ABSTRACT
To assess the effect of eConsultation in providing Orthopaedic Surgery specialist service to patients in Nunavut. A cross-sectional study of 161 Orthopaedic Surgery consultations received from primary care providers (PCPs) in Nunavut via the Champlain Building Access to Specialist service through eConsult (BASETM) service over the 2-year period from January 2017 to December 2018. Data captured were: reason for consultation, impact of advice on referral, perceived value to the PCPs and time spent. eConsult avoided unnecessary in-person consultation 62% of the time while catching 5% of the referrals that would have otherwise been missed. PCP referral behaviour was modified 48% of the time. 94% of eConsults were rated as valuable to PCPs in their practice and 100% of eConsults resulted in actionable advice. Further, eConsults took an average of 15.4 minutes of specialist time to complete, and the mean time from referral to response was 1.4 days. eConsultation spares unnecessary consultation to Orthopaedic Surgery, catches important referrals that would have otherwise been missed, decreases wait time, and may reduce cost in remote healthcare systems such as Nunavut.
KEYWORDS:
Introduction
Access to specialist care in Canada, including orthopaedic surgery, is challenging in today’s health care environment. Wait times for specialist service are growing in Canada due to the inability of limited resources to meet the demands of an ageing demographic[Citation1]. Ontario provides the speciality service medical care to the Baffin region of the territory of Nunavut. The average time between primary care provider (PCP) referral and orthopaedic surgery consultation in Ontario is currently 14.6 weeks, and average time to subsequent intervention is an additional 24.4 weeks[Citation1]. Interestingly, Nunavut does not report wait times and there is no current program in place to track wait times for the territory [Citation1,Citation2]. In addition to being the longest wait times across all speciality services, this is also much longer than clinically agreed upon acceptable time to wait for intervention of 13.5 weeks established via experienced clinician surveys in the field [Citation1–5]. One way to reduce the wait times is through the use of electronic consultation services [Citation6,Citation7]. The Champlain Building Access to Specialist through eConsultation (BASETM) service is a novel communication platform that addresses the wait time between PCP referral and specialist response.
Access to speciality service is even more challenging in remote northern regions of Canada due to significant geographic and economic barriers. With an approximate population of 37,000 distributed over a vast 2-million square kilometre area, Nunavut faces tremendous challenges delivering basic primary care, let alone specialist services [Citation8]. Illustrative of this paradigm, most of the primary care services provided to smaller communities are delivered by nurses and nurse practitioners, with intermittent visits by family physicians, and rare specialist visits confined to larger centres [Citation9]. There are currently no full-time orthopaedic surgeons practicing in the territory of Nunavut. This circumstance exacerbates wait times in accessing specialist care, and often requires travel outside of the territory to cities thousands of kilometres away. As a consequence of this geography, the Government of Nunavut Department of Health reported spending more than a third of its total operational budget on medical travel in 2016–2017 [Citation10]. Utilising novel ways of accessing specialist care in Nunavut, such as the BASETM system, can provide prompt specialist advice with significant cost savings [Citation11].
Previous studies have demonstrated promising results using the BASETM service developed in Ottawa, Ontario. This program allows rapid remote access by PCPs to specialist services. eConsult provides a platform that is secure and asynchronous. While other studies have explored the use of eConsult for the delivery of specialist surgical care [Citation12–14], no previous study has investigated the impact of eConsult on delivery of orthopaedic care on the Nunavut population. The purpose of this paper is to describe the use, benefits, and effect on the need for face-to-face orthopaedic surgery consultation of eConsults from Nunavut processed through the Champlain BASETM service.
Materials and methods
Study design
A cross-sectional analysis of utilisation pattern, question types, diagnoses and outcomes of eConsults from PCPs in Nunavut to orthopaedic surgeon speciality service through electronic consultation from January 2017 to December 2018. Ethics approval for this study was provided by the Ottawa Health Science Network Research Ethics Board.
Setting
Nunavut is a territory in northern Canada with a population of 36,919 [Citation10]. Communities range in size from several hundred to a few thousand people. Each remote community has a health centre run by nurses, with physician consultation available by phone. The majority of tertiary care is provided in Ottawa, Ontario, and the vast majority of orthopaedic care is handled by orthopaedic surgeons at The Ottawa Hospital and the Children’s Hospital of Eastern Ontario.
