ABSTRACT
Introduction: Freezing cold injuries (FCI) are a common risk in extreme cold weather warfare operations. The Norwegian Armed Forces (NAF) have the expertise and capabilities in education and training for warfighting capabilities in the Arctic. Nevertheless, a substantial number of Norwegian soldiers sustain freezing cold injuries annually. The aim of this study was to describe the FCI in the NAF, the associated risk factors and clinical associations.
Methodology: The subjects for the study were soldiers registered with FCI in the Norwegian Armed Forces Health Registry (NAFHR) between January 1st 2004–July1st 2021. The soldiers answered a questionnaire regarding background, activities at the time of injury, description of the FCI, risk factors, medical treatment and any sequelae from their FCI.
Results: FCI in the NAF were most frequently reported among young conscripts (mean20.5 years). Hands and feet are most often injured (90.9%). Only a minority (10.4%) received medical treatment. The majority (72.2%) report sequelae. Extreme weather conditions was the most important risk factor (62.5%).
Conclusions: Most soldiers had the knowledge to avoid FCI, but they were injured anyway. It is concerning that only one in 10 injured soldiers received medical treatment after diagnosed with FCI, increasing the risk of FCI sequelae.
Introduction
Despite a long history of human existence in cold environments and a general appreciation of protective technologies to survive the cold, there are still many spectacular examples of human failure, often in the setting of military conflicts. Hannibal’s crossing of the Alps about 218 BC [Citation1], the two World Wars in the twentieth century and the Falkland Conflict of 1982 [Citation2] all illustrate the relevance of the cold in both ancient and modern times. In a non-military setting, the number of injuries due to cold is increasing, especially in those who partake in winter sports, mountaineering or Alpine and Nordic skiing [Citation3].
The Norwegian boreal winter climate offers arctic conditions, especially in the northern part of the country, where many military field operations are conducted. Changes in wind, humidity and temperature impose additional dimensions of external stress on military personnel working under already harsh conditions [Citation3].
The main task of the Norwegian Armed Forces (NAF) is to protect Norway from external threat or attack. Norway is also a member of the North Atlantic Treaty Organization (NATO). Norway hosts NATO's Centre of Excellence-Cold Weather Operations (COE-CWO) and acts as the main provider and coordinator of expertise and capabilities in the area of Cold Weather Operations in NATO [Citation4]. This includes specific education, training and medical knowledge for warfighting capabilities in the Arctic. A vital part of the Arctic military strike force is a cold weather medicine component, with a focus on prevention, diagnosis and treatment of Cold Weather Injuries (CWI).
Freezing Cold Injuries (FCI) are caused by tissue temperature below −0.55°C. When tissue reaches temperatures below −0.55°C, ice crystals form within the cells. This causes a cellular shift of electrolytes with cell membrane lysis and death. The inflammatory process that develops can cause tissue ischaemia and necrosis [Citation5–7].
Soldiers with peripheral freezing injuries can experience life-long changes in microcirculation and disruption of neurological functions [Citation8]. Long-term sequela are still not thoroughly understood, but some of the consequences following a freezing cold injury are cold hypersensitivity, chronic pain, sensory loss and osteoarthritis [Citation9,Citation10]. The consequences of the soldier’s personal health can be severe and render them unfit for continued service but will also have consequences for civilian occupation and possibly reduce quality of life if severely injured [Citation6].
The treatment options for FCI are limited; these are often regarded as experimental or characterised as off-label treatment [Citation11,Citation12]. Since no evidence-based therapy is available, prevention plays an important role in FCI. However, effective prevention is also hampered by the poor understanding of individual risk factors and environmental risk factors.
The Norwegian Armed Forces – Joint Medical Services (NAF-JMS) is the central organisation responsible for medical matters in the NAF, including FCI [Citation13]. The Joint Medical Services also serves as caretaker for the Norwegian Armed Forces Health Registry (NAFHR), containing health data from all Norwegian military personnel, including information regarding all types of injuries in the NAF. The primary objective of the registry is to identify risks linked to the different services and provide a foundational tool for research and data analysis [Citation14–16].
The aim of this study was to describe the Freezing Cold Injuries reported in the Norwegian Armed Forces Health Registry, and the associated risk factors and clinical associations.
Materials and methods
Freezing cold injury diagnostic criteria
In principle, FCI occurs at temperatures below the freezing point of the tissue, which is found to be
−0.55°C [Citation3,Citation17]. Local frostbite with a specific “frostbite pathophysiology” does not occur at temperatures above the freezing point of the tissue. Symptoms arising at higher tissue temperatures than −0.55°C are not regarded as FCI. Symptoms, for instance, blisters arising from FCI, tend to be in specific regions, like the tip of fingers, tip of toes and exposed areas in the face. A possible challenge in diagnosing frostbite could be that the symptoms fluctuate, making an exact diagnosis difficult. The FCI diagnosis in this study has been set by military doctors trained in cold weather injuries according to the clinical criteria used in previous research ().
