ABSTRACT
Background
To share a case of an unusual occurrence of an ectopic pregnancy that appeared 2 weeks after a miscarriage.
Case presentation
A lady in her 30s, whose intrauterine early pregnancy was verified by transvaginal ultrasound. The patient two-weeks later experienced severe lower abdominal pain, at which time we discovered a left tubal pregnancy with an empty uterus. The patient had a history of missed miscarriage and vaginal bleeding two weeks prior to the ultrasound assessment. The patient was hospitalized for a diagnostic laparoscopy and left salpingectomy.
Conclusion
The purpose of this case report is to draw attention to a rare situation in which clinicians in the early pregnancy unit and the gynecology team should not dismiss the patient’s clinical signs and should instead re-confirm the early pregnancy location by ultrasound if the patient presents with symptoms suggestive of acute pregnancy-related issues despite a previous diagnosis of an intrauterine early pregnancy.
Introduction
Scans performed early in pregnancy to determine the normal location of the pregnancy, viability, and healthy pregnancy are regarded as the crucial stages by which many decisions may be addressed. There are cases where two separate pregnancies occur, one inside the uterine cavity and the other outside it, and this is something that has been described both in the medical literature and clinical practice. Which we call: Heterotopic pregnancy [Citation1]. So far, however, there have been no clinical reports or cases documented in the literature documenting the transition of a pregnancy from an intrauterine position to the tube. Once a pregnancy has been confirmed inside the uterus, the possibility of an ectopic is rarely considered. In recent decades, there has been a rise in the occurrence of both multiple pregnancies and heterotopic pregnancies due to the prevalence of pelvic inflammatory diseases and the widespread use of ovarian stimulation with or without assisted reproductive techniques (ART) [Citation2]. Numerous types of heterotopic pregnancies have been described; for example, 15 case reports of heterotopic quadruplet pregnancies appeared in the literature between 1989 and 2021 [Citation3].
Herein, we report a rare case of an ectopic pregnancy that appeared two weeks after the top miscarriage, in which the patient had a scan revealed intrauterine pregnancy, but if we had solely relied on that information, we might have missed a ruptured ectopic pregnancy with intra-abdominal bleeding when she presented later with lower abdominal pain. Despite its rarity, this case highlights the importance of tailoring investigations and treatment for each patient based on clinical sense.
Case presentation
A lady in her thirties, with a BMI of 28. Non-smoker, no alcohol use. With no past surgical or medical relevant significant issues.
Gravida 3 Para 1 + 2. The patient had a ventouse delivery 3 years ago. Had 1 medical termination of pregnancy (MTOP) at 16 weeks and 1 stillbirth at 24 + 3 weeks, the patient had amniocentesis 3 weeks before her stillbirth for fetal brain abnormalities.
The patient used to have normal regular periods and normal up-to-date cervical smears.
On her first attendance, she presented to the emergency department with mild lower abdominal pain, vaginal spots, 8 weeks of amenorrhea and a positive urine pregnancy test. We assessed the patient, did some blood tests and arranged a trans-vaginal ultrasound scan at the early pregnancy unit. The scan showed that there is an intrauterine embryo with absent fetal heart activity. This measured 20 mm which gives 8 weeks gestation pregnancy. (Please refer to & in the investigations section).
Figure 1. Showed an intrauterine pregnancy at the transverse view of the uterus by the trans-vaginal scan, (fetal pole) shown at the same view.
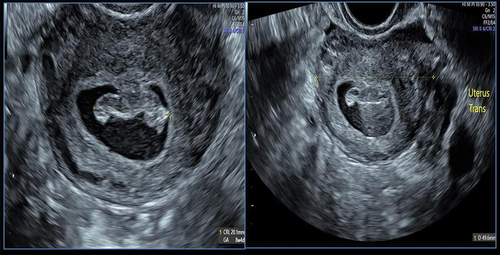
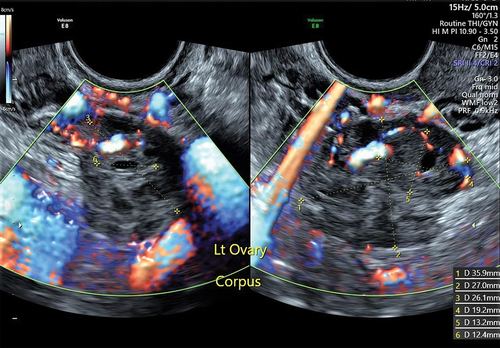
Figure 3. Left ovary: normal. Size: 36 mm x 27 mm x 26 mm. Volume: 13.2 ml. Corpus luteum: 19 mm x 13 mm x 13 mm, solid.
