ABSTRACT
There is growing awareness and recognition of the importance of the One Health paradigm to address existing environmental threats and recognise emerging ones at an early stage among Arctic residents, public health agencies, and wildlife resource managers. The One Health approach, emphasising the interconnectedness of human, animal, and ecosystem health, plays a pivotal role in addressing these multifaceted issues. Warming climate and permafrost thaw may influence both contaminant exposure and the spread of zoonotic infectious diseases and have impacts on water and food security. Migration from rural regions to larger communities and urban centres along with increased tourism may be accompanied by changes in exposure to contaminants and zoonotic diseases. Universities have developed educational programmes and research projects on One Health in the Arctic, and under the Arctic Council there is running a project of One Arctic, One Health. These arctivities have produced interdisciplinary information and practical solutions for local communities, decision-makers, and in scientific forums. There is a need for epidemiological zoonotic/human disease models, as well as new approaches to integrate existing and future surveillance data to climatic and environmental data. This requires not only regional and international collaboration but also multi-agency and transdisciplinary research.
Introduction
The Arctic is an important component of the globe (similar in size to the African continent) and reflects the impacts of climate warming, long-range contaminant transport, increased human activities, and existing and newly emerging infections, such as the COVID-19 pandemic. The Arctic has around seven million inhabitants, about one million of whom are Indigenous, and three-quarters of the Arctic population resides in settlements of more than 5000 people [Citation1,Citation2]. In coastal regions, there is a population of around one million people. The Arctic environment is in a process of change, which already has or will have significant impacts, especially on those five million inhabitants living in permafrost regions [Citation1,Citation3].
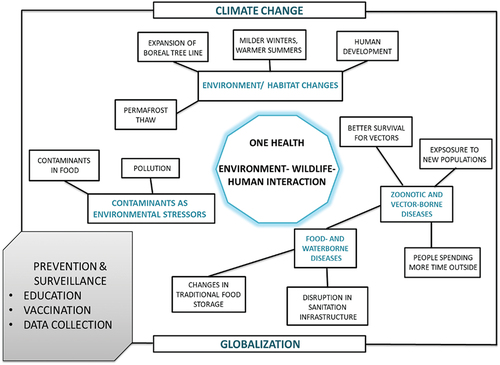
The One Health concept recognises that humans, animals, and ecosystem health are interrelated and interdependent in complex ways. It uses the responses to human mental, physical, cultural, and social wellbeing, which demand transdisciplinary and holistic approaches. Human, domestic animal, and wildlife health practitioners must work closely with ecosystem health scientists to achieve optimal results (). One Health is the intuitive world view of Indigenous people everywhere, and it is an increasingly established concept worldwide as populations face the complex challenges associated with global climatic and environmental changes. These include changes in landscape/land-use; the effects of urbanisation; emerging infectious diseases, biological invasive species, and reduction in biodiversity; global demographic changes; and worldwide circulation of anthropogenic contaminants and spread of existing infectious diseases. The bridging of contact between animals and humans frequently results in the emergence and re-emergence of zoonoses from wildlife reservoirs [Citation4]. Ecosystem change is a major driver of disease emergence (). This paper describes close connections between the Arctic regions and connections to the rest of world studied in the different projects, which use the One Health approach. It is based on a chapter of The Arctic in a global context in the AMAP Assessment 2021: Human Health in the Arctic [Citation5].
One health collaboration in the Arctic
Arctic council
In the Arctic Council, there are six working groups, and two of them have human health sub-groups: the Arctic Human Health Expert Group (AHHEG) under the Arctic Council’s Sustainable Development Working Group (SDWG) and the Human Health Assessment Group (HHAG) under the Arctic Monitoring and Assessment Programme (AMAP) [Citation6]. The HHAG was created almost immediately after AMAP was established, since contaminants in the Arctic were clearly found to be a threat to human health. The International Circumpolar Surveillance (ICS) programme, which monitors infectious diseases in the Arctic countries, has been integrated into AHHEG in recognition of the key role of climate in the ecology of infectious disease pathogens, including zoonotic pathogens, in the Arctic [Citation7]. The Climate Sensitive Infection Workgroup under ICS focuses on trends in existing zoonoses and the emergence of newly arriving zoonoses as ocean and air temperatures rise, and range extension carries southern wildlife species further north. The Conservation of Arctic Flora and Fauna (CAFF) programme, one of the initial Arctic Council programmes, assesses plant and wildlife health in the Arctic.