Table 1. Clinical criteria based on levels of frostbite (19).
highlights the importance of blisters in the staging criteria. In this study, we have, therefore, used the presence of blister and the colour of the blister content to define FCI grades 1, 2 and 3. FCI has numerous clinical pictures, and this study categorises the classification into four different degrees/levels analogous to the classification of burn injuries [Citation18]. If only the dermal layer is involved in an FCI, the injury has traditionally been regarded as a superficial FCI, subdivided into grade 1 and grade 2. A freezing process involving the subcutaneous layers and/or deeper into muscles, tendons and bones is classified as a deep FCI, subdivided into grade 3 and grade 4 [Citation5].
Study subjects
From 1 January 2004– 1 July 2021, 2,387 persons were registered with different degrees of freezing cold injuries in the NAFHR [Citation19]. This study is based on data from all personnel registered with the International Statistical Classification of Diseases and Related Health Problems (ICD-10) diagnosis codes related to CWI. Demographic variables and pre-service data were collected from the soldiers’ medical files. As the ICD codes do not impart information about the circumstances of the injury, this information was collected through a survey distributed to personnel registered with freezing cold injuries in the NAFHR.
The NAFHR is a Norwegian central health registry that contains data from NAF personnel, including conscripts as well as civilian and military staff employed by the Armed Forces [Citation9,Citation18]. The types of personal data that can be processed are defined by sections 1–8 of the regulations concerning the collection and processing of information in the NAFHR [Citation20]. Pursuant to the regulations, the registry may contain personal information, administrative information, medical information and workplace information. The information in the Armed Forces Health Registry is drawn from NAF medical records and HR systems, as well as internal health surveys. The Ministry of Defense is the data controller, and the NAF-JMS is the data user. Medical and operational responsibility lies with the Institute of Military Medicine and Epidemiology (NAF-JMS), at Sessvollmoen garrison outside the capital Oslo.
Data from the health registry contribute increasingly to research seeking to identify health injuries during, or as a consequence of, military service [Citation19,Citation21,Citation22]. Data regarding place of service were collected from the Armed Forces Personnel and National Service Center (FPVS).
The inclusion criteria were to have sustained a FCI during service in the NAF during the given period, based on ICD codes.
Exclusion criteria included refusal to participate, inability to give informed consent and non-compliance soldiers.
Institutional review board and mandatory ethical approval was granted (REK 278429) before the database was accessed, identifying eligible patients for study. Written informed consent was obtained from all participants.
In earlier years, conscription in Norway was compulsory for men 19 years of age and above. The annual number of conscripts in the study period varied between 7,156 and 10,322 yearly. From 2010, both men and women were subjected to conscript duty, but it was still compulsory only for men. On 1 January 2016, ordinary conscript duty was made compulsory for both men and women born after 1997. Conscript duty in the NAF usually lasts for 12 months.
The proportion of women among the conscripted soldiers increased from 3.6% in 2004 to 35.8% in 2021. Because of the shift in gender proportion across the years of the survey, gender-specific incidence will be grouped into three periods: 2004–2010, 2011–2015 and 2016–2020.
Less than 60% of the conscripts perform their service in the coldest areas in Norway. The anticipated proportion of soldiers expected to be operating under extreme high risk of FCI is, therefore, regarded to include one-third of the total number of conscripts.
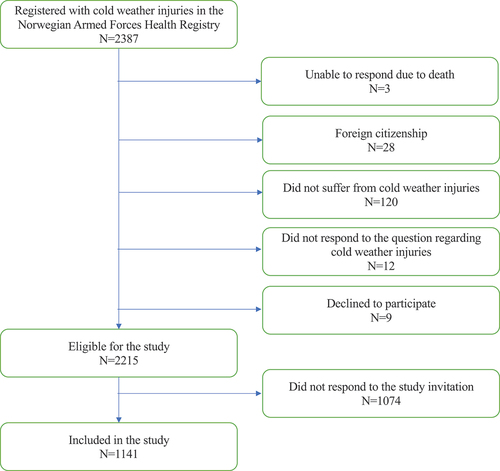
A total of 2,387 soldiers in the NAFHR met the inclusion criteria. Three soldiers had died by the time of the survey, and 28 soldiers were excluded due to foreign citizenship. Furthermore, 120 soldiers reported that they did not have a history of FCI, 12 did not respond to the question regarding FCI and 9 soldiers were unwilling to participate. This left 2,215 soldiers were eligible for the study. Of these, 1,074 did not reply to the study invitation, leading to 1,141 soldiers (51.5% response rate) to constitute the basis for this study ().
