Abstract
This study investigated the feasibility (treatment completion, and acceptability) and preliminary effectiveness of computerized working memory (WM) training in a psychiatric outpatient context for adults with ADHD. Self-ratings, neuropsychological tests, and clinician’s assessments were performed pre- and post-Cogmed WM training, as well as at the 2-month follow-up, which included 24 (age M = 36.75 SD = 8.37) participants. Of the 24 participants, 16 (66.67%) completed the 25 sessions within 7 weeks. Completers reported high treatment credibility, but a few spontaneously reported feeling stressed because of the time-consuming nature of the WM training (n = 4). Preliminary effectiveness analyses indicate fewer cognitive difficulties and increased neuropsychological performance in non-trained tests that remained stable at follow-up. Future development of WM training paradigms could investigate ways of making the perception of training experience less demanding regarding being time-consuming. The indication of preliminary effectiveness merits further randomized controlled studies in a clinical context.
Background
Attention Deficit Hyperactivity Disorder (ADHD) is characterized by high symptom levels of inattention and/or hyperactivity/impulsivity (American Psychiatric Association, Citation2013) with an estimated prevalence of around 2.5% in adulthood (Song et al., Citation2021). ADHD is associated with impairments in academic, occupational, and social functioning as well as a psychiatric burden and reduced quality of life (Faraone et al., Citation2021). Although pharmacological interventions can be effective (Cortese et al., Citation2018), impairing symptoms may remain, and not everyone wishes to start or continue with medication over time (Edvinsson & Ekselius, Citation2018; Fredriksen & Peleikis, Citation2016). Thus, there is a need for continued development of non-pharmacological treatment options. Since working memory (WM) is closely related to attention (Oberauer, Citation2019), computerized WM training could be a key to reducing ADHD symptoms and associated functional impairments (Klingberg et al., Citation2005). However, there are only few studies investigating WM training in adults with ADHD. Furthermore, there is limited information regarding clinical implementation i.e., how many adults with ADHD that manage to complete the WM training and how they perceived this intervention. Even though the prevalence of ADHD in outpatient psychiatric populations has been estimated to be between 15% and 27% (Adamis et al., Citation2022), we were not able to identify any previous study investigating the feasibility of computerized WM training in a psychiatric outpatient setting.
WM, described as the ability to actively retain and manipulate information (Miyake et al., Citation2000), has been shown to be impaired in adults with ADHD relative to controls (Alderson et al., Citation2013). Beyond being a possible core deficit giving rise to ADHD symptoms, especially the symptoms of inattentiveness (Martinussen et al., Citation2005), working memory capacity facilitates reasoning, planning, comprehension (Cowan, Citation2014) and is associated with several functional impairments related to adult ADHD (Sjowall & Thorell, Citation2022). Improving WM could therefore result in reduced symptoms of inattentiveness and increased everyday functioning.
Using cognitive training as a possible remedy rest on the assumption that neuroplasticity (Constantinidis & Klingberg, Citation2016) can be induced by increasingly challenging WM tasks, leading to higher WM capacity or efficiency (von Bastian & Oberauer, Citation2014). Such effects have been seen in children, although it has been debated if the observed WM improvements translate into reduced ADHD symptoms and functional impairments (Cortese et al., Citation2015). There is a lack of studies investigating the feasibility and effects of WM training for adults with ADHD (Scholz et al., Citation2020). For Cogmed, one of the most widely used WM training programs, results show gains in WM capacity but limited transfers to daily functioning in adult students with ADHD (Gropper et al., Citation2014; Liu et al., Citation2017; Mawjee et al., Citation2017; Mawjee et al., Citation2015) and adults with ADHD recruited from outpatient settings (Dentz et al., Citation2020). Although current efforts have not been able to produce the desired transfer, future training regimes may be more effective as WM training continues to evolve. Beyond being able to produce improvement in WM, it is important to consider clinical implementation. As treatment interruption can be as high as 82% in various psychiatric outpatient groups (Mazzotti & Barbaranelli, Citation2012), one very important step in the continued development of WM training is investigating feasibility, e.g., attrition and the perspectives of the intended users (O'Cathain et al., Citation2019).
A methodological limitation in previous studies investigating feasibility of WM training in adults is that most are based on student populations. Adults with ADHD that pursue higher education might be relatively well functioning while it has been suggested that outpatient populations might have a higher degree of psychiatric comorbidity and functional impairment (Bitter et al., Citation2019; Edvinsson et al., Citation2010; Fredriksen & Peleikis, Citation2016; Goodman et al., Citation1997). Hence, it should be considered that adults with ADHD from outpatient settings can differ in several aspects that might affect treatment efficacy and feasibility. Still, based on the few studies that have investigated WM training in adults with ADHD (Dentz et al., Citation2020; Gropper et al., Citation2014; Liu et al., Citation2017; Mawjee et al., Citation2015, Citation2017), dropout rates cannot with certainty be attributed to sample characteristics. However, as pointed out, only one study has included an outpatient sample (Dentz et al., Citation2020) and, to the best of our knowledge, no study has had an outspoken aim to investigate feasibility.
