Abstract
Cognitive deficits are common after brain injury and can be measured in various ways. Many neuropsychological tests are designed to measure specific cognitive deficits, and self-report questionnaires capture cognitive complaints. Measuring cognition in daily life is important in rehabilitating the abilities required to undertake daily life activities and participate in society. However, assessment of cognition in daily life is often performed in a non-standardized manner. In this opinion paper we discuss the various types of assessment of cognitive functioning and their associated instruments. Drawing on existing literature and evidence from experts in the field, we propose a framework that includes seven dimensions of cognition measurement, reflecting a continuum ranging from controlled test situations through to measurement of cognition in daily life environments. We recommend multidimensional measurement of cognitive functioning in different categories of the continuum for the purpose of diagnostics, evaluation of cognitive rehabilitation treatment, and assessing capacity after brain injury.
Introduction
Many people experience cognitive problems as a result of neurodevelopmental conditions, mental health problems, after acquired brain injury (ABI), or as a result of degenerative brain conditions. These cognitive problems negatively affect patients’ independence and their quality of life (Cumming et al., Citation2014; Heruti et al., Citation2002). Assessment of cognition is undertaken for many reasons, such as diagnosing neurological conditions and assessing the impact of the brain condition on cognitive functions. Moreover, identifying the associated consequences of cognitive impairment for everyday life can inform predictions about the ability to live independently (Maruish, Citation2004). These contexts for assessment reflect the different components of the model that underlies the WHO International Classification of Functioning, Disability and Health (ICF) (World Health Organization, Citation2001). In this model, human functioning is classified by the components ‘body structures and functions,’ ‘activities’, and ‘participation’, while taking into account the influence of personal and environmental factors. When applied to cognitive functioning after brain damage, a distinction can be made between measurement at the body function level (e.g., measuring cognitive impairment), at the level of activities (e.g., measuring the impact of cognitive impairment on the performance of specific activities in daily life) and at the level of participation (e.g., measuring the impact of cognitive impairment on participating in wider valued societal roles). This distinction illustrates that the consequences of a condition (such as a brain injury) are manifested at different levels of functioning, and that the ultimate impact of the condition is influenced by factors other than those directly related to the condition. Moreover, the model shows that there are different levels at which human (and therefore cognitive) functioning can be classified and that these levels are related to each other. The latter is illustrated by the fact that measures of cognitive impairment, among other factors, can predict whether a person will successfully return to work after a stroke (van der Kemp et al., Citation2019). Personal and external factors interact with (cognitive) functioning and influence overall quality of life (Goretti et al., Citation2010).
Cognitive functioning and its impact on daily life functioning and participation is complex and multidimensional. In this paper, we characterize the different types of existing measurement instruments for cognitive functioning, thereby illustrating the differences between the assessment of cognitive functions in lab-based test settings and in real-world environments. A particular focus is placed on measuring cognition in daily life, which can be defined as the cognitive component of spontaneous behavior and addresses cognitive functioning, rather than the performance on a specific task (i.e., functional ability).
Literature review and expert meetings
This opinion paper is informed by a narrative review of the literature and two national expert meetings with colleagues working in this area. These meetings were organized to further explore the different types of cognition measurement, to classify the available measures, and to identify their perceptions of the most suitable approach to measuring cognition in daily life. Participants of the expert group (n = 13, 77% female) were purposively selected based on their involvement in the development of measurement instruments for cognition and on the basis of being active as researchers and/or healthcare professionals (rehabilitation physician, psychologist, occupational therapist, nurse, or physician for social insurance) in various sectors of health care (hospital care, rehabilitation care, or elderly care) (Supplementary Appendix 1). The following sections describe the methods of measuring cognition that resulted from the literature review and expert meetings.
Neuropsychological assessment
Cognitive functioning is measured by means of a comprehensive neuropsychological assessment (NPA). A NPA typically consists of tests, observations during test administration, and detailed history from referral information, medical records, as well as from the patient and relative(s) on the basis of interviews and questionnaires. The primary aim of neuropsychological assessment is to reveal any impairments in cognitive domains or subdomains. To this end, a profile of a patient’s cognitive strengths and weaknesses is established by combining test results with contextual sources of information. This profile indicates areas of impairment and cognitive domains in which the performance is consistent with norm-referenced performance, corrected for demographic influences such as gender, age and education level as appropriate.