Measures
A questionnaire was developed to collect data on the soldier’s background: activities at the time of injury, description of the FCI, risk factors including equipment and weather, medical treatment received and if they experience sequelae from their FCI. The relevant content of the questionnaire is displayed in .
Table 2. Selected questions in the FCI questionnaire for this study.
The questions were validated through pilot testing among scientists in the field (n = 4), conscripts (n = 3), officers (n = 3) and medical doctors (n = 5). Additionally, questions from a previous frostbite study were used. The questionnaire also include other instruments such as the European Quality of Life Scale (EuroQol) with five dimensions of health status to quantify health-related quality of life (EQ-5D) [Citation21] and Patient Subjective Symptom Score (PSSS) to describe the most important subjective symptoms following a primary frostbite; pain, hypersensitivity to cold, numbness of fingers and declined sensitivity of touch [Citation11] (). The questionnaire consisted of multiple-choice questions leading to a higher number of answers than the total number of participants in some cases.
The questionnaire was distributed on 1 December 2021 using the software Confirmit. Reminders were sent after 5 and 8 weeks. A third reminder was published on NAF’s Instagram account and on NAF’s local internet site.
Data measurements and handling
Data collection at NAFHR was performed according to the regulations of the registry [Citation19]. All military data within NAFHR are stored on a secure server, and the server-services are provided by the Cyber Defense Department of the NAF. Only approved study workers were given access to the database.
Study participants were given a study identification number to protect their identities when their data was extracted from NAFHR. The list that connects patient identity to their study identification number was kept and stored on a separate NAFHR-data server. The identification list was not, at any time, available to the researchers.
NAFHR distributed the questionnaire to the participating soldiers through a secure digital communication (DigiPost) by FPVS. Responses were given on a digital form and NAFHR transferred data to a secure registry server. The researchers were not involved in the data coding and collecting process.
Data from the questionnaire was added to previous recorded health data within the NAFHR before the extraction of an anonymous dataset for statistical analysis.
Statistical analyses and study power calculation
With a margin of error of 5%, a confidence level of 95% and a heterogeneity of 50%, we needed a minimum sample of n = 370 to represent the 8,860 potential population of frostbitten soldiers for adequate study power [Citation22]. Only injured soldiers seeking medical attention in the primary military healthcare are found in the registry. A previous survey [Citation6] has revealed that only 25% of the injured soldiers were found in the registry, calculating the potential population of soldiers with an FCI to be 2,215 × 4 = 8,860.
Descriptive statistics were carried out using cross-tabulation and frequency analyses. For between-group analyses, Pearson chi-square tests and Fisher exact tests were used for categorical variables while independent sample t-tests were used for continuous variables. The significance level was set at p < 0.05. The analyses were conducted using SPSS V.29.0 for Windows.
Results
Frostbite injuries
The participants were mainly men (72.8%) at a young age (mean 20.5 years) with a rather short period of military service (6 months or less, 65.5%), mainly conscripts (80.5%).
More than half (55.3%) of all FCIs were reported from four garrisons in the coldest parts of northern Norway (Setermoen, Bardufoss, Høybuktmoen and Skjold). Regarding severity of the injury, 44.3% reported a grade 1 FCI, 19.3% reported a grade 2 and 6.5% reported a grade 3 FCI. One-third of the soldiers (29.9%) did not respond to the parameters needed to grade their FCI (). As the survey included personnel from all types of services in the NAF, the gender- and year-specific incidence only presents the incidence among conscripts.
Table 3. Basic characteristics of the participants.
The overall incidence in our data is 0.61% as displayed in . Four out of five FCI soldiers were injured during their conscript duty (80.4%). Since the proportion of women among the conscripts varied greatly within the study periods, an incidence calculation was performed on the selected periods stratified by gender for all the Norwegian conscripts. The overall incidence is 0.61 with higher incidence among women (1.02) compared to men (0.51) in all three periods of the study ().
Table 4. Gender and year-specific incidence of FCI among Norwegian conscripts.
1) The total number of injuries in represents the injured soldiers who have responded both to gender and year of injury
These numbers are only applicable for conscripts, but injuries happen in all personnel groups. According to this adjustment, the more reliable incidence among Norwegian conscripts is around 2.0%.