The Arctic Council has recognised the concept of One Health, and coordination between the various Arctic Council programmes and working groups has been improved in order to achieve an integrated One Health approach. AMAP, CAFF, and SDWG address all elements of One Health, although their scopes of work currently differ due to the requirements of agencies funding the research, and to a lesser extent by the perceived professional boundaries of the researchers within the working groups. The multidisciplinary cooperation that produced the Arctic Climate Impact Assessment [Citation8], and more recently, the joint report on the COVID-19 pandemic in the Arctic [Citation9,Citation10], are all examples of a trend towards a One Health approach to a wide variety of emerging environmental and human/wildlife health issues. The SARS-CoV-2 virus is a “textbook example” of the development of a novel pathogen with subsequent worldwide infection. Early detection of novel pathogens in biota, development of appropriate monitoring of environmental reservoirs, as well as vulnerable human hosts, are key elements of the One Health programme [Citation11].
During the U.S. Chairmanship (2015–2017) of the Arctic Council, the USA and Canada introduced the “One Arctic, One Health” project designed to strengthen regional knowledge sharing, establishing knowledge hubs and coordination regarding a variety of Arctic One Health concerns in the Arctic member states [Citation12]. The project continued during the Finnish (2017–2019), Icelandic (2019–2021), Russian s (2021–2023) and Norwegian (2023–2025) chairmanships. The main task of the One Health project is to build firm linkages between human, animal, and environmental health, and local communities, policymakers, researchers, and residents, to advance Arctic regional resilience and reduce health risks, as mentioned above. One form of operationalising multi-sectoral collaboration in the case of hypothetical health emergencies (such as forest fires or a transboundary disease outbreak among land/sea animals), is through the One Health Table Top Exercises (TTX) concept [Citation13]. The scenarios focus on the coordination and information flow needed to rapidly diagnose and respond to the outbreak.
Arctic networks in one health research and education
Northern universities have made many significant contributions to the wider application of One Health principles. Contributions to the science of physical environmental monitoring, the application of civil engineering expertise to village environmental health problems, and village-based environmental biomonitoring have all developed through cooperation between community and tribal organisations, wildlife resource agencies, public health agencies, and universities [Citation14].
Undergraduate and graduate degree programmes are under development in several universities and should eventually result in a steady supply of young scientists and experts trained in applying One Health principles to the growing challenges faced by residents worldwide. For example, the University of Alaska (Fairbanks) has developed a Masters’ degree programme [Citation15], and Nordic countries are developing a Nordic One Health course.
Other important agencies, networks, and projects for collaboration, such as the University of Alaska (Fairbanks) and the Thematic Network of Health and Well-being in the Arctic (under the University of the Arctic), also enhance collaboration and improve the visibility of the education and research of One Health. EU-funded projects are another excellent example, including INTERACT [Citation16], for monitoring of possible vectors of zoonotic diseases, Nunataryuk [Citation17] for modelling and human health risk assessment of anthrax and contaminants evaporated from thawing permafrost, and the Nordic Centre of Excellence project CLINF [Citation18] for research on climate change effects on zoonotic diseases in the North. The current pandemic arising from the COVID-19 virus represents a classic example of the interdependence of environmental, wildlife, and human health.
Current status of one health components in the Arctic
Environmental contaminants
Higher temperatures cause changes in sea ice, snow cover, permafrost, ocean temperatures, and precipitation. Climate change is also occurring together with unprecedented globalisation in the Arctic. Increased accessibility to remote locations, increased levels of tourism and industry, and social change all bring new health challenges to the Arctic [Citation1,Citation19], in addition to already complex issues such as high levels of environmental contaminants and rising chronic disease rates [Citation20]. The geographic differences in the concentrations and trends in many contaminants reflect the differences in culture, lifestyle, and dietary habits evident across the Arctic [Citation5].