The patient had at that time beta- hCG which was 2500 mIU/mL. Serum progesterone 30 nmol/L. Hb level 113 g/L.
The patient opted for expectant management, was reassured that the scans didn’t show any ectopic pregnancy, and has been counseled to repeat the scan within 2 weeks. Safety netting has been given with advice to come back if any heavy bleeding or pain increased or any other unusual symptoms happened.
Two weeks later, the patient presented with severe left lower quadrant pain with ongoing bleeding that has been interpreted by the patient as miscarriage symptoms for her missed miscarriage. The blood tests have been repeated which showed beta- hCG 500 mIU/mL. Serum progesterone 5.3 nmol/L. Hb level 109 g/L.
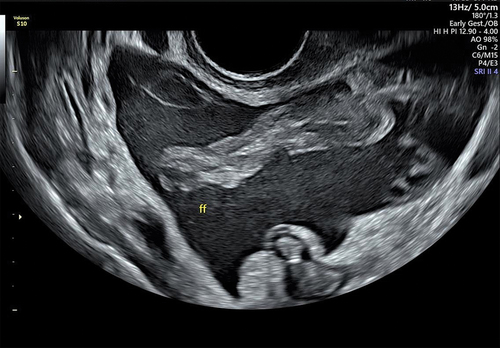
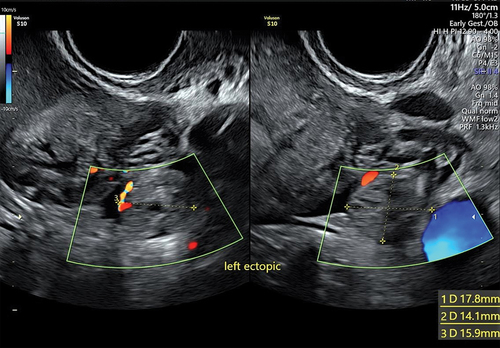
We repeated the trans-vaginal scan, which showed no intrauterine pregnancy, with confirmed left ectopic pregnancy, and a large amount of free fluid in the Douglas pouch (Please refer to & at the investigations section).
The patient has been explained the situation, and she opted for the surgical management of the ectopic pregnancy (as it is clinically recommended due to internal hemorrhage).
Investigations
On the first Visit to the early pregnancy unit, the patient had a routine blood test including FBC, BhCG, and Serum progesterone.
Beta- hCG which was 2500 mIU/mL. Serum progesterone 30 nmol/L. Hb level 113 g/L.
The patient had a trans-vaginal ultrasound scan which confirmed an early intrauterine pregnancy as a suspected missed miscarriage.
is showing an intrauterine pregnancy at the transverse view of the uterus by the trans-vaginal scan, with the crown-rump (fetal pole) shown at the same view.
Gestational Sac: present; intrauterine. Gestational sac size: 19 mm x 11 mm x 27 mm.
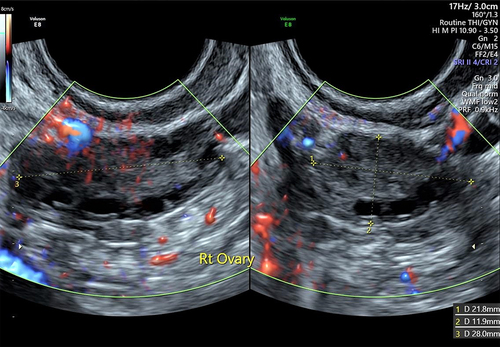
The Right ovary as shown in : is normal. Size: 22 mm x 12 mm x 28 mm. Volume: 3.9 ml.
The Left ovary as shown in : is normal. Size: 36 mm x 27 mm x 26 mm. Volume: 13.2 ml. The same image is showing a Corpus luteum: 19 mm x 13 mm x 13 mm, solid.
