Abstract
West Africa’s Ebola epidemic of 2014–2016 exposed, among other problems, the under-funding of transnational global health activities known as global common goods for health (CGH), global functions such as pandemic preparedness and research and development (R&D) for neglected diseases. To mobilize sustainable funding for global CGH, it is critical first to understand existing financing flowing to different types of global CGH. In this study, we estimate trends in international spending for global CGH in 2013, 2015, and 2017, encompassing the era before and after the Ebola epidemic. We use a measure of international funding that combines official development assistance (ODA) for health with additional international spending on R&D for diseases of poverty, a measure called ODA+. We classify ODA+ into funding for three global functions—provision of global public goods, management of cross-border externalities, and fostering of global health leadership and stewardship—and country-specific aid. International funding for global functions increased between 2013 and 2015 by $1.4 billion to a total of $7.3 billion in 2015. It then declined to $7.0 billion in 2017, accounting for 24% of all ODA+ in 2017. These findings provide empirical evidence of the reactive nature of international funders for global CGH. While international funders increased funding for global functions in response to the Ebola outbreak, they failed to sustain that funding. To meet future global health challenges proactively, international funders should allocate more funding for global functions.
Introduction
Since the West African Ebola epidemic of 2014–2016, the international health and development community has become intensely aware that a number of crucial transnational global health activities have been under-funded. In previous research, we used the term “global functions” to refer to these activities.Citation1 This term has the same meaning as “global common goods for health” (global CGH), the terminology employed in this special issue of Health Systems and Reform on financing common goods for health. Global CGH address health challenges that go beyond the boundaries of individual nation states—such as pandemics, antimicrobial resistance (AMR), and the cross-border spread of non-communicable disease risk factors—and they reap transnational (regional or global) health benefits. Yamey and colleagues have described how the 2014–2016 Ebola epidemic exposed the relative neglect of several global CGH.Citation2 For example, under-funding of product development for neglected and emerging infectious diseases of poverty meant that no disease-specific control tools were available (i.e., there was no Ebola vaccine, therapeutic, or rapid diagnostic test), while regional surveillance systems under-performed.
Over the last five years, several new initiatives have emerged to mobilize attention to and funding for global CGH. In the wake of the Ebola outbreak, for example, the Coalition for Epidemic Preparedness Innovations (CEPI) was launched to mobilize new financing to develop vaccines for epidemic diseases.Citation3 Under Germany’s presidency of the G20, in 2017 a new Global AMR Research and Development (R&D) Hub was launched to “improve the coordination of international efforts and initiatives to tackle AMR while further increasing investments into R&D for AMR.”Citation4 The new Global Action Plan for Healthy Lives and Wellbeing for All, which is supported by twelve multilateral health and development agencies, identifies seven cross-cutting areas (called “accelerators”) for intensified collaboration to accelerate progress, including several global CGH.Citation5 Global public goods are also one of the pillars of the World Health Organization’s 13th General Programme of Work for 2019–2023.Citation6
In order to foster sustainable financing modalities for global CGH, it is critical to estimate existing financing flows to different types of global CGH. To the best of our knowledge, only one comprehensive study, published in 2015, has estimated the amount of international funding for health that targets global CGH. In this study, Schäferhoff and colleagues analyzed international funding in a single year 2013.Citation1 They used two major data sources. First, they obtained data on official development assistance (ODA) from the Creditor Reporting System (CRS) database of the Organisation for Economic Cooperation and Development (OECD)’s Development Assistance Committee (DAC).Citation7 Second, they obtained data on funding for neglected disease product development from the Global Funding for Innovation for Neglected Diseases (G-FINDER) database.Citation8 Using a taxonomy developed by The Lancet Commission on Investing in Health (CIH),Citation9 Schäferhoff and colleagues classified international funding for health into two broad types:
Funding for global functions: These are functions “characterized by their ability to address transnational issues.”Citation1,Citation10 Global functions can be further categorized into three areas: (i) provision of global public goods (e.g., R&D for health tools, and knowledge generation and sharing); (ii) fostering of global health leadership and stewardship (e.g., global health advocacy and priority setting, and promoting aid effectiveness); and, (iii) management of negative regional and global cross-border externalities (e.g., pandemic preparedness, and control of AMR). shows how the CIH’s term global functions relates to the global CGH terminology used in this special issue.