Environmental contaminants are one important component of the One Health model. The persistent organic pollutants (POPs) listed in the annexes to the Stockholm Convention continue to circulate in the environment [Citation21]. Environmental factors and the impacts of climate change will affect the volatilisation and distribution of POPs and heavy metals [Citation22,Citation23]. For example, despite the general declining trend in polychlorinated biphenyl (PCB) levels in human biological matrices and biota, modelling of atmospheric PCB composition and behaviour predicted some increase in environmental concentrations under a warmer climate [Citation22]. Another concern is exposure of Arctic Indigenous Peoples to high levels of mercury (Hg), which are high enough to have health impacts [Citation24].
Adverse health outcomes (e.g. neurodevelopmental outcomes in young children and youth and cardiovascular disease in adults) have been found to be associated with Hg exposure [Citation5,Citation24]. Due to dietary transition and advise, Hg levels in cord blood and from pregnant women have decreased in the Arctic region, e.g. in Faroe Islands (2008) being 20% of those levels found 30 years earlier [Citation5]. However, in Nunavik and Greenland, the levels are 4–5 times higher than measured in the other Arctic regions [Citation5].
Permafrost thaw caused by climate change has major implications for the global Hg cycle [Citation23]. Northern permafrost soils represent the largest reservoir of Hg on the planet, storing nearly twice as much Hg as all other soils, the ocean, and the atmosphere combined, indicating a need to re-evaluate the role of the Arctic regions in the global Hg cycle. This Hg is vulnerable to release due to the permafrost thaw projected for the coming century. Modelling of the atmospheric PCB composition and behaviour indicated higher environmental concentrations in a warmer Arctic, but a general decline in PCB levels is still the most prominent feature [Citation22]. “Within-Arctic” processing of PCBs will be affected by climate change-related processes such as changes in wet deposition. These in turn will influence biological exposure and uptake of PCBs [Citation22]. Contaminants will also be released from melting sea ice and glaciers.
Infectious diseases
Melting permafrost and a warming climate, especially in Arctic Russia, cause threats of release and re-emergence of ancient pathogens, exemplified by anthrax, and pollutants as mercury and other contaminants [Citation25,Citation26]. The risk of outbreaks of anthrax and other microbiological infections are real when the climate is warming, and permafrost is thawing. Revich and co-workers [Citation27] have made an overview about the risks of Anthrax burial sites in Russia, and he concluded that there is a need to combine data on permafrost, number of anthrax cattle burials, trends in average long-term temperatures, and population density for risk assessment.
Rates of diagnosed infectious diseases in the Arctic are highly variable, depending on country, disease, age, gender of the affected individuals, and geographic location [Citation28]. Overall, improved sanitation, medical treatment, vaccination, and education have decreased infectious disease and health disparities between Indigenous and non-Indigenous populations across the Arctic. Bourgeois et al. [Citation29] studied tuberculosis incidence in the Arctic (between years 2006 and 2016) and found this to vary among Arctic countries and to be higher in Indigenous populations, and higher in males than females. Current trends in infectious diseases in the Arctic also include the high prevalence of sexually transmitted diseases, introduction of new pathogens such as COVID-19 [Citation9,Citation10,Citation30], changes in the emergence of food and waterborne diseases, and the spread of vector-borne and zoonotic diseases due to climate change [Citation4,Citation28,Citation31–34].
Climate change is predicted to be one of the most influential factors in the emergence of infectious diseases [Citation31] and will have both direct and indirect impacts on human health, especially in relation to infectious diseases [Citation20,Citation35]. Higher sea and land temperatures can increase growth rates of pathogens and animals, including insect vectors [Citation36,Citation37]. Extreme precipitation events may cause flooding and disrupt water/sanitation infrastructure, raising the risk for waterborne disease outbreaks. Indirectly, climatic factors affect infectious disease transmission by altering human behaviour, such as using public bathing waters and enabling more opportunities for the start of a waterborne disease outbreak [Citation38] or spending more time outside (e.g. in forests), which increases the likelihood of contracting a tick-borne disease [Citation39]. Changes in climatic factors can expand or compress a disease vector’s geographic range, change the seasonality of vector-borne diseases, increase/decrease its population size, and alter vector species and individuals’ ability to survive the winter [Citation33,Citation34,Citation36,Citation40,Citation41]. However, increased public and health personnel education, vaccination programmes, and hygiene can help combat the spread of disease, potentially reducing infections despite more opportunities for infection because of climate change.