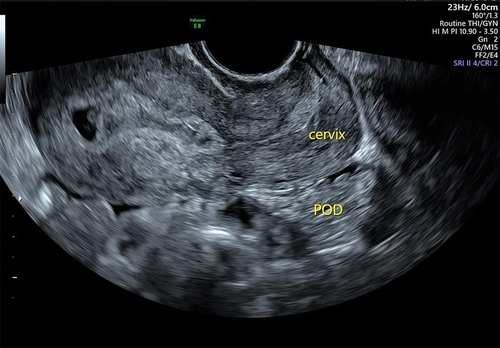
Pouch of Douglas : showing No free fluid seen.
At the second attendance (2 weeks later)
The blood tests have been repeated which showed beta- hCG 500 mIU/mL. Serum progesterone 5.3 nmol/L. Hb level 109 g/L.
We have repeated the trans-vaginal ultrasound scan with the following findings:
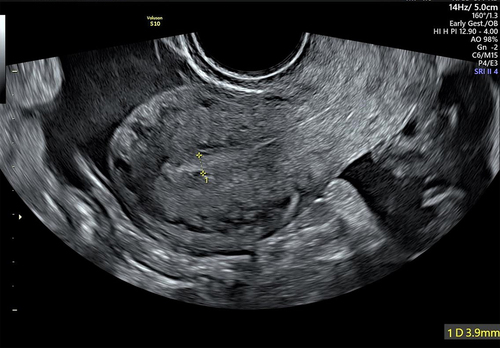
An empty uterus with no obvious intrauterine pregnancy. Endometrial thickness of 3.9 mm as shown in .
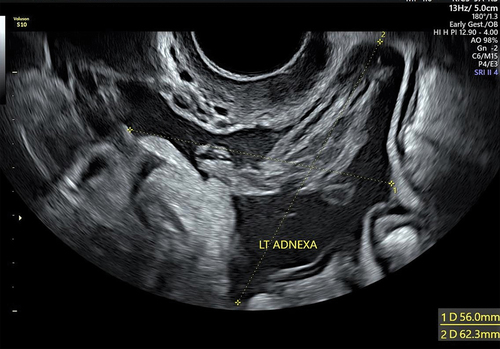
Left adnexa with marked free fluid in the pouch of Douglas. .
Marked free fluid in the pouch of Douglas .
Confirmed Left ectopic pregnancy as shown in .
Differential diagnosis
After the second transvaginal scan, many possibilities were considered; however, the diagnosis of ectopic pregnancy on top of missed miscarriage emerged as the clear winner.
The scan led us to suspect a heterotopic pregnancy in which the intrauterine pregnancy had miscarried, but it is clear that there was an interval between the appearance of intrauterine pregnancy alone and the appearance of ectopic pregnancy. During the two weeks that passed between the initial trans-vaginal scan and the second, the patient reported on and off mild bleeding which indicated a miscarriage happened. Since chorionic villi are confirmed by the specimen’s histopathology report, alternative diagnoses like a ruptured corpus luteal cyst could be discounted. It is evident from the scan images that the pregnancy location was intrauterine (), and on the second visit, the images showed an empty uterus, yet the team of consultants who reviewed the scan images did not even consider the possibility that the patient had been misdiagnosed with an ectopic pregnancy.
Corpus luteum was one of the differential diagnoses.
Subsequently, during our Multidisciplinary Team (MDT) discussion, we scrutinized the ultrasound (US) images, focusing on the following aspects:
The corpus luteum that we have seen () is located within the ovary, and the ectopic pregnancy was tubal.
Using the color flow Doppler, we identified reduced color flow, which supports the diagnosis of the corpus luteum.
In the course of the surgical intervention, we were able to precisely pinpoint the corpus luteum and observe the associated physiological changes in the left ovary”.
Treatment
The patient consented to the surgical management of ectopic pregnancy, in which she was taken to the emergency theater for diagnostic laparoscopy and left salpingectomy.
In the abdominal cavity exploration conducted via laparoscopy, a significant quantity of blood was observed to fill the Pouch of Douglas, amounting to 500 milliliters. In response, appropriate measures were taken to suction and irrigate the accumulated blood. Further examination revealed a ruptured ectopic pregnancy at the ampulla site of the left tube, measuring 2 centimeters. The left ovary displayed normal physiological indications alongside the presence of a corpus luteal cyst, while the right tube and right ovary exhibited no abnormalities.
