 2 December 31, 2020, Alaska Department of Health and Social Services Bulletin, 2021 Jan 29 2021. http://www.epi.alaska.gov/bulletins/docs/b2021_02.pdf
- McLaughlin J, Castrodale L. Alaska Section of Epidemiology Bulletin. Summary of COVID-19 Hospitalizations – Alaska, January 1 through October 15, 2020. Bulletin No. 12., 29 10 2020. Available at:http://www.epi.alaska.gov/bulletins/docs/b2020_12.pdf
- Arrazola J, Masiello MM, Joshi S, et al. (2020).COVID-19Mortality among American Indian and Alaska native persons—14 states, January–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(49):1853–9.
- NIOSH-approved N-95 Particulate Filtering Facepiece Respirators 8 2 2022. Retrieved from:https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/n95list1.html
- Implementing filtering facepiece respirator (FFR) reuse, including reuse after decontamination, when there are known shortages of n95 respirators. (2020 19 10 2020). Retrieved from:https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
- Heimbuch BK, Wallace WH, Kinney K, et al. A pandemic influenza preparedness study: use of energetic methods to decontaminate filtering facepiece respirators contaminated with H1N1 aerosols and droplets. Am J Infect Control. 2011;39(1):e1–9.
- Darnell MER, Subbarao K, Feinstone SM, et al. Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV. J Virol Methods. 2004;121(1):85–91.
- Price A, Chu LF (25 03 2020) Addressing COVID-19 face mask shortages (v1.3) [Fact sheet]. anesthesia/Stanford AIM Lab COVID-19 evidence service. Stanford Medicine. https://stanfordmedicine.app.box.com/v/covid19-PPE-1-2
- Hossain E, Bhadra S, Jain H, et al. Recharging and rejuvenation of decontaminated N95 masks. Phys Fluids. 2020;32(9):093304.
- Fit testing procedures (mandatory) part I. OSHA-accepted fit test protocols (Appendix A to §1910.134). U.S. Department of Labor 04 08 2004. Retrieved from: https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA
- PortaCount PRO 8030 and portacount PRO+ 8038 respirator fit testers operation and service manual, march 2015, (appendix C) 03 2015. https://tsi.com/getmedia/76df3dbb-6d8d-4d78-aa24-5aff19e889e9/8030_8038_PortaCountPro_Manual_6001868
- Hoover MD, Lackey JR, Vargo GJ. Independent evaluation of the lepestok filtering facepiece respirator. Pacific Northwest National Laboratory. Prepared for the U.S. Department of Energy under Contract DE-AC06-76RL01830.(07 2021). https://www.pnnl.gov/main/publications/external/technical_reports/pnnl-13581.pdf
- Rupp JC, Locatelli M, Grieser A, et al. Host Cell Copper Transporters CTR1 and ATP7A are important for Influenza A virus replication. Virol J. 2017;14(1):11.
- Gamble A, Fischer RJ, Morris DH, et al. Heattreated virus inactivation rate depends strongly on treatment procedure: illustration with SARS-CoV-2 [Preprint]. Microbiology. 2020. DOI:10.1101/2020.08.10.242206
- Guillier L, Martin-Latil S, Chaix E, et al. Modeling the inactivation of viruses from the coronaviridae family in response to temperature and relative humidity in suspensions or on surfaces. Applied and Environmental Microbiology. (2020);86(18). 10.1128/AEM.01244-20
- Chu CM. Inactivation of haemagglutinin and infectivity of influenza and Newcastle disease viruses by heat and by formalin. J Hygiene. 1948;46(3):247–251.
- Jonges M, Liu WM, van der Vries E, et al. Influenza virus inactivation for studies of antigenicity and phenotypic neuraminidase inhibitor resistance profiling. J Clin Microbiol. 2010;48(3):928–940.
- Jeong EK, Bae JE, Kim IS. Inactivation of influenza A virus H1N1 by disinfection process. Am J Infect Control. 2010;38(5):354–360.
- Zou S, Guo J, Gao R, et al. Inactivation of the novel avian influenza A (H7N9) virus under physical conditions or chemical agents treatment. Virol J. 2013;10(1):289.