Abstract
When patients fail symptom validity tests (SVTs) and/or performance validity tests (PVTs), their self-reported symptoms and test profiles are unreliable and cannot be taken for granted. There are many well-established causes of poor symptom validity and malingering is only of them. Some authors have proposed that a cry for help may underlie poor symptom validity. In this commentary, we argue that cry for help is a (1) metaphorical concept that is (2) difficult to operationalize and, at present, (3) impossible to falsify. We conclude that clinicians or forensic experts should not invoke cry for help as an explanation for poor symptom validity. To encourage conceptual clarity, we propose a tentative framework for explaining poor symptom validity.
Patients present their symptoms in many different ways and sometimes they exaggerate their symptoms and/or their impairments. In such cases, they exhibit problematic (i.e., poor) symptom validity. For the clinician or the forensic expert, detection of poor symptom validity is of pivotal importance. Ignoring poor symptom validity may lead to wrong diagnoses (e.g., diagnosing a patient with epilepsy rather than feigned seizures; e.g., Bass & Jones, Citation2011), with potentially severe adverse effects. Likewise, it may lead to overdiagnoses (e.g., diagnosing a healthy person with mild cognitive impairment; Roor et al., Citation2016). Overlooking poor symptom validity may contribute to harmful treatment interventions (e.g., neuroleptics or prolonged admission to a psychiatric hospital; e.g., van der Heide et al., Citation2020a) or to unjustified prosecution (e.g., the case of a person with factitious disorder who claimed to be a serial killer; Fischer et al., Citation2017). When gone undetected, poor symptom validity may impact society at large (e.g., increased health care costs, undeserved disability benefits; Armistead-Jehle & Green, Citation2016; Onofrj et al., Citation2021).
There is now a considerable corpus of literature (e.g., Sweet et al., Citation2021) documenting that two types of tests may be helpful in the detection of poor symptom validity: self-report symptom validity tests (SVTs) that intend to measure overreporting of symptoms, and performance validity tests (PVTs) that measure underperformance on cognitive tests (Larrabee, Citation2012). In this article, we will use the term symptom validity in its traditional superordinate sense, encompassing both symptom and performance validity.
Suppose that several SVTs and/or PVTs were administered to a patient and that all tests have been validated for the type of problem with which the patient presents (e.g., cognitive problems). What does it mean when the patient fails a sufficient number of these tests? The lege artis conclusion to be drawn from such pattern is that the validity of the patient’s claims and of their test profile cannot be confirmed (Merten & Merckelbach, Citation2013; Miskey et al., Citation2020; Rubenzer, Citation2020). Identifying the sources of this poor symptom validity is a next (and not always necessary) step and requires additional information.
Malingering is one potential explanation of poor symptom validity, but clinicians can only conclude with confidence that symptoms are malingered when there is compelling evidence of (1) a voluntary, intentional act of response distortion; (2) a substantial external incentive underlying this behavior, and (3) the absence of other factors or conditions that might fully account for failure on SVTs/PVTs (Sherman et al., Citation2020). Apart from malingering, there are other well-established antecedents of poor symptom validity, such as careless responding (Merckelbach et al., Citation2019), factitious disorder (Chafetz et al., Citation2020), acute psychotic symptoms (van der Heide et al., Citation2020b), or excuse-making behavior (Dandachi-FitzGerald et al., Citation2020), that are conceptually distinct from malingering and that can be subject to scientific scrutiny. For example, if careless or inattentive responding is hypothesized to be the source of poor symptom validity rather than malingering, one would expect to find that the patient is endorsing bizarre infrequency scale items that have nothing to do with symptoms (e.g., “I cannot remember a time when I talked with someone who wore glasses”; Kim et al., Citation2018). Some authors (e.g., Williams et al., Citation2020; Young, Citation2019) have proposed that a “cry for help” may underlie poor symptom validity. For example, Young (Citation2019) wrote that “the relationship between symptom overreporting and dissociation could be explained by the common denominator of a cry for help (…) Moreover, the cry for help in the assessment and testing context might not be to get psychotherapy, but just to get attention and be heard (rather than dismissed, like usual) in prior assessments and so on” (p. 231). We disagree because, in our opinion, cry for help is (1) a metaphorical descriptor that (2) is not open to independent empirical operationalization and (3) is, at present, not falsifiable.
