Abstract
Uncontrollable anger is a debilitating consequence of acquired brain injury (ABI). This proof-of-concept study investigated the preliminary efficacy of an emotion regulation intervention for managing post-ABI anger. A secondary objective was to determine which participant characteristics were related to intervention gains. With a pre-post intervention design and three-month follow-up, there were five individually administered meetings on Zoom, over a four-month period. 24 adults who had sustained an ABI were enrolled. Participants were mostly males, from 24 to 85 years old. A series of one-way repeated-measures ANOVAs were conducted to determine the intervention’s efficacy, and Spearman’s rho bivariate correlations for the association between participant characteristics and intervention gains. Significant differences were observed in external anger from baseline to post-treatment; there were no further changes from post-treatment to follow-up. Of the participant characteristics, only readiness to change and anxiety were correlated. The proposed intervention presents a brief, feasible, and preliminary efficacious alternative for regulating post-ABI anger. Intervention gains are associated with readiness to change and anxiety, which has important implications for clinical delivery.
Introduction
Acquired brain injuries (ABIs) have been identified as one of the leading causes of death and disability worldwide (Dewan et al., Citation2019; Institute for Health Metrics and Evaluation (IHME),), Citation2018). An ABI is an insult to the brain that occurs after birth and is unrelated to a genetic or degenerative condition (World Health Organization, Citation1996). Causes include a traumatic brain injury, cerebrovascular accident, infections, tumors, and hypoxic or anoxic events (Chan et al., Citation2013). Notably, uncontrolled anger is a common and long-term consequence of an ABI, affecting up to 41% of survivors during the first five years after injury (Baguley et al., Citation2006; Roy et al., Citation2017).
Verbal manifestations of anger are particularly prevalent after an ABI, and are often characterized by a short temper, outbursts of swearing and yelling, and threats of violence (Gould et al., Citation2019; Pouwels et al., Citation2019; Rao et al., Citation2009; Roy et al., Citation2017). Survivors reported that lifestyle changes like functional impairments from neurological deficits, or cognitive impairments like language difficulties, were particular sources of frustration (see Choi-Kwon & Kim, Citation2022 for a review). They also identified specific individuals (e.g., family members, work colleagues) or issues (e.g., adverse economic circumstances) as sources of anger. However, spontaneous outbursts in the absence of a specific cause, individual, or issue were not uncommon (Choi-Kwon & Kim, Citation2022).
Notably, post-ABI anger has been identified by loved ones as the single most problematic symptom of their survivors’ injuries (Choi-Kwon & Kim, Citation2022; Saban et al., Citation2016). Understandably, this behavior has detrimental effects on personal relationships, with family members and spouses describing a loss of their pre-injury loving relationships and a particular fear of their survivors’ anger (Gould et al., Citation2019; Saban et al., Citation2015; Yasmin & Riley, Citation2022). As such, they are usually the targeted recipients of anger outbursts, noting that their survivors are less tolerable due to their impulsivity, hostility, irritability, and sometimes physical aggression over inconsequential matters (Alderman et al., Citation2013; Choi-Kwon & Kim, Citation2022; Saban et al., Citation2015). Thus, uncontrollable anger is an influential contributor to caregiver burden, which, compared to other health conditions, is especially high for those looking after survivors of ABI (Choi-Kwon & Kim, Citation2022; Harding et al., Citation2015). Apart from these relational consequences, anger is also emotionally maladaptive for survivors of ABI, with depression and anxiety being important and lasting correlates (Baguley et al., Citation2006; Caplan et al., Citation2017; Gould et al., Citation2019; Roy et al., Citation2017; Tateno et al., Citation2003). Thus, targeted anger modulation interventions are much needed, for the wellbeing of both survivors and their loved ones (Cattelani et al., Citation2010; Demark & Gemeinhardt, Citation2002).
Effectiveness of existing interventions
The primary approach for interventions to manage anger has been cognitive behavioral therapy or CBT (Aboulafia-Brakha et al., Citation2013; Hart et al., Citation2012; Medd & Tate, Citation2000; Walker et al., Citation2010). This appears to be moderately effective at reducing anger after ABI (see Byrne & Coetzer, Citation2016; Cattelani et al., Citation2010; Iruthayarajah et al., Citation2018 for reviews). Anger outcome measures such as the State-Trait Anger Expression Inventory-2 (STAXI-2; Spielberger, Citation1999) and the Aggression Questionnaire (AQ-12; Bryant & Smith, Citation2001; Buss & Perry, Citation1992) speak to issues of the duration of treatment effectiveness and the type of anger response.
In terms of short-term effectiveness, CBT-based interventions typically show clear gains from baseline to post-treatment, on measures of external but not internal manifestations of anger. For example, survivors of ABI might display external manifestations by shouting or cursing at others, or internal manifestations by pouting or keeping their anger in (Choi-Kwon & Kim, Citation2022; Lefkovits et al., Citation2021). Findings from Byrne and Coetzer (Citation2016) and Iruthayarajah and colleagues’ (2018) reviews of previous post-ABI anger management interventions demonstrated significant improvements in externally directed anger (as measured by the Trait Anger [TA], Anger Expression-Outwards [AXO], and Anger Control [AC] subscales of the STAXI-2), except for one study (no significant changes were observed on the AQ-12; Aboulafia-Brakha et al., Citation2013). However, internally directed anger seems unaffected (as measured by the Anger Expression-Inwards [AXI] subscale of the STAXI-2). Thus, CBT-based interventions appear to improve external (but not internal) anger immediately after treatment.
In terms of long-term effectiveness, the picture is more complicated, but includes the suggestion that these interventions may maintain or improve not only externally directed anger, but also show some internal gains (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018). This literature suggests that post-treatment gains were, in some cases, maintained when no significant changes were observed on external measures of anger (Walker et al., Citation2010). In other cases, gains continued when significant improvements were observed from baseline to follow-up on these external measures (including the AQ-12; Aboulafia-Brakha et al., Citation2013; Aboulafia-Brakha & Ptak, Citation2016). Moreover, internally directed anger (i.e., AXI) sometimes improved from baseline to follow-up (Aboulafia-Brakha & Ptak, Citation2016). Thus, CBT-based interventions demonstrate mixed evidence of improvement in external anger months after completing treatment, with the added advantage of sometimes also improving internal anger.
Limitations of CBT
Although CBT appears effective for post-ABI anger, it is accompanied by several practical (e.g., number of sessions, type of administration; see Alderman et al., Citation2013 for a review) and theoretical challenges (Witten et al., Citation2022).
One limitation relates to the number of sessions. Some studies include as many as 12 (e.g., Hart et al., Citation2015; Walker et al., Citation2010). Predictably, these have resulted in substantial recruitment difficulties, and attrition rates as high as 25% (Iruthayarajah et al., Citation2018). Multiple sessions also typically comprise several different components (e.g., psychoeducation, relaxation techniques, emotion regulation), potentially obscuring which of the treatment components had the most impact on outcomes (Aboulafia-Brakha & Ptak, Citation2016; Hart et al., Citation2012; Rochat et al., Citation2019).
A second limitation relates to individual versus group administration. Most CBT interventions are group-based (Iruthayarajah et al., Citation2018). While there are social and cost-effective benefits (Demark & Gemeinhardt, Citation2002; Walker et al., Citation2010), a group setting is not always ideal for individuals who may have varying levels of cognitive impairment (Alderman et al., Citation2013; Cattelani et al., Citation2010; Iruthayarajah et al., Citation2018). In these situations, such interventions would benefit from custom-designed content that caters to the nature of cognitive disorders (Aboulafia-Brakha et al., Citation2013; Hart et al., Citation2012, Citation2015; Walker et al., Citation2010 for examples), or be administered one-to-one, so the patient can receive individualized attention from the therapist (Hart et al., Citation2012; Medd & Tate, Citation2000).
A third limitation relates to the theoretical foundations of existing CBT-based interventions for post-ABI anger. This approach does have elements relating to emotion regulation (i.e., the ability to modify and control emotional experiences and reactions; Gross, Citation1998a, Citation2002), such as cognitive restructuring or alternative thinking (Beck, Citation1976; Fenn & Byrne, Citation2013). However, emotion regulation (ER) strategies are not central to the design and implementation of CBT-based interventions. Given the important role of executive functions in emotion management, it should be no surprise that individuals who have sustained lesions to the frontal lobes are especially vulnerable to anger dysregulation (Gyurak et al., Citation2012; Holley et al., Citation2017; Öner, Citation2018; Potegal, Citation2012; Schmeichel & Tang, Citation2015). An ER-based theoretical approach would therefore provide the opportunity to design targeted interventions for survivors of ABI, that apply one or several ER strategies to reduce anger in everyday situations (Salas et al., Citation2019; Witten et al., Citation2022).