Funding for country-specific functions: This refers to funding given to an individual country to support disease control activities (e.g., reducing maternal mortality) that will benefit that country alone. Jamison and colleagues have defined country-specific functions as activities that tackle “time-limited problems within individual countries that justify international collective action because of highly constrained national capacity.”Citation10
TABLE 1. How the Term “Common Goods for Health” Relates to the Term "Global Functions”
Schäferhoff et al. had expanded the traditional definition of ODA by adding additional public spending on product development for neglected diseases that is not reported to the OECD DAC. They called their expanded topic “health official development assistance plus” (ODA+) and argued that “it provides a more comprehensive picture of donor support for health.”Citation1
The study found that in 2013, only about one fifth of all international spending for health ($4.7 billion out of a total of $22 billion) was directed at global functions. The results, argued the authors, provided “a baseline of current support for global versus country-specific functions that could help inform discussions on the optimum levels of such funding.”
Has the recent rise in attention to global CGH been accompanied by increased funding for such goods? In this study, which the World Health Organization (WHO) commissioned to inform this special issue, we set out to answer this question. Using a new methodological approach, we conduct for the first time a time series analysis to examine trends in funding for global CGH in the years 2013, 2015, and 2017.
Methodology
Analytical Framework
Our study tracked international funding for the three global functions suggested by the CIH versus country-specific funding. We further classified international funding for the three main categories of global functions into 11 sub-functions ().
TABLE 2. Categorization of Health ODA+ into Global and Country-Specific Functions
For research and development (R&D) for health tools, which is a sub-function of supplying global public goods (GPGs), we included product development for poverty-related and neglected diseases (as defined by G-FINDER.Citation8) These include: HIV/AIDS, tuberculosis, malaria, neglected tropical diseases (e.g., helminth infections), pneumonia, and diarrhea. While R&D for other diseases could also be considered a GPG, we narrowed our scope to poverty-related and neglected diseases for two reasons. First, annual funding for these diseases is very well documented in the G-FINDER surveys, which use a replicable and validated methodology, allowing year-by-year trend analysis. The second reason is the “limited purchasing power of both governments and patients in the countries where such diseases predominate; unlike for other diseases, there is no positive spillover from drug development targeted at more affluent markets.”Citation11,Citation12
In the category of managing negative regional and global cross-border externalities, we included some activities that deliver personal services to individual patients, such as treatment of drug-resistant tuberculosis (TB) and efforts to eliminate malaria and eradicate polio. Although the term global CGH as used in this special issue generally refers to population-based functions or interventions requiring collective financing, we consider personal services to address drug-resistant TB, or which contribute to the elimination of malaria or eradication of polio, to have clear benefits in controlling negative regional and global externalities. Thus is why we consider them to be global CGH. This is aligned with findings from the CIH and The Lancet Commission on Tuberculosis.Citation9,Citation13
As discussed by Yamey et al.,Citation2 while the benefits of supporting global functions are transnational, these investments can be made at different levels:
The global and regional level: Financial support for global functions can be channeled into global institutions. One example is a global vaccine stockpile, such as the stockpile of oral cholera vaccine established by WHO.Citation14 An example of financing global functions at the regional level is the Coalition for African Research and Innovation, a regional research and development platform.Citation15
Within low-income countries (LICs) and middle-income countries (MICs): In-country spending is another important way to support global functions. Examples include international funding to individual LICs and MICs to tackle drug-resistant TB, eradicate polio, or conduct pandemic preparedness activities.