Cry for help is a metaphor
A cry for help in the sense discussed in this paper refers to behavior that might be interpreted as expressing a need for attention, care, and support. As a concept, cry for help emerges in highly diverse areas of the clinical literature ranging from studies on suicide (e.g., Steer et al., Citation1988) and eating disorders (e.g., Noordenbos et al., Citation1998) to dermatitis artefacta (e.g., Wojewoda et al., Citation2012). Reading through this literature gives one the impression that cry for help is employed as a broad metaphorical description rather than as an explanatory concept. In this broad metaphorical sense, every person who presents symptoms to a clinician cries for help and this might be even true for those who would qualify as malingerers or persons with factitious disorder as illustrated in the following two examples.
Consider, as a first example, refugees who grossly exaggerate symptoms in order to obtain a permit to stay in the host country (e.g., van der Heide & Merckelbach, Citation2016). Technically, this would be malingering. Yet, malingering is what reasonable people may do when they are faced with harsh and adversarial circumstances and there are no alternatives (Rogers, Citation1990). With their traumatic backgrounds and the extensive asylum procedures they are involved in, many refugees find themselves in adversarial circumstances. In such a context, malingering may reflect, metaphorically speaking, a cry for help, although the metaphor itself adds nothing to our understanding of the real problems of these people. Also, the adverse situation itself does not automatically result in a feigned symptom presentation; else, malingered symptomatology would emerge in all persons who are confronted with misery.
Consider, as a second example, factitious behavior. A widely accepted view is that factitious symptom presentations are attempts to seek nurturance and sympathy for being ill (for a detailed discussion, see Boone, Citation2021; Feldman & Yates, Citation2018). In keeping with this, the recently developed Symptom and Disposition Interview (SDI; van Impelen et al., Citation2017), an interview that intends to measure factitious motives, addresses the patient’s willingness to engage in patient-related activities, such as participating in patient support groups or scientific studies and undergoing treatment or diagnostic procedures, even if they are unpleasant or have serious potential side effects. One could easily describe such behaviors as a cry for help, but again this metaphorical term possesses no explanatory depth.
Cry for help lacks well-defined operationalization
Are there any clues in the extant literature suggesting that a cry for help can be upgraded in the direction of a well-defined, clearly delineated concept that can be empirically studied? To explore this, we looked for publications in which researchers have tried to induce a cry for help and to evaluate whether their induction method is, indeed, highly specific and non-redundant with other concepts. The only relevant study that we were able to identify was that of Berry et al. (Citation1996), who examined the effect of a cry-for-help instruction on MMPI-2 parameters. Their participants were instructed as follows (Berry et al., Citation1996, p. 29, paraphrased summary): You have been experiencing difficulties at work and home for some time, with gradually increasing distress. After one year of trying to cope with the problems alone, you seek help at a local mental health care center. However, you learn that the center has a long waiting list, and only severe cases are seen on a priority basis. To determine the severity of the mental health problems, patients are asked to fill in the MMPI-2. You feel that after already battling alone for months, help is needed now. Therefore, you decide to fill in the psychological test in such a way to convince the center that you are a priority case.
Berry et al. (Citation1996) found that this instruction produces similar overreporting on the MMPI-2 as a fake bad response style that one expects to see in, for example, malingerers. Yet, the essential question is whether it is conceptually different from such a fake bad response style. We submit that it is not. In our opinion, the cry-for-help instruction of Berry et al. (Citation1996) alludes to a hidden agenda on the part of the patient (van Egmond & Kummeling, Citation2002): it describes a person who faces work- and family-related problems and considers symptom exaggeration to obtain prioritized access to mental health facilities to deal with these problems. Technically speaking, this intentional exaggeration of symptomatology would amount to feigning. Other researchers have come to a similar conclusion. For example, Rogers et al. (Citation2003) included the Berry et al. (Citation1996) study in their meta-analysis of studies using the MMPI-2 for the detection of malingering.