An ER approach to post-ABI anger
The Process Model of ER (Gross, Citation1998b, Citation2014) has informed emotion management interventions for survivors of ABI (Rowlands et al., Citation2020, Citation2021; Salas et al., Citation2013, Citation2014). This framework presents five groups of ER strategies that can be applied at varying stages of the emotion generation experience (Gross, Citation2015). Antecedent-focused strategies (i.e., cognitive change, attentional deployment, situation modification, situation selection) are used to manipulate an emotional response before it occurs, whereas response-focused strategies (i.e., response modulation) are used to manipulate an emotional response after it occurs (John & Gross, Citation2004; Mauss et al., Citation2007). Further details on these strategies and their use for post-ABI anger are discussed in Witten et al. (Citation2022). Importantly, incorporating at least two types of ER techniques could be advantageous for survivors of ABI, as this design would cater to individual preferences as well as cognitive strengths or vulnerabilities (Witten et al., Citation2022).
An example of a cognitive change technique is reappraisal (i.e., changing the perception of a situation; Gross, Citation2014). This is the most widely investigated ER technique, and the only one that has been explored as part of an emotion management intervention for survivors of ABI. Although reappraisal has demonstrated the ability to reduce the intensity of negative emotions, its implementation relies on cognitive abilities that are susceptible to impairment following brain injury (Rowlands et al., Citation2020, Citation2021, Salas et al., Citation2013, Citation2014). For this reason, a less cognitively demanding technique, such as distraction (i.e., redirecting attention toward memories that are not connected to the target emotion; Gross, Citation1998b), has been suggested as part of an anger regulation intervention (Witten et al., Citation2022).
Correlates of intervention gains
Determining which participant characteristics are associated with intervention gains is an important component of evaluating treatment outcomes (Cattelani et al., Citation2010; Hart et al., Citation2012, Citation2023). However, such relationships are not always investigated in post-ABI anger. Four important participant characteristics that warrant exploration are mental health, readiness to change, use of ER techniques, and cognitive abilities.
Mental health
Depression and anxiety are common and lasting consequences of ABI (see Juengst et al., Citation2017; Menzel, Citation2008; Osborn et al., Citation2016; Scholten et al., Citation2016, for reviews). ER-based work in this clinical group has either only reported on the presence and severity of mental health symptomology (Salas et al., Citation2014), or on the association between depression and the regulation of positive emotions (Rowlands et al., Citation2020). It seems critical to investigate whether symptoms of both depression and anxiety are associated with intervention gains for anger modulation after ABI, especially considering their relationship (Baguley et al., Citation2006; Caplan et al., Citation2017; Roy et al., Citation2017; Tateno et al., Citation2003).
Readiness to change
Openness to change a targeted behavior has been associated with treatment outcome in several anger management interventions (Howells & Day, Citation2003, for a discussion). For example, higher scores have been correlated with larger improvements in offender populations (Howells et al., Citation2005; Williamson et al., Citation2003). In relation to ABI, readiness to change was first measured as an associate of alcohol consumption (Bombardier et al., Citation1997; Sander et al., Citation2012). One study has investigated this variable as a predictor of treatment outcome in post-ABI anger, with the paradoxical finding that lower readiness to change was associated with greater improvement (Hart et al., Citation2023).
Daily strategy use
The daily use of an ER strategy has been significantly associated with its effectiveness for emotion management after ABI (Rowlands et al., Citation2021). However, the influence on anger, in particular, is less well known. Participating in an anger management intervention has significantly increased the use of ER techniques, such as reappraisal, in the daily lives of survivors of ABI (Aboulafia-Brakha & Ptak, Citation2016). Hence, this seems like a worthy line of research.
Cognitive abilities
Cognitive impairment is another common and long-term consequence of ABI (Cattelani et al., Citation2010; Marsh et al., Citation2016), and is suggested to be a significant correlate of treatment outcome (Hart et al., Citation2012, Citation2015). When selecting cognitive measures, we were mindful of previous ER work in survivors of ABI. Thus, measures of working memory, verbal fluency, and inhibition were employed, as these three cognitive domains have been associated with the implementation of reappraisal in survivors of ABI (Rowlands et al., Citation2020, Citation2021; Salas et al., Citation2013, Citation2014). Importantly, despite the presence of cognitive difficulties, survivors of ABI can still benefit from an anger reduction intervention (e.g., Aboulafia-Brakha & Ptak, Citation2016; Rochat et al., Citation2019).
Study aims
The present study is the first to investigate the preliminary efficacy of a Process Model-based intervention for regulating anger after ABI. The intervention was designed to be efficient: administered individually, and virtually, to participants in as brief as a single session. Furthermore, it includes two ER techniques (see Witten et al., Citation2022 for a justification of the chosen techniques), allowing participants to select one for use in their daily lives, based on their personal preferences and circumstances.
As regards the intervention’s preliminary efficacy, we predicted significant differences in the subscales of the main outcome measures (i.e., STAXI-2 and AQ-12) for characteristic anger, anger expression, and anger control between: (1) baseline and post-treatment and (2) baseline and 3-month follow-up (3MFU). We predicted no significant differences in these same subscales between (3) post-treatment and 3MFU.
As regards the correlates of intervention gains, we predicted significant associations between the differences in the main outcome measures (from baseline to 3MFU) and (1) mental health; (2) readiness to change; (3) ER strategy use; and (4) cognitive functioning.
Method
Design
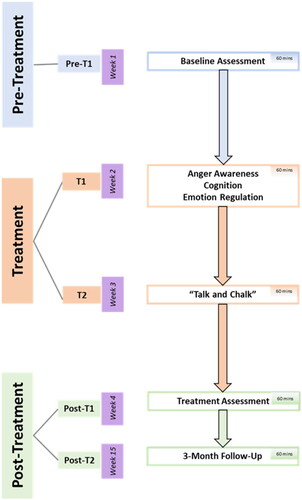
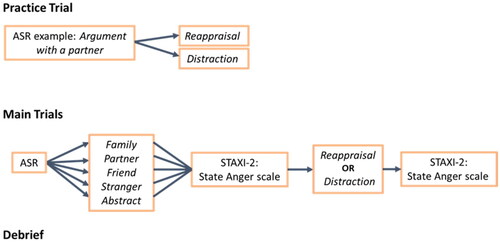
The present study used a pre-post intervention design with a further 3MFU. There were five individually administered, 1-hour Zoom meetings with the Lead Researcher [JAW], over a period of approximately four months. The first four meetings (Pre-T1, T1, T2, and Post-T1) were scheduled to occur once a week, and the follow-up (Post-T2) three months after the intervention (T2). Realistically, the first four meetings occurred, on average, every two weeks (Days: M = 13.60; SD = 3.59) depending on the participant’s availability, and the follow-up, three months and two weeks after the intervention (Weeks: M = 101.04; SD = 10.72). See for an overview of the study’s administration.
Participants
24 participants with an ABI were recruited from brain injury support organizations in the United Kingdom (UK). 14 participants were from Headway UK, two from the Active Care Group, two from Global Brain Injury Awareness (GBIA), and six were recruited via word-of-mouth from these organizations. Like Rowlands et al. (Citation2021), this sample size was governed by the highest number of participants that we were able to recruit, in this case, under conditions of the COVID-19 pandemic (across 2021 and 2022).
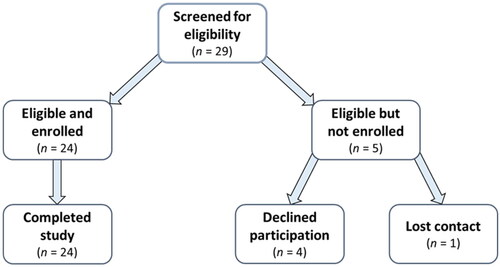
Eligible participants were fluent English-speakers (including Welsh-English bilinguals) who had sustained any type of ABI at least nine months prior to recruitment. Exclusion criteria included any major perceptual or motor impairments that would interfere with task completion, or major neurological or mental health conditions unrelated to the ABI. All screened individuals met the study inclusion criteria (n = 29). However, five did not enroll; four for personal reasons. A total of 24 participants enrolled in and completed the study; none were lost to follow-up. See for an overview of the recruitment process.
10 females and 14 males participated in the study. Participants were, on average, 50.08 years old (SD = 16.85; range 24–85) with 14.63 years of education (SD = 3.49; range 10–22). In addition, they had sustained an ABI an average of 7.88 years ago (median = 5.13; SD = 7.82; range 11 months − 32 years). Mann-Whitney U tests demonstrated no significant differences between males and females with regards to age [U = 85.00, p = .40] and time since injury [U = 70.00, p = 1.00]. A series of paired sample investigations between pre-morbid and post-injury anger demonstrated significant differences in characteristic anger [STAXI-2 Trait Anger t(21) = −3.42, p < .01; AQ-12 t(21) = −3.79, p < .01] and in the outward control of this emotion [t(21) = 2.75, p < .05], with medium to large effect sizes. See for a description of each participant’s demographic and injury characteristics.
Table 1. Demographic and injury characteristics of the current sample (n = 24).
Materials
Anger elicitation
The Affective Story Recall (ASR; Turnbull et al., Citation2005) is an autobiographical recall task used for emotion elicitation. The psychometric properties of the ASR have not been investigated. However, this task has been used in previous studies to elicit emotions in neurologically healthy individuals (Salas et al., Citation2012) and those with ABI (Rowlands et al., Citation2020, Citation2021; Salas Riquelme et al., Citation2015; Tondowski et al., Citation2007). During this task, participants have three minutes to verbally recall a personal event where someone from a particular relationship category (i.e., family member, romantic partner, friend or colleague, stranger, or abstract) made them feel frustrated or angry. These categories were chosen by the researchers as they have previously been identified as relationship types affected by uncontrolled anger (Beames et al., Citation2019).
