Abstract
Depression is associated with cognitive deficits and changes in the brain. Major depression is often associated with cognitive problems; however, there are only a few studies that have focused on the systematic use of cognitive remediation in depression. The objective of this study was to assess the effectiveness of computerized cognitive remediation in depressed patients with cognitive dysfunction. Patients (n = 20) with depression were randomly assigned to the active or control group. The active intervention (computerized cognitive remediation) comprised 12 sessions focused on the remediation of attention and executive functions through the CogniPlus software. All participants completed neuropsychological testing before and after the intervention. A mixed-design analysis of variance revealed a significant time × group interaction in the attention and planning task, on the Beck Depression Inventory and on the Shifting, Emotional Control and Initiating sub-scales of the Behavior Rating Inventory of Executive Function-Adult. The results showed that patients undergoing cognitive remediation improved in domains related to attention and executive functions and scored significantly lower on the Beck Depression Inventory. The findings provide some evidence that cognitive remediation could be an efficient approach to dealing with cognitive deficits in depression.
Introduction
Depression is a very common disease that is prevalent throughout the world. According to some data, depression affects more than 264 million people (WHO, Citation2017). The depressive disorder presents a difficulty for public health, with a prevalence ranging from 10% to 25% for women and 5% to 12% for men (APA, Citation1994). Major depressive disorder (MDD) is considered the most severe subcategory of depressive disorders; it has a high level of comorbidity with other mental illnesses in clinical samples (Gao et al., Citation2013). The individual usually exhibits a depressed mood, loss of interest of enjoyment, and reduced energy leading to increased fatigability and diminished activity. Other common symptoms are disturbed sleep, diminished appetite, ideas or acts of self-harm or suicide, reduced self-esteem, and reduced concentration and attention (WHO, Citation1992). Major depression is often associated with cognitive impairment and may predominate over the clinical picture, affect the overall functioning of the affected individual, and cause so-called pseudodementia (Perini et al., Citation2019).
The impairment of executive functions and attention in depressive disorders
Cognitive dysfunction is a core feature of depressive disorder, and it is the main reason for the reduced ability to function (Pan et al., Citation2019). Cognitive deficits continue to persist after the elimination of emotional symptoms, which reflects the distinction between mood symptoms and cognitive symptoms during the depression (Zuckerman et al., Citation2018).
Authors have reported on deficiencies in various cognitive domains, such as executive functions, attention, memory, and psychomotor speed (Hammar & Årdal, Citation2009). Patients with depression experience deficits in a variety of tasks associated with attention (Hammar et al., Citation2003), even though it is difficult to determine precisely the nature of the impairment because different studies have investigated different aspects of the concept of attention. In addition, attention is closely related to other cognitive domains, especially more complex forms of attention with executive functions. It has been established that depression is associated with impairment related to the speed of processing, while functions of selective attention are believed to remain intact (Pardo et al., Citation2006).
The acute phase of depressive disorder is frequently reported to include a decline in executive function; deficiencies occur with regard to tasks of problem-solving and planning (Naismith et al., Citation2003), mental flexibility (Naismith et al., Citation2003), verbal fluency (Reischies & Neu, Citation2000), decision-making and working memory (Rose & Ebmeier, Citation2006), and inhibitory control (Hugdahl et al., Citation2009). Furthermore, researchers have suggested that lack of mental flexibility or shifting between mental sets, respectively, is the most evident deficiency in the executive function of patients with depression (Austin et al., Citation2001).
Paelecke-Habermann et al. (Citation2005) predicted that patients with depression would show cognitive efficiency in areas of attention and executive functions compared with the control group (healthy participants). They also maintained that patients experiencing an acute manifestation of this disorder would perform poorer in neuropsychological tests compared with patients with mild manifestations of the illness. Results from the three domains of attention (visual orientation, sustained attention, and executive attention) confirm the hypothesis that in patients with depression, cognitive dysfunction in the domain of attention and executive functions is also present during remission. The authors defined remission as a period of at least 3 months during which the participants do not meet the criteria of a depressive episode. The groups of patients with depression did not differ in terms of the level of dysfunction in the attention tasks; however, patients with acute manifestations of the disease showed a significantly higher level of impairment in their executive function tasks than those with a mild manifestation of the illness (Paelecke-Habermann et al., Citation2005). While it has been established that depression increases the risk of cognitive impairment, recently obtained evidence shows that cognitive dysfunction during remission also increases individuals’ vulnerability to longer periods of illness and relapse (Gotlib & Joormann, Citation2010).
Irrespective of the specific dysfunction of cognitive domains in patients with depression, the latter are believed to show a decline in the more demanding tasks requiring cognitive, while exhibiting normal functioning when it comes to automatized tasks. Automatized processing of information differs from complex/higher-level processing in that the latter demands well-focused attention and motivation (Hammar et al., Citation2003).