Furthermore, in an informal, small study conducted on the online platform Qualtrics, we gave the Berry et al. (Citation1996) cry-for-help instruction to 22 colleagues (16 licensed psychologists working in a clinical setting, four in a forensic setting, and two working in both settings) and asked them how they interpreted this instruction. Does it reflect malingering, factitious behavior, feigning, random responding, a cry for help, psychopathology, and/or stress? Respondents could tick several answer options. Participation was anonymously. The most frequently endorsed interpretations were: cry for help (77%), psychopathology (73%), and stress (68%). On average, respondents endorsed 3.5 alternatives (SD = 1.4), which often also included factitious behavior (50%), feigning (36%), and malingering (32%). Only 32% of the respondents exclusively endorsed psychological motives (i.e., a cry for help and/or to emphasize stress symptoms and/or psychopathology). Thus, although the vignette was recognized by most respondents as a cry-for-help instruction, it lacked specificity as professional experts found it hard to distinguish between several alternative motives and intentions.
Another route to clarify the meaning and measurement of cry for help is described by Young (Citation2019), who proposed to measure cry for help with a scale containing six items, such as “The situation is unbearable and is worsening how I feel” and “No one is giving me the help I need or cares, and I’m getting worse because of it,” rated on a four-point Likert scale (0 = never; 3 = very frequent). Does Young’s cry-for-help scale offer a genuinely independent operationalization that is immune to malingering, factitious disorder, and random responding? To explore this, we gave the cry-for-help (CFH) scale to a group of 41 psychology students and 17 licensed clinical psychologists. Obtaining approval for this type of small-scale pilot study was not deemed necessary by the standing ethical committee. Data were collected in accordance with the Helsinki principles. In total, 23 of the participants (15 students; 8 clinicians) were instructed with the cry-for-help vignette of Berry et al. (Citation1996) and 35 (24 students; 9 clinicians) were given a straightforward case vignette previously used in an experimental malingering design (Dandachi-FitzGerald & Merckelbach, Citation2013). With these vignettes in mind, the students and clinicians completed the CFH scale. There was no statistically significant difference in CFH scores between those who had the cry-for-help vignette (M = 10.96, SD = 2.38) and those instructed to follow the malingering design (M = 9.74, SD = 2.41; t(56) = 1.89, p = .064). Admittedly, our sample size was relatively small. However, it achieved a power of .90 (α = .05, one-tailed) to detect a large effect (i.e., Cohen’s d ≥ 0.8), which is arguably needed to be diagnostically relevant in professional practice. Thus, our preliminary results suggest that the CFH scale is not going to be helpful in differentiating between malingering and a cry for help as interpretative options for poor symptom validity.
Cry for help is non-falsifiable
Whether they are explicit advocates of Karl Popper’s (Citation1968) falsification principle or not, most researchers would agree that the explanatory power of a concept depends on the degree to which it can be refuted by observations. For example, an “inferiority complex” has little or no explanatory value, precisely because an expert could construe practically every possible behavior as a manifestation of such complex. The inferiority complex lacks falsifiability and much the same is true for cry for help. According to Young (Citation2019), a cry for help may be conscious or unconscious. The latter implies that peoples’ behavior might be a cry for help without them knowing. One step further, people could deny that their behavior signals a cry for help and an expert could still maintain that a cry for help is the one and only correct interpretation. The burden to articulate a cry-for-help interpretation such that it can be refuted by observations rests on the shoulders of authors who commend this concept to the scientific community.
A tentative framework for explaining poor symptom validity
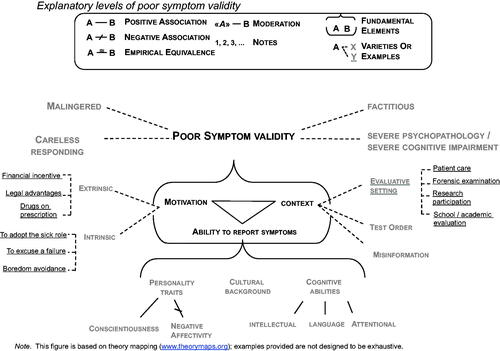
What we need, then, is more conceptual rigor. One way to achieve this is by formulating a theory. Gray (Citation2017) proposed a technique to visually map theories according to specific notation principles. Using this technique, we designed a tentative theory of poor symptom validity (see ). At the same explanatory level, there are different manifestations of poor symptom validity (e.g., malingering). At a deeper explanatory level, there are antecedents of poor symptom validity (i.e., the fundamental elements). Different combinations of fundamental elements lead to different manifestations (i.e., varieties) of poor symptom validity. As can be seen in , we submit that poor symptom validity emerges from the interrelated elements “motivation,” “context,” and “ability to report symptoms.”