Risk factors associated with FCI
Most of the soldiers report sufficient knowledge to avoid (62.2%) and detect (63.3%) FCI. A majority of the injured soldiers used snuff (sniffing tobacco) (53.3%) and/or were smoking (22.4%) at the time of the FCI. Only a minority report to have ever had reported a previous FCI as a potential risk factor (3.1%). A total of 898 soldiers (93.6%) used the regular layer-based clothing provided by the NAF. Only 5.1% used civilian clothing or a combination of both. There was no association between the type of clothing and the degree of FCI (p = 0.811).
Among other risk factors, the soldiers most often report too little sleep (16.8%), too little rest (16.3%), wet clothing (15.9%), too little nutrition (13.1%) and excessive physical work activity (9.9%), however, with no associations between these factors and the degree of FCI (p > 0.222) ().
Table 5. Factors associated with the frostbite severity.
The soldiers were also asked about their self-perceived reasons for the FCI. Extreme weather conditions were the most important factor (62.5%), followed by commanders’ misjudgement (38.6%), their own misjudgement (23.7%) and wrong use of clothing (22.3%). Commanders’ misjudgement and commanders' lack of knowledge and training were positively associated with the most severe grade of FCI’s (p < 0.005, ).
Clinical associations with frostbite severity
Most of the soldiers had injured their hands (49.7%) or feet (41.2%). FCI to hands led most frequently to a grade 2 FCI (61.4%), while the feet were most frequently reported with a grade 3 FCI (52.7%) (). A total of 13.9% of the soldiers were not diagnosed correctly when they first visited the medical personnel in the NAF. Most of the soldiers (84.8%) were back on duty in less than 2 weeks after the FCI.
Table 6. Clinical associations with frostbite severity.
Only a minority of the injured soldiers (15.1%) received medical treatment for their FCI. Those few who did were most often treated in a primary military health care (6.6%) while 3.2% were treated in a hospital and 2.7% were treated by their civil general practitioner. Medication was mainly given for pain/inflammation and anticoagulation, most often for the most serious FCIs. The majority (72.2%) reported sequelae from their FCI. The most frequently reported long-term effects of FCI were cold hypersensitivity (66.4%) followed by pain (34.5%) and paraesthesia (24.1%). Nevertheless, most of the soldiers (97.0%) stated that their health status at the time of the survey was good ().
Discussion
A number of FCI in the NAFHR were most frequently reported among young, less experienced soldiers during their conscript duty. Hands and feet were most often injured, and only a minority have received medical treatment for their FCI. The majority of the injured soldiers had sequelae from their FCI.
Epidemiology
This survey is descriptive in nature and does not primarily focus on the occurrence of FCI, complicating incidence calculations. The overall incidence in our data corresponds to the annual incidences reported in other studies [Citation7,Citation23,Citation24], although the true incidence may be as high as 8% given that previous studies have indicated significant under-reporting as only 25% of the frostbitten conscripts report their injuries to the medical doctor. Some soldiers are unaware of their injuries, especially if they are not severe and debilitating.
Sullivan-Kwantes et al. found a doubling in the incidence of CWI in a group of Canadian soldiers who were individually examined by a physician compared to self-reported rates of injury [Citation25]. It is known that commanders do not want to report injuries as this may be constructed to be a reflection of poor leadership and training of the soldiers. Some soldiers do not want to get their FCI registered due to their wish to continue their military service and to get their promotion. Thus, we can conclude that most military studies relying on soldier, unit and medical reporting are underestimates of the true rates of CWI.
However, the anticipated proportion of conscripts operating under freezing weather conditions is regarded to be only one-third of the total number of conscripts. Our numbers are therefore not the true population under risk, as a substantial part of the soldiers do all their conscript duty in regions where they do not encounter freezing temperatures. According to the adjusted (1/3) of conscripts under specific risk for freezing weather conditions, the more reliable incidence among Norwegian conscripts may be 2.0% in line with previous research [Citation6,Citation23] and found in comparable studies [Citation24,Citation26].
There is an overall higher incidence of FCI rate among women (1.02%) versus men (0.51%) throughout the whole period 2004–2020, although the majority of soldiers suffering from FCI are men (71%) due to more men than women in the army.
The overall incidence of FCI is highest in garrisons having the largest groups of personnel serving in the coldest parts of northern Norway. The variation in incidence according to the local climate is in accordance with a previous study [Citation6]. The Norwegian winter climate in the inland areas and in the far north reach −30 to −40°C in the winter, with −51.2°C recorded as the lowest measured temperature. To some extent, the rate of FCI is expected, due to the harsh weather condition in these areas, which is held to be the most frequent (62.5%) self-perceived reason for FCI.