Aim
The primary aim was to evaluate the feasibility (treatment completion, and acceptability) of the Cogmed standard WM training program in an outpatient context for adults with ADHD. The secondary aim was to study preliminary effectiveness after completing the training, as well as at a 2-month follow-up, using both self-ratings and neuropsychological tests and clinician assessments.
Methods
This was an open feasibility study in a psychiatric outpatient context including adults with ADHD. The study was approved by the Regional Ethics Committee in Stockholm (2012/1767-31). Data was collected 2013–2015. Similarity of the analyzed training program regarding current training algorithms were confirmed in 2022. All participants gave their written informed consent before inclusion in the study. The study adhered to the CONSORT 2010 Checklist for pilot and feasibility trials. Patient recruitment was conducted at psychiatric outpatient clinics in Stockholm County (Capio Psychiatry Nacka, The Neuropsychiatric Unit, Psychiatry Northwest, Stockholm Health Care Services, The ADHD clinic, Psychiatry North, Stockholm Health Care Services, and WeMind Psychiatry) by referring newly diagnosed adults with ADHD to the Capio Psychiatry clinic.
Participants and recruitment
The participants were recruited from the psychiatric clinics involved in the study, but a few additional participants were included after hearing about the study through word-of-mouth. The people who expressed an interest in participating were informed of the inclusion criteria and the study, and those who fitted these criteria and were interested were then booked for eligibility assessment and validation of their ADHD diagnosis.
Inclusion criteria were being between age 18 and 60, having an ADHD diagnosis, and having the practical possibility to perform cognitive computerized training 30–45 min, 5 days/week for 5 weeks. Since we aimed at including a referred sample typically present in an outpatient psychiatric setting, common psychiatric comorbid disorders (e.g., anxiety and depression disorders) were not excluding criteria. Both individuals with and without ADHD medication were included except for individuals who had made changes in ADHD medication during the last month. No restrictions regarding other medications were included in the exclusion criteria. Exclusion criteria were current problematic substance use (during the previous 3 months); intellectual disability (if IQ < 70 was reported in available medical charts) organic brain injury; severe current psychiatric problems (e.g., schizophrenia) or severe adverse psychosocial circumstances (e.g., being homeless), which made successful participation unlikely or impossible.
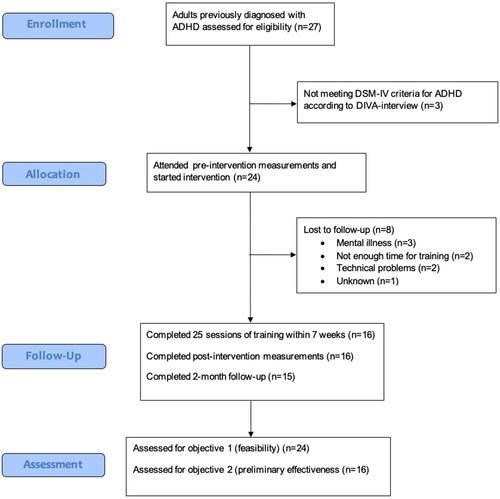
The 27 individuals that were booked for eligibility assessment, were provided with oral and written information for the study and completed the consent form before the initial interview. An experienced psychologist (MB) conducted a D.I.V.A. interview (Kooij & Francken, Citation2010), which assesses ADHD criteria according to DSM-IV to validate the participants’ community-based ADHD diagnoses, and participants also completed a demographic self-assessment form (Hirvikoski et al., Citation2009). Of the 27 individuals, 24 (88.89%) met the inclusion criteria, while three were excluded due to not meeting the ADHD criteria according to the D.I.V.A. Potential practical issues and other obstacles for carrying out the training were discussed with the participants, and a treatment schedule was decided upon. They all agreed to the terms of the training program and the study.
Intervention
The training method that was used in this study was Cogmed QM for older adolescents and adults as developed by Cognitive Medical Systems AB, Stockholm, Sweden. The training included 25 training sessions that were performed 5 days/week for 5 weeks through Cogmeds online platform from the participant’s homes. Each training session took about 30–45 min and included 12 auditory-verbal and visual-spatial WM tasks. The difficulty level of the tasks was automatically adjusted during the 5 weeks of training to ensure that participants are challenged close to their maximum WM capacity. Participants received feedback once a week through phone or email from the psychologist (MB) who had completed Cogmeds online coaching course. All participants initiated the training within the following 5 days after the screening and baseline assessments, as planned. If a participant did not follow the training plan, which was then indicated in the online training portal, they were contacted by the psychologists (MB) for a checkup and discussion on strategies for continuing the training. The participants also had the possibility to contact the psychologist if they had any questions or wanted to discuss any problems with the training. If they chose to end the training program, they were interviewed regarding the reasons why and how they experienced the working memory training. All but one of the participants that did not complete the training was reached.