Neuropsychological tests
A central component of NPAs is valid and reliable neuropsychological tests, or cognitive tests, which are typically aimed at specific cognitive domains (Lezak et al., Citation2012). Ideally, such tests are administered in a controlled environment (e.g. free of distractions such as noise) to facilitate optimal comparison with normative sample data (Bouma et al., Citation2012). Given that neuropsychological tests are aimed at measuring cognitive impairments in a controlled environment, they take little to no account of the positive and negative influence of personal or environmental factors on performance that would be present in the real world, outside of a test situation. Furthermore, the results of neuropsychological tests do not necessarily reflect everyday activity performance (Chevignard et al., Citation2000), as some patients may effectively use (external) compensatory strategies that reduce the impact of cognitive deficits on performance of everyday activities. Such compensatory strategies (i.e. taking notes to compensate for memory problems) are typically not permitted during testing.
The limited generalization of neuropsychological test results may be especially relevant in the context of evaluating cognitive rehabilitation interventions. Cognitive rehabilitation includes interventions targeting specific cognitive impairments, but the evidence to date suggests that impaired cognitive functions cannot typically be restored to normal, though everyday functioning may be improved by impairment-focused cognitive strategies. Cognitive rehabilitation programs are often based on the results of neuropsychological assessment (Tsaousides & Gordon, Citation2009), and are generally aimed at improving the patient's independence through psychoeducation, environmental adaptation and cognitive (strategy) training (Sohlberg & Mateer, Citation2017). This way, patients learn to cope with the limitations cognitive impairments impose in daily life albeit not necessarily reducing the cognitive impairments. Whilst cognitive rehabilitation is considered to be effective (Cicerone et al., Citation2019), the specific effects, or outcomes, are measured in many different ways and on many different levels of the ICF framework (van Heugten et al., Citation2020). Since the goals of cognitive rehabilitation are most commonly at the activity level and given the fact that neuropsychological tests typically measure on a body functions level (impairment), improvement on these tests as a result of cognitive rehabilitation is not to be expected. Adding to this is the risk of measuring task-specific practice effects instead of improvement in cognitive function (Calamia et al., Citation2012). Neuropsychological tests are therefore usually unsuitable for measuring treatment effects and therefore, NPAs can be supplemented with other measurement instruments that differ from classical neuropsychological tests.
Ecologically valid tests of cognitive functioning
In response to the low generalizability of neuropsychological test results to daily life, ‘ecologically valid’ tests were developed to supplement classical neuropsychological tests as part of a neuropsychological assessment. Ecological validity refers to the extent to which the results obtained in a controlled environment correspond to performance in a naturalistic setting. Such tests are still aimed at measuring impairments in a specific cognitive domain, but typically measure these by means of tasks with a greater similarity to daily life. Generally, two approaches to establishing ecological validity of neuropsychological tests have been described, referred to as verisimilitude and veridicality (Chaytor & Schmitter-Edgecombe, Citation2003). Verisimilitude refers to the extent to which the test relies on cognitive functions corresponding to the cognitive load of an actual situation and is often associated with high degrees of face validity, as the tasks resemble tasks of daily life. Veridicality, on the other hand, is a measure of the extent to which the results of a test (which may not necessarily resemble an everyday activity) correlate with the level of functioning in daily life (such as employment status), and could therefore be the best estimation of a patient’s ability to function in daily life without actually observing a patient in their natural environment. However, most neuropsychological tests show only modest correlations with daily life functioning (Fortin et al., Citation2003), and these estimations are to a large extent dependent of the indicator of daily functioning that is being used (Chaytor & Schmitter-Edgecombe, Citation2003). Thus, despite the fact that results of tests with increased ecological validity better approximate the patients’ everyday functioning, large discrepancies often remain between test results and functioning in daily life. This might be explained by the fact that daily life is more complex than structured tests focusing on a single domain of cognition, meaning that almost all tasks in everyday life utilize multiple cognitive functions and could therefore be impaired as a result of deficits in one of many cognitive functions.
Besides measuring cognitive impairment through neuropsychological tests, cognitive functioning can be evaluated in terms of ‘functional cognition’, defined as “the ability to use and integrate thinking and performance skills to accomplish complex everyday activities” (Giles et al., Citation2017). As functional cognition instruments involve the performance of complex tasks that are dependent of cognition, they often rely on the integration of multiple bits of information over an extended period of time and therefore may be particularly useful in assessing executive functioning, or cognitive control, compared to more traditional table-top or lab tests (Poncet et al., Citation2017). Functional cognition can be evaluated through informal but consistent use of a practical task as part of rehabilitation care (e.g., asking all patients to prepare the same meal), or by means of standardized, semi-controlled tasks such as those in the Assessment of Motor and Process skills (AMPS (Pan & Fisher, Citation1994)), or uncontrolled tasks assessed as part of the ADL and IADL Profile (Bottari et al., Citation2009; Citation2020). This method of testing, also known as performance-based measurement, is often used by occupational therapists to determine the degree of a patient’s independence and can serve as a risk assessment when patients return home after admission to the hospital or rehabilitation center (Giles et al., Citation2017), providing an invaluable element of assessment in rehabilitation care. As the observation of cognitive functioning is based on a meaningful task, functional cognition tasks can be used to estimate daily functioning, (Skidmore, Citation2017), although their predictive validity has not been studied widely (Casaletto & Heaton, Citation2017). Nonetheless, these assessments are often still carried out in a standardized environment, such as an institution or the practice of the care provider, or using an artificial task.