Anger outcome measures
The STAXI-2 (Spielberger, Citation1999) was chosen as the primary outcome measure of anger. In terms of its psychometric properties, it has demonstrated acceptable reliability and validity (Culhane & Morera, Citation2010; Etzler et al., Citation2014), and is a widely used measure of anger in survivors of ABI (see Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018, for reviews). The STAXI-2 has a total of 57 items and contains three major subscales relating to various components of anger.
Current anger
The State Anger subscale of the STAXI-2 was used as a measure of current anger intensity during the intervention tasks. It has 15 items scored on a 4-point Likert scale, with response options ranging from 1 (“not at all”) to 4 (“very much so”). Higher scores on this subscale indicate more intense feelings of anger.
Characteristic anger
The Trait Anger subscale of the STAXI-2 was used as the primary measure of characteristic anger. It has 10 items scored on a 4-point Likert scale, with response options ranging from 1 (“almost never”) to 4 (“almost always”). Higher scores on this subscale indicate more frequent experiences of anger over time.
The AQ-12 (Bryant & Smith, Citation2001; Buss & Perry, Citation1992) was used as a secondary outcome measure of characteristic anger. In terms of its psychometric properties, it has demonstrated satisfactory reliability and validity (Bryant & Smith, Citation2001), and has been used to measure aggression in survivors of ABI (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018, for reviews). This brief measure has 12 items scored on a 6-point Likert scale, with response options ranging from 1 (“extremely uncharacteristic of me”) to 6 (“extremely characteristic of me”). Higher scores on this measure indicate a higher predisposition toward aggressive behavior.
Anger expression and control
The Anger Expression and Anger Control subscales of the STAXI-2 was used as a measure of the inwards and outwards expression and control of anger. Collectively, these two subscales have 32 items scored on a 4-point Likert scale, with response options ranging from 1 (“almost never”) to 4 (“almost always”). Higher scores on the Expression subscales indicate more frequent outward expressions or inward suppressions of anger. Higher scores on the Control subscales indicate more control over anger.
Mental health
The Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, Citation1983) was used as a measure of anxiety and depression. In terms of its psychometric properties, the HADS has demonstrated good reliability and validity (see Bjelland et al., Citation2002, for a review), and is commonly used to measure mood in survivors of ABI (Aboulafia-Brakha et al., Citation2013; Medd & Tate, Citation2000; Rowlands et al., Citation2020; Salas et al., Citation2014). It has 14 items scored on a scale of 0–3, with response options varying according to each item. Higher scores on this measure indicate a higher state of anxiety or depression.
Readiness to change
The Anger Readiness to Change Questionnaire (ARCQ; Rollnick et al., Citation1992; Williamson et al., Citation2003) was used as a measure of openness to change anger-related behavior. In terms of its psychometric properties, the ARCQ has demonstrated acceptable reliability and validity (Bombardier & Heinemann, Citation2000; Heather et al., Citation1993; Rollnick et al., Citation1992; Williamson et al., Citation2003), and has been used to measure readiness to change certain behaviors in survivors of ABI (Bombardier et al., Citation1997; Sander et al., Citation2012). It has 12 items (4 items representing a subscale for each of the three stages of change) scored on a 5-point Likert scale, with response options ranging from −2 (“strongly disagree”) to 2 (“strongly agree”). Participants are classified into the pre-contemplation, contemplation, or action stages according to their highest score on the relevant subscale. Higher scores on this measure indicate more readiness to change.
Emotion regulation
The Emotion Regulation Questionnaire (ERQ; Gross & John, Citation2003) was used as a measure of the use of ER strategies. In terms of its psychometric properties, the ERQ has demonstrated good reliability and validity (Preece et al., Citation2020, Citation2021), and is a widely used measure of ER in survivors of ABI (Mantua et al., Citation2018; McDonald et al., Citation2010; Salas et al., Citation2013, Citation2014). It has 10 items measuring the use of cognitive reappraisal and expressive suppression, scored on a 7-point Likert scale with response options ranging from 1 (“disagree strongly”) to 7 (“agree strongly”). As the ERQ does not have any items measuring the use of attentional deployment, members of the research team created six additional questions pertaining to this strategy. Higher scores on this measure indicate the more frequent use of ER strategies.
Neuropsychological assessment
A short battery of tests measured the cognitive domains associated with reappraisal implementation in ABI (Rowlands et al., Citation2020, Citation2021; Salas et al., Citation2014). Working memory was measured using the Digit Span subtest from the Wechsler Adult Intelligence Scale – Fourth Edition (WAIS-IV; Wechsler, Citation2010). Verbal generativity was measured using the Letter Fluency subtest from the Verbal Fluency Test in the Delis-Kaplan Executive Function System (DKEFS; Delis et al., Citation2001). Inhibition was measured using the Hayling Sentence Completion Test from the Hayling and Brixton Tests (Burgess & Shallice, Citation1997). All tests have demonstrated satisfactory psychometric properties (Burgess & Shallice, Citation1997; Delis et al., Citation2001; Strong et al., Citation2010; Wechsler, Citation2010), and have been used as cognitive measures in survivors of ABI (e.g., Aboulafia-Brakha & Ptak, Citation2016; McDonald et al., Citation2010; Rowlands et al., Citation2020, Citation2021; Salas Riquelme et al., Citation2015; Salas et al., Citation2014).
Procedure
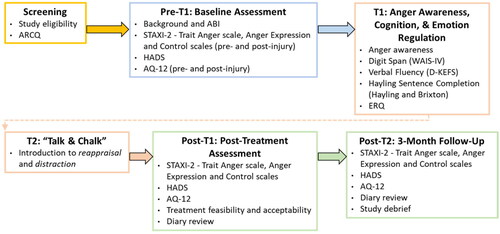
Ethical approval was granted by the Research Ethics and Governance Committee at Bangor University’s School of Human and Behavioral Sciences (reference no. 2020-16812). Informed consent was obtained from all participants. See for a description of each meeting’s content.
All questionnaires were administered verbally by JAW, who read each item out loud to the participant. To avoid potential memory difficulties, the participant was able to simultaneously view the questionnaire items and response options through the screen share feature on Zoom. They were also offered regular breaks throughout each meeting to avoid fatigue. Notably, the administration of self-report measures to survivors of ABI through a videoconferencing platform is suggested to be as effective and reliable as those administered in-person (Rietdijk et al., Citation2017).
Screening
Participant eligibility was confirmed during a screening interview with JAW, which focused on demographic- (e.g., age, language) and injury- (e.g., type, date sustained) related information. The participant also completed a measure of readiness to change their anger-related behavior (i.e., ARCQ).
Baseline assessment (Pre-T1)
The assessment commenced with a background (e.g., years of education completed, marital status) and medical history (e.g., other neurological or mental health conditions) interview. The participant also completed the baseline and pre-morbid measures of anger (i.e., Trait Anger Scale and Anger Expression and Control Scales of the STAXI-2; AQ-12) and a baseline measure of anxiety and depression (i.e., HADS).
Anger awareness, cognition, and emotion regulation (T1)
The session commenced with an anger awareness interview on the cognitive (e.g., “What goes through your mind when you are getting angry?”) and physiological (e.g., “How does it feel in your body when you are getting angry?”) components that identify their anger. In addition to the three cognitive tests measuring working memory, verbal generativity, and inhibition, the participant also completed a measure of how they regulate their emotions in everyday life (i.e., ERQ).
“Talk and Chalk” intervention (T2)
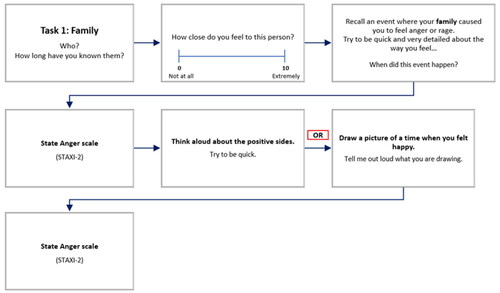
Before commencing the main trials, the participant completed a practice trial, where they could familiarize themselves with the tasks. For each main trial, they recalled an anger-inducing event for one of the five relationship categories (i.e., ASR), after rating their attachment to the specified individual or entity. Next, the participant deployed one of the two ER techniques to regulate their anger for this event (i.e., reappraisal/“Talk” or distraction/“Chalk”). Their current feelings of anger were captured by the State Anger subscale of the STAXI-2 twice: Immediately after recalling the event, and then again after deploying one of the ER techniques. The purpose of these two measurements was to determine whether the ER technique produced any changes in the intensity of anger the participant felt while recalling the event. See for an example of the visual aids that accompanied the main trials.
For example, one participant described a situation where a parent did not approve of his current romantic relationship. This situation was reappraised as bringing him closer to his parent, as well as leading to the re-evaluation of his relationships in general (including friendships). Another participant described a situation where her daughter had neglected her responsibilities to care for her pets. She then engaged in the distraction task, by drawing and describing a picture of a particular path that she enjoys walking on, which is surrounded by trees and wildflowers.