Measures
After the eligibility assessment, the included participants proceeded to baseline assessment including baseline self-ratings, neuropsychological tests, and clinician’s ratings (T1). These measurements were also administered post-training ± 5 days (T2) and at a 2-month follow-up ± 2 weeks (T3).
Demographic, background information, and validation of ADHD diagnosis
As part of the eligibility assessment, participants completed a demographic self-assessment form (Hirvikoski et al., Citation2009) and a D.I.V.A. interview (Kooij & Francken, Citation2010), and information about comorbid diagnoses were gathered from patient journals. In addition, a self-report scale was completed to assess childhood ADHD symptoms using WURS (Ward et al., Citation1993; Swedish translation Sehlin 1997). It was scored on a Likert scale between 0-4 (from 0= “not at all/very slightly” to 4= “very often”), with higher scores indicating a higher degree of childhood ADHD symptoms. Of the 61 questions, the 25 most important (i.e., most indicative of childhood ADHD) were counted in the total sum of the WURS-25 (Ward et al., Citation1993).
Primary outcome: feasibility
Treatment completion was measured by the number of participants that completed 25 sessions of the WM training within 7 weeks. Since perspectives on computerized WM training from adult outpatient psychiatric populations are lacking, interviews with participants who did not complete the training were performed.
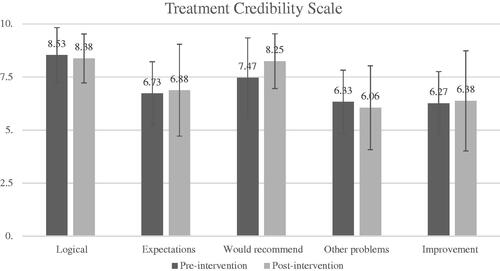
Acceptability was addressed by measuring credibility and safety. Treatment credibility was measured at T1 and T2 using The Treatment Credibility Scale, TCS (Borkovec & Nau, Citation1972). The TCS consisted of five questions and answers were given on a visual analogous scale between 0 (most negative) and 10 (most positive). The questions were: “1. How logical does the treatment offered to you seem?” “2. How successfully do you think this treatment is for reducing your ADHD symptoms?”, “3. How confident would you be in recommending this treatment to a friend with ADHD?”, “4. How successful do you think this treatment is for other types of problems?”, and “5. How improved do you expect to be from this type of treatment?". The total score was the mean of the individual item ratings, with a high sum indicating high perceived credibility. Only individuals who completed the training were included when reporting the treatment credibility before and after training. Safety was measured by noting adverse events, registered in the individual’s case report form. Adverse events were defined as spontaneous reports of any inconvenience that participants reported, and serious adverse events were anything that required inpatient hospitalization.
Secondary outcomes: effectiveness
Effectiveness was measured using self-ratings, performance-based neuropsychological tests, and clinician assessment. Participants completed the ASRS questionnaire (Kessler et al., Citation2005). It consisted of 18 items, regarding ADHD symptoms, and was scored on a Likert scale between 0 and 4 (from 0= “never” to 4= “very often”) where a higher number indicated higher symptom levels. Items were summarized both as a total sum and in separate indexes for inattention and hyperactivity/impulsivity. To get a wider appraisal of cognitive difficulties in everyday life, participants completed the Cognitive Failures Questionnaire (Broadbent et al., Citation1982), measuring cognition, perception, memory, and motor function problems during the last week, including 25 items scored on a Likert scale between 0 and 4 (from 0 = “never” to 4 = “very often”). Higher scores indicated more pronounced difficulties. In addition, to assess ADHD-related executive function problems during the last 2 weeks, participants completed The Barkley Deficits in Executive Functioning Scale, BDEFS (Barkley, Citation2011) which was translated by the authors and back-translated by a native English speaker (PhD and research psychologist, after permission by the scale’s developer (personal communication, April 2011). The 89 items were scored on a Likert scale between 1 and 4 (from 1 = “never/rarely” to 4 = “very often”). The total score, and the Short Form with 11 items especially relevant for ADHD, were used. Higher scores indicated more difficulties.