Climate and environmental change
Climate and environmental change and increased human activity threaten the health of the Arctic wildlife. Globally, parasites constitute a major component of biodiversity [Citation42] and are often identified as wildlife and/or human pathogens. Many animal species inhabit the Arctic, including permanent residents and those that migrate in seasonally. These include over 200 species of bird, 100 species of mammal, 300 species of fish, and thousands of species of invertebrates and microorganisms [Citation43]. Environmental threats include rising sea and air temperatures, and the associated changes in biota, habitat, foraging grounds, breeding areas, and migration routes. These same environmental changes also affect disease-vector populations, ranges, and lifecycles.
Simultaneously, the Arctic is the focus of increased human interest and activity, which in turn brings additional challenges that may impact upon infectious diseases among wildlife, e.g. increased shipping traffic could introduce rat-borne diseases from ports in northwestern Scandinavia and the Russian Federation. The rapid influx of people (and their pets) has the potential to introduce new pathogens, establish new hosts, and alter the wildlife environment through industry, construction, and pollution. Change can also stress animals, potentially making them more vulnerable to infectious diseases [Citation44].
Many Arctic pathogens may have environmental hosts that have not been identified. For example, the intracellular bacterium Coxiella burnetti (causing human Q fever) has recently been identified in northern fur seals and their placenta and may well be found in the crabs feeding on these placentas at rookeries in the Bering Sea. Francisella tularensis (a type of aerobic bacterium causing human tularaemia) causes an antibody response, which has not previously been found in polar bears, but has now been [Citation45]. The environmental reservoirs for these recently documented new Arctic infections are not known. The ecology of Arctic pathogens is a topic that needs collaborative investigation, involving local knowledge as well as western science [Citation46].
Changes in nature and environment have impacts on Indigenous peoples in the Arctic. Thinning and reduction of the sea ice during wintertime, a reduced snow cover duration, risks of natural disasters, such avalanches and tsunamis are risks for travelling and hunting [Citation35,Citation47]. From a One Health perspective, it is necessary to monitor marine mammal health and the risks caused by changing ice condition and temperature for them [Citation35].
Future directions
Clean, safe, fresh water is one of the most important natural resources and the focus of one of the United Nations Sustainable Development Goals under Agenda 2030. Safe drinking water and adequate sanitation are key factors for human life and health. Arctic climate conditions affect water security and sanitation services in the Arctic countries. Some challenges, such as loss of permafrost, affect regional water and sanitation services in similar ways, while others are more limited in distribution. There are still people in Arctic regions that lack centralised drinking water and sanitation systems, and alternative drinking water sources and transport options continue to be needed. The state of water services in the Arctic was reviewed for the One Arctic, One Health project [Citation48].
Permafrost thaw affects infrastructure, livelihoods, and access to clean drinking water and food. According to the results of Ramage et al. [Citation3] climate-driven permafrost projections suggest that 42% of the permafrost settlements (3.3 million people) will become permafrost-free due to thawing by 2050, and around 42% of those which stay on permafrost are in high hazard zones. Permafrost degradation has far-reaching consequences for the global climate and profound impacts on local and regional livelihoods [Citation3].
Langer and co-workers [Citation49] recently published a paper about the contaminated sites on the Arctic permafrost. They identified 4500 industrial sites, where potentially hazardous substances are actively used or stored in the permafrost-dominated regions. Energy and agriculture, forestry, and other land use account for the largest proportion of industrial sites, but 70% of them remain unknown. There might be up to 15 000 more. Industrial contaminants have been neglected in existing climate impact analyses, and they are an important risk factor locally and globally.