This block of tasks (i.e., ASR > State Anger > ER technique > State Anger) was administered up to five times according to the five relationship categories. These categories, and the use of reappraisal or distraction, were counterbalanced to avoid practice effects. See for the “Talk and Chalk” intervention process.
Homework diary
Like previous anger reduction interventions for survivors of ABI (e.g., Medd & Tate, Citation2000; Rochat et al., Citation2019), participants had the option to practice applying the ER techniques to everyday situations of anger using a diary (based on Deffenbacher & Stark, Citation1992). For each situation, they were encouraged to provide a brief description of what occurred, along with an anger intensity rating (from “0” or “no anger” to “10” or “the most angry I have ever been”). Next, they chose and documented one of the two ER techniques, and rated their anger intensity for the situation after deploying their chosen technique.
10 of the 24 participants (41.7%) used the diary. The group recorded a total of 32 events, with an average of 3 (range 1–11). Reappraisal was chosen for 26 events (81.2%) and distraction for 6 (18.8%). Common reasons for not using the diary were related to practicalities (e.g., no events to record, not having the diary on them when an event occurred), memory (i.e., forgetting to use it), and personal preference (e.g., not being a diary person, already having effective emotion management techniques).
Post-treatment (post-T1) and 3-month follow-up (post-T2) assessments
Both assessments commenced with the baseline measures of anger and anxiety and depression. At Post-T1, the participant also completed an interview on the feasibility and acceptability of the intervention. Any diary entries recorded by the participant were reviewed at both assessments.
Methodological comment
The intervention was designed with the aim of being as clinically realistic and practical as possible. Therefore, the number of trials that participants completed in the 60-minute session was tailored to their individual circumstances. The only requirement was to complete a minimum of two trials, to practice deploying each of the ER strategies at least once. Participants’ individual circumstances were governed by time and relationship category.
Regarding time, the majority of participants grasped the tasks easily, and were able to complete most (if not all) of the trials efficiently . However, some required more time during the practice trial to familiarize themselves with the tasks, resulting in less time allocation for the main trials. As a result, the group completed between two to five main trials: Three of the 24 participants (12.5%) completed all five, 12 participants (50%) completed four, one participant (4.17%) completed three, and eight participants (33.3%) completed two.
Regarding relationship categories, some participants were not able to recall an event for a specific category. This was because they could not identify an individual or entity belonging to this category that angered them. As a result, the “Friend” category was completed by 19 of the 24 participants (79.2%), “Abstract” by 18 (75%), “Stranger” by 16 (66.7%), “Partner” by 15 (62.5%), and “Family” by 14 (58.3%).
Data management and statistical analyses
All statistical analyses were conducted using SPSS. The threshold for statistical significance was set at α = 0.05, unless indicated otherwise.
Intervention’s preliminary efficacy
The intervention’s preliminary efficacy was evaluated through three categories of change: characteristic anger (measured by the Trait Anger subscale of the STAXI-2 and the AQ-12), anger expression (measured by the Anger Expression-In [AXI] and Anger Expression-Out [AXO] subscales of the STAXI-2), and anger control (measured by the Anger Control-In [ACI] and Anger Control-Out [ACO] subscales of the STAXI-2).
All three categories were measured across three timepoints: baseline, post-treatment, and 3MFU. T-scores were used for the STAXI-2 subscales (i.e., scaled scores adjusted for gender and age), and raw scores for the AQ-12. A series of one-way repeated-measures ANOVAs were conducted, and, in the case where sphericity was violated (this only applied to ACI), the Greenhouse-Geisser correction was used. Score differences were calculated between: (1) baseline and post-treatment; (2) baseline and 3MFU; and (3) post-treatment and 3MFU.
Correlates of intervention gains
Participant characteristics
A set of secondary analyses were conducted to explore any relationships between the four participant factors and intervention gains. The first factor, mental health, was derived by calculating the total raw scores for the depression and anxiety subscales on the HADS. The second factor, readiness to change, was derived by converting data from the ARCQ to a continuous variable, by summing the reverse scored precontemplation score with the contemplation and action scores (see Williamson et al., Citation2003 for further details). The third factor, ER strategy use, was derived by calculating the total raw score for the reappraisal subscale on the ERQ, and for the attentional deployment items. The fourth factor, cognitive functioning, was derived by converting the following total or overall raw scores to scaled scores: Digit Span subtest (working memory), Letter Fluency subtest (verbal generativity) and Hayling Sentence Completion Test (Inhibition). Intervention gains were calculated through difference scores between baseline and 3MFU for the measures representing characteristic anger. A series of Spearman’s rho bivariate correlations were then conducted (as the data were not normally distributed) between the difference scores and the four participant factors.
Diary usage
Secondary analyses were also conducted to explore the relationship between diary use and intervention gains. A series of Pearson’s bivariate correlations were conducted between baseline and 3MFU difference scores for the two measures of characteristic anger (continuous variable) and diary use (coded as a dichotomous “yes/no” categorical variable).
Results
Emotional and cognitive functioning
To characterize the group’s emotional and cognitive functioning, and to explore participant factors that could predict the magnitude of improvement, data were collected on four categories: (1) mental health (HADS), (2) readiness to change (ARCQ), (3) ER strategy use (ERQ), and (4) for the three cognitive abilities of working memory, verbal generativity, and inhibition. See for a descriptive summary of their performance on these measures.
Table 2. Descriptive statistics for the sample’s emotional and cognitive functioning (n = 24).
Regarding mental health, the group scored, on average, within the normal range for symptoms of depression (M = 5.75; SD = 4.18) and anxiety (M = 7.54; SD = 4.86). Regarding readiness to change, most participants were classified as being in the contemplation (37%) or action (42%) stages. There was no difference between the reported use of reappraisal and attentional deployment in daily life [t(23) = 0.85, p = .41, small effect size]. Regarding cognitive abilities, the group scored, on average, within the normal range for working memory (M = 9.04; SD = 2.79), verbal generativity (M = 9.13; SD = 2.64), and inhibition (M = 5.25; SD = 1.07).
Intervention’s preliminary efficacy
To determine the intervention’s preliminary efficacy, data were collected on six outcome measures representing characteristic anger (Trait Anger subscale, AQ-12), anger expression (AXI and AXO subscales), and anger control (ACI and ACO subscales), at baseline, post-treatment, and 3-month follow-up (3MFU). Overall, the group demonstrated significant improvements from baseline to 3MFU on five of the six outcome measures. The exception was AXI, where no improvements were evident. See for a descriptive summary of their performance on these measures.
Table 3. Descriptive statistics for the anger outcome measures at three timepoints (n = 24).
Characteristic anger
As seen in , scores on Trait Anger improved from baseline (M = 56.33; SD = 14.55) to 3MFU (M = 47.00; SD = 8.69). A series of one-way repeated measures ANOVAs confirmed significant improvements between baseline and post-treatment [F(1, 23) = 16.59, p < .001, η2 = 0.42 (large effect size), Power = 97%], and baseline and 3MFU [F(1, 23) = 14.06, p = .001, η2 = 0.38 (large effect size), Power = 95%], demonstrating that the greatest gains were observed during the intervention period. Scores on Trait Anger continued to improve from post-treatment to 3MFU, however this improvement was not significant.
Scores on the AQ-12 also improved from baseline (M = 30.38; SD = 10.48) to 3MFU (M = 23.50; SD = 9.12). This improvement was significant [F(1, 23) = 30.39, p < .001, η2 = 0.57 (large effect size), Power = 100%], as was that between post-treatment and 3MFU [F(1, 23) = 14.81, p < .01, η2 = 0.39 (large effect size), Power = 96%], demonstrating that the greatest gains were observed after the intervention period. Scores on the AQ-12 also improved from baseline to post-treatment, however this improvement was not significant.
Anger expression
As seen in , scores on AXI improved slightly from baseline (M = 56.83; SD = 13.03) to 3MFU (M = 57.75; SD = 11.64). However, a series of one-way repeated measures ANOVAs confirmed no significant improvements between any of the three time points. Scores on AXO also improved from baseline (M = 55.83; SD = 15.92) to 3MFU (M = 47.67; SD = 11.78). This improvement was significant [F(1, 23) = 9.55, p < .01, η2 = 0.29 (large effect size), Power = 84%], as was that between baseline and post-treatment [F(1, 23) = 7.21, p < .05, η2 = 0.24 (large effect size), Power = 73%], demonstrating that the greatest gains were observed during the intervention period. Scores on AXO continued to improve from post-treatment to 3MFU, however this improvement was not significant.
Anger control
As seen in , scores on ACI improved from baseline (M = 44.50; SD = 10.50) to 3MFU (M = 51.42; SD = 9.41). A series of one-way repeated measures ANOVAs confirmed that this was the only subscale where significant improvements were observed between all three time points [F(2, 46) = 7.66, p < .01, η2 = 0.25 (large effect size), Power = 85%], demonstrating that the greatest gains were observed both during and after the intervention period.