Cognitive impairments in patients with depression can also forecast a less favorable outcome in anti-depressive therapy (Kampf-Sherf et al., Citation2004) and cognitive-behavioral interventions (Crews & Harrison, Citation1995). Deficits in the attentional system and executive functions frequently contribute to poor therapeutic outcomes. Namely, a study by Dunkin et al. (Citation2000) reported that there were no significant differences among participants in their response to antidepressants regarding age, education, premorbid intelligence quotient (IQ), or the number of previous depressive episodes; however, participants who did not respond well to antidepressants performed significantly poorer in executive function tests than those who did respond well.
Neuroplasticity as a basis for cognitive remediation in the case of depression
The prefrontal cortex (PFC) is considered a significant neurological center of behavioral regulation and it is also connected to depression (Liu et al., Citation2017). Functional brain imaging studies in patients with depression have consistently disclosed hypometabolism in certain parts of the PFC and the basal ganglia (Dunkin et al., Citation2000). A study of positron emission tomography, looking into the cerebral metabolism of glucose in patients with unipolar depression, showed that depressive disorder correlates with abnormalities of the left dorsal anterolateral PFC (Baxter et al., Citation1989). The activation of the dorsolateral, medial ventrolateral, and dorsal frontal cingulate cortex (FCC) is associated with a wide range of (different) cognitive domains, such as perception, executive control, working memory, inhibition of response, and problem-solving (Duncan & Owen, Citation2000).
Depression causes changes in synaptic plasticity; these alterations are linked with structural and functional changes in the hippocampus. The efficiency of transmission through synapses depends on the modulation of connectivity between neurons and neural circuits and adaptation to the environment (Marsden, Citation2013). Indeed, we can assume that if a healthy brain is capable of changing its function and structure as it acquires new knowledge and skills, a brain that has changed due to illness should, after recuperating, be able to achieve at least partial functional recovery with the help of similar mechanisms and techniques. Every time we acquire new knowledge or skills (with repeated practice), the synaptic communication between neurons grows stronger. With each new trial, re-establishment of the neuron cycle and reinstatement of neural transmission between the involved neurons enhance the efficiency of synaptic transmission. Communication between the relevant neurons is thus facilitated, and cognitive activities are carried out at an increasingly faster pace (Kolb et al., Citation2010). These are the principles of the concept of cognitive remediation and rehabilitation.
Methods of cognitive remediation
Recent developments in therapeutic research have witnessed a strong emphasis on the importance of neuropsychology in the field of rehabilitation of psychiatric diseases. Cognitive remediation can influence the structure and functioning of the brain and also highlight the effects they have on neurobiological systems in the case of mood disorders and illnesses such as schizophrenia (Bell et al., Citation2003). Over the last 20 years, cognitive remediation therapy (CRT) had been used to reduce deficits in the field of attention, memory, information processing, visual-spatial perception, visual-constructional abilities, planning, and reasoning, especially in patients with brain damage, early stages of dementia, schizophrenia, and hyperactivity with the lack-of-attention disorder (Beck et al., Citation1988; Deckersbach et al., Citation2010; O’Connell et al., 2006; Yehuda & Diller, Citation1993). Cognitive remediation is a non-pharmacological method aimed at improving cognitive functions in people with mental health issues. It developed from the realization that in chronic schizophrenia, for example, more cognitive impairment leads to a poorer outcome in the treatment (Wykes et al., Citation1992). Cognitive remediation can be carried out via computer-aided programs of various lengths and complexity. They can also be implemented by individually trained clinicians. It has proven to be an effective method, especially when combined with vocational rehabilitation (Galletly & Rigby, Citation2013). Although cognitive deficits in patients with depression differ from those in patients with neurological illnesses or schizophrenia, studies suggest that targeted interventions can partially improve altered functions (Porter et al., Citation2013). Cognitive remediation involves repeated exercises, training, and strategies aimed at improving and compensating for the deficits, while at the same time the goal is to transfer these habits into everyday functioning and work (Fan et al., Citation2017).
With the development of computer technology, CRT has in recent years has evolved into computerized cognitive remediation therapy (CCRT). Based on neuroplasticity, clinicians use this treatment to improve cognitive functions with the activation and training of specific neural networks in the brain. With CCTR is needed less staff time as one staff member can supervise several participants, and staff does not require specialized skills (Galletly & Rigby, Citation2013).
Although there is strong empirical evidence in favor of the use of cognitive remediation in patients with schizophrenia, there are only a few studies in which researchers have assessed the efficiency of cognitive remediation on samples of individuals with depression. We can assume that in the case of patients with depression, there will be a significant improvement in the scores of neuropsychological tests after cognitive remediation, both in self-reported and objective measures. Nevertheless, Fan et al. (Citation2017) emphasized the need for continued development and establishment of more targeted and standardized cognitive remediation, the need for larger samples of patients with mental disorders, and the need for further study of factors influencing the efficiency of cognitive remediation.