Different constellations of these fundamental elements explain variations of poor symptom validity. For example, poor symptom validity of a person, evaluated in a forensic assessment (context) to determine eligibility for disability benefits (extrinsic motivation) might best be explained as malingering (e.g., Sherman et al., Citation2020). Alternatively, consider a student who participates in a psychological study (context) for course credits (extrinsic motivation), and wants to finish the questionnaires as quickly as possible (intrinsic motivation). His or her poor symptom validity is best conceptualized as careless responding (e.g., Bowling et al., Citation2016). A somewhat different constellation is depicted by a third example: Consider a patient with a psychotic disorder, who is admitted to a psychiatric hospital and undergoes neuropsychological assessment (context). There is no clear incentive to exaggerate (no extrinsic motivation). The patient suffers from anhedonia, lack of motivation, lack of interest, emotional numbing, which results in reduced engagement in assessment. In this case, symptom validity test failure can best be understood as resulting from severe psychopathology (fully explains SVT/PVT failure) (e.g., van der Heide et al., Citation2020b). Of note, in this example, SVT failure would qualify for being a true positive (i.e., reflecting an inability to report symptoms on psychological tests due to severe psychopathology, and consequently the validity of the other psychological test data cannot be confirmed). On the other hand, PVT failure would qualify for being false positive, as long as the patient’s test performance was within the limits of his capacities, given the concrete circumstances at the time of the assessment.
Discussion
Is cry for help a useful interpretation of poor symptom validity? We do not think so. We pointed out that this concept is fuzzy and difficult to delineate from malingering and factitious motives, that it lacks well-defined operationalization, and cannot be refuted by observations. In effect, the concept adds confusion rather than clarification. In the older MMPI literature, at a time that patient feigning was not fully recognized, a “plea for help” was coined to describe overreporting of symptoms without a known external incentive (see, for a discussion: Berry et al., Citation1996). However, since then, several studies have shown that patients exhibiting a symptom overreporting profile on the MMPI are extremely prone to noncompliance with therapy and often prematurely discontinue treatment (e.g., Anestis et al., Citation2015; Greene, Citation1988). A lack of treatment adherence has also been identified as a correlate of a failure on PVTs (e.g., Roor et al., Citation2021). Arguably, these findings are difficult, if not impossible, to reconcile with a cry-for-help interpretation. That is, it stretches credulity to argue that patients who are most likely to dropout therapy are the ones who experience a strong need for therapeutic attention. Hence, a cry-for-help explanation has no practical utility. Except, perhaps, that it may serve to alleviate the clinician's cognitive dissonance and discomfort when faced with invalid symptom presentation (Carone et al., Citation2013; Martin & Schroeder, Citation2021). While understandable, using a cry-for-help explanation this way is merely a euphemistic way of describing symptom exaggeration by patients. As stated by Carone et al. (Citation2013, p. 109): “This [cry for help] explanation that has been exalted in mainstream clinical practice, not as a result of research evidence to support its accuracy, but simply because it is proffered in textbooks and computer scoring programs as a benign explanation for this behavior.” In the same vein, Iverson (Citation2006) characterized the cry-for-help concept as a euphemism, and its inappropriate use for explaining away validity test failure as an ethical issue for the clinician or forensic professional.
In our view, the cry-for-help concept flags conceptual confusion. There are other examples of such confusion in symptom validity research. For instance, Henry et al. (Citation2018) suggested that illness perception, specifically the tendency to attribute a high number of symptoms to one’s current illness (i.e., symptom identity), might underlie poor symptom validity. In their study, patients were given PVTs but also a self-report scale measuring symptom identity. A logistic regression analysis with poor symptom validity as criterion and illness perception parameters as predictors showed that illness perception, notably symptom identity, are indeed, statistically speaking, predictors of poor symptom validity. But are these illness perception parameters causal antecedents of poor symptom validity? The Henry et al. (Citation2018) study cannot answer that question because it was cross-sectional in nature. A reversed logistic regression with poor symptom validity as predictor and illness perception parameters as dependent variables would probably show that poor symptom validity is a powerful predictor, statistically speaking, of exaggerated symptom identity. The point here is that illness perception was measured with a self-report instrument of which we do not know whether it is immune to malingering, factitious tendencies, and random/inattentive responding. Sweet et al. (Citation2021) rightly remarked that “self-report measures in the absence of objective SVT data are purely subjective and therefore of unknown reliability and validity” (p. 31). Thus, as long as the validity of a self-report score has not been clarified, it is premature to invoke illness perception, or cry for help for that matter, as a causal antecedent of poor symptom validity.