Given the advancement of laparoscopic techniques, the utilization of bipolar current has replaced the previous employment of mono-polar current [Citation6]. Accordingly, the left tube was coagulated using bipolar current and subsequently severed. The THUNDERBEAT® seal and cut system were employed for this purpose. Emphasis was placed on ensuring adequate hemostasis, ultimately leading to the preservation of the patient’s left ovary. The excised tissue was promptly sent for histopathological analysis, and the patient received a comprehensive post-operative briefing.
Overall, the surgical procedure was executed successfully, yielding satisfactory outcomes.
Outcome and follow up
The medical team may have anticipated some satisfactory outcomes, but it would be irresponsible to ignore the patient’s perspsective.
The outcome from the medical team’s view
We made an accurate diagnosis of ectopic pregnancy, which could have been masked by the previous scan results which showed an intrauterine early pregnancy. We have decided on time to operate on this patient, we did a successful operation in which we controlled the internal bleeding and managed the relocating ruptured ectopic pregnancy. The histopathology confirmed the diagnosis of ectopic pregnancy; as the histology showed a Fallopian tube with dilated lumen containing chorionic villi in blood clot, confirming ectopic pregnancy.
Outcome from the patient’s perspective
The patient appreciated how the team dealt with her emergency and saved her life. However, we cannot neglect the feelings that were considered by the patient, we cannot ignore counting the outcomes from the patient’s point of view:
The patient had shocking news to hear that her pregnancy is no longer intrauterine. The outcome of losing one tube as it was necessary to be removed as a part of the surgical management of the ectopic pregnancy to stop bleeding and to prevent any possibility of having ectopic in the future from the same side.
Despite the patient was so emotional for hearing that she had two different situations at the same time; miscarriage and ectopic pregnancy, however, she understood the situation and at least realized that she still had the chance to have a normal conception in the future from the other side. The patient appreciated as well that her left ovary hadn’t been damaged or removed during the operation.
The patient’s recovery went well. We supported the patient emotionally and offered more detailed debriefing sessions if needed. The patient stayed for one night after the procedure and was discharged home the next day. The post-operative blood tests were normal with no much drop in her Haemoglobin level after the procedure.
We agreed with the patient that once she plans and gets pregnant, we will arrange early appointments and follow-ups in the early pregnancy unit.
Discussion
Although ectopic pregnancies that are associated with another intrauterine pregnancy come in a variety of forms, they all fall under the umbrella term of heterotopic pregnancy, which describes the detection of multiple pregnancies at different sites. Heterotopic pregnancies are unusual, but they should not be ruled out if the patient’s clinical presentation or pelvic imaging raises suspicions [Citation4].
Interestingly, some women have reported having heterotopic pregnancies, in which one pregnancy develops normally in the uterine cavity while the other develops in a different uterine or pelvic location. These alternative sites include the tubes, the cervical canal [Citation5], the cesarean section scar [Citation7], the ovarian location [Citation8], and other sites.
Multiple reports of heterotopic pregnancies have been documented in the literature, including cases of quadruplet pregnancy [Citation3] and triplet pregnancy with twin tubal pregnancy [Citation9]. In regards to the gestational ages, an ectopic pregnancy on top of a 26-week intrauterine pregnancy is one of the rarest examples recorded in the literature [Citation10].
We can consider our case report to be a rare case of a unique and rare ailment because no situations involving the relocating ectopic pregnancy on top of the miscarriage of intrauterine pregnancy have been found in the literature.
From the patient’s scenario, and based on the patient’s history and the findings of the various investigations, we may conclude that the pregnancy began in the uterus, underwent a miscarriage process, and then an ectopic pregnancy appeared at (the left tube), becoming an ectopic pregnancy. This is one of the most unusual cases of its kind to be described in the medical literature as it is a rare type of heterotopic pregnancy.
To determine the most suitable approach for management of ectopic and or heterotopic pregnancy, various factors such as clinical presentation, gestational age at diagnosis, beta-human chorionic gonadotropin (β-hCG) levels, ultrasound findings, and patient preferences must be carefully considered. An interesting article published in 2020 highlights two cases of ectopic pregnancy effectively treated with systemic Methotrexate (MTX) and Mifepristone, even in the presence of significant β-hCG levels and vital embryos. The cases demonstrated favorable outcomes, with β-hCG levels becoming undetectable in relatively short periods, emphasizing the potential of a combined protocol consisting of systemic multidose MTX therapy along with a single oral dose of Mifepristone as a first-line approach, especially in asymptomatic patients. The management of IP remains a subject of ongoing debate, but these cases suggest that this combined regimen can be a viable option, even in instances with elevated serum β-hCG levels [Citation11].