Methodology
All participants signed a consent form prior to entering the research project. They received a detailed explanation of the aim of the study and how it would develop. The study was approved by the research ethics committee of the University Rehabilitation Institute (URI) Soča.
Participants
The research sample comprised 20 patients with depression who had previously been diagnosed with depressive episodes by a psychiatrist in accordance with the adopted International Classification of Disease, 10th revision (ICD-10; WHO, Citation1992). At the time, they also had at least a mild level of depression according to the Beck Depression Inventory (BDI). The participants involved in this study came from the Centre for Vocational Rehabilitation at the URI. They had been referred to work rehabilitation through employment services or they had been included in programs of vocational rehabilitation through health care for assessing their ability to work and the amount and type of help they needed to return to work. The experimental group comprised 10 participants subjected to CCRT. The control group, with 10 participants with depression, was similar to the experimental group in terms of gender and age, but they did not receive cognitive remediation. Patients in both groups had a long-term history of depressive disorder and did not differ significantly in the length of disease duration. Data were obtained from the patient’s medical records, the date of the first onset of the disease was recorded. Both groups were subjected to antidepressant therapy, and none of the participants started a new program of psychotherapy during rehabilitation. Patients with simultaneous psychological illnesses of other kinds, substance abuse, defects of sight or hearing, organic pathologies, intellectual deficiencies, or major physical disorders were not included in the study.
Cognitive assessments
Test for Attentional Performance
We selected the Test for Attentional Performance (TAP; Zimmermann & Fimm, Citation2016) attention tasks from the computerized test battery to assess the following components: Alertness, Go/No Go, Divided Attention, and Flexibility. The test battery was first published in 1992 and is based on the measurement of specific functions of attention with the help of simple reaction times paradigms.
Alertness is a simple task of psychomotor reaction to a visual stimulus with or without a sound signal. In the first 20 trials and in the final part, the stimulus appears on the screen without warning (Part A), while in Part B the warning tone appears before the impulse does (Catale et al., Citation2009). The Divided Attention task consists of simultaneously performing the visual and listening tasks. The task takes into consideration the reaction times as well as the incorrect recognition of tones and errors of omission (Catale et al., Citation2009). The Go/No Go task of selection and inhibition is a selective task, which estimates the ability of detection and recognition of target stimuli (× symbol) by pressing the response button, and by inhibiting the response to similar but insignificant stimuli (+ symbol). The Flexibility task is one of switching between two different modalities of the stimulus. Our task involved a more complex condition, namely the alternating track condition: letter–number (Zimmermann & Fimm, Citation2016).
Tower of London (TOL)
TOL tasks and variants have been frequently used in clinical and experimental neuropsychology to measure executive functions of planning and problem-solving (Berg & Byrd, Citation2002). In the task, planning is essential for an efficient transition from a given initial state to the desired target state, namely for optimal problem-solving in the fewest possible number of moves (Kaller et al., Citation2012). With regard to difficulty, the test should be able to successfully discriminate between high and low achievers, and the authors also reported a satisfactory split-half coefficient of reliability (r = 0.72) and internal consistency (Cronbach’s α = 0.69; Kaller et al., Citation2012).
Self-reported cognitive measures
Behavior Rating Inventory of Executive Function-Adult (BRIEF-A)
BRIEF-A was developed as a tool to assess the efficiency of executive functions with adults in day-to-day functioning (Gioia et al., Citation2000). It consists of 75 questions comprising nine clinical scales and two higher-order indices: the Behavioral Regulation Index (BRI; including the scales Inhibition, Switching, Emotional Control, and Self-Control) and the Metacognition Index (MCI; including Initiation, Working Memory, Planning/Organization, Control of Tasks, and Organization of Materials). Analyses of reliability (Roth et al., Citation2005) have shown high internal consistency of the two indices (the MCI and the BRI) as well as the GEC (Cronbach’s α = 0.96). The self-evaluation questionnaire asks the participant above all to verify the extent to she or he felt that the skills obtained in trained tasks were transferred into areas, which were not directly targeted by the remediation (namely, emotional regulation, initiation, planning, and working memory).
Clinical measures
BDI-II
The BDI emerged from clinical observations of behavior and symptoms often exhibited by patients with depression but seldom expressed by undepressed psychiatric patients (Beck et al., Citation1961). Clinical observations were systematically combined into 21 symptoms in the form of items rated from 0 to 3, depending on the intensity. The questionnaire takes 5–10 min and the total score is obtained by summing the results of each of the 21 items (Beck et al., Citation1988). The authors reported high internal consistency in psychiatric samples as well as in the population of non-psychiatric individuals—the average Cronbach’s α was 0.87, and the test–retest estimate of reliability showed a correlation of over 0.60 (Beck et al., Citation1988).