Scores on ACO also improved from baseline (M = 40.42; SD = 12.89) to 3MFU (M = 46.83; SD = 9.99). This improvement was significant [F(1, 23) = 7.89, p < .05, η2 = 0.26 (large effect size), Power = 77%], as was that between baseline and post-treatment [F(1, 23) = 5.65, p < .05, η2 = 0.20 (large effect size), Power = 62%], demonstrating that the greatest gains were observed during the intervention period. Scores on the ACO continued to improve from post-treatment to 3MFU, however this improvement was not significant.
Time since injury as a predictor of intervention gains
To determine whether time since injury predicted intervention gains, a series of simple regression analyses were conducted with the difference scores between baseline and 3MFU for each of the six outcome measures (dependent variable) and months since injury (predictor variable). These investigations confirmed that time since injury did not significantly predict the amount of change observed for any of the six outcome measures: Trait Anger R2 = 0.01, F(1, 23) = 0.22, p > .05; AQ-12 R2 = 0.01, F(1, 23) = 0.32, p > .05; AXI R2 = 0.01, F(1, 23) = 0.13, p > .05; AXO R2 = 0.01, F(1, 23) = 0.20, p > .05; ACI R2 = 0.00, F(1, 23) = 0.05, p > .05; ACO R2 = 0.00, F(1, 23) = 0.04, p > .05.
Correlates of intervention gains
Participant characteristics
To determine the correlates of intervention gains, a series of bivariate correlations for non-normally distributed data were conducted between the four participant factors, and the baseline to 3MU difference scores for the characteristic anger outcome measures. Overall, anxiety and readiness to change were significantly associated, whereas depression, the use of ER strategies, and levels of cognitive functioning were not ().
Table 4. Relationship between participant characteristics and intervention gains (n = 24).
Readiness to change was the most significant correlate of intervention gains in characteristic anger. While correlation does not imply causality, as seen in , this positive relationship suggests that increases in readiness to change are associated with increases in intervention gains (Trait Anger subscale, p = .007; AQ-12. p = .03). Anxiety was also positively correlated, suggesting that higher levels are associated with increases in intervention gains (Trait Anger subscale, p = .04).
Diary usage
A second set of bivariate correlations were conducted to determine whether diary usage was associated with intervention gains. These findings demonstrated a significant positive relationship for the AQ-12 (r = 0.46, p < .05), but not Trait Anger (r = 0.19, p = .38). It may be of clinical importance that increases in diary entries are associated with increases in intervention gains.
Methodological note
One concern with the varying number of main trials completed during the “Talk and Chalk” intervention, is the possible advantage that the completion of more trials has on the intervention’s efficacy. Thus, a series of investigations confirmed that the number of trials completed did not significantly influence intervention gains for any of the anger outcome measures: Trait Anger F(3, 20) = 1.69, p = .20; AQ-12 F(3, 20) = 2.23, p = .12; AXI F(3, 20) = 1.27, p = .31; AXO F(3, 20) = 0.08, p = .97; ACI F(3, 20) = 0.09, p = .97; ACO F(3, 20) = 0.61, p = .62.
Discussion
The present proof-of-concept study evaluated the initial efficacy of a virtually administered, ER-based intervention for managing post-ABI anger. Although existing interventions are effective (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018), limitations to previous studies include multiple intervention sessions, group administration, and varying conceptual frameworks. Thus, “Talk and Chalk” was designed as a response to these limitations, by providing a theoretically driven, pragmatic yet comparably efficacious alternative. Additional benefits include its delivery via a videoconferencing platform, and the choice between two ER techniques. The main findings are discussed in relation to: (1) the intervention’s short- and long-term efficacy and (2) participant characteristics that are associated with intervention gains.
“Talk and Chalk” reduces anger in the short-term
Determining whether the proposed intervention demonstrates short-term benefits has important implications for its efficacy and acceptability to patients and clinicians. Our results demonstrated clear gains from baseline to post-treatment on external (but not internal) measures of anger. Consistent with existing interventions (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018), participants experienced, and outwardly expressed, less anger, and had better control over this emotion, after the intervention. On the other hand, there were no changes in the way that they internalized their anger.
One possible explanation for this finding is that changing internal anger may require time beyond the intervention period, as this process involves a level of reflection and practice from the individual (Iruthayarajah et al., Citation2018). Future work may therefore explore this possibility, by extending the follow-up period to six or 12 months. Another explanation may be that self-report measures are not sensitive enough to detect changes in internal anger. Therefore, future work may consider using objective approaches such as physiological measures. Nonetheless, although improvements in internal anger would have been beneficial, external expressions are arguably more important, as these are the types of behaviors that affect family members and loved ones (Gould et al., Citation2019; Saban et al., Citation2015; Yasmin & Riley, Citation2022). Taken together, these findings support the initial efficacy of “Talk and Chalk” for post-ABI anger modulation in the short-term. Given these promising results, it was of interest to determine whether these gains were maintained over time.
“Talk and Chalk” shows promise in the long-term
Determining whether the proposed intervention demonstrates long-term benefits has important implications for its real-world applicability. Our results demonstrated that the type of gains observed for external measures of anger depend on the evaluation period. Consistent with existing interventions (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018), improvements continued from pre-treatment to follow-up, in the way that participants experienced and outwardly expressed anger, as well as their control over this emotion. However, there were no further improvements from post-treatment to follow-up.
These findings suggest a noteworthy real-world implication, in that individuals can, indeed, demonstrate improvements in external anger over time. However, as a group, gains stabilized at post-treatment. In addition, consistent with short-term findings, internal anger remained non-significant over time. Building upon Iruthayarajah et al. (Citation2018) explanation, future studies may consider extending their follow-up period to 6 or 12 months. However, this recommendation is less urgent, as improvements in external anger remain important for personal relationships with family members and loved ones. Taken together, these findings support the notion that “Talk and Chalk” potentially has long-lasting benefits for post-ABI anger modulation, with important consequences for the field.
Relevance to the field
In sum, “Talk and Chalk” produced similar short- and long-term gains to existing interventions (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018), by improving external (but not internal) anger, and maintaining these gains at follow-up. Not only is it an efficient, feasible, and initially efficacious alternative for regulating post-ABI anger, “Talk and Chalk” also has other advantages over existing interventions.
Firstly, “Talk and Chalk” can be administered in a single session, minimizing attrition rates (cf., Hart et al., Citation2015; Walker et al., Citation2010). Relatedly, this session focused on ER, while existing interventions address multiple topics (e.g., psychoeducation, relaxation techniques), making it difficult to establish which produced therapeutic gains (Aboulafia-Brakha & Ptak, Citation2016; Hart et al., Citation2012; Rochat et al., Citation2019). Secondly, “Talk and Chalk” was administered individually, suggesting that this type of delivery is comparable to group designs (and perhaps contributed to the zero drop-out rate), while allowing the practitioner to tailor the content to the participant’s cognitive needs. Thirdly, the intervention’s theoretical foundation is based on improving ER through the application of two techniques. These relatively simple techniques avoid abstract theories and skills that may require a level of metacognitive ability (cf., CBT; Moritz et al., Citation2019; Sassaroli et al., Citation2015).
Two additional benefits to the study design are notable. Firstly, “Talk and Chalk” was delivered online, via a videoconferencing platform. Despite the limitations to virtual care (see Tenforde et al., Citation2017 for a review), our participants reported that this mode of delivery was preferrable, as it avoided travel and logistical requirements of an in-person appointment. Secondly, this is the first study to investigate patient choice in an ER intervention for post-ABI anger (Witten et al., Citation2022). Our participants were provided with two ER techniques, and, during the homework activity, chose one based on personal preferences or situational practicalities. Thus, in addition to addressing some of the limitations in the field, these additional benefits might make “Talk and Chalk” a more appealing and flexible option to patients.
Readiness to change and anxiety are important correlates
Identifying which participant characteristics are related to intervention gains may have implications for clinical care (Cattelani et al., Citation2010; Hart et al., Citation2012, Citation2023). Firstly, in keeping with similar research in offender populations (Howells et al., Citation2005; Williamson et al., Citation2003) and those with ABI (Hart et al., Citation2023), readiness to change appears to be an important factor for improvements in characteristic anger. The second important factor was anxiety, which could be explained by the finding that anxious individuals have demonstrated behavior improvements due to increased perfectionism (see Hewitt et al., Citation2002). Nonetheless, considering the high prevalence of post-ABI anxiety (Osborn et al., Citation2016; Scholten et al., Citation2016), clinicians could have concerns regarding “Talk and Chalk’s” suitability for anxious patients, and may therefore, along with readiness to change, include these two variables as part of their criteria for potential intervention candidates.Footnote1
Depression, strategy use, and cognitive functioning were not related
Identifying which participant characteristics are unrelated to intervention gains are equally important. Depression and the use of ER strategies were not associated with treatment outcome, although our findings are inconsistent with previous studies that found an association between depression and the modulation of positive emotions (Rowlands et al., Citation2020), or between the use of ER strategies and the effectiveness of an ER technique (Rowlands et al., Citation2021). Regarding domains of cognitive functioning (i.e., working memory, verbal generativity, inhibition), our results are consistent with a previous study that found these variables were not correlated (Rowlands et al., Citation2020). Thus, it appears that depression, the use of an ER strategy, and certain cognitive domains should not be included as contraindications for potential “Talk and Chalk” candidates.