Within the home country of the international funder: ODA+ includes all funding for product development for neglected diseases regardless of where it is spent. Because there is urgent need for new tools to control diseases that disproportionally affect people in low- and middle-income countries, in line with G-FINDER’s approach, we include funds that are channeled through research institutions within the home countries of R&D funders (e.g. funding for the development of an HIV vaccine channeled by the US government through the National Institutes of Health; see Appendix A1).
In this paper, we discuss how ODA+ is distributed across these levels. One implication of these different levels of investment is that some global CGH are both national and global. For example, international investments in a LIC’s outbreak surveillance system have both national and transnational benefits, and would be included as an example of a global CGH or global function in our study. In contrast, international investments into a LIC’s maternal mortality surveillance system has only national benefits and would be classified as a country-specific investment.
Data Sources
The first key source of data we used to assess funding flows to global functions was the OECD DAC’s CRS, which is based on official data reported by donor agencies (labeled as international funders for the purposes of this paper). The CRS covers both bilateral and multilateral outflows and includes data provided by 30 DAC donor countries, 20 non-DAC donor countries, and 46 multilateral funders.Citation16,Citation17 Although technically classified as private flows, the CRS also includes funding from the Bill & Melinda Gates Foundation; we thus included it in our analysis as well. The CRS also provides information about ODA recipients (a total of 143 eligible recipient countries).Citation18
We assessed three CRS purpose codes for “aid to health”: “health, general (purpose code 121),” “basic health (purpose code 122),” and “population policies/programmes and reproductive health (purpose code 130).” We also assessed purpose code 16064 (“social mitigation of HIV”). In addition, we conducted an assessment of humanitarian aid purpose codes (72010, 72040, 72050, 73010, and 74010) to investigate whether they included additional funding for epidemic and pandemic preparedness and response. Project descriptions of humanitarian aid projects are often weaker compared to those under the health purpose codes and are therefore more difficult to assess. Ultimately, we have taken a conservative approach and report separately on the results from the humanitarian purpose codes to not overinflate our findings.
In order to examine time trends in international funding for global functions, we assessed health ODA disbursements for the years 2013, 2015, and 2017 (US Dollars, constant 2017 prices). We used the April 9, 2019 update of the CRS and downloaded the data on June 11, 2019.
The second key source of data was survey data from G-FINDER, which tracks spending on product development for 33 poverty-related and neglected diseases (PRNDs), including all relevant product types and basic research on PRNDs.Citation8 Some funding in the G-FINDER database is also reported by international funders to the OECD DAC and is thus included in the CRS. To avoid double-counting, we extracted R&D for PRNDs from the CRS. Our assessment includes all G-FINDER funding by all countries reporting to the DAC and funding by the Bill & Melinda Gates Foundation (which together account for about 80% of all funding included in the G-FINDER in 2013–2017). We did not include funding for R&D on neglected diseases by either the private sector or low- and middle-income countries (Appendix A1 gives further details on what was included in our definition of health ODA+).
Approach
We downloaded all projects (“aid activities”) from the CRS for the years 2013, 2015, and 2017. In total, there were 84,011 health projects in these three years. In addition, there were 37,910 humanitarian aid projects for the three years. We analyzed the projects in two steps: (1) a keyword search to identify projects that potentially supported global functions; and, (2) a manual coding exercise to qualitatively analyze and confirm which projects supported global functions and identify the primary sub-function.
For our first step, we used a keyword search to assess the 84,011 health projects and 37,910 humanitarian aid projects in order to identify those aid projects that potentially supported global functions. CRS keyword searches are a common strategy to analyze financing for specific health areas.Citation19-Citation21 For each of the 11 sub-functions of global functions (see ), we established a list of keywords (shown in Appendix A2) and translated the keywords into seven languages. Using these keywords, we searched the CRS database to identify those aid projects that potentially provided funding for global functions. We identified 21,172 health projects with keywords related to global functions. In other words, approximately 25% of all health projects in the years 2013, 2015, and 2017 potentially supported global functions. In addition, the search identified 3,507 humanitarian aid projects (9%) that potentially supported epidemic and pandemic preparedness.