Questionnaires measuring cognitive complaints
Another method for measuring cognitive functioning is with questionnaires focusing on subjective cognitive impairment, or questionnaires focusing on the subjective impact of cognitive impairment on daily life, sometimes referred to as patient-reported outcome measures (PROMS). The importance of patient perspectives is increasingly recognized (Black, Citation2013). One limitation of self-reported measurement instruments is that not all patients are capable of completing these, for example due to severe cognitive impairment, communication problems, or limited awareness of or insight in their disease and degree of functioning (Bach & David, Citation2006), the latter potentially resulting in under-reporting of problems. In the case of incapacity to self-report, proxy-reporting by an informal caregiver or healthcare professional is sometimes employed as an alternative. Research has shown important discrepancies between self and proxy reporting in the case of cognitive functioning, and indicates that proxy reporting often correlates higher with cognitive test performance (Howland et al., Citation2017). Self-reporting can result in over-reporting of complaints, as presenting a patient with examples of difficulties can lead to an affirmative response bias, compared with spontaneous complaint reporting (Nolin et al., Citation2006). There may also be over-reporting due to an external motive, such as financial compensation (Bianchini et al., Citation2006), and the results of self-reported questionnaires are often influenced by personal factors (Nijsse et al., Citation2017).
In summary, cognition can be measured in a variety of ways, which can all contribute to an understanding of a patient’s functioning after a brain condition. Measuring cognitive impairment by means of neuropsychological tests is essential for diagnostic purposes, but does not tell the full story, as performance in an artificial environment provides incomplete insight into cognitive functioning in daily life. Furthermore, measuring cognitive limitations when performing assigned tasks may reflect performance in real life situations, but may not fully correspond to functioning in a patient’s own habitat. Moreover, questionnaires focusing on subjective cognitive impairment can be biased as a result of the consequences of brain damage, and are influenced by environmental and personal factors. In addition, situational factors, such as the unusual environment of a hospital admission, can influence a patient’s ability to perform tests, carry out assignments or complete questionnaires.
Measuring cognition in daily life
One missing piece of the puzzle of understanding the impact of cognitive impairments is the evaluation of cognition in actual everyday life situations. In the case of diagnosing the severity of cognitive problems after ABI or dementia, understanding the impact of the cognitive problems on daily life situations is already part of most NPAs. However, it often remains based on unstructured observations, is aggregated out of multiple sources of information (Bootes & Chapparo, Citation2002), or is estimated by means of instruments measuring Instrumental Activities of Daily Living. Although IADL performance is related to cognitive impairment (Dodge et al., Citation2005), it can be heavily influenced by other factors, such as physical impairment (Cromwell et al., Citation2003).
In treatment settings, such as cognitive rehabilitation, the focus of the interdisciplinary team is often on understanding 1) whether cognitive impairments are present, 2) the nature of any cognitive impairment, and 3) how they impact functioning in daily life. Therefore, it is important to use instruments that measure the cognitive component of spontaneous behavior in daily life when designing and evaluating treatment interventions.
Spontaneous behavior is defined here as behavior that has not been commanded and which can be observed over a longer period as compared to assignments in artificial environments, such as standardized tests. Spontaneous behavior can be observed in a clinical situation (such as a hospital ward or rehabilitation facility), as well as in residential facilities and in people's homes, community or work places, by healthcare professionals or informal caregivers. The behavior takes place in a naturalistic environment, meaning that there are no specific environmental constraints that limit normal behavioral functioning. The cognitive component of these spontaneous behaviors can be referred to as ‘cognition in daily life’, is organized according to cognitive functions, and reflects the level of cognitive functioning rather than the level of performance on a specific task. For example, cognition in daily life reflects the extent to which a patient continues a task when he/she is interrupted by a ringing phone (attention), able to remember the recipe (memory), and able to complete steps in a logical order (executive functioning), rather than how well this patient is able to prepare a meal. Instruments for measuring cognition in daily life could be employed to measure change in the impact of cognitive impairment on daily life, and could therefore be a valuable asset in both clinical practice and scientific research.
As the performance of complex tasks is heavily dependent on the context they are performed in, the observation of a particular cognitive function needs to be based on the expression of cognitive abilities during a variety of daily tasks over a prolonged observation period. Consequently, measurement of cognition in daily life needs to be performed by clinicians who have spent sufficient time to allow for thorough observation, such as nurses, which may be challenging in some clinical services.