Operationalising One Health requires application of the One Health paradigm to the issues to be addressed. It requires the development of metrics to monitor trends in recognised threats, to detect emerging ones, and evaluate the results of mitigation and adaptation strategies. The strategy should take advantage of Indigenous and local knowledge, as well as scientific application of technology, where appropriate. In the circumpolar north, where many community challenges are climate-sensitive, a One Health approach may help in developing an effective and sustainable response. In the European Union, the One Health approach has been the basic element of the new funding calls together with community-based participatory elements of including local and Indigenous populations. Communities benefit from a well-functioning system for systematically monitoring trends in environmental change and diseases or other threats to wildlife, such that residents and jurisdictional health systems can respond effectively. This may include physical monitoring, for example concerning shoreline erosion or permafrost temperature; as well as biomonitoring to collect evidence of subsistence animal exposure to zoonotic diseases and contaminants. The data from a well-designed community-based, resident-operated programme enables communities to develop local adaptation strategies that can be critical to sustaining a traditional diet, protecting vulnerable residents, and protecting village infrastructure [Citation50]. The use of the Table Top Exercise methodologies for improving collaboration and planning for the future is an important tool [Citation13].
Conclusion
The holistic view of Indigenous peoples, the communities’ willingness to contribute traditional ecological knowledge, and local observations of environmental abnormalities are essential parts of the One Health approach. Local wildlife management agencies and laboratories can help train communities to develop their own environmental monitoring systems. Combining the knowledge of local observers and western science offers the best opportunity to develop community-based strategies for monitoring, adaptation and mitigation [Citation14,Citation47]. Development of strategies for actions and programmes utilising One Health to address the consequences of a warming Arctic will depend on these cooperative efforts between scientists with diverse professional backgrounds, together with the contributions of Arctic residents.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Jungsberg L, Turunen E, Heleniak T, et al. Atlas of population, society and economy in the Arctic. Nordregio working paper. 2019:3. Nordregio, Stockholm, Sweden.
- Young TK, Bjerregaard P. Towards estimating the indigenous population in circumpolar regions. Int J Circumpolar Health. 2019;78(1):1653749. doi: 10.1080/22423982.2019.1653749
- Ramage J, Jungsberg L, Wang S, et al. Population living on permafrost in the Arctic. Popul Environ. 2021;43(1):22–8. doi: 10.1007/s11111-020-00370-6
- Ma Y, Destouni G, Kalantari Z, et al. Linking climate and infectious disease trends in the Northern/Arctic region. Nat Sci Rep. 2021;11(1):20678. doi: 10.1038/s41598-021-00167-z
- AMAP. AMAP assessment 2021: human health in the Arctic. Tromsø, Norway: Arctic Monitoring and Assessment Programme (AMAP); 2021. p. x+240.
- Arctic Council. Available from: https://arctic-council.org
- Parkinson JA, Bruce MG, Zulz Y. International circumpolar surveillance, an Arctic network for the surveillance of infectious diseases. Emerg Infect Dis. 2008;14(1):18–24. doi: 10.3201/eid1401.070717
- ACIA. Impacts of a warming Arctic: Arctic climate impact assessment. ACIA overview report. New York: Cambridge University Press; 2005.
- Sustainable Development Working Group (SDWG). Covid-19 in the Arctic Assessment Report. 2023 [cited 2024 Jan 25]. Available from: www.sdwg.org
- Arctic Yearbook. Arctic pandemics. In: Spence J, Exner-Pilot H, Petrov A. editors. COVID-19 and other pandemic experiences and lessons learned. 2023. Arctic Portal. 2023 [cited 2024 Jan 25]. Available from: https://arcticyearbook.com/arctic-yearbook/2023-special-issue
- Mushi V. The holistic way of tackling the COVID-19 pandemic: the one health approach. Trop Med Int Health. 2020;48(1):69. doi: 10.1186/s41182-020-00257-0
- [cited 2024 Jan 25]. Available from: https://sdwg.org/what-we-do/projects/one-health-iii/
- Vesterinen HM, Cutcher TV, Errecaborde KM, et al. Strengthening multi-sectoral collaboration on critical health issues: One Health Systems Mapping and Analysis Resource toolkit (OH-SMART) for operationalizing one health. PLOS ONE. 2019;14(7):e0219197. doi: 10.1371/journal.pone.0219197
- Ruscio BA, Brubaker M, Glasser J, et al. One health – a strategy for resilience in a changing arctic. Int J Circumpolar Health. 2015;74(1):27913. doi: 10.3402/ijch.v74.27913
- [cited 2024 Jan 25]. Available from: www.uaf.edu/onehealth
- INTERACT - International Network for Terrestial Research and Monitoring in the Arctic [cited 2024 Jan 25]. Available from: https://eu-interact.org
- Nunataryuk [cited 2024 Jan 25]. Available from: https://nunataryuk.org
- Climate change effects on the epidemiology of infectious diseases and the impacts on Norhern societies (CLINF) [cited 2024 Jan 25]. Available from: https://clinf.org
- Larsen JN, Fondahl G. In: Larsen NJ. Major findings and emerging trends in Arctic human development. In: Fondahl G, editor. Arctic human development report: regional processes and global linkages. Vol. 567. Copenhagen: Nordic Council of Ministers; 2014. p. 475–497. TemaNord.