Intervention
CogniPlus
We used the computerized rehabilitation system CogniPlus for remediation of impaired cognitive functions. The system is easy to use, namely, it has a small number of large buttons, the instructions are simple, and the program itself provides a user-friendly environment, suitable for people who are not accustomed to using the computer. The program recognizes the level of the participant’s abilities and automatically adjusts to them, and it increases the complexity of the tasks as the participant progresses (Schuhfried, Citation2017). Each session is followed by the computer displaying the analysis of success in a single session and between individual sessions. In addition, every patient has the option of following the number and percentage of errors made and the speed of response for her or his own information (Starovastnik Žagavec & Čuš, Citation2013). The present research includes training pertaining to functions of attention and executive abilities, namely the ALERT (which includes the ability of temporary enhancement and sustaining of attention), SELECT (training of selective attention, the ability of speedy response to appropriate stimuli, and inhibition of inappropriate responses), FOCUS (ability to respond only to appropriate stimuli in the midst of a high level of distraction), DIVIDE (ability to perform multiple tasks simultaneously), and HIBIT-R (inhibition abilities) tasks. In CogniPlus the ability dimensions being trained are almost always embedded in lifelike scenarios, which offers more realistic and perhaps motivating design.
Procedure
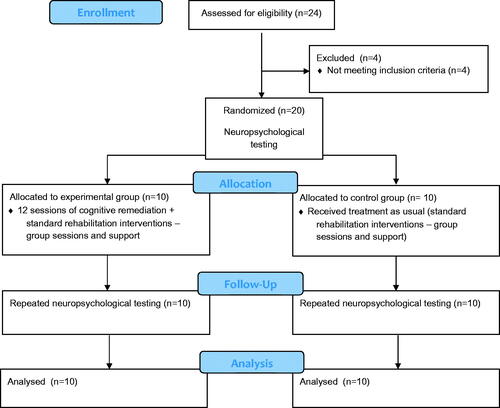
Participants in our study had taken part in vocational rehabilitation and were selected because they were previously diagnosed with depressive disorder by their psychiatrist. Upon entrance to the vocational rehabilitation program, we administered to participants with a diagnosis of a depressive episode a checklist containing symptoms that represent exclusion criteria (head injury, other psychiatric diagnoses, neurological diseases…). The experimental group carried out cognitive training individually, in a quiet space. The training took place over a period of 10 weeks and each participant received 12 sessions. The length of each session ranged from 40 to 50 min. Before the start of each session, the participant together with the experimenter read and repeated the instructions, which were again introduced by the program at the beginning of each session. Each task from the CogniPlus battery is tailored to a specific deficit because studies have shown that the use of too complicated tasks can actually worsen efficiency. The level of difficulty during the course of the sessions automatically adjusted to the participant’s progress. Neuropsychological testing was carried out before and after the cognitive remediation, and the results, afterward, were presented and explained to the participants. The control group received treatment as usual which included standard rehabilitation interventions in the vocational rehabilitation center in the form of group treatments and support, which was also provided to the experimental group. The procedure is thoroughly presented in the flow diagram in .
Statistical analyses
We examined the effects of cognitive remediation on reducing depression and improving cognitive functions using a mixed-design analysis of variance (ANOVA), with time (measured before and after remediation) as the within-group factor and group (experimental and control) as the between-groups factor. As the repetition of identical tests could generate an alpha error or false positive, the level of statistical significance was lowered from 0.05 to 0.01.
Results
Efficiency of random arrangement among groups
There were no significant differences between the experimental and control groups with regard to age, years of education, gender, and disease duration ().
Table 1. Demographic and clinical characteristics of the sample.
We used the t-test for independent samples to verify whether in the initial measurements (prior to remediation) there were differences between the two groups. There were no statistically significant between-group differences on any of the included scales ().
Table 2. t-Test results for independent samples, comparison between groups before the intervention.
Results of cognitive measures (TOL, TAP)
We used multivariate analysis of variance (MANCOVA) to examine whether the performance on TOL tasks was different between the groups in the post-treatment phase. To this end, we used the post-treatment TOL test results as the dependent variables, while pre-treatment TOL test results were the covariates. There was a difference between the experimental and the control group on the post-treatment TOL test (F(4, 11) = 10.39, p = 0.001, Pillai’s Trace = 0.27, η2 = 0.79). In addition, the mixed-design ANOVA () revealed that the remediation (time × group) had an impact on the total move score (TOL A), the number of correct solutions (TOL B), and total problem-solving time (TOL C), but not on total execution time. This means that the experimental group in post-treatment testing exhibited a significantly greater improvement in results compared with the control group.