Since cognition in daily life concerns behavior in a natural context, it reflects cognitive functioning while allowing for the use of compensatory strategies. This means that deficits in cognition may be apparent from errors in task performance, but successful task performance does not mean that no cognitive impairment is present. Furthermore, observation in daily life depends on the skills of an observer and is therefore prone to bias. As a result, interpreting measures of cognition in daily life should occur in conjunction with results from other sources, such as neuropsychological tests. Like any other instrument for measuring cognition, outcomes need to be interpreted alongside information on other factors that influence functioning, such as fatigue, which can provide further context in understanding cognitive problems.
A continuum of cognitive functioning measurement
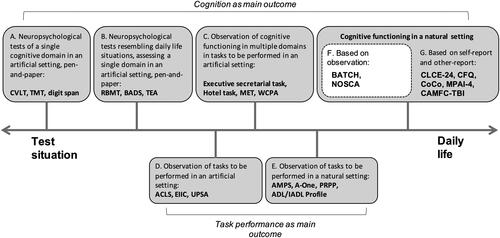
Over the course of two expert meetings, a continuum of different ways of measuring cognitive functioning was formulated and is presented in . The expert group concluded that the various ways of assessing cognitive functioning range from, on the one hand, the isolated, highly controlled measurement of specific cognitive domains in test situations, to, on the other hand, real-life cognition, either as reported by a proxy, or as experienced by the patient. A detailed description of each of the categories, the associated measurement instruments, and their characteristics is provided in Supplementary Appendix 2.
Figure 1. Continuum of instruments for measuring cognitive functioning. Based on the continuum as presented in NOSCA development and validation of the nurses’ observation scale for cognitive abilities (thesis) by A. Persoon, 2010, p114 (Persoon et al., Citation2011).
An exploration of measurement instruments for cognition in daily life
Cognition in daily life reflects the cognitive component of spontaneous behavior and addresses cognitive functioning, rather than the performance on a specific task. Therefore, category F measurement instruments arguably are the most appropriate for measuring cognition in daily life. Generally, these instruments contain descriptions of observable behaviors that are organized into a set of cognitive domains. Healthcare professionals observe patients over an extended period of time (usually several days) and identify behaviors that reflect strengths or weaknesses in each domain of cognition. We aimed to identify existing measurement instruments for cognition in daily life which met the following criteria: 1) the instrument measures cognitive functioning in a natural setting, 2) the instrument focuses on the observation of spontaneous behavior, 3) the instrument has cognitive functioning as its main outcome, and 4) the instrument covers multiple cognitive domains. To the best of our knowledge, four instruments met these criteria. and summarize the properties and content of these measures.
Table 1. Measurement instrument properties.
Table 2. Measurement instrument composition.
The Behavioral Assessment Tool of Cognition and Higher function (BATCH) (Miller et al., Citation2007) is a measurement instrument for observing multiple cognitive functions. The BATCH is a clinician-rated tool composed of 60 items, divided over ten domains. The examiner rates the patient on five to eight behaviors within each domain. Performance is scored on a five-point Likert scale classifying the frequency of each behavior (e.g., ‘patient remains alert during the day’, 1: never − 5: always). The BATCH has only been validated for patients with neuropsychiatric disorders. It showed very high internal consistency. Construct validity was also very high when subdomains of the BATCH were correlated with NUCOG subdomains. The BATCH also showed very high concurrent validity when total scores were correlated with total NUCOG and MMSE scores in a sample of neuropsychiatry inpatients (n = 76). Furthermore all subscales correlated strongly with associated subscales of the NUCOG (Miller et al., Citation2007), but no information on divergent validity is available, meaning that these subscale relationships might not be specific to the associated cognitive domain. The Hoensbroeckse Disability Scale for Brain Injury (HDSB) (Torenbeek et al., Citation1998) is a clinician-rated measurement instrument for the observation of functioning which features a separate subscale for cognition, composed of 13 items. Each cognitive skill is described by a single item and rated along a four-point scale describing behavior associated with the score for that particular skill. For example, the item ‘knowing people’s names’ can be scored a 0: he/she knows nobody’s name, except for those of his/her parents or partner’. The HBSH has only been validated in a small sample (n = 33) of rehabilitation patients with brain injuries. The sample size was insufficient to reliably evaluate responsiveness of the measure. No seperate indices for concurrent or divergent validity were provided for the cognition items. The Nurses' Observation Scale of Cognitive Abilities (NOSCA) (Persoon et al., Citation2011) is a nurse-rated observation scale covering nine cognitive domains. Each domain contains a number of sample behaviors that are rated on a four-point Likert scale reporting frequency. One score is attributed to each item within every domain. For example, the domain ‘memory’ consists of six items such as ‘the patient can remember appointments made today or yesterday’ (0: never − 4: repeatedly). The NOSCA has been developed and validated for elderly patients admitted to geriatric wards. In a validation study among this population (n = 50), the total scale showed excellent reliability and satisfactory validity. Convergent validity of the subscales against measures of cognition (NOSGER and MMSE) or dementia severity (Clinical Dementia Rating) ranged from poor to fair, meaning that it is unclear whether the NOSCA is able to discriminate between cognitive domains. Divergent validity with depressive symptoms was confirmed. The Utrecht Scale for Evaluation of Rehabilitation (USER) (Post et al., Citation2009) is an instrument to measure the outcomes of clinical rehabilitation and features a concise subscale for the observation of cognition, covering five domains. A single score is attributed to each domain, reflecting independence in activities relying on the particular cognitive function (e.g. needs assistance to understand verbal and non-verbal information, visually or in writing). In a sample of rehabilitation inpatients (n = 60), the USER cognition subscale demonstrated excellent inter-rater reliability and internal consistency. The USER cognitive functioning score was skewed, but it did not show any floor or ceiling effects. Concurrent validity of total scores against measures of general functioning (Functional Independence Measure and Barthel Index) were strong. No separate information on concurrent or divergent validity was available for the cognition subscale. Responsiveness of the cognition subsale was insufficient.