System employed
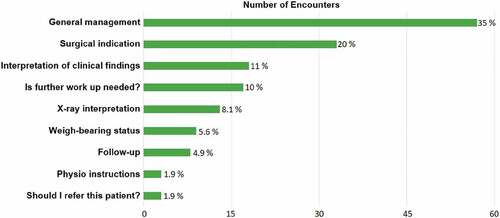
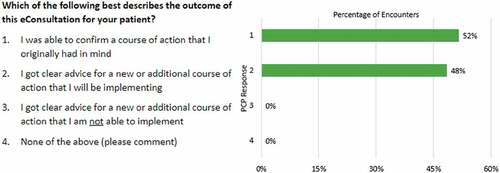
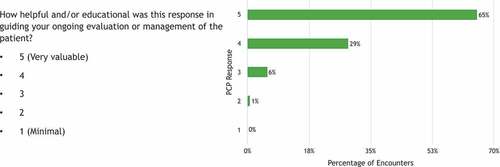
The Champlain Building Access to Specialists through eConsultation (BASETM) service was developed in Ottawa, Canada, by authors AA, CL and EK with assistance from Local Health Integration Network (LHIN) to facilitate remote access to specialist medical services. A protocol for its delivery is previously published [Citation15]. Briefly, this system allows interaction between PCPs and orthopaedic surgeons through a standardised form with additional ancillary information (lab results, imaging, etc.) attached. The orthopaedic surgeon can then offer advice as to (1) treatment decisions and (2) whether further referral or contact is warranted. Each interaction is associated with a mandatory survey () that assesses (1) the utility to the patient, (2) the impact on subsequent in-person consultation, and (3) the utility to the PCP.
Study participants
All 161 eConsults received by orthopaedic surgeons in Ontario from Nunavut completed through the Champlain BASETM service from January 2017 to December 2018 were analysed. All study participant identities were kept confidential and each case was assigned a coded number to ensure anonymity.
Data collection
All data were collected and stored securely in the Champlain BASETM system via robust methods described elsewhere [Citation15]. These data were collected prospectively at the time of consultation and analysed retrospectively. Data collected included: reason for consultation, the written dialogue of the consultation, the length of time to receive a response, the results of the eConsult, time billed, type of PCP (MD vs. NP) and the primary care provider response surveys closing each encounter.
Data review
eConsults were reviewed by two independent reviewers (AS and BM) and categorised by clinical content and type of questions asked using a predetermined classification/taxonomy, whereby clinical content and enquiries were grouped in a reasonable manner and groupings were crosschecked by three trained Orthopaedic Surgeons Where disagreements arose, a third reviewer (WH) was engaged to settle discrepancies. A total of nine types of clinical questions and 27 clinical problem categories were defined.
Results
In 2017 and 2018 a total of 161 consultations originating from PCPs in Nunavut submitted through the Champlain BASETM service were received and reviewed by an orthopaedic surgeon. Out of those, 0.6% (1/161) were from nurse practitioners and 99.4% from family physicians. Paediatric population represents 19% (30/161) and 81% were adults. The average time for the PCP to receive their response after placing a request for consultation was 1.4 days (median 0.5 days). The average amount of time required of an orthopaedic surgeon to respond to these consult requests was 15.4 minutes. Orthopaedic NU eConsults represents 19.5% (161/827) of all eConsults received from Nunavut and 0.6% (161/26,679) of all consults handled by the Champlain BASETM.
The most frequent question types asked were those classed as “general management” (57/161 or 35%), where either multiple questions were asked, or the essential question was “what should I do next?”. The second most common question asked was whether surgery was indicated (33/161 or 20%) ().
The most frequent content of the questions asked related to fracture care (112/161 or 70%), of which ankle fracture (22/161 or 14%) was most common, followed by distal radius fracture (17/161 or 11%), foot fracture (15/161 or 9.3%), clavicle fracture (14/161 or 8.7%) and hand fractures (13/161 or 8.1%) ().
Figure 3. Content of eConsult asked by primary care providers of orthopaedic surgeons. FC = fracture care.

At the end of each eConsult, a mandatory survey was completed by the PCP, answering the three questions shown in . Just over half (52%) of the eConsults confirmed the initial course of action the PCP had in mind, while 48% resulted in a new course of action to be implemented. None of the eConsults resulted in advice that PCPs were unable to implement ().