We used MANCOVA to evaluate differences in the post-treatment TAP test results between the groups. The results of the tests after remediation served as dependent variables, while the results of the pre-treatment test functioned as covariates. There was an experimental impact (the influence of rehabilitation; F(4, 11) = 6.06, p = 0.008, Pillai’s Trace = 0.69, η2 = 0.69). This means that taking into account the pre-treatment test results, there was a statistically significant difference in the post-treatment TAP test results between both groups. The mixed-design ANOVA () revealed a significantly greater improvement in post-treatment test in the experimental compared with the control group on the Alertness (TAP A), Inhibition (TAP B), Flexibility (TAP C), and Divided Attention (TAP D) tasks. The effect sizes (η2s > 0.30) also point to significant improvement. We conclude that all TAP scales indicate the efficiency of computer-assisted remediation.
Self-reported cognitive measure (BRIEF-A)
We applied the BRIEF-A questionnaire because we were interested in whether there were also statistically significant differences between groups in the subjective experience of cognitive improvement. We evaluated this possibility using MANCOVA, with the results of BRIEF-A sub-scales after remediation as dependent variables and the pre-treatment results as covariates. There was a difference between the groups in terms of subjective reporting after remediation, considering the results of the first measurement (F(6, 7) = 18.96, p = 0.001, Pillai’s Trace = 0.94, η2 = 0.94). The mixed-design ANOVA () showed significantly greater improvement in post-treatment results of experimental than the control group on the Shift (BRIEF B), Emotional Control (BRIEF C), and Initiate (BRIEF D) scales, but not on the Inhibition (BRIEF A), Working Memory (BRIEF E), and Plan/Organize (BRIEF F) scales.
Table 3. Means, standard deviations, and mixed ANOVA after intervention.
Measure of depression (BDI)
The mixed-design ANOVA showed that there was no group effect (F(1, 18) = 0.04, p = 0.840, η2 = 0.00). However, the test did show a time effect (F(1, 18) = 14.98, p = 0.001, η2 = 0.45), which testifies to the improved post-treatment results, even if the group type was not taken into account. There was also a time × group interaction (F(1, 18) = 9.92, p = 0.006, η2 = 0.35). This finding indicates that group type, namely one group of patients who underwent treatment and one group of patients who did not receive treatment, significantly influenced the improvement in post-treatment results. The results thus suggest that the participants in the experimental group scored significantly lower on the BDI and reported significantly greater improvement in mood in post-treatment testing compared with the control group.
Discussion
In a pilot study, we aimed to verify the effectiveness of cognitive remediation and to assess potential improvements in cognitive functioning and mood on a sample of patients with depression. In this respect, we were primarily interested in the areas of attention and executive functions. Psychological tests were carried out in pre-treatment, assessing functions of psychomotor response, selective and divided attention, and flexibility. In addition, planning/organizing abilities, working memory, and speed of problem-solving were assessed in the executive domain. Cognitive remediation was carried out in a computerized manner over a period of a month and a half. Upon its completion, the post-test was performed using the same tests.
The first significant finding in our research relates to an improvement in cognitive functions related to attention and executive functions. In the domain of executive functions, after cognitive remediation, the experimental group showed significant improvement in planning abilities, problem-solving, and the speed of problem-solving, measured by the TOL test (Shallice, Citation1982). Objective measurements were coupled with subjective executive function measures from the self-report BRIEF-A questionnaire (Roth et al., Citation2005). There was a significant improvement in functions of switching, initiation, and emotional control; these findings indicate that post-treatment the participants reported increased mental flexibility, greater ease of initiation of activities and switching between activities and better control of emotional responses. Our findings are consistent with Elgamal et al. (Citation2007), who claimed that participants who received cognitive training showed improvements in the neuropsychological tests of attention, verbal learning, psychomotor skills, and executive functions.
In the area of attention, after cognitive remediation, the experimental group showed considerable improvement in functions of selective attention (selection of targeted and non-targeted impulses), psychomotor reactivity (speed of psychomotor reactions), divided attention (simultaneous paying attention to two modalities of impulses), and flexibility (ability to switch between two modalities). There is compelling evidence for remediation after a stroke, where researchers have reported that computerized cognitive training resulted in activation of the frontal lobe and improved memory and attention in stroke patients (Hwi-Young et al., Citation2015). While, as researchers have pointed out, the physiological mechanism responsible for cognitive restoration remains unknown, studies do support the fact that repetitive exercising and training could prove an efficient means of improving cognitive functioning also in the case of psychiatric illnesses (Elgamal et al., Citation2007).