There are important differences with respect to the comprehensiveness of the instruments. Some measures, such as the USER, were developed for screening purposes and therefore less informative when it comes to detailed information about cognition in daily life. Observers give scores per cognitive domain (instead of items within these domains) and therefore, these measures provide a global estimation of the concerning domain. They heavily rely on the knowledge of the healthcare professional regarding the domain, or depend on the use of a manual describing the typical behaviors that characterize a certain level of functioning within a cognitive domain. Notably, there is inconcistency in the domains that are assessed between the selected measurement instruments. The apparent interrelatedness of different cognitive domains and the need to examine single domains in light of other domains has been acknowledged previously (Harvey, Citation2019), however, no consensus exists on the subdomains of which cognitive functioning is comprised.
In short, we lack widely available, well-validated, and applicable standardized measurement instruments for the measurement of cognition in daily life. Therefore, observation of spontaneous behavior is often performed in an unstructured way. Measurement of cognition in daily life could be used in addition to traditional neuropsychological tests, functional cognition tasks, and questionnaires. In doing so, it may be possible to more accurately measure cognitive functions, which will facilitate the prediction of how a person will perform in everyday functional tasks. If we want to predict whether someone will be able to return to their job, we can draw on traditional tests (e.g. a word learning test) but also our understanding of cognitive strengths and weaknesses evident in other functional tasks (e.g. shopping). If we identify cognitive strengths and weaknesses as they are reflected in functional tasks, then we can make predictions about performance of many other everyday tasks and activities. Moreover, as instruments for cognition in daily life rely on clinician or informal caregiver observation, they can be used when assessment using other instruments is unfavorable or impossible.
Recommendations for healthcare professionals and future research
The expert group emphasized the importance of multidimensional measurement of cognition. Ideally, cognitive functioning is measured by means of a NPA that measures at impairment and activity as well as participation levels for accurate diagnostics and prognostics. Furthermore, the level of performance on tasks of (instrumental) activities of daily living needs to be assessed in order to evaluate the impact of cognitive functioning on safe and independent living. In diagnostic settings, measuring cognition on a broader level than impairment level can shed light on cognitive problems that do not (yet) show on cognitive tests, or provide insight into already acquired compensation strategies. In the case of dementia, the interference of cognitive problems with daily life is even one of the diagnostic criteria (McKhann et al., Citation2011), demonstrating the need for standardized observation of this relationship. In the case of evaluating the effectiveness of cognitive rehabilitation treatment, cognition in daily life might be the most important outcome. As improvement at an impairment level is often not expected, we hypothesize that changes in functioning after cognitive rehabilitation might best be captured by assessing the ability to manage the cognitive demands that are associated with everyday tasks. Moreover, evaluating participation levels as treatment outcomes might be too ‘distant’ from the proximal treatment effect, as participation can be influenced by a multitude of other factors, such as life events or personal factors (Anaby et al., Citation2009; Boosman et al., Citation2017). When patients efficiently apply skills and strategies to compensate for any cognitive impairment, there will be fewer cognitive problems during everyday tasks. This lessened impact of cognitive impairment on daily life reflects the ultimate goal of cognitive rehabilitation, and may therefore be the most sensitive outcome for measuring change after interventions (Cicerone, Citation2005). In the context of assessing capacity to return home or to work, multidimensional measurement of cognition allows linking of impairments at one end of the continuum to cognitive complaints at the other end, thereby ensuring the ultimate impact of the cognitive problems is taken into account. To better understand the impact of cognition in daily life, clinicians from various disciplines need to join forces and combine their expertise to meet the complex needs of these patients.