The consequence of eConsult is shown in ; a schematic representation of the answers to question two. This figure demonstrates that unnecessary referral was avoided in 62% of cases originally planned for referral, while PCP decisions were altered 48% of the time. In addition, two cases not initially intended for in-person referral were recognised as needing more direct attention from an orthopaedic surgeon subsequent to eConsult.
Finally, the eConsult system’s perceived value to primary care providers was ranked as “valuable” and “very valuable” 94% of the time ().
Discussion
The eConsult service studied provides prompt access to orthopaedic specialist services in Nunavut, as evidenced by a 1.4-day average response time to PCP requests for consultation. This is much faster than the Ontario provincial average of 14.6 weeks for in-person consultation, thus offering a tremendous advantage in expediting care of many patients’ orthopaedic problems. This system is clearly advantageous in cases where in-person referral was not ultimately necessary; negating both wait and travel time for the patient, and clinic resources for the orthopaedic surgeon. Furthermore, the average time spent on an eConsult case was 15.4 minutes, which is arguably less than the time spent by the medical system on a typical clinic visit if the time of the surgeon, nurse and clerk are summed and considered.
Our study also demonstrates the impact eConsult has on referral patterns to orthopaedic surgery, as 62% of the cases initially considered for referral were subsequently avoided as a result of the advice offered via eConsult. This has enormous potential to free up surgeons’ clinic time and subsequently shorten waitlists for patients who do require in-person consultation. In addition, nearly half (48%) of the eConsults examined in this study altered the PCPs behaviour, meaning that these patients benefited directly from specialist consultation. Lastly, PCPs have exhibited a high degree of satisfaction with this eConsult service; 94% of users ranking the service as either valuable or very valuable. These results are similar to previously reported studies of non orthopaedic specialities using this eConsult system [Citation12–14].
Another significant finding of this study is that 5% (2/40) of the patients who were initially not considered for in-person referral to an orthopaedic surgeon were subsequently referred after eConsult. These patients represent a cohort who may have otherwise been lost to necessary orthopaedic follow up. One example was a female patient in her 30s who had an ankle injury whose initial X-ray was read as normal and she was treated non operatively. A subsequent e-consult was initiated, and the surgeon recommended full tibia and fibula imaging and diagnosis of Maisonneuve fracture were made. This is an inherently unstable pattern and the recommendation was to send the patient out for surgical management. Missing these fractures could have caused significant ankle instability leading to end stage ankle arthritis and subsequent pain and hardship for the patient [Citation16]. Overall, even though there were only 2 patients, this finding is consistent with previously published data that in which initial in-person consult was not considered but as a result of eCunsult, the referral was subsequently made. Liddy et al previously found that in 3.4% (188 of 5601) of cases PCP did not initially contemplate referral to specialist, but as a result of eConsult, one was subsequently made [Citation17]. The authors summarise that the delay in referral can have significant and detrimental health consequences for the patient.
In the analysis of the “decision to refer to an orthopaedic surgeon” one patient case was labelled as “other”. This patient in question was a patient who had previous surgical fixation of his patella that was performed in Ottawa. This patient had original follow up in Ottawa by the operating surgeon, but was subsequently incarcerated in the local correctional facility in Nunavut. To transport him to Ottawa for follow up appointment required two guards as escorts, adding cost and great logistical effort to the medial travel out of the territory. By using eConsult, this in-person follow up visit was avoided, negating the substantial systemic burden and travel costs associated.
It is interesting to note that the majority of eConsult cases (70%) from Nunavut involved fracture care and general management questions. There are currently no full-time practicing orthopaedic surgeons in the territory. Therefore, access to in-person surgical care is limited to a few weeks each year when visiting surgeons run scheduled clinics, or accomplished at great cost via medical evacuation to a larger centre in the south. This means that even basic management and follow-up questions normally answered by an orthopaedic surgeon in less remote settings, require PCP management. Although no direct studies exist to our knowledge that compare outcomes whether direct care was provided by Orthpaedic Surgeon vs PCP getting advice from surgeon and providing care, recent publications in General Surgery literature show non-inferiority of 94% when comparing telemedicine vs in person consult [Citation18]. In addition, Higgins et al recently published on use of mobile app for home monitoring for post op anterior cruciate ligament reconstruction (ACL) vs conventional in person follow up and found that there was no difference between groups in clinical outcome measures or complication rates [Citation19]. This circumstance further reinforces the ongoing utility of eConsults for this demographic.