Alongside improvement in cognition, our second significant finding associate with the decline in depressive mood following the CCRT, namely the experimental group reported significantly greater improvement in mood compared with the control group. A previous study reported similar results in a sample of elderly adults; the researchers revealed that computerized cognitive intervention, targeted at executive functions, improved the mood and cognitive functions in the case of depression in later periods of life (Morimoto et al., Citation2014). Naismith et al. (Citation2011) randomized 44 patients to receive cognitive intervention and found no effect on mood, perhaps unsurprisingly given the low baseline level of depression. Improvement in the area of emotional regulation and, consequently, better control of negative emotional states could be seen as a mediator in support of the aforementioned finding that cognitive remediation had a positive effect on the mood of the participants in the experimental group.
Cognitive remediation affects the areas of the brain that are associated with depression; thus, it is possible to assume that it indirectly alleviates the symptoms of depression. Elgamal et al. (Citation2007) tested a sample of 12 patients with depression and found that cognitive remediation in the case of these patients compared with a control group receiving treatment as usual resulted in a significant improvement in cognitive functions. However, there was no improvement in the patients’ mood. Indeed, both groups reported relatively low values on the Hamilton Depression Rating Scale during initial measurements, which probably lessened the possibility of observing a significant difference after remediation.
Finally, we wish to reflect on the transfer or generalization of cognitive improvement to other areas. In our study, the directly trained/targeted areas involved psychomotor response, divided and selective attention, maintained attention, and inhibition. We also observed improvement in domains not directly targeted by our intervention, such as the ability to plan/organize, flexibility, and emotional regulation or control. The participants, however, did not report improvement in the domains of working memory and inhibition, even though objective measures proved just that, namely that there was an improvement in inhibition. Thus, our findings regarding generalization to other cognitive domains are not uniform. Furthermore, in the experimental group, we did not observe improvement in all the trained tasks. Another investigation that studied attention, executive functions, verbal learning, and memory (Elgamal et al., Citation2007) arrived at similar findings, which can be attributed to several factors, including the possibility that aspects of some of the tasks differ from those cognitive functions that were targeted by the remediation. Another reason for this might be that some but not all cognitive functions measured with our assessment battery were subjected to generalization.
Limitations of the study
One of the limitations of the study is the relatively small number of participants. Despite limited power, however, we found a number of significant performance improvements related specifically to the effects of the cognitive intervention. Our approach relied upon multiple analyses, raising the possibility of Type I errors. We consider this unlikely, however, given the consistency of positive findings both within and across our different cognitive measures. As the repetition of identical tests could generate an alpha error or false positive, the level of statistical significance was also lowered from 0.05 to 0.01. Future studies should involve larger numbers of participants in the experimental and control groups. In addition, those areas of the memory system that are known to be prone to damage and a decrease in functionality connected to depression should also be evaluated. It would also be useful to verify the extent to which the program influenced the quality of life of our respondents. The study also does not shed a light on the persistence of the effects of cognitive remediation over a longer period of time. There is a general lack of studies that have investigated the long-term effect of cognitive intervention in terms of follow-up studies months after the completion of the training or the program.
Conclusion
Computerized cognitive remediation in the case of psychiatric illnesses can be an efficient intervention means for improved cognitive functioning in patients, with schizophrenia showing most of the evidence for this claim. The present study implies that cognitive remediation can provide an efficient, albeit simple and economical approach to dealing with depression. In the future, it could be integrated into the holistic treatment of psychiatric patients, as it tends to be a key part of the mosaic of long-term/lasting rehabilitation and relapse prevention in psychiatric patients.
Additional information
Funding
References
- Airaksinen, E., Larsson, M., Lundberg, I., & Forsell, Y. (2004). Cognitive functions in depressive disorders: Evidence from a population-based study. Psychological Medicine, 34, 83–91.
- APA. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). American Psychiatric Association.
- Austin, M. P., Mitchell, P., & Goodwin, G. M. (2001). Cognitive deficits in depression: Possible implications for functional neuropathology. British Journal of Psychiatry, 178, 200–206.
- Baxter, L. R., Schwartz, J. M., Phelps, M. E., Mazziotta, J. C., Guze, B. H., & Selin, C. E. (1989). Reduction of prefrontal cortex glucose metabolism common to three types of depression. Archives of General Psychiatry, 46, 243–250. https://doi.org/10.1001/archpsyc.1989.01810030049007
- Beck, A. T., Steer, R. A., & Carbin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8, 77–100.
- Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571.
- Beck, C., Heacock, P., Mercer, S., Thatcher, R., & Sparkman, C. (1988). The impact of cognitive skills remediation training on persons with Alzheimer’s disease or mixed dementia. Journal of Geriatric Psychiatry, 21(1), 73–88.
- Bell, M., Bryson, G., & Wexler, B. E. (2003). Cognitive remediation of working memory deficits: Durability of training effects in severely impaired and less severely impaired schizophrenia. Acta Psychiatrica Scandinavica, 108, 101–109.