The standardized performance-based tests targeted various neuropsychological functions. Importantly, these tests were neither computerized nor included in the intervention. For all tests, higher scores indicated better performance. The Spatial Span from WMS-III (Wechsler, Citation1997) was used to measure visual spatial WM. In this test, the participant was instructed to repeat increasingly longer sequences as indicated on a visual board by the researchers. This was done twice, and the second time, the instruction was to repeat the sequence in reverse order. The USA age normed scaled score (population M = 10, SD = 3, range = 1–19) for the total sum was used. Auditory WM was measured using Digit Span from WMS-III (Wechsler, Citation1997). Numbers in increasingly longer sequences were read out loud, and the participants were asked to repeat them, first in order, and later, with other number sequences in reversed order. The USA age normed scaled score for the total sum was used. Mental processing speed, matching numbers with symbols, was measured with the Digit Symbol from WAIS-IV (Wechsler, Citation2008). The Swedish age normed scaled score of the total sum of correct items was used. Perceptual inhibition of automated responses was measured with the Colour-Word Interference Test (Delis et al., Citation2004). The USA age normed total scaled score for completion time was used. Visual attention was measures using D2 Test of Attention (Brickenkamp & Zillmer, Citation1998). The instruction is to mark as many target letters as possible while ignoring other letters. The USA age converted standard scale score for the number of items processed minus errors.
Furthermore, The Clinical Global Impression, CGI (Guy, Citation1976) where the severity of the participants’ disability regarding ADHD symptoms was estimated by an experienced psychologist (MB) at T1, T2, and T3 based on the patients’ reports on their current functioning and well-being. It consisted of one item on a Likert scale between 0 and 7 (from 0 = “not assessed” and 1 = “no dysfunction/normal” to 7 = “among the most severely ill patients”).
Statistical analyses
All 16 participants who finished the working memory training were included in the analysis of treatment efficacy, where repeated measures ANOVAs were used to test for within-subject effects over time. All who finished the working memory training, according to the completion criteria (25 sessions within 7 weeks), completed the post-intervention measurements (T2), and all but one at the 2-month follow-up (T3). The data of the participant who did not perform the 2-month follow-up was copied from T2 to T3 (i.e., last observation carried forward). Test of contrasts included both pre-intervention with post-intervention (i.e., intervention effects) and post-intervention with the 2-month follow-up measurements (i.e., the stability of the improvements). Effect sizes for the contrast were reported using Cohen’s: 0.2 = small, 0.5 = medium, and 0.8 = large (Cohen, Citation1988). The alpha level applied was p < 0.05. IBM SPSS Statistics version 28 was used for analyzing data.
Results
Demographic and clinical characteristics
As can be seen in , a majority (n = 14, 58.30%) of the participants had either one (n = 7 out of 24, 29.17%) or several (n = 7 out of 24, 29.17%) psychiatric diagnoses in addition to ADHD. The most common was depression (n = 9, 37.50%), but participants also had autism, stress-related diagnoses, and several other psychiatric diagnoses (mainly anxiety disorders). Close to 80% of the participants worked, studied or were on parental leave, full or part-time, whereas around 20% were unemployed, on long-term sick leave, or disability pension.
Table 1. Demographic and background data reported for the total group, the group who completed the working memory training, and the non-completers.
Feasibility
Treatment completion
Of the 24 participants, 66.67% (n = 16) completed the 25 sessions of WM training within the 7 weeks predetermined as the cutoff for compliance (see Flowchart). All but one participant was reached after drop-off and the causes for not completing the training were problems regarding aspects of their psychological well-being (n = 3), not having enough time for the training (n = 2), and technical problems (n = 2). As can be seen in , participants who did not complete the training were less likely to have taken part in university studies and had higher levels of hyperactivity/impulsivity and less psychiatric comorbidity ().
Acceptability
The mean treatment credibility for all items was 7.07 (range 4.4–8.2) before starting the WM training and 7.19 (range 4–10) after completion. As indicated by the staples in , the individual items measuring treatment credibility were similar pre-and post-intervention. Of the 16 participants who completed the training, 4 spontaneously reported experiencing, what could be considered adverse effects in the form of increased subjective stress related to the perception that the WM training was time-consuming. No serious adverse events were noted.
Figure 2. The group average includes error bars representing the standard deviation pre-and post-intervention on the Treatment Credibility Scale, rated 0–10. The clustered bars in the figure represent the following questions: “‘1. How logical does the treatment offered to you seem?’ ‘2. How successfully do you think this treatment is for reducing your ADHD symptoms?’, ‘3. How confident would you be in recommending this treatment to a friend with ADHD?’, ‘4. How successful do you think this treatment is for other types of problems?’, and ‘5. How improved do you expect to be from this type of treatment?’”.