Adapting “Talk and Chalk”
Tailoring the “Talk and Chalk” content to suit each participant’s individual circumstances highlighted further considerations for its clinical implementation. Firstly, some patients may be able to complete all five trials relatively quickly, whereas others may complete as few as two if they require more time to grasp the task. Importantly, our results suggested that the number of trials completed did not influence the intervention’s initial efficacy. Secondly, clinicians may consider skipping a relationship category if a patient is unable to recall an anger-inducing event, if, for example, they have never had a romantic partner. Finally, diary use was associated with intervention gains. It therefore may be appropriate for clinicians to encourage patients to use this resource to apply the ER techniques to their day-to-day situations of anger. Notably, these adaptions were possible due to the one-to-one administration of the intervention, rendering “Talk and Chalk” most suitable for individual therapy.
Limitations
The present study has important clinical implications, however there are several limitations to consider when interpreting the results.
First, like previous exploratory studies (Aboulafia-Brakha et al., Citation2013; Hart et al., Citation2012) we used a pre-post intervention design as the first step in establishing proof-of-concept. As such, our findings are governed by a small sample size and the lack of a comparison group. Nonetheless, considering that our outcome measures demonstrated changes in the anticipated direction, the next step would be to conduct a randomized control trial (RCT) with a waitlist control group and larger sample size.
Second, in this RCT study, the influence of clinically important variables (e.g., pretreatment strategies) on the main outcome measures would be investigated through analytic approaches such as an ANCOVA. Relatedly, although the varying number of completed trials did not influence the intervention’s initial efficacy, the RCT should ensure that all participants complete the same number of trials for purposes of consistency and treatment fidelity. Due to practical considerations, participants in our study completed fewer intervention trials involving situations with a family member or partner. Given that these individuals are especially affected by post-ABI anger (Alderman et al., Citation2013; Choi-Kwon & Kim, Citation2022; Saban et al., Citation2015), it is particularly important that such situations are represented in the RCT.
Third, although some of our participants had mild-to-moderate levels of clinical or cognitive impairment, overall, the group scored within the normal range on these measures. Thus, our results may not generalize to a more severely impaired population, and future work may consider using a sample of persons with more severe cognitive impairment. Relatedly, future work may consider including additional tests of executive function that may contribute to the day-to-day application of ER techniques, such as those measuring abstract reasoning or cognitive flexibility.
Fourth, injury severity could not be established given the heterogeneous nature of the group’s ABI etiologies. Relatedly, a small number of participants provided diagnostic data via self-report only, which would have potentially limited the accuracy of grading injury severity in these cases. Future work may therefore consider establishing injury severity (and its potential influence on outcome measures) through a single etiology (e.g., TBI), and to confirm any self-reported ABI descriptors through objective clinical records. Nonetheless, our mixed group is arguably also a strength of the study, as it is reflective of the diverse ABI population (Rowlands et al., Citation2021).
Lastly, although our study, like many others in the field (Byrne & Coetzer, Citation2016; Iruthayarajah et al., Citation2018) measures efficacy through self-report measures, there is always the risk that responses are susceptible to demand characteristics. Thus, future research may consider including a supplementary outcome measure that is, for example, physiological in nature, to overcome some of the limitations inherent to self-report data after brain injury (e.g., subjectivity, impact of potential cognitive difficulties, impairments in self-awareness). Alternatively, administering the self-report outcome measures to a participant’s family member or partner would not only validate their responses, but also provide valuable insights into whether reductions in their self-perceived external manifestations of anger are consistent with real-world observations.
Conclusion
The present proof-of-concept study evidences the preliminary efficacy of a virtually administered, Process Model-based, ER intervention for post-ABI anger. “Talk and Chalk” presents an efficient and possibly more patient-friendly alternative to existing interventions such as CBT. It improves external manifestations of anger in the short-term and maintains treatment gains over time. Furthermore, personal characteristics, such as readiness to change and anxiety, are associated with intervention gains. These findings justify a RCT, and are relevant to healthcare professionals who are providing clinical care to survivors of ABI.
Acknowledgments
The authors would like to thank all the participants and staff at Headway UK, the Active Care Group, and Global Brain Injury Awareness (GBIA) for their invaluable contributions to this work. We would also like to thank the individual stroke survivors across North Wales, who gave their time to share their experiences.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
Notes
1 Given the importance of readiness to change and anxiety, it was of interest to investigate whether these two variables were related. However, a Spearman’s rho correlational analysis demonstrated non-significant findings (r = 0.40, p = .06).
References
- Aboulafia-Brakha, T., Greber Buschbeck, C., Rochat, L., & Annoni, J. M. (2013). Feasibility and initial efficacy of a cognitive-behavioural group programme for managing anger and aggressiveness after traumatic brain injury. Neuropsychological Rehabilitation, 23(2), 216–233. https://doi.org/10.1080/09602011.2012.747443
- Aboulafia-Brakha, T., & Ptak, R. (2016). Effects of group psychotherapy on anger management following acquired brain injury. Brain Injury, 30(9), 1121–1130. https://doi.org/10.1080/02699052.2016.1174784
- Alderman, N., Knight, C., & Brooks, J. (2013). Rehabilitation approaches to the management of aggressive behaviour disorders after acquired brain injury. Brain Impairment, 14(1), 5–20. https://doi.org/10.1017/BrImp.2013.7
- Baguley, I. J., Cooper, J., & Felmingham, K. (2006). Aggressive behavior following traumatic brain injury: How common is common? Journal of Head Trauma Rehabilitation, 21(1), 45–56. https://doi.org/10.1097/00001199-200601000-00005
- Beames, J. R., O’Dean, S. M., Grisham, J. R., Moulds, M. L., & Denson, T. F. (2019). Anger regulation in interpersonal contexts: Anger experience, aggressive behavior, and cardiovascular reactivity. Journal of Social and Personal Relationships, 36(5), 1441–1458. https://doi.org/10.1177/0265407518819295
- Beck, A. T. (1976). Cognitive therapy and the emotional disorders. Penguin.
- Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale: An updated literature review. Journal of Psychosomatic Research, 52(2), 69–77. https://doi.org/10.1016/S0022-3999(01)00296-3
- Bombardier, C. H., Ehde, D., & Kilmer, J. (1997). Readiness to change alcohol drinking habits after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 78(6), 592–596. https://doi.org/10.1016/S0003-9993(97)90424-X
- Bombardier, C. H., & Heinemann, A. W. (2000). The construct validity of the readiness to change questionnaire for persons with TBI. Journal of Head Trauma Rehabilitation, 15(1), 696–709. https://doi.org/10.1097/00001199-200002000-00008
- Bryant, F. B., & Smith, B. D. (2001). Refining the architecture of aggression: A measurement model for the Buss–Perry Aggression Questionnaire. Journal of Research in Personality, 35(2), 138–167. https://doi.org/10.1006/jrpe.2000.2302
- Burgess, P. W., & Shallice, T. (1997). The Hayling and Brixton tests. Thames Valley Test.
- Buss, A. H., & Perry, M. (1992). The aggression questionnaire. Journal of Personality and Social Psychology, 63(3), 452–459. https://doi.org/10.1037/0022-3514.63.3.452
- Byrne, C., & Coetzer, R. (2016). The effectiveness of psychological interventions for aggressive behavior following acquired brain injury: A meta-analysis and systematic review. NeuroRehabilitation, 39(2), 205–221. https://doi.org/10.3233/NRE-161352
- Caplan, B., Bogner, J., Brenner, L., Neumann, D., Malec, J. F., & Hammond, F. M. (2017). The relations of self-reported aggression to alexithymia, depression, and anxiety after traumatic brain injury. Journal of Head Trauma Rehabilitation, 32(3), 205–213.
- Cattelani, R., Zettin, M., & Zoccolotti, P. (2010). Rehabilitation treatments for adults with behavioral and psychosocial disorders following acquired brain injury: A systematic review. Neuropsychology Review, 20(1), 52–85. https://doi.org/10.1007/s11065-009-9125-y
- Chan, V., Zagorski, B., Parsons, D., & Colantonio, A. (2013). Older adults with acquired brain injury: A population based study. BMC Geriatrics, 13(1), 1–12. https://doi.org/10.1186/1471-2318-13-97
- Choi-Kwon, S., & Kim, J. S. (2022). Anger, a result and cause of stroke: A narrative review. Journal of Stroke, 24(3), 311–322. https://doi.org/10.5853/jos.2022.02516
- Culhane, S. E., & Morera, O. F. (2010). Reliability and validity of the Novaco Anger Scale and Provocation Inventory (NAS-PI) and State-Trait Anger Expression Inventory-2 (STAXI-2) in Hispanic and non-Hispanic white student samples. Hispanic Journal of Behavioral Sciences, 32(4), 586–606. https://doi.org/10.1177/0739986310381458
- Deffenbacher, J. L., & Stark, R. S. (1992). Relaxation and cognitive-relaxation treatments of general anger. Journal of Counseling Psychology, 39(2), 158–167. https://doi.org/10.1037/0022-0167.39.2.158
- Delis, D. C., Kaplan, E., & Kramer, J. H. (2001). Delis-Kaplan executive function system (D-KEFS). The Psychological Corporation.