We do hope that the tentative framework presented above will contribute to conceptual clarity as well as inspire future research. For example, it would be informative to test experimentally whether providing this model to clinicians helps in forming a more balanced judgment of poor symptom validity. Also, future research could examine in a systematic fashion the potential incremental value of combining symptom validity tests with historical data (e.g., the number of hospital visits, invasive medical procedures, prescribed drugs, treatment adherence) so as to better understand the drivers of poor symptom validity. Likewise, specific tests such as the SDI (van Impelen et al., Citation2017) and infrequency items might be useful tools for differentiating between the antecedents of poor symptom validity. The development of a flowchart or decision tree to distinguishing between causal antecedents might be a fruitful next step in further refining the model and increasing its utility in clinical practice.
In sum, given that cry for help is a metaphorical concept, difficult to operationalize, and at present impossible to measure in a well-defined way, it does not contribute to our understanding of poor symptom validity. Therefore, we advise against invoking cry for help as an explanation for poor symptom validity.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Anestis, J. C., Finn, J. A., Gottfried, E., Arbisi, P. A., & Joiner, T. E. (2015). Reading the road signs: The utility of the MMPI-2 Restructured Form Validity Scales in prediction of premature termination. Assessment, 22(3), 279–288. https://doi.org/10.1177/1073191114541672
- Armistead-Jehle, P., & Green, P. (2016). Model for the effects of invalid styles of response. Applied Neuropsychology. Adult, 23(6), 449–458. https://doi.org/10.1080/23279095.2016.1178646
- Bass, C., & Jones, D. (2011). Psychopathology of perpetrators of fabricated or induced illness in children: Case series. The British Journal of Psychiatry, 199(2), 113–118. https://doi.org/10.1192/bjp.bp.109.074088
- Berry, D. T., Adams, J. J., Clark, C. D., Thacker, S. R., Burger, T. L., Wetter, M. W., & Baer, R. A. (1996). Detection of a cry for help on the MMPI-2: An analog investigation. Journal of Personality Assessment, 67(1), 26–36. https://doi.org/10.1207/s15327752jpa6701_2
- Boone, K. B. (2021). Performance validity in somatoform/conversion disorders, factitious disorder, and malingering: Do we need a new diagnostic schema? In K. B. Boone (Ed.), Assessment of feigned cognitive impairment, A neuropsychological perspective (pp. 433–452). The Guilford Press.
- Bowling, N. A., Huang, J. L., Bragg, C. B., Khazon, S., Liu, M., & Blackmore, C. E. (2016). Who cares and who is careless? Insufficient effort responding as a reflection of respondent personality. Journal of Personality and Social Psychology, 111(2), 218–229. https://doi.org/10.1037/pspp0000085
- Carone, D. A., Bush, S. S., & Iverson, G. L. (2013). Providing feedback on symptom validity, mental health, and mild traumatic brain Injury. In D. A. Carone & S. S. Bush (Eds.), Mild traumatic brain injury, symptom validity assessment and malingering (pp. 101–118). Springer.
- Chafetz, M. D., Bauer, R. M., & Haley, P. S. (2020). The other face of illness-deception: Diagnostic criteria for factitious disorder with proposed standards for clinical practice and research. The Clinical Neuropsychologist, 34(3), 454–476. https://doi.org/10.1080/13854046.2019.1663265
- Dandachi-FitzGerald, B., & Merckelbach, H. (2013). Feigning ≠ feigning a memory deficit: The Medical Symptom Validity Test as an example. Journal of Experimental Psychopathology, 4(1), 46–63. https://doi.org/10.5127/jep.025511
- Dandachi-FitzGerald, B., Merckelbach, H., Bošković, I., & Jelicic, M. (2020). Do you know people who feign? Proxy respondents about feigned symptoms. Psychological Injury and Law, 13(3), 225–234. https://doi.org/10.1007/s12207-020-09387-6
- Feldman, M., & Yates, G. (2018). Dying to be ill: True stories of medical deception. Routledge.