Secondary outcomes
As can be seen in , the repeated measures ANOVA showed a significant effect of the WM training on self-rated symptoms of inattention when including all three time-points (p = 0.02). The decreases in symptoms of inattentiveness T1–T2, and T2–T3 (d = 0.24–0.26), did not reach significance (ps > 0.07). However, the repeated measures ANOVA showed a significant effect on self-rated symptoms of cognitive difficulties for CFQ and the BDEFS-short (ps < 0.04). The reduction of cognitive difficulties between pre- to post-measurements were small (d = 0.24–0.40, ps < 0.03) and remained stable to the 2-month follow-up (ps > 0.79). The repeated measures ANOVAs showed significant effects of WM training on all neuropsychological tests (ps < 0.001) except for visual attention (p = 0.06). The increase in neuropsychological performance pre- to post-intervention ranged from d = 0.52 (mental processing speed) to d = 0.89 (auditory working memory) and remained stable to the 2-month follow-up. Finally, the clinician’s global impression of how impairing the participant’s ADHD symptoms were significantly changed according to the repeated measures ANOVA (p < 0.001). While the clinician’s assessment of impairment decreased between pre- to post-intervention (d = 1.33, p < 0.001), it increased back to baseline level between post-intervention assessment and the 2-month follow-up (d = 1.33, p < 0.001).
Table 2. The table includes the average scores (M) and standard deviations (SD) for the effect-related measures for T1, T2 and T3, as well as the F-statistics, p-value, and effect size (Cohen’s d) from the repeated measures ANOVA, for within-subjects change.
Discussion
This study evaluated the feasibility and preliminary effectiveness of computerized WM training in a psychiatric outpatient context for adults with ADHD as such investigations are lacking, to the best of our knowledge. The majority of the participants (66.67%) completed the WM training and reported high levels of treatment credibility both before and after the intervention. Moreover, preliminary analyses of effectiveness showed reduced self-reported cognitive difficulties in everyday life and improved neuropsychological functioning measured with non-trained tests. However, we also identified possible targets for improvement of feasibility, related to the intervention being perceived as time-consuming.
Feasibility
Treatment completion
Of the 24 participants that were allocated to the intervention, one-third did not complete the WM training according to the predefined criteria. The available studies of computerized WM training for adults with ADHD have mainly included student populations, and treatment interruption has varied between 13 (Gropper et al., Citation2014) to 45% (Mawjee et al., Citation2017). Investigating feasibility only in student populations might be misleading as the level of comorbid expressions and symptom severity could be lower than in outpatient settings. There is a need to investigate WM training in settings where it likely to be implemented and in a population that exhibit comorbid expressions that might affect feasibility. In the one study, we were able to identify that included an outpatient population (Dentz et al., Citation2020), dropout rates for active controls and the WM training group were 20% (only reported together). Thus, based on the present study and the few other studies available, it does not seem that dropout rates are higher in adults recruited from outpatient contexts. Also, when compared to other psychiatric treatments in a clinical context, dropout rates are still in an acceptable range (Mazzotti & Barbaranelli, Citation2012).
When investigating possible reasons for not completing the WM training, one needs to take into consideration that the present, as well as the other available studies, have limited sample sizes. However, some results warrant further attention as this is the first study, to our knowledge, to investigate individual characteristics of non-completers including a thorough clinical assessment. All but one of the non-completers displayed the combined form of ADHD and following this also showed higher levels of hyperactivity/impulsivity than the completers. Possibly related, Mawjee et al. (Citation2015) found lower levels of traits related to grit, such as ambition and perseverance, among non-completers. This suggests that the WM training could be improved by paying closer attention to individuals with these characteristics and developing ways to detect and support them when motivation fails and the impulse to quit emerges. The present study also found that non-completers had lower educational levels and less psychiatric comorbidity. However, as we cannot find support for these findings in the other studies on WM training in adults with ADHD, we suggest that replication in other clinical samples is needed before further elaboration is relevant.
Turning to the participant perspective, we managed to interview all but one of the non-completers to understand the reasons behind not completing the training. There were several reasons behind not completing the training including technical problems, such as not feeling mentally well, and not having the time. Of the specific reasons reported, “Not having the time” was also reported by the participants that dropped out in the other study including an outpatient sample (Dentz et al., Citation2020), as well as one of the studies including students (Liu et al., Citation2017). Perhaps there is a need to involve participants even more and discuss these matters before starting the WM training and help create an individualized schedule for the training. Relatedly, four of the participants who completed the training reported adverse events in the form of stress due to the time-consuming nature of the intervention. This also suggests that further attention should be directed toward organizing and supporting participants during the intervention.
Acceptability
Despite the perceived subjective stress, the completer group reported generally high treatment credibility (above 7 on a 0–10-point scale) both before and after the intervention. This indicates sustained trust in the intervention after having the experience of training themselves and being able to evaluate it on their own. No previous study including adults with ADHD has included specific measurements of treatment credibility although positive feedback was reported in the study by Gropper and colleagues (Citation2014).