- Berg, W. K., & Byrd, D. (2002). The tower of London spatial problem-solving task: Enhancing clinical and research implementation. Journal of Clinical and Experimental Neuropsychology, 24, 586–604.
- Catale, C., Marique, P., Closset, A., & Meulemans, T. (2009). Attentional and executive functioning following mild traumatic brain injury in children using the Test for Attentional Performance (TAP) battery. Journal of Clinical and Experimental Neuropsychology, 31(3), 331–338.
- Crews, D. W., & Harrison, W. D. (1995). The neuropsychology of depression and its implications for cognitive therapy. Neuropsychology Review, 5, 81–123.
- Deckersbach, T., Nierenberg, A. A., Kessler, R., Lund, H. G., Ametrano, R. N., Sachs, G. (2010). Cognitive rehabilitation for bipolar disorder: An open trial for employed patients with residual depressive symptoms. CNS Neuroscience & Therapeutics, 16(5), 298–307. https://doi.org/10.1111/j.1755-5949.2009.00110.x
- Duncan, J., & Owen, A. M. (2000). Common regions of the human frontal lobe recruited by diverse cognitive demands. Trends in Neurosciences, 23, 475–483.
- Dunkin, J. J., Leuhter, A. F., Cook, I. A., Kasl-Godley, J. E., Abrams, M., & Rosenberg-Thompson, S. (2000). Executive dysfunction predicts nonresponse to fluoxetine in major. Journal of Affective Disorders, 60, 13–23.
- Elgamal, S., McKinnon, M. C., Ramakrishnan, K., Joffe, R. T., & MacQueen, G. (2007). Successful computer-assisted cognitive remediation therapy in patients with unipolar depression: A proof of principle study. Psychological Medicine, 37(9), 1229–1238.
- Fan, Q., Liao, L., & Pan, G. (2017). The application of cognitive remediation therapy in the treatment of mental disorders. Shanghai Arch Psychiatry., 29, 373–375.
- Galletly, C., & Rigby, A. (2013). An overview of cognitive remediation therapy for people with severe mental illness. ISRN Rehabilitation, 2013, 1–6. https://doi.org/10.1155/2013/984932
- Gao, K., Wang, Z., Chen, J., Kemp, D. E., Chan, P. K., & Conroy, C. M. (2013). Should an assessment of Axis I comorbidity be included in the initial diagnostic assessment of mood disorders? Role of QIDS-16-SR total score in predicting number of Axis I comorbidity. Journal of Affective Disorders, 148(2–3), 256–264. https://doi.org/10.1016/j.jad.2012.12.004
- Gioia, G., Isquith, P. K., Guy, S. C., & Kenworthy, L. (2000). Test review: Behavior Rating Inventory of executive function. Child Neuropsychology, 6, 235–238.
- Gotlib, I. H., & Joormann, J. (2010). Cognition and depression: Current status and future directions. Annual Review of Clinical Psychology, 6, 258–312.
- Hammar, Å., & Årdal, G. (2009). Cognitive functioning in major depression—A summary. Frontiers in Human Neuroscience, 3, 26.
- Hammar, A., Lund, A., & Hugdahl, K. (2003). Selective impairment in effortful information processing in major depression. Journal of the International Neuropsychological Society, 9, 954–959.
- Hugdahl, K., Westerhausen, R., Alho, K., Medvedev, S., Laine, M., & Hämäläinen, H. (2009). Attention and cognitive control: Unfolding the dichotic listening story. Scandinavian Journal of Psychology, 50, 11–22.
- Hwi-Young, C., Ki-Tae, K., & Jin-Hwa, J. (2015). Effects of computer assisted cognitive rehabilitation on brain wave, memory and attention of stroke patients: A randomized control trial. The Journal of Physical Therapy Science, 27(4), 1029–1032.
- Kaller, C. P., Unterrainer, J. M., & Stahl, C. (2012). Assessing planning ability with the Tower of London Task: Psychometric properties of a structurally balanced problem set. Psychological Assessment, 24(1), 46–53. https://doi.org/10.1037/a0025174
- Kampf-Sherf, O., Zlotogorski, Z., Gilboa, A., Speedie, L., Lereya, J., & Rosca, P. (2004). Neuropsychological functioning in major depression and responsiveness to selective serotonin reuptake inhibitors antidepressants. Journal of Affective Disorders, 82, 453–459.
- Kolb, M., Muhammad, A. & Gibb, R. (2010). Searching for factors underlying cerebral plasticity in the normal and injured brain. Journal of Communication Disorders, 44(5), 503–514.