Lastly, the use of eConsult offers potential direct cost savings to the system. Although the proper cost analysis for direct and indirect savings is beyond the scope of the present study, simple calculations of cost savings can be inferred. The 2016–2017 Annual Report from the Department of Health in Nunavut [Citation20], states that more than one third of the $371 M health care budget was spent on medical travel ($74 M) and physician and hospital services ($62 M) outside of the territory. In this time period, there were more than 32,000 medical travel related trips, at an average cost of $2,285.31 per trip. This number is even higher if the trip in question is to a larger centre for specialist care, as there are often ancillary costs associated with escorts and interpreters and can be as high as $22,000 per transport [Citation21]. A previous cost analysis of eConsult delivery in Nunavut in the context of specialist care estimated a savings of $1,191.30 per eConsult rendered [Citation10]. In addition, recent published data from interviews of 90 air evacuation decision makers from Nunavut, found that lack of expertise available, i.e. no specialist, was a frequent reason for making a transport decision [Citation21]. If, according to the current study, in-person consultation can be avoided in 62% of the cases, significant savings could be appreciated in the orthopaedic surgery context. We can further speculate that less procedurally-focused specialities may obviate an even greater percentage of otherwise undertaken in-person consults. This may help the health authorities to channel more resources towards remote consults instead of evacuation flight to southern cities.
Remote health care in Arctic region and its challenges are not unique to Canada and Nunavut. Similar challenges of remoteness and access to orthopaedic specialist in Norway were recently published showing cost effectiveness of telemedicine [Citation22]. Although cost effective, this system requires both patient and/or PCP and the specialist to connect at the same time. The advantage of eConsult is that they do not need to have simultaneous time commitment. In addition, the remoteness of the Arctic communities in Canada, Alaska, Norway, Sweden, Greenland and Iceland aided in the curtailing of the COVID-19 pandemic as they fared better than the southern regions of the same country [Citation23], further justifying the use of eConsult as a distancing measure.
There are limitations to the present study. In its current form, only physicians and nurse practitioners may access the Champlain BASETM service, while many small communities rely only on nurses to provide in person full-time health care to the community. This study is also limited by a lack of objective follow up data, as repeat visits for the same patient are not currently a component of the Champlain BASETM service. In addition, there is no method to ensure that the PCPs have implemented the advice given by the specialist. Any study concerning a small population will be somewhat limited by its sample size. Regarding orthopaedic care in Nunavut, this issue is compounded by fact that many orthopaedic cases are ipso facto inappropriate for eConsult (emergencies, clear surgical indications, etc.). These cases are typically handled directly via telephone call to an “on-call” surgeon, where rapid decisions regarding transport and/or initial care can be made.
Universal Health Care systems such as Canada’s face many challenges, not least of which is the issue of long wait times. Therefore, innovative solutions to reduce these wait times are needed. In the Canadian North, this is even more relevant, as distance, remoteness, and low population density make access to specialist health care even more challenging. The eConsult service studied here promises to play a role in reducing wait times and potentially lowering cost associated with travel to seek specialist care.
Conclusions
The eConsult service studied is efficient, spares unnecessary face-to-face consultation with orthopaedic surgery, catches important referrals that would have otherwise been missed, saves the time of patients, PCPs, and specialists, and has enormous potential to reduce health care costs, especially in remote and rural contexts like Nunavut.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bacchus B, Jacque D Waiting your turn: wait times for health care in Canada, 2018 report. Fraser Institute. [ cited 29 Mar 2020]. Available from: https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2018
- Segall RE, Takata JL, Urbach DR. Wait-time reporting systems for elective surgery in Canada: a content analysis of provincial and territorial initiatives. CMAJ Open. 2020 Dec 10;8(4):E844–E851. PMID: 33303570; PMCID: PMC7867034.
- Day B Reducing wait times for health care: what Canada can learn from theory and international experience. 2013. Fraser Institute. [cited 2020 Mar 29]. Available from: https://www.fraserinstitute.org/sites/default/files/reducing-wait-times-for-health-care.pdf
- Neimanis I, Gaebel K, Dickson R, et al. Referral processes and wait times in primary care. Can Fam Physician. 2017 Aug;63(8):619–8. PMID: 28807959; PMCID: PMC5555331.