Secondary outcomes
A strength of this study was the multi-modal measurement methods investigating the preliminary effectiveness of WM training using self-ratings, performance-based neuropsychological tests, and the clinician’s assessments, also including a 2-month follow-up. Although some indication of a reduction of inattentive symptoms, the small effect did not research significance. However, participants reported fewer cognitive difficulties with small effect sizes that remained stable to follow-up. Medium to large increases in performance were observed for most untrained neuropsychological tests that remained stable at the 2-month follow-up. The clinician’s global impression of the burden of participants’ ADHD symptoms had decreased post-intervention but did not remain stable at the 2-month follow-up. The effects are in line with what has been shown in a previous study including a control group (Gropper et al., Citation2014) but there is a need to include active controls (placebo) and double-blinded assessments (Dentz et al., Citation2020). This suggest that the effectiveness on secondary outcomes in this study should be interpreted cautiously. However, the observed effects exceeds what can be expected from retest designs of performance-based tests of WM (Scharfen et al., Citation2018). Also, the indications of transfer effects to untrained tasks merit further controlled studies in clinical contexts given the lack of evidence-based non-pharmacological interventions for this target group.
Limitations
This study included a detailed characterization of the sample and a thorough methodological assessment. However, the major limitation of this feasibility study was that the sample size was small. Furthermore, one of the authors also functioned as the coach for the patients and performed all interviews and assessments, which increased the risk for bias. Regarding the secondary analyses, there was no control group, and we were therefore not able to investigate the level of test-retest effect on the performance-based neuropsychological tests.
Conclusions
To the best of our knowledge, this was the first psychiatric outpatient study to investigate the feasibility of WM training in adults with ADHD. A majority of the participants completed the intervention and found it acceptable both before and after completion. Future WM training paradigms for adults with ADHD could be completed by several more individuals if closer attention is directed to individuals who are more hyperactive/impulsive and by finding ways to reduce stress during the intervention. Future studies should investigate the potential effectiveness shown in this study with controlled designs.
Ethics approval
The study was approved by the Regional Ethics Committee in Stockholm (2012/1767-31) and was performed in accordance with the ethical standards of the Declaration of Helsinki (1964) and its later amendments. Written informed consent was obtained from all individual participants.
Informed consent
Written informed consent to participate, including publication of the study results, was obtained from all individual participants.
Acknowledgements
We want to thank all participants in this study. We would also like to thank PhD Lea Forsman for back-translating the BDEFS, and research assistants Elina Renhorn, Mathilde Annerstedt, and Frida Johansson for entering and controlling data in the database. In addition, we thank the management at Capio, WeMind, and Stockholm Health Care Services, for the opportunity to conduct this study.
Disclosure statement
None of the authors have received financial benefits from education, talks, or presentations related to this study. MB was (during the conception and data collection) employed at Capio Psychiatry Nacka, Stockholm County, and WeMind, TH was at The Neuropsychiatric Unit, Psychiatry Northwest, Stockholm Health Care Services. The founder of the intervention used has previously acted as a supervisor for DS and TH but has not been involved in any phase of this study. TH receives royalties from Hogrefe for non-pharmacological intervention manuals not related to this study.
Data availability
The datasets used during the current study are not made available due to regulations in the ethical permissions for this study.
Additional information
Funding
References
- Adamis, D., Flynn, C., Wrigley, M., Gavin, B., & McNicholas, F. (2022). ADHD in adults: A systematic review and meta-analysis of prevalence studies in outpatient psychiatric clinics. Journal of Attention Disorders, 26(12), 1523–1534. https://doi.org/10.1177/10870547221085503
- Alderson, R. M., Kasper, L. J., Hudec, K. L., & Patros, C. H. (2013). Attention-deficit/hyperactivity disorder (ADHD) and working memory in adults: A meta-analytic review. Neuropsychology, 27(3), 287–302. https://doi.org/10.1037/a0032371
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author.
- Barkley, R. A. (2011). Barkley deficits in executive functioning scale (BDEFS) manual. Guilford Press.
- Bitter, I., Mohr, P., Balogh, L., Látalová, K., Kakuszi, B., Stopková, P., Zmeškalová-Jelenová, D., Pulay, A., & Czobor, P. (2019). ADHD: A hidden comorbidity in adult psychiatric patients. Attention Deficit and Hyperactivity Disorders, 11(1), 83–89. https://doi.org/10.1007/s12402-019-00285-9
- Borkovec, T. D., & Nau, S. D. (1972). Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry, 3(4), 257–260. https://doi.org/10.1016/0005-7916(72)90045-6
- Brickenkamp, R., & Zillmer, E. (1998). The d2 test of attention. Hogrefe & Huber Publishers.