Conclusion/learning points/take home messages
This case report describes the ectopic pregnancy that happened on top of a missed miscarriage, which is extremely unusual but should be reported nonetheless because it will diversify the scientific encyclopedia and encourage healthcare professionals to consider all possible outcomes.
To guide and accomplish proper management, a multidisciplinary team (MDT) strategy was necessary. Our on-call gynecology team, early pregnancy unit staff, anaesthetic team, nurses, and operating room staff all did outstanding work to ensure this patient’s smooth and successful operation and recovery.
Clinical signs should never be disregarded, and all relevant investigations should be used correctly to get an appropriate diagnosis.
Author contribution
* Mena Abdalla (The author) has done all related data related to this case report including:
Abstract.
Collecting data
Literature of review – manuscript writing
Case report and discussion.
Data sharing
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Informed consent
Written informed consent (Consent to Participate and Consent to Publish) was obtained from the patient. All photos on this article have been taken with the patient’s consent.
Informed consent
Written informed consent (Consent to Participate and Consent to Publish) was obtained from the patient. All photos in this article have been taken with the patient’s consent.
Disclosure statement
No potential conflict of interest was reported by the author.
Additional information
Funding
References
- American College of Obstetricians and gynecologists’ committee on practice bulletins—gynecology. ACOG practice bulletin no. 193: tubal ectopic pregnancy. Obstet Gynecol. 2018;131(3):e91–e103. doi: 10.1097/AOG.0000000000002560
- Lyu J, Ye H, Wang W, et al. Diagnosis and management of heterotopic pregnancy following embryo transfer: clinical analysis of 55 cases from a single institution. Arch Gynecol Obstet. 2017;296(1):85–92. doi: 10.1007/s00404-017-4384-y
- Cimpoca B, Moldoveanu A, Gică N, et al. Heterotopic quadruplet pregnancy: literature review and case report. Medicina. 2021;57(5):483. doi: 10.3390/medicina57050483
- Nguyen KP, Hudspeth M, Milestone H. Spontaneous heterotopic pregnancy: Diagnosis and management. Case Rep Obstet Gynecol. 2022;2022:1–4. doi: 10.1155/2022/2994808
- Fan Y, Du A, Zhang Y, et al. Heterotopic cervical pregnancy: case report and literature review. J Obstet Gynaecol Res. 2022;48(5):1271–1278. doi: 10.1111/jog.15193
- Elnaggar EA, Elwan YA, Ibrahim SA, et al. Hormonal changes after laparoscopic ovarian diathermy in patients with polycystic ovarian syndrome. J Obstet Gynecol India. 2016;66(S1):528–533. doi: 10.1007/s13224-016-0882-2
- Marchand GJ, Masoud AT, Coriell C, et al. Treatment of cesarean scar ectopic pregnancy in China with uterine artery embolization—a systematic review and meta-analysis. J Clin Med. 2022;11(24):7393. doi: 10.3390/jcm11247393
- Al Naimi A, Moore P, Brüggmann D, et al. Ectopic pregnancy: a single-center experience over ten years. Reprod Biol Endocrinol. 2021;19(1):19. doi: 10.1186/s12958-021-00761-w
- Simsek T, Dogan A, Simsek M, et al. Heterotopic triplet pregnancy (twin tubal) in a natural cycle with tubal rupture: case report and review of the literature. J Obstet Gynaecol Res. 2008;34(4pt2):759–762. doi: 10.1111/j.1447-0756.2008.00921.x
- Kajdy A, Muzyka-Placzyńska K, Filipecka-Tyczka D, et al. A unique case of diagnosis of a heterotopic pregnancy at 26 weeks – case report and literature review. Bmc Pregnancy Childbirth. 2021;21(1):21. doi: 10.1186/s12884-020-03465-y
- Stabile G, Romano F, Buonomo F, et al. Conservative treatment of interstitial ectopic pregnancy with the combination of mifepristone and methotrexate: our experience and review of the literature. Bio Med Res Int. 2020;2020:1–7. doi: 10.1155/2020/8703496