- Demark, J., & Gemeinhardt, M. (2002). Anger and it’s management for survivors of acquired brain injury. Brain Injury, 16(2), 91–108. https://doi.org/10.1080/02699050110102059
- Dewan, M. C., Rattani, A., Gupta, S., Baticulon, R. E., Hung, Y. C., Punchak, M., Agrawal, A., Adeleye, A. O. M. G., Shrime, M. G., Rubiano, A. M., Rosenfeld, J. V., & Park, K. B. (2019). Estimating the global incidence of traumatic brain injury. Journal of Neurosurgery, 130(4), 1080–1097. https://doi.org/10.3171/2017.10.JNS17352
- Etzler, S. L., Rohrmann, S., & Brandt, H. (2014). Validation of the STAXI-2: A study with prison inmates. Psychological Test and Assessment Modeling, 56(2), 178–194.
- Fenn, K., & Byrne, M. (2013). The key principles of cognitive behavioural therapy. InnovAiT: Education and Inspiration for General Practice, 6(9), 579–585. https://doi.org/10.1177/1755738012471029
- Gould, K. R., Hicks, A. J., Hopwood, M., Kenardy, J., Krivonos, I., Warren, N., & Ponsford, J. L. (2019). The lived experience of behaviours of concern: A qualitative study of men with traumatic brain injury. Neuropsychological Rehabilitation, 29(3), 376–394. https://doi.org/10.1080/09602011.2017.1307767
- Gross, J. J. (1998a). Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology, 74(1), 224–237. https://doi.org/10.1037/0022-3514.74.1.224
- Gross, J. J. (1998b). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. https://doi.org/10.1037/1089-2680.2.3.271
- Gross, J. J. (2002). Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology, 39(3), 281–291. https://doi.org/10.1017/S0048577201393198
- Gross, J. J. (2014). Emotion regulation: Conceptual and empirical foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 3–20). Guilford Press.
- Gross, J. J. (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. https://doi.org/10.1080/1047840X.2014.940781
- Gross, J. J., & John, O. P. (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well‐being. Journal of Personality and Social Psychology, 85(2), 348–362. https://doi.org/10.1037/0022-3514.85.2.348
- Gyurak, A., Goodkind, M. S., Kramer, J. H., Miller, B. L., & Levenson, R. W. (2012). Executive functions and the down-regulation and up-regulation of emotion. Cognition & Emotion, 26(1), 103–118. https://doi.org/10.1080/02699931.2011.557291
- Harding, R., Gao, W., Jackson, D., Pearson, C., Murray, J., & Higginson, I. J. (2015). Comparative analysis of informal caregiver burden in advanced cancer, dementia, and acquired brain injury. Journal of Pain and Symptom Management, 50(4), 445–452. https://doi.org/10.1016/j.jpainsymman.2015.04.005
- Hart, T., Brockway, J. A., Fann, J. R., Maiuro, R. D., & Vaccaro, M. J. (2015). Anger self-management in chronic traumatic brain injury: Protocol for a psycho-educational treatment with a structurally equivalent control and an evaluation of treatment enactment. Contemporary Clinical Trials, 40, 180–192. https://doi.org/10.1016/j.cct.2014.12.005
- Hart, T., Maiuro, R. D., Fann, J. R., Vaccaro, M. J., & Chervoneva, I. (2023). Predictors of treatment response to a psychoeducational intervention for anger in chronic moderate-severe traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 35(2), 158–164. https://doi.org/10.1176/appi.neuropsych.21110279
- Hart, T., Vaccaro, M. J., Hays, C., & Maiuro, R. D. (2012). Anger self-management training for people with traumatic brain injury: A preliminary investigation. Journal of Head Trauma Rehabilitation, 27(2), 113–122. https://doi.org/10.1097/HTR.0b013e31820e686c
- Heather, N., Rollnick, S., & Bell, A. (1993). Predictive validity of the readiness to change questionnaire. Addiction, 88(12), 1667–1677. https://doi.org/10.1111/j.1360-0443.1993.tb02042.x
- Hewitt, P. L., Caelian, C. F., Flett, G. L., Sherry, S. B., Collins, L., & Flynn, C. A. (2002). Perfectionism in children: Associations with depression, anxiety, and anger. Personality and Individual Differences, 32(6), 1049–1061. https://doi.org/10.1016/S0191-8869(01)00109-X
- Holley, S. R., Ewing, S. T., Stiver, J. T., & Bloch, L. (2017). The relationship between emotion regulation, executive functioning, and aggressive behaviors. Journal of Interpersonal Violence, 32(11), 1692–1707. https://doi.org/10.1177/0886260515592619
- Howells, K., & Day, A. (2003). Readiness for anger management: Clinical and theoretical issues. Clinical Psychology Review, 23(2), 319–337. https://doi.org/10.1016/S0272-7358(02)00228-3
- Howells, K., Day, A., Williamson, P., Bubner, S., Jauncey, S., Parker, A., & Heseltine, K, K. (2005). Brief anger management programs with offenders: Outcomes and predictors of change. Journal of Forensic Psychiatry & Psychology, 16(2), 296–311. https://doi.org/10.1080/14789940500096099
- Institute for Health Metrics and Evaluation (IHME). (2018). Findings from the global burden of disease study 2017 [policy report]. https://www.healthdata.org/sites/default/files/files/policy_report/2019/GBD_2017_Booklet.pdf.
- Iruthayarajah, J., Alibrahim, F., Mehta, S., Janzen, S., McIntyre, A., & Teasell, R. (2018). Cognitive behavioural therapy for aggression among individuals with moderate to severe acquired brain injury: A systematic review and meta-analysis. Brain Injury, 32(12), 1443–1449. https://doi.org/10.1080/02699052.2018.1496481
- John, O. P., & Gross, J. J. (2004). Healthy and unhealthy emotion regulation. Personality processes, individual differences, and lifespan development. Journal of Personality, 72(6), 1301–1333. https://doi.org/10.1111/j.1467-6494.2004.00298.x
- Juengst, S. B., Kumar, R. G., & Wagner, A. K. (2017). A narrative literature review of depression following traumatic brain injury: Prevalence, impact, and management challenges. Psychology Research and Behavior Management, 10, 175–186. https://doi.org/10.2147/PRBM.S113264
- Lefkovits, A. M., Hicks, A. J., Downing, M., & Ponsford, J. (2021). Surviving the “silent epidemic”: A qualitative exploration of the long-term journey after traumatic brain injury. Neuropsychological Rehabilitation, 31(10), 1582–1606. https://doi.org/10.1080/09602011.2020.1787849
- Mantua, J., Helms, S. M., Weymann, K. B., Capaldi, V. F., & Lim, M. M. (2018). Sleep quality and emotion regulation interact to predict anxiety in veterans with PTSD. Behavioural Neurology, 2018, 1–10. https://doi.org/10.1155/2018/7940832
- Marsh, N. V., Ludbrook, M. R., & Gaffaney, L. C. (2016). Cognitive functioning following traumatic brain injury: A five-year follow-up. NeuroRehabilitation, 38(1), 71–78. https://doi.org/10.3233/NRE-151297
- Mauss, I. B., Cook, C. L., Cheng, J. Y., & Gross, J. J. (2007). Individual differences in cognitive reappraisal: Experiential and physiological responses to an anger provocation. International Journal of Psychophysiology, 66(2), 116–124. https://doi.org/10.1016/j.ijpsycho.2007.03.017
- McDonald, S., Hunt, C., Henry, J. D., Dimoska, A., & Bornhofen, C. (2010). Angry responses to emotional events: The role of impaired control and drive in people with severe traumatic brain injury. Journal of Clinical and Experimental Neuropsychology, 32(8), 855–864. https://doi.org/10.1080/13803391003596405
- Medd, J., & Tate, R. L. (2000). Evaluation of an anger management therapy programme following acquired brain injury: A preliminary study. Neuropsychological Rehabilitation, 10(2), 185–201. https://doi.org/10.1080/096020100389246
- Menzel, J. C. (2008). Depression in the elderly after traumatic brain injury: A systematic review. Brain Injury, 22(5), 375–380. https://doi.org/10.1080/02699050802001492
- Moritz, S., Klein, J. P., Lysaker, P. H., & Mehl, S. (2019). Metacognitive and cognitive-behavioral interventions for psychosis: New developments. Dialogues in Clinical Neuroscience, 21(3), 309–317. https://doi.org/10.31887/DCNS.2019.21.3/smoritz
- Öner, S. (2018). Neural substrates of cognitive emotion regulation: A brief review. Psychiatry and Clinical Psychopharmacology, 28(1), 91–96. https://doi.org/10.1080/24750573.2017.1407563
- Osborn, A. J., Mathias, J. L., & Fairweather-Schmidt, A. K. (2016). Prevalence of anxiety following adult traumatic brain injury: A meta-analysis comparing measures, samples and post injury intervals. Neuropsychology, 30(2), 247–261. https://doi.org/10.1037/neu0000221
- Potegal, M. (2012). Temporal and frontal lobe initiation and regulation of the top-down escalation of anger and aggression. Behavioural Brain Research, 231(2), 386–395. https://doi.org/10.1016/j.bbr.2011.10.049
- Pouwels, C. G. J. G., Spauwen, P. J. J., Bus, B. A. A., Winkens, I., & Ponds, R. W. H. M. (2019). Prevalence and manifestations of aggression in adult patients with acquired brain injury: A review. Tijdschrift Voor Psychiatrie, 61(12), 862–878.