Extreme weather conditions are probably one of the most important risk factors for FCI, and we expected that the rates of FCI would be high in the high north. However, our results show a tendency that FCI reported at the low-risk garrisons tends to be more severe, although at a non-significant level. This apparent difference might be due to less awareness and lower vigilance about FCI in these areas in comparison to the north where education and awareness about FCI has a high priority.
Decisions about which FCI-related ICD codes to include in the study are challenging due to a potential misclassification by the treating physician when the FCI occurred. The inclusion of soldiers in an FCI dataset with the diagnostic codes T68 (hypothermia) and T69 (other condition caused by reduced temperature) might also be questioned. To ensure that only soldiers with an FCI were participating in the study, the soldiers were asked whether they had suffered from an FCI while serving in the NAF. All participants replying no to this question were excluded from the study.
The risk of recall and information bias must be taken into account when interpreting the results from this study. The self-assessment of FCI by the conscripts for the study is a major concern to the validity of such data. The reliance on this self-assessment might be a challenge since only 63% reported they would be able to recognise FCI.
The authors are aware of the threat to the reliability of the data since 120 soldiers (5% of the cohort) on the NAFHR who recorded as having sustained an FCI reported that they had not. On the other hand, a 5% misclassification could also be expected due to inaccuracy in the diagnostic work among young military doctors, particularly if the diagnosis is worked out while being under manoeuvre out in a tent in the dark arctic winter night conditions. Bearing in mind all the factors that might complicate the initial diagnose, a 5% level of incorrect diagnosis still permits reasonable estimates from the NAFHR.
As some participants were treated in more than one place and received more than one treatment, the total number of treatments and treatment levels may influence (overestimate) the number of participants receiving frostbite treatment.
Risk factors associated with FCI
Regarding risk-factors in general, most of the soldiers stated that they were aware of the important FCI threats, and they also knew how to avoid FCI. The soldiers are educated in cold weather injuries and especially FCIs. Having received this instruction, we expected the soldiers who say that they were aware of FCI threats to effectively avoid injury; however, there is clearly a difference between knowledge and the actions that come from training experience.
Their young age and lack of outdoor experience, combined with an eagerness to perform as conscripts/soldiers may be part of the explanation of why they experienced FCI despite this awareness. As most of the injuries are registered during national service, it naturally involves people of young age. The reasons for this group to get injured are multifactorial, but less training and experience with cold weather are highly relevant for this group.
On the other hand, the reporting of extreme weather conditions as being the most important risk factor indicates that it might be challenging to totally avoid FCI in military training.
Nicotine, disturbance of peripheral circulation (Raynaud) or previous FCI might lead to peripheral vasoconstriction [Citation27], which might be a risk factor for FCI. In addition to the vasoconstriction, there might also be a risk of FCI to the fingers when smoking or preparing tobacco in very cold conditions. However, these factors were not associated with the severity of FCI. This conclusion must be drawn with caution due to small numbers failing to present the differences found in a statistically significant manner.
As vaping only has existed for a short time and e-cigarettes with nicotine are forbidden in Norway, this was not applicable to ask about in this study [Citation28]. Smoking has also been forbidden in public areas in Norway since 2004, and since then, this is a less common source of nicotine. Snuff, on the other hand, is widely used in Norway and among military personnel, and highly relevant in FCI injuries. Nicotine per se has a vasoconstrictive effect; however, the casualties between FCI and Nicotine use have not been documented.
Most Norwegian soldiers use the Armed Forces layer-based clothing that is in line with the principles of cold weather clothing protection [Citation29,Citation30]. However, the data in this study do not describe the specifics of hand and foot protection, which are more pertinent and, if isolation is poor, could lead to FCI [Citation31]. To draw conclusions regarding clothing, further investigations are needed.
Clothing, alongside rest, sleep, nutrition and level of physical activity were not found to relate to the severity or degree of injury in this study. However, previous studies have explored possible associations between these factors and incidence rather than the severity. This makes it challenging to compare the findings of this study with existing evidence [Citation24,Citation32,Citation33], and conclusions cannot be drawn.
The soldiers admit that their own misjudgements could be a reason for FCI although they hold commander’s lack of knowledge, training and misjudgement as significant risk factors for FCIs. However, any conclusion regarding the commander’s military performance must be drawn with extensive caution due to potential bias from the injured soldier.
Clinical associations with frostbite
In accordance with previous studies, hands and feet were most prone to FCI in the present study [Citation34]. These sites are also more frequently reported among the more serious grade 2 and 3 FCI; thus, hands and feet should be the focus in FCI prevention.
It is difficult to predict the outcome of frostbite [Citation6,Citation8,Citation12,Citation35,Citation36]. It is also a medical challenge that only 15.1% of the soldiers with FCI received medical treatment for their injuries. As one could expect, a higher proportion among the most injured soldiers seek medical attention. This could in part be explained by the fact that no evidence-based treatment is available, and the most injured patients are more likely to be offered off-label or experimental treatment in the hospitals [Citation8,Citation12,Citation37].