With respect to measuring cognition in daily life, four measurement instruments were identified. A comprehensive measurement instrument with evidence of applicability to all settings and patient groups that encounter cognitive problems currently does not seem to exist. Future research could focus on continuing the search for a comprehensive and universal measurement instrument, perhaps initially by means of a systematic review. Furthermore, the exploration of expert opinions could be expanded to capture perspectives from a larger number of experts in a wide range of healthcare disciplines. Alternatively, researchers could focus on the translation, further development, or wider validation of an existing tool such as the BATCH (Miller et al., Citation2007) or NOSCA (Persoon et al., Citation2011). Further, the development of a new measurement instrument could be considered. A novel instrument could be developed based on step-wise assessment methods, such as Computerized Adaptive Testing. These methods allow for measurement of cognitive problems that range from very light to very severe, thereby involving items for the observation of behavior outside an inpatient facility. An example of this technique was applied in the development of the CAMFC-TBI (category G) (Donovan et al., Citation2011). In order to improve multidisciplinary communication, this measurement instrument would ideally adopt cognitive subdomains as used in NPA and be used alongside other measurement techniques. In order to obtain a complete and nuanced image of these cognitive domains, the domains should be evaluated using multiple items per domain, which differentiate between the absence of a problem and not having observed the specific behavior. In addition, the application of instruments for observing cognition in daily life should be investigated outside the clinical setting, for example when an informal caregiver is responsible for the observation of behavior. Although there still is little evidence on the usefulness of measuring cognition using ecological momentary assessment (Verhagen et al., Citation2019), the application of these techniques for measuring cognition in real-world settings can be further explored in the future.
Conclusion
We identified seven categories of instruments for measuring cognition that can be visualized on a continuum. The continuum ranges from the measurement of specific cognitive domains and associated impairment in controlled testing environments to cognitive functioning as experienced by the patient in their everyday life. These categories reflect cognitive functioning on different levels of functioning (functions, activities, participation). In light of the goals of current practice, measuring cognition in daily life can be considered an important addition to the range of approaches to measuring cognition. Four existing measurement instruments that fall within this category were identified, but these were developed for screening purposes, or for specific patient populations. A validated and widely applicable measurement instrument should become available to enrich diagnostic practice, shape and evaluate cognitive rehabilitation therapy more accurately, and assist the estimation of capacity to return home or to work. In rehabilitation contexts, interdisciplinary expertise on the impact of cognitive functioning (and dysfunction) on daily life activities needs to be combined to improve clinical decision making and improve care for people with cognitive problems.
Supplementary_Appendix_2
Download MS Word (16.7 KB)Supplementary Appendix_1.docx
Download MS Word (15.5 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Anaby, D., Miller, W. C., Eng, J. J., Jarus, T., Noreau, L., & Group, P. R, PACC Research Group (2009). Can personal and environmental factors explain participation of older adults? Disability and Rehabilitation, 31(15), 1275–1282.
- Bach, L. J., & David, A. S. (2006). Self-awareness after acquired and traumatic brain injury. Neuropsychological Rehabilitation, 16(4), 397–414.
- Bianchini, K. J., Curtis, K. L., & Greve, K. W. (2006). Compensation and malingering in traumatic brain injury: A dose-response relationship? The Clinical Neuropsychologist, 20(4), 831–847.
- Black, N. (2013). Patient reported outcome measures could help transform healthcare. BMJ, 346, f167. https://doi.org/10.1136/bmj.f167
- Boosman, H., Winkens, I., van Heugten, C. M., Rasquin, S. M., Heijnen, V. A., & Visser-Meily, J. M. (2017). Predictors of health-related quality of life and participation after brain injury rehabilitation: The role of neuropsychological factors. Neuropsychological Rehabilitation, 27(4), 581–598. https://doi.org/10.1080/09602011.2015.1113996
- Bootes, K., & Chapparo, C. J. (2002). Cognitive and behavioural assessment of people with traumatic brain injury in the work place: occupational therapists' perceptions. Work, 19(3), 255–268.
- Bottari, C., Dassa, C., Rainville, C., & Dutil, É. (2009). The criterion-related validity of the IADL Profile with measures of executive functions, indices of trauma severity and sociodemographic characteristics. Brain Injury, 23(4), 322–335.
- Bottari, C., Dutil, É., Auger, C., & Lamoureux, J. (2020). Structural validity and internal consistency of an ecological observation‐based assessment, the Activities of Daily Living Profile. Australian Occupational Therapy Journal, 67(5), 407–416.