- Arctic Council. Tromsø declaration. 2009 [cited 2024 Jan 25]. Available from: https://oaarchive.arctic-council.org/handle/11374/91
- Dientz R, Lecher RJ, Desforges J-P, et al. Current state of knowledge on biological effects from contaminants on arctic wildlife and fish. Sci Total Environ. 2019;696:133792. doi: 10.1016/j.scitotenv.2019.133792
- Carlsson P, Breivik K, Brorström-Lundén E, et al. Polychlorinated biphenyls (PCBs) as sentinels for the elucidation of Arctic environmental change processes: a comprehensive review combined with ArcRisk project results. Environ Sci Pollut Res Int. 2018;25(23):22499–22528. doi: 10.1007/s11356-018-2625-7
- Schuster PF, Schaefer KM, Aiken GR, et al. Permafrost stores a globally significant amount of mercury. Geophys Res Lett. 2018;45(3):1463–1471. doi: 10.1002/2017GL075571
- Basu N, Abass K, Dientz R, et al. The impact of mercury contamination on human health in the Arctic: a state of the science review. Sci Total Environ. 2022;831:154793. doi: 10.1016/j.scitotenv.2022.154793
- Orlov D, Menshakova M, Thierfelder T, et al. Health ecosystems are a prerequisite for human health – a call for action in the era of climate change with a focus on Russia. Int J Environ Res Public Health. 2020;17(22):8453. doi: 10.3390/ijerph17228453
- Everett L, editor. Understanding and responding to global health security risks from microbial threats in the Arctic. National Academies Press; 2020. Available from: www.nap.edu/read/25887/chapter/1
- Revich BA, Shaposhnikov DA, Raichich SR, et al. Creating zones in administrative districts located in the Russian Arctic region specific as per threats of cattle burials decay due to permafrost degradation. Health Risk Anal. 2021;(1):115–125. doi: 10.21668/health.risk/2021.1.12.eng
- Waits A, Emelyanova A, Oksanen A, et al. Human infectious diseases and the changing climate in the Arctic. Environ Int. 2018;121:703–713. doi: 10.1016/j.envint.2018.09.042
- Bourgeois AC, Zulz T, Bruce MG, et al. Tuberculosis in the circumpolar region, 2006–2012. Int J Tuberc Lung Dis. 2018;22(6):641–648. doi: 10.5588/ijtld.17.0525
- Petrov AN, Welford M, Golosov N, et al. Spatiotemporal dynamics of the COVID-19 pandemic in the Arctic: early data and emerging trends. Int J Circumpolar Health. 2020;79(1):1835251. doi: 10.1080/22423982.2020.1835251
- Omazic A, Bylund H, Boqvist S, et al. Identifying climate-sensitive infectious diseases in animals and humans in Northern regions. Acta Vet Scand. 2019;61(1):53. doi: 10.1186/s13028-019-0490-0
- Van Oort BEH, Hovelsrud GK, Risvoll C, et al. A mini-review of Ixodues ticks climate sensitive infection dispersion risk in the Nordic region. Int J Environ Res Public Health. 2020;17(15):5387. doi: 10.3390/ijerph17155387
- Jore S, Vanwambeke SO, Viljugrein H, et al. Climate and environmental change drives ixodes ricinus geographical expansion at the northern range margin. Parasites Vectors. 2014;7(1):11. doi: 10.1186/1756-3305-7-11
- Goren A, Viljugrein H, Rivrud IM, et al. The emergence and shift in seasonality of Lyme borreliosis in Northern Europe. Proc R Soc B. 2023;290(1993):20222420. doi: 10.1098/rspb.2022.2420
- Tryland M, editor. Arctic one health. 2022. Challenges for northern animals and people. Springer (ebook); 2022 [cited 2024 Jan 25]. doi: 10.1007/978-3-030-87853-5
- Bruce M, Zulz T, Koch A. Surveillance of infectious diseases in the Arctic. Public Health. 2016;137:5–12. doi: 10.1016/j.puhe.2016.06.014
- Noskov AK, Ya A, Nikitin EI, et al. Клещевой вирусный энцефалит в Российской Федерации: Особенности эпидемического процесса в период устойчивого спада заболеваемости, эпидемиологическая ситуация в 2016 г. прогноз на 2017 г. [Tick-borne virus encephalitis in the Russian Federation: features of epidemic process in steady morbidity decrease period. Epidemiological situation in 2016 and the forecast for 2017]. Проблемы Особо Опасных Инфекций. 2017;1:37–43.