It is a concern, from the medical point of view, that most of the soldiers with FCI suffer from late effects that might last for the rest of their life. The group of injured personnel is mainly young (20 years), and the injury might have an impact on their ability to continue service and may lead to limitations in their life also outside the army, both personally and professionally.
Sequelae from FCI seem to be equally distributed among the different grades of FCI. This indicates that frostbite is initially perceived as mild, and may also result in chronic health ailments in correspondence with previous studies. Cold hypersensitivity might be regarded as a minor complaint, although our clinical experience indicates that this can lead to discomfort and cause disability. Despite this, most of the soldiers define their general health as very good. This may indicate that the symptoms they experience do not have a large impact on their daily life and work ability or that they perceive the complaints as the price to pay for their performance as a soldier.
The clinical data in this study might be challenged. Medical records are for clinical use rather than for research purposes and are imported directly into the NAFHR. The nature of these clinical data might not be optimal for science as they are mostly used to track events in treatment and follow-up of patients. As these clinical raw data are directly imported to the NAFHR and made available for this study, the registered data are dependent on the accuracy of the doctors. We acknowledge the challenge for doctors in distinguishing between FCI and other conditions such as chilblains, transient neuropraxia and blisters due to chafing that commonly occur in military personnel during cold weather exercises. The authors are therefore concerned about whether all diagnoses have been set correctly. Work needs to be done on the NAFHR to improve the reliability of data entry for future studies.
Strengths and limitations
The main limitation of this study is the fact that the selection for this survey might be biased as 25% of frostbitten soldiers do not report their FCI and are therefore not available for this study [Citation6]. This could have led to an under-reporting of mild FCIs, leading to a larger proportion of severe FCI in the sample, compared to the population of freezing cold injured soldiers. Some of the soldiers might also have been misclassified or enlisted with a wrong diagnosis or condition due to challenges in classification of FCI [Citation5]. This misclassification is, however, expected to be limited as all participants had to confirm an FCI to be included in the study.
In our experience, diagnostic code T68/T69 has been misused for personnel with actual FCI; therefore, injuries coded as T68 and T69 were added to the inclusion criteria. This may have led to an overestimation of FCIs.
Another limitation of this study is the response rate of 52% which means that we, in combination with the 75% who did not report their FCI to the registry, only have a sample representing 13% of the target population. A power calculation revealed, however, that we have sufficient power in the study as we needed a sample of 370 to represent the target population of 8,860 for sufficient power. We, on the other hand, cannot rule out the possibility that there is an overrepresentation of soldiers suffering from late effects of their FCI eager to share their experience with the researchers.
There is a risk of information bias in this study. While self-reported data can be a useful tool for researchers, there are some limitations to consider. Participants may be inclined to present themselves in a favourable light, which can lead to inaccuracies in self-reported data. They may provide responses that are socially acceptable or what they think the researcher wants to hear, rather than the truth. This is, on the other hand, limited by the fact that the data were collected anonymously and without the researcher present while filling in the questionnaire. There is also a risk of recall bias where participants may not remember or may misremember certain details about their attitudes, behaviours, or experiences. This can lead to inaccurate or incomplete data.
Self-reported data may be limited to the questions that are asked in the survey or questionnaire. It may not capture important nuances or factors that are relevant to the research question. Participants may also have misinterpreted the questions or provided ambiguous responses, which can lead to misunderstandings or inaccuracies in the data. Overall, while self-reported data can provide valuable insights into attitudes, behaviours and experiences, researchers should be aware of its limitations and consider supplementing it with other sources of data whenever possible [Citation38].
The validity and reliability of the questionnaire study design need specific attention. There will always be a potential to improve the coding, layout and content. In this study, we used the research group’s experience and the expertise in the NAF when developing the questionnaire. The pilot testing of the questionnaire increased the content validity of the study [Citation6,Citation8]. Additionally, the template for this study is based on a validated study used among military personnel [Citation6]. This study also profits from the experience in questionnaire surveys at NAFHR.
Future research
The data in this study may be criticised due to the potential biases as already outlined in the discussion. For future research, it is important to improve the clinician’s assessment as the accuracy of the FCI diagnosis is challenged by the rather unreliable clinical signs [Citation39]. The grading of the FCI should be done in relation to the onset of the FCI to get more reliable data. Information bias should be reduced, and the inaccuracy of the respondent’s subjective assessment of an FCI should be avoided.