- Bouma, A., Mulder, J., Lindeboom, J., & Schmand, B. (2012). Handboek neuropsychologische diagnostiek. Pearson.
- Calamia, M., Markon, K., & Tranel, D. (2012). Scoring higher the second time around: meta-analyses of practice effects in neuropsychological assessment. The Clinical Neuropsychologist, 26(4), 543–570.
- Casaletto, K. B., & Heaton, R. K. (2017). Neuropsychological assessment: Past and future. Journal of the International Neuropsychological Society: JINS, 23(9-10), 778–790. https://doi.org/10.1017/S1355617717001060
- Chaytor, N., & Schmitter-Edgecombe, M. (2003). The ecological validity of neuropsychological tests: A review of the literature on everyday cognitive skills. Neuropsychology Review, 13(4), 181–197.
- Chevignard, M., Pillon, B., Pradat-Diehl, P., Taillefer, C., Rousseau, S., Le Bras, C., & Dubois, B. (2000). An ecological approach to planning dysfunction: script execution. Cortex; a Journal Devoted to the Study of the Nervous System and Behavior, 36(5), 649–669.
- Cicerone, K. D. (2005). Methodological issues in evaluating the effectiveness of cognitive rehabilitation. In P. W. Halligan & D. T. Wade (Eds.), Effectiveness of Rehabilitation for Cognitive Deficits (pp. 43–58). Oxford University Press.
- Cicerone, K. D., Goldin, Y., Ganci, K., Rosenbaum, A., Wethe, J. V., Langenbahn, D. M., Malec, J. F., Bergquist, T. F., Kingsley, K., Nagele, D., Trexler, L., Fraas, M., Bogdanova, Y., & Harley, J. P. (2019). Evidence-based cognitive rehabilitation: systematic review of the literature from 2009 through 2014. Archives of Physical Medicine and Rehabilitation, 100(8), 1515–1533. https://doi.org/10.1016/j.apmr.2019.02.011
- Cromwell, D. A., Eagar, K., & Poulos, R. G. (2003). The performance of instrumental activities of daily living scale in screening for cognitive impairment in elderly community residents. Journal of Clinical Epidemiology, 56(2), 131–137.
- Cumming, T., Brodtmann, A., Darby, D., & Bernhardt, J. (2014). The importance of cognition to quality of life after stroke. Journal of Psychosomatic Research, 77(5), 374–379. https://doi.org/10.1016/j.jpsychores.2014.08.009
- Dodge, H. H., Kadowaki, T., Hayakawa, T., Yamakawa, M., Sekikawa, A., & Ueshima, H. (2005). Cognitive impairment as a strong predictor of incident disability in specific ADL-IADL tasks among community-dwelling elders: the Azuchi Study. The Gerontologist, 45(2), 222–230. https://doi.org/10.1093/geront/45.2.222
- Donovan, N. J., Heaton, S. C., Kimberg, C. I., Wen, P.-S., Waid-Ebbs, J. K., Coster, W., Singletary, F., & Velozo, C. A. (2011). Conceptualizing functional cognition in traumatic brain injury rehabilitation. Brain Injury, 25(4), 348–364. https://doi.org/10.3109/02699052.2011.556105
- Fortin, S., Godbout, L., & Braun, C. M. (2003). Cognitive structure of executive deficits in frontally lesioned head trauma patients performing activities of daily living. Cortex; a Journal Devoted to the Study of the Nervous System and Behavior, 39(2), 273–291.
- Giles, G. M., Edwards, D. F., Morrison, M. T., Baum, C., & Wolf, T. J. (2017). Screening for functional cognition in postacute care and the Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014. American Journal of Occupational Therapy, 71(5), 7105090010p1–7105090010p6.
- Goretti, B., Portaccio, E., Zipoli, V., Razzolini, L., & Amato, M. (2010). Coping strategies, cognitive impairment, psychological variables and their relationship with quality of life in multiple sclerosis. Neurological Sciences, 31(S2), 227–230. https://doi.org/10.1007/s10072-010-0372-8
- Harvey, P. D. (2019). Domains of cognition and their assessment. Dialogues in Clinical Neuroscience, 21(3), 227–237. https://doi.org/10.31887/DCNS.2019.21.3/pharvey
- Heruti, R. J., Lusky, A., Dankner, R., Ring, H., Dolgopiat, M., Barell, V., Levenkrohn, S., & Adunsky, A. (2002). Rehabilitation outcome of elderly patients after a first stroke: effect of cognitive status at admission on the functional outcome. Archives of Physical Medicine and Rehabilitation, 83(6), 742–749. https://doi.org/10.1053/apmr.2002.32739
- Howland, M., Allan, K. C., Carlton, C. E., Tatsuoka, C., Smyth, K. A., & Sajatovic, M. (2017). Patient-rated versus proxy-rated cognitive and functional measures in older adults. Patient Related Outcome Measures, 8, 33–42.