- Fischer, C. A., Beckson, M., & Dietz, P. (2017). Factitious disorder in a patient claiming to be a sexually sadistic serial killer. Journal of Forensic Sciences, 62(3), 822–826. https://doi.org/10.1111/1556-4029.13340
- Gray, K. (2017). How to map theory: Reliable methods are fruitless without rigorous theory. Perspectives on Psychological Science, 12(5), 731–741. https://doi.org/10.1177/1745691617691949
- Greene, R. L. (1988). The relative efficacy of F-K and the obvious and subtle scales to detect overreporting of psychopathology on the MMPI. Journal of Clinical Psychology, 44(2), 152–159. https://doi.org/10.1002/1097-4679(198803)44:2<152::AID-JCLP2270440210>3.0.CO;2-U
- Henry, G. K., Heilbronner, R. L., Suhr, J., Gornbein, J., Wagner, E., & Drane, D. L. (2018). Illness perceptions predict cognitive performance validity. Journal of the International Neuropsychological Society, 24(7), 735–745. https://doi.org/10.1017/S1355617718000218
- Iverson, G. L. (2006). Ethical issues associated with the assessment of exaggeration, poor effort, and malingering. Applied Neuropsychology, 13(2), 77–90. https://doi.org/10.1207/s15324826an1302_3
- Kim, D. S., McCabe, C. J., Yamasaki, B. L., Louie, K. A., & King, K. M. (2018). Detecting random responders with infrequency scales using an error-balancing threshold. Behavior Research Methods, 50(5), 1960–1970. https://doi.org/10.3758/s13428-017-0964-9
- Larrabee, G. (2012). Performance validity and symptom validity in neuropsychological assessment. Journal of the International Neuropsychological Society, 18(4), 625–630. https://doi.org/10.1017/s1355617712000240
- Martin, P. K., & Schroeder, R. W. (2021). Feedback with patients who produce invalid testing: Professional values and reported practices. The Clinical Neuropsychologist, 35(6), 1134–1153. https://doi.org/10.1080/13854046.2020.1722243
- Merckelbach, H., Dandachi-FitzGerald, B., van Helvoort, D., Jelicic, M., & Otgaar, H. (2019). When patients overreport symptoms: More than just malingering. Current Directions in Psychological Science, 28(3), 321–326. https://doi.org/10.1177/0963721419837681
- Merten, T., & Merckelbach, H. (2013). Symptom validity testing in somatoform and dissociative disorders: A critical review. Psychological Injury and Law, 6(2), 122–137. https://doi.org/10.1007/s12207-013-9155-x
- Miskey, H. M., Martindale, S. L., Shura, R. D., & Taber, K. H. (2020). Distress tolerance and symptom severity as mediators of symptom validity failure in veterans with PTSD. The Journal of Neuropsychiatry and Clinical Neurosciences, 32(2), 161–167. https://doi.org/10.1176/appi.neuropsych.17110340
- Noordenbos, G., Jacobs, M. E., & Hertzberger, E. (1998). Chronic eating disorders: The patients’ view of their treatment history. Eating Disorders, 6(3), 217–223. https://doi.org/10.1080/10640269808249256
- Onofrj, M., Digiovanni, A., Ajdinaj, P., Russo, M., Carrarini, C., Di Giannantonio, M., Martinotti, G., & Sensi, S. L. (2021). The factitious/malingering continuum and its burden on public health costs: A review and experience in an Italian neurology setting. Neurological Sciences, 42(10), 4073–4083. https://doi.org/10.1007/s10072-021-05422-9
- Popper, K. R. (1968). The logic of scientific discovery. Columbia University Press.