However, the data in this study bring forward useful information in a field where most studies suffer from flaws in the current data collection system. The present study is therefore the most needed source of knowledge on the way to develop a reliable registry that could offer the international community more valid data on FCI in the future.
Conclusion
This descriptive study adds to the existing knowledge of risk-factors leading to FCI by taking the injured soldiers’ perspective. This further strengthens the understanding that it is difficult to completely avoid FCI in military training, as the injuries are associated with the very nature of the military training, namely, extreme weather conditions. The high number of soldiers reporting late effects from FCI, and the lack of evidence-based FCI therapies is a major concern from the medical point of view. More targeted education to the soldiers and the commanding officers might improve role-modelling among the youngest military leaders.
Authors’ contributions
TS and AJN conceived the study, and AEK and TS conducted the initial and final analyses. TS and AJN drafted the initial version of the paper. All authors gave input into how to interpret and structure the findings and reviewed subsequent versions. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the Regional Committee for Medical and Health Research Ethics (REK 278,429). Informed consent was obtained from all participants.
Availability of data and materials
The raw dataset is not available due to Norwegian privacy regulations. Applicants for any data must be prepared to conform to Norwegian privacy regulations.
Acknowledgments
The authors wish to thank the Norwegian Armed Forces Health Registry and the Armed Forces HR and Conscription Centre for contributing to the data for the study. We also appreciate all valuable input and discussions with our colleagues at the Joint Medical Services and at the UiT – The Arctic University of Norway.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Wikipedia. Available from: https://en.wikipedia.org/wiki/Hannibal%27s_crossing_of_the_Alps
- Golden FSC, Francis TJR, Gallimore D. Lessons from history: morbidity of cold injury in the royal marines during the Falklands conflict of 1982. Extreme Physiol Med. 2013;2(1):1–13. doi: 10.1186/2046-7648-2-23
- Handford C, Buxton P, Russell K, et al. Frostbite: a practical approach to hospital management. Extreme Physiol Med. 2014;3(1):1–10. doi: 10.1186/2046-7648-3-7
- https://no.wikipedia.org/wiki/Forsvarets_vinterskole
- Norheim AJ, Sulliwan-Kwantes W, Steinberg T, The classification of freezing cold Injuries - a NATO research task group position paper. Int J Circumpolar Health. 2022;82. (In press). doi: 10.1080/22423982.2023.2203923
- Norheim AJ, Borud E Frostbite in the Norwegian armed forces. Tidsskrift for den Norske laegeforening. 2018;138(14). doi: 10.4045/tidsskr.17.1070
- Ikaheimo TM, Hassi J. Frostbites in circumpolar areas. Glob Health Action. 2011;4(1):4. doi: 10.3402/gha.v4i0.8456
- Norheim AJ, Mercer J, Musial F. A new treatment for frostbite sequelae; Botulinum toxin. Int J Circumpolar Health. 2017;76(1):1273677. doi: 10.1080/22423982.2016.1273677
- Arvesen A, Rosén L, Eltvik L. Skin microcirculation in patients with sequelae from local cold injuries. International Journal Of Microcirculation. 1994;14(6):335–342. doi: 10.1159/000178852
- Hutchison RL. Frostbite of the hand. J Hand Surg. 2014;39(9):1863–1868. doi: 10.1016/j.jhsa.2014.01.035
- Norheim AJ, Mercer J, de Weerd L. Botulinum Toxin a in the treatment of frostbite sequelae – results from a blinded, early-phase, comparative trial. International Journal Of Circumpolar Health. 2023;82(1). (In press). doi: 10.1080/22423982.2023.2189556
- Poole A, Gauthier J, MacLennan M. Management of severe frostbite with iloprost, alteplase and heparin: a Yukon case series. CMAJ Open. 2021;9(2):E585–E91. doi:10.9778/cmajo.20200214.
- https://www.forsvaret.no/en/organisation/joint-departments
- Fadum EA, Fønnebø V, Borud EK. Presence of minor and major mental health impairment in adolescence and death from suicide and unintentional injuries/accidents in men: a national longitudinal cohort study. J Epidemiol Community Health. 2017;71(1):19–24. doi: 10.1136/jech-2016-207656
- Strand LA, Martinsen JI, Fadum EA, et al. External-cause mortality among 21 609 Norwegian male military peacekeepers deployed to Lebanon between 1978 and 1998. Occup Environ Med. 2017;74(8):573–577. doi: 10.1136/oemed-2016-104170
- Strand LA, Martinsen JI, Borud EK. Cancer risk and all-cause mortality among Norwegian military united nations peacekeepers deployed to Kosovo between 1999 and 2011. Cancer Epidemiol. 2014;38(4):364–368. doi: 10.1016/j.canep.2014.04.003
- TR HK, Robertson G, Porter A. Freezing and non-freezing cold weather injuries: a systematic review. Br Med Bull. 2016 Mar;117(1):79–93. Epub 2016 Feb 12. PMID: 26872856. doi: 10.1093/bmb/ldw001
- Imray C, Grieve A, Dhillon S. Cold damage to the extremities: frostbite and non-freezing cold injuries. Postgrad Med J. 2009;85(1007):481–488. doi: 10.1136/pgmj.2008.068635
- Forsvarets helseregister. [ Available from: https://www.forsvaret.no/forskning/forsvarets-helseregister-ime
- Norheim AJ, Borud EK. Frostbite in the Norwegian armed forces. Tidsskr Nor Legeforen 2018 doi: 10.4045/tidsskr.17.1070. 2018.