- Preece, D. A., Becerra, R., Hasking, P., McEvoy, P. M., Boyes, M., Sauer-Zavala, S., Chen, W., & Gross, J. J. (2021). The emotion regulation questionnaire: Psychometric properties and relations with affective symptoms in a United States general community sample. Journal of Affective Disorders, 284, 27–30. https://doi.org/10.1016/j.jad.2021.01.071
- Preece, D. A., Becerra, R., Robinson, K., & Gross, J. J. (2020). The emotion regulation questionnaire: Psychometric properties in general community samples. Journal of Personality Assessment, 102(3), 348–356. https://doi.org/10.1080/00223891.2018.1564319
- Rao, V., Rosenberg, P., Bertrand, M., Salehinia, S., Spiro, J., Vaishnavi, S., Rastogi, P., Noll, K., Schretlen, D. J., Brandt, J., Cornwell, E., Makley, M., & Miles, Q. S. (2009). Aggression after traumatic brain injury: Prevalence and correlates. The Journal of Neuropsychiatry and Clinical Neurosciences, 21(4), 420–429. https://doi.org/10.1176/jnp.2009.21.4.420
- Rietdijk, R., Power, E., Brunner, M., & Togher, L. (2017). Reliability of videoconferencing administration of a communication questionnaire to people with traumatic brain injury and their close others. The Journal of Head Trauma Rehabilitation, 32(6), E38–E44. https://doi.org/10.1097/HTR.0000000000000282
- Rochat, L., Manolov, R., Aboulafia-Brakha, T., & Berner-Burkard, C, M. (2019). & Van der Linden. Reducing anger outbursts after a severe TBI: A single-case study. Neuropsychological Rehabilitation, 29(1), 107–130.
- Rollnick, S., Heather, N., Gold, R., & Hall, W. (1992). Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Addiction, 87(5), 743–754. https://doi.org/10.1111/j.1360-0443.1992.tb02720.x
- Rowlands, L., Coetzer, R., & Turnbull, O. (2021). This time it’s personal: Reappraisal after acquired brain injury. Cognition and Emotion, 35(2), 305–323. https://doi.org/10.1080/02699931.2020.1839384
- Rowlands, L., Coetzer, R., & Turnbull, O. H. (2020). Good things better? Reappraisal and discrete emotions in acquired brain injury. Neuropsychological Rehabilitation, 30(10), 1947–1975. https://doi.org/10.1080/09602011.2019.1620788
- Roy, D., Vaishnavi, S., Han, D., & Rao, V. (2017). Correlates and prevalence of aggression at six months and one year after first-time traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 29(4), 334–342. https://doi.org/10.1176/appi.neuropsych.16050088
- Saban, K. L., Griffin, J. M., Urban, A., Janusek, M. A., Pape, T. L. B., & Collins, E. (2016). Perceived health, caregiver burden, and quality of life in women partners providing care to veterans with traumatic brain injury. Journal of Rehabilitation Research and Development, 53(6), 681–692. https://doi.org/10.1682/JRRD.2015.07.0143
- Saban, K. L., Hogan, N. S., Hogan, T. P., & Pape, T. L. B. (2015). He looks normal but…challenges of family caregivers of veterans diagnosed with a traumatic brain injury. Rehabilitation Nursing, 40(5), 277–285. https://doi.org/10.1002/rnj.182
- Salas, C. E., Radovic, D., & Turnbull, O. H. (2012). Inside-out: comparing internally generated and externally generated basic emotions. Emotion (Washington, D.C.), 12(3), 568–578. 10.1037/a0025811 22023364
- Salas Riquelme, C. E., Radovic, D., Castro, O., & Turnbull, O. H. (2015). Internally and externally generated emotions in people with acquired brain injury: Preservation of emotional experience after right hemisphere lesions. Frontiers in Psychology, 6, 1–9. https://doi.org/10.3389/fpsyg.2015.00101
- Salas, C. E., Gross, J. J., Rafal, R. D., Viñas-Guasch, N., & Turnbull, O. H. (2013). Concrete behaviour and reappraisal deficits after a left frontal stroke: A case study. Neuropsychological Rehabilitation, 23(4), 467–500. https://doi.org/10.1080/09602011.2013.784709
- Salas, C. E., Gross, J. J., & Turnbull, O. H. (2014). Reappraisal generation after acquired brain damage: The role of laterality and cognitive control. Frontiers in Psychology, 5, 1–10. https://doi.org/10.3389/fpsyg.2014.00242
- Salas, C. E., Gross, J. J., & Turnbull, O. H. (2019). Using the process model to understand emotion regulation changes after brain injury. Psychology & Neuroscience, 12(4), 430–450. https://doi.org/10.1037/pne0000174
- Sander, A. M., Bogner, J., Nick, T. G., Clark, A. N., Corrigan, J. D., & Rozzell, M. (2012). A randomized controlled trial of brief intervention for problem alcohol use in persons with traumatic brain injury. Journal of Head Trauma Rehabilitation, 27(5), 319–330. https://doi.org/10.1097/HTR.0b013e318269838c
- Sassaroli, S., Brambilla, R., Cislaghi, E., Colombo, R., Cislaghi, E., Centorame, F., Veronese, G., Favaretto, E., Fiore, F., Veronese, G., & Ruggiero, G. M. (2015). Emotion-abstraction patterns and cognitive interventions in a single case of standard cognitive-behavioral therapy. Research in Psychotherapy: Psychopathology, Process and Outcome, 17(2), 65–72. https://doi.org/10.4081/ripppo.2014.146
- Schmeichel, B. J., & Tang, D. (2015). Individual differences in executive functioning and their relationship to emotional processes and responses. Current Directions in Psychological Science, 24(2), 93–98. https://doi.org/10.1177/0963721414555178
- Scholten, A. C., Haagsma, J. A., Cnossen, M. C., Olff, M., Van Beeck, E. F., & Polinder, S. (2016). Prevalence of and risk factors for anxiety and depressive disorders after traumatic brain injury: A systematic review. Journal of Neurotrauma, 33(22), 1969–1994. https://doi.org/10.1089/neu.2015.4252
- Spielberger, C. D. (1999). STAXI-2: State-trait anger expression inventory-2. Professional manual. Psychological Assessment Resources.
- Strong, C. A. H., Tiesma, D., & Donders, J. (2010). Criterion validity of the Delis-Kaplan Executive Function System (D-KEFS) fluency subtests after traumatic brain injury. Journal of the International Neuropsychological Society, 17(2), 230–237. https://doi.org/10.1017/S1355617710001451
- Tateno, A., Jorge, R. E., & Robinson, R. G. (2003). Clinical correlates of aggressive behavior after traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 15(2), 155–160. https://doi.org/10.1176/jnp.15.2.155
- Tenforde, A. S., Hefner, J. E., Kodish-Wachs, J. E., Iaccarino, M. A., & Paganoni, S. (2017). Telehealth in physical medicine and rehabilitation: A narrative review. PM&R, 9(5), S51–S58. https://doi.org/10.1016/j.pmrj.2017.02.013
- Tondowski, M., Kovacs, Z., Morin, C., & Turnbull, O. H. (2007). Hemispheric asymmetry and the diversity of emotional experience in anosognosia. Neuropsychoanalysis, 9(1), 67–81. https://doi.org/10.1080/15294145.2007.10773543
- Turnbull, O. H., Evans, C. E. Y., & Owen, V. (2005). Negative emotions and anosognosia. Cortex, 41(1), 67–75. https://doi.org/10.1016/s0010-9452(08)70179-5
- Walker, A. J., Nott, M. T., Doyle, M., Onus, M., McCarthy, K., & Baguley, I. J. (2010). Effectiveness of a group anger management programme after severe traumatic brain injury. Brain Injury, 24(3), 517–524. https://doi.org/10.3109/02699051003601721
- Wechsler, D. (2010). Wechsler Adult Intelligence Scale – Fourth UK edition (WAIS-IV UK) administration manual. Pearson.
- Williamson, P., Day, A., Howells, K., Bubner, S., & Jauncey, S. (2003). Assessing offender readiness to change problems with anger. Psychology, Crime & Law, 9(4), 295–307. https://doi.org/10.1080/1068316031000073371
- Witten, J. A., Coetzer, R., & Turnbull, O. H. (2022). Shades of rage: Applying the process model of emotion regulation to managing anger after brain injury. Frontiers in Psychology.
- World Health Organization. (1996). Geneva, Switzerland.
- Yasmin, N., & Riley, G. A. (2022). Are spousal partner perceptions of continuity and discontinuity within the relationship linked to the symptoms of acquired brain injury? Disability and Rehabilitation, 44(16), 4249–4256. https://doi.org/10.1080/09638288.2021.1900410
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x