- Rogers, R. (1990). Models of feigned mental illness. Professional Psychology: Research and Practice, 21(3), 182–188. https://doi.org/10.1037/0735-7028.21.3.182
- Rogers, R., Sewell, K. W., Martin, M. A., & Vitacco, M. J. (2003). Detection of feigned mental disorders: A meta-analysis of the MMPI-2 and malingering. Assessment, 10(2), 160–177. https://doi.org/10.1177/1073191103010002007
- Roor, J. J., Dandachi-FitzGerald, B., Peters, M. J. V., Knoop, H., & Ponds, R. W. H. M. (2021). Performance validity and outcome of cognitive behavior therapy in patients with chronic fatigue syndrome. Journal of the International Neuropsychological Society, 2021, 1–10. https://doi.org/10.1017/S1355617721000643
- Roor, J. J., Dandachi-FitzGerald, B., & Ponds, R. W. H. M. (2016). A case of misdiagnosis of mild cognitive impairment: The utility of symptom validity testing in an outpatient memory clinic. Applied Neuropsychology: Adult, 23(3), 172–178. https://doi.org/10.1080/23279095.2015.1030018
- Rubenzer, S. (2020). The case for assessing for negative response bias, not malingering. Journal of Forensic Psychology Research and Practice, 20(4), 323–340. https://doi.org/10.1080/24732850.2020.1732767
- Sherman, E. M. S., Slick, D. J., & Iverson, G. L. (2020). Multidimensional malingering criteria for neuropsychological assessment: A 20-year update of the malingered neuropsychological dysfunction criteria. Archives of Clinical , 35(6), 735–764. https://doi.org/10.1093/arclin/acaa019
- Steer, R. A., Beck, A. T., Garrison, B., & Lester, D. (1988). Eventual suicide in interrupted and uninterrupted attempters: A challenge to the cry-for-help hypothesis Suicide & Life-Threatening Behavior, 18(2), 119–128. https://doi.org/10.1111/j.1943-278x.1988.tb00146.x
- Sweet, J. J., Heilbronner, R. L., Morgan, J. E., Larrabee, G. J., Rohling, M. L., Boone, K. B., Kirkwood, M. W., Schroeder, R. W., & Suhr, J. A. (2021). American Academy of Clinical Neuropsychology (AACN) 2021 consensus statement on validity assessment: Update of the 2009 AACN consensus conference statement on neuropsychological assessment of effort, response bias, and malingering. The Clinical Neuropsychologist, 35(6), 1053–1106. https://doi.org/10.1080/13854046.2021.1896036
- van der Heide, D., Boskovic, I., van Harten, P., & Merckelbach, H. (2020a). Overlooking feigning behavior may result in potential harmful treatment interventions: Two case reports of undetected malingering. Journal of Forensic Sciences, 65(4), 1371–1375. https://doi.org/10.1111/1556-4029.14320
- van der Heide, D., Boskovic, I., van Harten, P., & Merckelbach, H. (2020b). Psychosis as a confounder of symptom credibility testing in a transcultural sample. The Journal of Forensic Psychiatry & Psychology, 31(1), 64–75. https://doi.org/10.1080/14789949.2019.1663899
- van der Heide, D., & Merckelbach, H. (2016). Validity of symptom reports of asylum seekers in a psychiatric hospital: A descriptive study. International Journal of Law and Psychiatry, 49(Pt A), 40–46. https://doi.org/10.1016/j.ijlp.2016.05.007
- van Egmond, J. J., & Kummeling, I. (2002). A blind spot for secondary gain affecting treatment outcome. European Psychiatry, 17(1), 46–54. https://doi.org/10.1016/S0924-9338(02)00622-3
- van Impelen, A., Merckelbach, H., Jelicic, M., Niesten, I. J., & À Campo, J. (2017). Differentiating factitious from malingered symptomatology: The development of a psychometric approach. Psychological Injury and Law, 10(4), 341–357. https://doi.org/10.1007/s12207-017-9301-y
- Williams, M. W., Graham, D., Sciarrino, N. A., Estey, M., McCurry, K. L., Chiu, P., & King-Casas, B. (2020). Does validity measure response affect CPT group outcomes in veterans with PTSD? Military Medicine, 185(3–4), e370–e376. https://doi.org/10.1093/milmed/usz385
- Wojewoda, K., Brenner, J., Kąkol, M., Naesström, M., Cubała, W. J., Kozicka, D., Nowicki, R., Sokołowska-Wojdyło, M., & Barańska-Rybak, W. (2012). A cry for help, do not omit the signs. Dermatitis artefacta–psychiatric problems in dermatological diseases (a review of 5 cases). Medical Science Monitor, 18(10), CS85–89. https://doi.org/10.12659/MSM.883474
- Young, G. (2019). The cry for help in psychological injury and law: Concepts and review. Psychological Injury and Law, 12(3–4), 225–237. https://doi.org/10.1007/s12207-019-09360-y