- Broadbent, D. E., Cooper, P. F., FitzGerald, P., & Parkes, K. R. (1982). The Cognitive Failures Questionnaire (CFQ) and its correlates. The British Journal of Clinical Psychology, 21(1), 1–16. https://doi.org/10.1111/j.2044-8260.1982.tb01421.x
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates, Publishers.
- Constantinidis, C., & Klingberg, T. (2016). The neuroscience of working memory capacity and training. Nature Reviews. Neuroscience, 17(7), 438–449. https://doi.org/10.1038/nrn.2016.43
- Cortese, S., Adamo, N., Del Giovane, C., Mohr-Jensen, C., Hayes, A. J., Carucci, S., Atkinson, L. Z., Tessari, L., Banaschewski, T., Coghill, D., Hollis, C., Simonoff, E., Zuddas, A., Barbui, C., Purgato, M., Steinhausen, H.-C., Shokraneh, F., Xia, J., & Cipriani, A. (2018). Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. The Lancet. Psychiatry, 5(9), 727–738. https://doi.org/10.1016/S2215-0366(18)30269-4
- Cortese, S., Ferrin, M., Brandeis, D., Buitelaar, J., Daley, D., Dittmann, R. W., Holtmann, M., Santosh, P., Stevenson, J., Stringaris, A., Zuddas, A., & Sonuga-Barke, E. J. S. (2015). Cognitive training for attention-deficit/hyperactivity disorder: Meta-analysis of clinical and neuropsychological outcomes from randomized controlled trials. Journal of the American Academy of Child and Adolescent Psychiatry, 54(3), 164–174. https://doi.org/10.1016/j.jaac.2014.12.010
- Cowan, N. (2014). Working memory underpins cognitive development, learning, and education. Educational Psychology Review, 26(2), 197–223. https://doi.org/10.1007/s10648-013-9246-y
- Delis, D. C., Kramer, J. H., Kaplan, E., & Holdnack, J. (2004). Reliability and validity of the Delis-Kaplan Executive Function System: An update. Journal of the International Neuropsychological Society: JINS, 10(2), 301–303. https://doi.org/10.1017/S1355617704102191
- Dentz, A., Guay, M. C., Parent, V., & Romo, L. (2020). Working memory training for adults with ADHD. Journal of Attention Disorders, 24(6), 918–927. https://doi.org/10.1177/1087054717723987
- Edvinsson, D., Bingefors, K., Lindstrom, E., & Lewander, T. (2010). ADHD-related symptoms among adults in out-patient psychiatry and female prison inmates as compared with the general population. Upsala Journal of Medical Sciences, 115(1), 30–40. https://doi.org/10.3109/03009730903532333
- Edvinsson, D., & Ekselius, L. (2018). Long-term tolerability and safety of pharmacological treatment of adult attention-deficit/hyperactivity disorder: A 6-year prospective naturalistic study. Journal of Clinical Psychopharmacology, 38(4), 370–375. https://doi.org/10.1097/JCP.0000000000000917
- Faraone, S. V., Banaschewski, T., Coghill, D., Zheng, Y., Biederman, J., Bellgrove, M. A., Newcorn, J. H., Gignac, M., Al Saud, N. M., Manor, I., Rohde, L. A., Yang, L., Cortese, S., Almagor, D., Stein, M. A., Albatti, T. H., Aljoudi, H. F., Alqahtani, M. M. J., Asherson, P., … Wang, Y. (2021). The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neuroscience and Biobehavioral Reviews, 128, 789–818. https://doi.org/10.1016/j.neubiorev.2021.01.022
- Fredriksen, M., & Peleikis, D. E. (2016). Long-term pharmacotherapy of adults with attention deficit hyperactivity disorder: A literature review and clinical study. Basic & Clinical Pharmacology & Toxicology, 118(1), 23–31. https://doi.org/10.1111/bcpt.12477
- Goodman, S. H., Lahey, B. B., Fielding, B., Dulcan, M., Narrow, W., & Regier, D. (1997). Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. Journal of Abnormal Psychology, 106(1), 3–14. https://doi.org/10.1037//0021-843x.106.1.3
- Gropper, R. J., Gotlieb, H., Kronitz, R., & Tannock, R. (2014). Working memory training in college students with ADHD or LD. Journal of Attention Disorders, 18(4), 331–345. https://doi.org/10.1177/1087054713516490
- Guy, W. (1976). Clinical global impression scale. The ECDEU assessment manual for psychopharmacology-revised. (Vol. DHEW Publ No ADM 76–338). U.S.: Department of Health, Education and Welfare.