- Lezak, M. D., Howieson, D. B., Bigler, E. D., & Tranel, D. (2012). Neuropsychological assessment (5th ed.). Oxford University Press.
- Maruish, M. E. (2004). The use of psychological testing for treatment planning and outcomes assessment: Volume 3: Instruments for adults. Routledge.
- McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R., Kawas, C. H., Klunk, W. E., Koroshetz, W. J., Manly, J. J., Mayeux, R., Mohs, R. C., Morris, J. C., Rossor, M. N., Scheltens, P., Carrillo, M. C., Thies, B., Weintraub, S., & Phelps, C. H. (2011). The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging‐Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's & Dementia, 7(3), 263–269. https://doi.org/10.1016/j.jalz.2011.03.005
- Miller, K., Walterfang, M., Randhawa, S., Scholes, A., Mocellin, R., & Velakoulis, D. (2007). Validity and reliability of the Behavioural Assessment Tool for Cognition and Higher Function (BATCH) in neuropsychiatric patients. The Australian and New Zealand Journal of Psychiatry, 41(8), 697–704.
- Nijsse, B., van Heugten, C. M., van Mierlo, M. L., Post, M. W., de Kort, P. L., & Visser-Meily, J. M. (2017). Psychological factors are associated with subjective cognitive complaints 2 months post-stroke. Neuropsychological Rehabilitation, 27(1), 99–115.
- Nolin, P., Villemure, R., & Heroux, L. (2006). Determining long-term symptoms following mild traumatic brain injury: Method of interview affects self-report. Brain Injury, 20(11), 1147–1154. https://doi.org/10.1080/02699050601049247
- Pan, A.-W., & Fisher, A. G. (1994). The Assessment of Motor and Process Skills of persons with psychiatric disorders. The American Journal of Occupational Therapy, 48(9), 775–780. https://doi.org/10.5014/ajot.48.9.775
- Persoon, A., Banningh, L. J.-W., van de Vrie, W., Rikkert, M. G., & van Achterberg, T. (2011). Development of the nurses' observation scale for cognitive abilities (NOSCA). ISRN Nursing, 2011, 895082. https://doi.org/10.5402/2011/895082
- Poncet, F., Swaine, B., Dutil, E., Chevignard, M., & Pradat-Diehl, P. (2017). How do assessments of activities of daily living address executive functions: a scoping review. Neuropsychological Rehabilitation, 27(5), 618–666.
- Post, M. W., Van de Port, I. G., Kap, B., & Berdenis van Berlekom, S. H. (2009). Development and validation of the Utrecht Scale for Evaluation of Clinical Rehabilitation (USER). Clinical Rehabilitation, 23(10), 909–917.
- Skidmore, E. R. (2017). Functional cognition: Implications for practice, policy, and research. The American Journal of Geriatric Psychiatry, 25(5), 483–484. https://doi.org/10.1016/j.jagp.2016.12.020
- Sohlberg, M. M., & Mateer, C. A. (2017). Cognitive rehabilitation: An integrative neuropsychological approach. Guilford Publications.
- Torenbeek, M., van der Heijden, G. J., de Witte, L. P., & Bakx, W. G. (1998). Construct validation of the Hoensbroeck disability scale for brain injury in acquired brain injury rehabilitation. Brain Injury, 12(4), 307–316.
- Tsaousides, T., & Gordon, W. A. (2009). Cognitive rehabilitation following traumatic brain injury: assessment to treatment. Mount Sinai Journal of Medicine, 76(2), 173–181. https://doi.org/10.1002/msj.20099
- van der Kemp, J., Kruithof, W. J., Nijboer, T. C., van Bennekom, C. A., van Heugten, C., & Visser-Meily, J. M. (2019). Return to work after mild-to-moderate stroke: work satisfaction and predictive factors. Neuropsychological Rehabilitation, 29(4), 638–653.
- van Heugten, C., Caldenhove, S., Crutsen, J., & Winkens, I. (2020). An overview of outcome measures used in neuropsychological rehabilitation research on adults with acquired brain injury. Neuropsychological Rehabilitation, 30(8), 1598–1623. https://doi.org/10.1080/09602011.2019.1589533
- Verhagen, S. J., Daniëls, N. E., Bartels, S. L., Tans, S., Borkelmans, K. W., de Vugt, M. E., & Delespaul, P. A. (2019). Measuring within-day cognitive performance using the experience sampling method: A pilot study in a healthy population. Plos One, 14(12), e0226409. https://doi.org/10.1371/journal.pone.0226409
- World Health Organization. (2001). International classification of functioning, disability and health. World Health Organization.