- Liu, W., Tongtong, G., Yashu, L., Zhenxiang, P., Jie, F., & Wei, Y. (2017). The role of neural plasticity in depression: From hippocampus to prefrontal cortex. Neural Plasticity 2017, 1–11. https://doi.org/10.1155/2017/6871089
- Marsden, W. N. (2013). Synaptic plasticity in depression: Molecular, cellular and functional correlates. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 43, 168–184. https://doi.org/10.1016/j.pnpbp.2012.12.012
- Morimoto, S. S., Wechsler, B. E., Liu, J., Hu, W., Seirup, J. & Alexopoulos, G. S. (2014). Neuroplasticity-based computerized cognitive remediation for treatment-resistant geriatric depression. Nature Communications, 5, 4579.
- Naismith, S. L., Hickie, I. B., Turner, K., Little, C. L., Winter, V., & Ward, P. B. (2003). Neuropsychological performance in patients with depression is associated with clinical, etiological and genetic risk factors. Journal of Clinical and Experimental Neuropsychology, 25, 866–877. https://doi.org/10.1076/jcen.25.6.866.16472
- Naismith, S. L., Diamond, K., Carter, P. E., Norrie, L. M., Redoblado-Hodge, M. A., Lewis, S. J. G. & Hickie, I. B. (2011). Enhancing memory in late-life depression: The effects of a combined psychoeducation and cognitive training program. The American Journal of Geriatric Psychiatry, 19(3), 240–248.
- O’Connell, R. G., Bellgrove, M. A., Dockree, P. M. & Robertson, I. H. (2006). Cognitive remediation in ADHD: Effects of periodic non-contingent alerts on sustained attention to response. Neuropsychological Rehabilitation, 16(6), 653–665.
- Paelecke-Habermann, Y., Pohl, J., & Leplow, B. (2005). Attention and executive functions in remitted major. Journal of Affective Disorders, 89, 125–135.
- Pan, Z., Park, C., Brietzke, E., Zuckerman, H., Rong, C., Mansur, R. B., Fus, D., Subramaniapillai, M., Lee, Y., & McIntyre, R. S. (2019). Cognitive impairment in major depressive disorder. CNS Spectrums, 24, 22–29. https://doi.org/10.1017/S1092852918001207
- Pardo, P. J., Pardo, J. V., Humes, S. W., & Posner, M. I. (2006). Neurocognitive dysfunction in antidepressant-free non – elderly patients with unipolar depression: Alerting and convert orienting of visuospatial attention. Journal of Affective Disorders, 92, 71–78.
- Perini, G., Cotta Ramusino, M., Sinforiani, E., Bernini, S., Petrachi, R., & Costa, A. (2019). Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatric Disease and Treatment, 15, 1249–1258.
- Porter, R. J., Bowie, C. R., Jordan, J. & Malhi, G. S. (2013). Cognitive remediation as a treatment for major depression: A rationale, review of evidence and recommendations for future research. Australian & New Zealand Journal of Psychiatry, 47(12), 1165–1175.
- Reischies, F. M., & Neu, P. (2000). Comorbidity of mild cognitive disorder and depression – a neuropsychological analysis. European Archives of Psychiatry and Clinical Neuroscience, 250, 186–193.
- Rose, E. J., & Ebmeier, K. P. (2006). Pattern of impaired working memory during major depression. Journal of Affective Disorders, 90, 149–161.
- Roth, R. M., Isquith, P. K., & Gioia, G. A. (2005). Behavior Rating Inventory of Executive Function—Adult Version: Professional manual. Psychological Assessment Resources.
- Schuhfried. (2017). CogniPlus. Schuhfried GmbH.
- Shallice, T. (1982). Specific impairments of planning. Philosophical Transactions of the Royal Society of London, Biology, 298, 199–209.
- Starovastnik Žagavec, B., & Čuš, A. (2013). Assessment and cognitive nevrorehabilitation of attentional deficits with TAP and CogniPlus software in stroke patients. Rehabilitacija, 12, 129–134.
- WHO. (1992). The ICD-10 classification of mental and behavioural disorders. World Health Organization.
- WHO. (2017). Depression, let’s talk. http://www.who.int/mental_health/management/depression/en/
- Wykes, T., Katz, R., Sturt, E. & Hemsley, D. (1992). Abnormalities of response processing in a chronic psychiatric group. A possible predictor of failure in rehabilitation programmes? The British Journal of Psychiatry, 160, 244–252.
- Yehuda, B-Y., & Diller, L. (1993). Cognitive remediation in traumatic brain injury: Update and issues. Archives of Physical Medicine and Rehabilitation, 74, 204–213.
- Zimmermann, P. & Fimm, B. (2016). Test of Attentional Performance Version 2.3. Psytest.
- Zuckerman, H., Pan, Z., Park, C., Brietzke, E., Musial, N., Shariq, A. S., Iacobucci, M., Yim, S. J., Lui, L., Rong, C., & McIntyre, R. S. (2018). Recognition and treatment of cognitive dysfunction in major depressive disorder. Frontiers in psychiatry, 9, 655. https://doi.org/10.3389/fpsyt.2018.00655