- Hirvikoski, T., Lindholm, T., Nordenstrom, A., Nordstrom, A. L., & Lajic, S. (2009). High self-perceived stress and many stressors, but normal diurnal cortisol rhythm, in adults with ADHD (attention-deficit/hyperactivity disorder). Hormones and Behavior, 55(3), 418–424. https://doi.org/10.1016/j.yhbeh.2008.12.004
- Kessler, R. C., Adler, L., Ames, M., Demler, O., Faraone, S., Hiripi, E., Howes, M. J., Jin, R., Secnik, K., Spencer, T., Ustun, T. B., & Walters, E. E. (2005). The World Health Organization Adult ADHD Self-Report Scale (ASRS): A short screening scale for use in the general population. Psychological Medicine, 35(2), 245–256. https://doi.org/10.1017/s0033291704002892
- Klingberg, T., Fernell, E., Olesen, P. J., Johnson, M., Gustafsson, P., Dahlström, K., Gillberg, C. G., Forssberg, H., & Westerberg, H. (2005). Computerized training of working memory in children with ADHD–a randomized, controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 44(2), 177–186. https://doi.org/10.1097/00004583-200502000-00010
- Kooij, J. J., & Francken, M. H. (2010). DIVA 2.0. Diagnostic Interview Voor ADHD in Adults bij volwassenen [DIVA 20 Diagnostic Interview ADHD in Adults]. DIVA Foundation.
- Liu, Z. X., Lishak, V., Tannock, R., & Woltering, S. (2017). Effects of working memory training on neural correlates of Go/Nogo response control in adults with ADHD: A randomized controlled trial. Neuropsychologia, 95, 54–72. https://doi.org/10.1016/j.neuropsychologia.2016.11.023
- Martinussen, R., Hayden, J., Hogg-Johnson, S., & Tannock, R. (2005). A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 44(4), 377–384. https://doi.org/10.1097/01.chi.0000153228.72591.73
- Mawjee, K., Woltering, S., Lai, N., Gotlieb, H., Kronitz, R., & Tannock, R. (2017). Working memory training in ADHD: Controlling for engagement, motivation, and expectancy of improvement (pilot study). Journal of Attention Disorders, 21(11), 956–968. https://doi.org/10.1177/1087054714557356
- Mawjee, K., Woltering, S., & Tannock, R. (2015). Working memory training in post-secondary students with ADHD: A randomized controlled study. PLoS One, 10(9), e0137173. https://doi.org/10.1371/journal.pone.0137173
- Mazzotti, E., & Barbaranelli, C. (2012). Dropping out of psychiatric treatment: A methodological contribution. Acta Psychiatrica Scandinavica, 126(6), 426–433. https://doi.org/10.1111/j.1600-0447.2012.01872.x
- Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., & Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex Frontal Lobe” tasks: A latent variable analysis. Cognitive Psychology, 41(1), 49–100. https://doi.org/10.1006/cogp.1999.0734
- Oberauer, K. (2019). Working memory and attention - a conceptual analysis and review. Journal of Cognition, 2(1), 36. https://doi.org/10.5334/joc.58
- O'Cathain, A., Croot, L., Duncan, E., Rousseau, N., Sworn, K., Turner, K. M., Yardley, L., & Hoddinott, P. (2019). Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open, 9(8), e029954. https://doi.org/10.1136/bmjopen-2019-029954
- Scharfen, J., Jansen, K., & Holling, H. (2018). Retest effects in working memory capacity tests: A meta-analysis. Psychonomic Bulletin & Review, 25(6), 2175–2199. https://doi.org/10.3758/s13423-018-1461-6
- Scholz, L., Werle, J., Philipsen, A., Schulze, M., Collonges, J., & Gensichen, J. (2020). Effects and feasibility of psychological interventions to reduce inattention symptoms in adults with ADHD: A systematic review. Journal of Mental Health. https://doi.org/10.1080/09638237.2020.1818189
- Sjowall, D., & Thorell, L. B. (2022). Neuropsychological deficits in relation to ADHD symptoms, quality of life, and daily life functioning in young adulthood. Applied Neuropsychology. Adult, 29(1), 32–40. https://doi.org/10.1080/23279095.2019.1704287
- Song, P., Zha, M., Yang, Q., Zhang, Y., Li, X., & Rudan, I. (2021). The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. Journal of Global Health, 11, 04009. https://doi.org/10.7189/jogh.11.04009
- von Bastian, C. C., & Oberauer, K. (2014). Effects and mechanisms of working memory training: A review. Psychological Research, 78(6), 803–820. https://doi.org/10.1007/s00426-013-0524-6
- Ward, M. F., Wender, P. H., & Reimherr, F. W. (1993). The Wender Utah Rating Scale: An aid in the retrospective diagnosis of childhood attention deficit hyperactivity disorder. The American Journal of Psychiatry, 150(6), 885–890. https://doi.org/10.1176/ajp.150.6.885
- Wechsler, D. (1997). Wechsler memory scale (2rd ed.). Pearson.
- Wechsler, D. (2008). Wechsler adult intelligence scale–Fourth Edition (WAIS–IV). Pearson.