- Health Quality Ontario. Time to Patient’s First Orthopedic Surgical Appointment. 2018[cited 2020 Mar 29]. Available from: https://www.hqontario.ca/System-Performance/Wait-Times-for-Surgeries-and-Procedures/Wait-Times-for-Orthopedic-Surgeries-including-Hip-Replacement-and-Knee-Replacement/Time-to-Patients-First-Orthopedic-Surgical-Appointment
- Liddy C, Hogel M, Blazkho V, et al. The current state of electronic consultation and electronic referral systems in Canada: an environmental scan. Stud Health Technol Inform. 2015. 10.3233/978-1-61499-505-0-75
- Vimalananda VG, Gupte G, Seraj SM, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323–330.
- Young TK, Chatwood S. Delivering more equitable primary health care in Northern Canada. CMAJ. 2017 Nov 13;189(45):E1377–E1378. PMID: 29133538; PMCID: PMC5687925.
- Marchildon GP, Torgerson R. Nunavut: a health system profile. Montreal (QC): McGill-Queen’s Press; 2013.
- Government of Nunavut Department of Health 2016/2017 Annual report on the operation of the medical care plan [cited 29 Mar 2020]. Available from: https://www.gov.nu.ca/sites/default/files/2016-2017_medical_care_act_annual_report_eng.pdf
- Liddy C, McKellips F, Armstrong CD, et al. Improving access to specialists in remote communities: a cross-sectional study and cost analysis of the use of eConsult in Nunavut. Int J Circumpolar Health. 2017;76(1):1323493.
- Kohlert S, Murphy P, Tse D, et al. Improving access to otolaryngology-head and neck surgery expert advice through eConsultations. Laryngoscope. 2018 Feb;128(2):350–355. Epub 2017 Jun 2. PMID: 28573644.
- Tran CS, Liddy CE, Liu DM, et al. eConsults to endocrinologist improve access to change primary care provider behaviour. Endocr Pract. 2016 Oct;22(10):1145–1150. PMID: 27732095.
- Witherspoon L, Liddy C, Afkham A, et al. Improving access to urologists through an electronic consultation service. Can Urol Assoc J. 2017 Aug;11(8):270–274. PMID: 28798830; PMCID: PMC5542837.
- Liddy C, Rowan MS, Afkham A, et al.Building access to specialist care through e-consultation.Open Med.2013 Jan 8;7:e1–8. PMID: 23687533; PMCID: PMC36545011
- Stufkens SA, van den Bekerom MP, Doornberg JN, et al. Evidence-based treatment of maisonneuve fractures. J Foot Ankle Surg. 2011 Jan-Feb;50(1):62–67. PMID: 21172642.
- Liddy C, Drosinis P, Fogel A, et al. Prevention of delayed referrals through the Champlain BASE eConsult service. Can Fam Physician. 2017 Aug;63(8):e381–e386. PMID: 28807973; PMCID: PMC5555345.
- Pabinger C, Lothaller H, Lorenz A, et al. Telemedicine versus on-site treatment at a surgical university clinic: study of 225 consecutive patients. Int J Med Inform. 2021 Jul; 151:104460 Epub 2021 Apr 30. PMID: 33965683
- Higgins J, Chang J, Hoit G, et al. Conventional follow-up versus mobile application home monitoring for postoperative anterior cruciate ligament reconstruction patients: a randomized controlled trial. Arthroscopy. 2020 Jul;36(7):1906–1916. Epub 2020 Apr 5. PMID: 32268161.
- Nunavut Department of Health Annual Report 2016-2017. [cited 2020 Mar 29]. available at https://www.gov.nu.ca/sites/default/files/health_annual_report_16-17_en.pdf
- McDonnell L, Lavoie JG, Healy G, et al. Non-clinical determinants of medevacs in nunavut: perspectives from northern health service providers and decision-makers. Int J Circumpolar Health. 2019 Dec;78(1):1571384. PMID: 30724715; PMCID: PMC6366434.
- Buvik A, Bergmo TS, Bugge E, et al. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019 Feb 19;21(2):e11330. PMID: 30777845; PMCID: PMC6399572.
- Petrov AN, Welford M, Golosov N, et al. Lessons on COVID-19 from Indigenous and remote communities of the Arctic. Nat Med. 2021 Sep;27(9):1491–1492. PMID: 34426705.