- EuroQol G EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
- Taherdoost H Determining sample size; how to calculate survey sample size. International Journal Of Economics And Management Systems. 2017;2.
- Mäkinen TM, Jokelainen J, Näyhä S. Occurrence of frostbite in the general population–work-related and individual factors. Scand J Work Environ Health. 2009;35:384–393. doi: 10.5271/sjweh.1349
- Lehmuskallio E, Lindholm H, Koskenvuo K, et al. Frostbite of the face and ears: epidemiological study of risk factors in Finnish conscripts. BMJ. 1995;311(7021):1661–1663. doi: 10.1136/bmj.311.7021.1661
- Sullivan-Kwantes W, Dhillon P, Goodman L. Medical encounters during a Joint Canadian/US exercise in the high arctic (Exercise Arctic Ram). Mil Med. 2017;182(9–10):e1764–e8. doi:10.7205/MILMED-D-16-00390.
- Ervasti O, Juopperi K, Kettunen P, et al. The occurrence of frostbite and its risk factors in young men. Int J Circumpolar Health. 2004;63(1):71–80. doi: 10.3402/ijch.v63i1.17650
- Hoiland DW II, Mercer L. The effect of oral uptake of nicotine in snus on peripheral skin blood circulation evaluated by thermography. Temperature (Austin). 2014;1(3):220–226. doi: 10.4161/23328940.2014.984553
- https://www.helsedirektoratet.no/tema/tobakk-royk-og-snus/e-sigaretter-elektroniske-sigaretter-og-regelverk
- Havenith G, Fiala D, Blazejczyk K, et al. The UTCI-clothing model. Int J Biometeorol. 2012;56(3):461–470. doi: 10.1007/s00484-011-0451-4
- Bakkevig MK, Nielsen R “Which sweater to choose in the cold: knitted or fleece”. Arctic Med Res. 1994;53(4):200–209.
- Ikäheimo TM, Hassi J Frostbites in circumpolar areas. Global Health Action. 2011;4(1):8456. doi: 10.3402/gha.v4i0.8456
- Rintamäki H. Predisposing factors and prevention of frostbite. Int J Circumpolar Health. 2000;59(2):114–121.
- Harirchi I, Arvin A, Vash JH, et al. Frostbite: incidence and predisposing factors in mountaineers. Br J Sports Med. 2005;39(12):898–901. doi: 10.1136/bjsm.2004.016097
- Imray C, Grieve A, Dhillon S. Cold damage to the extremities: frostbite and non-freezing cold injuries. Postgrad Med J. 2009;85(1007):481–488. doi: 10.1136/pgmj.2008.068635
- Cattermole TJ. The epidemiology of cold injury in Antarctica. Aviat Space Environ Med. 1999;70(2):135–140.
- Cauchy E, Chetaille E, Marchand V, et al. Retrospective study of 70 cases of severe frostbite lesions: a proposed new classification scheme. Wilderness Environ Med. 2001;12(4):248–255. doi: 10.1580/1080-6032(2001)012[0248:RSOCOS]2.0.CO;2
- Regli IB, Strapazzon G, Falla M. Long-term sequelae of frostbite—a scoping review. Int J Environ Res Public Health. 2021;18(18):9655. doi: 10.3390/ijerph18189655
- Robinson JP, Shaver PR, Wrightsman LS, editors. Measurement and Control of Response Bias. Academic Press; 1991. p. 17–59. ISBN 9780125902410. doi: 10.1016/B978-0-12-590241-0.50006-X. https://www.sciencedirect.com/science/article/pii/B978012590241050006X
- Norheim AJ, Sullivan-Kwantes W, Steinberg T, et al. The classification of freezing cold injuries-a NATO research task group position paper. Int J Circumpolar Health. 2023;82(1):2203923. doi: 10.1080/22423982.2023.2203923