- Eze JI, Scott EM, Pollock KG, et al. The association of weather and bathing water quality on the incidence of gastrointestinal illness in the west of Scotland. Epidemiol Infect. 2014;142(6):1289–1299. doi: 10.1017/S0950268813002148
- Saegerman C, Humblet M-F, Leandri M, et al. First expert elicitation of knowledge on possible drivers of observed increasing human cases of Tick-Borne Encephalitis in Europe. Viruses. 2023;15(3):791. doi: 10.3390/v15030791
- Parham PE, Waldock J, Christophides GK, et al. Climate, environmental and socio-economic change: weighing up the balance in vector-borne disease transmission. Phil Trans R Soc London B. 2015;370(1665):20130551. doi: 10.1098/rstb.2013.0551
- Chashchin VP, Popova ON, Byzinov RB, et al. Эпидемиологические особенности распространения клещевого вирусного энцефалита в Архангельской области [Epidemiological character of tick-borne viral encephalitis extension in the Arkhangelsk region]. Экология Человека. 2017;4:12–19.
- Dobson A, Lafferty KD, Kuris AM, et al. Homage to Linnaeus: how many parasites? How many hosts? Proc Natl Acad Sci, USA. 2008;105(supplement_1):11482–11489. doi: 10.1073/pnas.0803232105
- CAFF. Arctic biodiversity assessment: status and trends in Arctic biodiversity. Akureyri: Conservation of Arctic Flora and Fauna (CAFF); 2013.
- Bradley M, Kutz SJ, Jenkins E, et al. The potential impact of climate change on infectious diseases of Arctic fauna. Int J Circumpolar Health. 2005;64(5):468–477. doi: 10.3402/ijch.v64i5.18028
- Atwood TC, Duncan C, Patyk KA, et al. Environmental and behavioral changes may influence the exposure of andofc apex predator to pathogens and contaminants. Sci Rep. 2017;7(1):13193. doi: 10.1038/s41598-017-13496-9
- Emelyanova A, Savolainen A, Oksanen A, et al. Research on selected wildlife infections in the circumpolar Arctic—a bibliometric review. Int J Environ Res Public Health. 2022;19(18):11260. doi: 10.3390/ijerph191811260
- Timlin U, Ingimundarson JH, Jungsberg L, et al. Living conditions and mental wellness in a changing climate and environment: focus on community voices and perceived environmental and adaptation factors in Greenland. Heliyon. 2021;7(4):e06862. doi: 10.1016/j.heliyon.2021.e06862
- Miettinen IT. One Arctic - One Health - Water security in circumpolar region. One Arctic – One Health, Finnish Food Authority, Research Report. 2019 Mar;21–23.
- Langer M, von Deimling TS, Westermann S, et al. Thawing permafrost poses environmental threat to thousands of sites with legacy industrial contamination. Nat Commun. 2023;14(1):1721. doi: 10.1038/s41467-023-37276-4
- O’Hara TM, Hueffer K, Murphy MD, et al. Developing a sentinel-based Baja California Sur Rural Mexico monitoring program: lessons learned from Alaska. Recursos Naturales y Sociedad. 2017;3:12–31.