As our second step, we manually coded the 21,172 CRS projects that potentially supported global functions to assign them among the three different categories of global functions and 11 sub-functions. We qualitatively analyzed the information in the CRS, such as project titles, long and short projection descriptions, and channels. Projects were then coded into three categories:
Global functions-targeted: The main metric in this study was global functions-targeted ODA+, defined as funding for projects with the primary objective of supporting global functions. An aid project was classified as “global functions-targeted” if the CRS project information indicated that the project primarily provided funding in support of global functions. If this was the case, the entire project amount counted towards global functions. We then coded the project to a single global function and the main sub-function. (If the project information suggested that the project focused on multiple sub-functions, we only selected the sub-function that was the primary focus. Apportioning project funding across different sub-functions was not feasible due to data limitations in the CRS.)
Global functions-inclusive: In addition to our main metric, we included this second category to account for the fact that a project could partially support global functions, while at the same time fulfilling the specific needs of individual countries (“country-specific support”). We included this “global functions-inclusive” category because our analysis of “global functions-targeted” funding only counted projects that were fully targeted at global functions and might underestimate the amount of financing for global functions when they were combined with other functions. The “global functions-inclusive” funding is the sum of two components: (i) global functions-targeted funding, and (ii) funding from “mixed” projects that provided both funding to global functions and country-specific funding. In other words, our estimate of global functions-inclusive funding included disbursements to projects with either primary or partial support to global functions. In a study on development assistance for adolescent health, Li et al. used a similar strategy to assess to what extent development assistance for health was adolescent-targeted or adolescent-inclusive.Citation19
Country-specific: If a project was entirely in support of individual countries and country-specific in nature, we coded it as “country-specific” support.
The main results presented in the Results section below are largely focused on global functions-targeted and country-specific funding. In the Appendix, we provide more details on the global functions-inclusive funding, which we consider to be a sensitivity analysis to our main findings (Appendix A3).
Our method for estimating financing flows to global functions differed from the method used by Schäferhoff et al.Citation1 in their 2015 analysis, which was based on an in-depth, project-by-project assessment of the CRS database and project-specific data from international funders. As that approach was highly labor-intensive, the original study looked at a relatively small sample of health projects (approximately 1,200 projects) for only one year (2013). The authors then extrapolated from the sample to make assumptions about all projects. In contrast, our new analysis estimates funding for global functions for multiple years. The other methodological advantage of this new study is that we assessed all health projects in the CRS for the targeted years rather than assessing and extrapolating from a sample.
Results
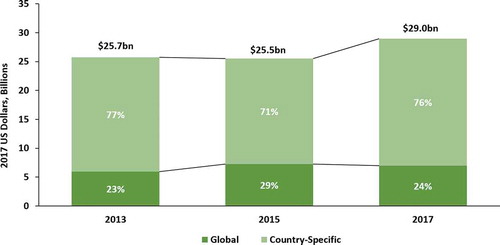
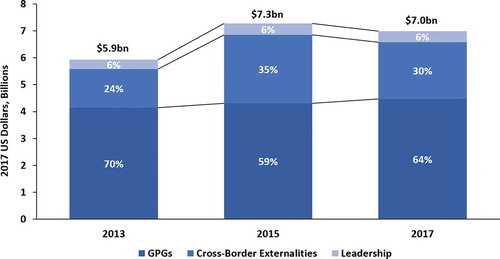
Total ODA+ (i.e., health ODA plus international funding for product development for PRNDs) remained roughly stagnant between 2013 ($25.7 billion) and 2015 ($25.5 billion). It then increased to $29.0 billion in 2017. The significant increase in 2017 was fueled by rises in both health ODA and funding for product development for PRNDs (Appendix 1A).Citation22 The share of ODA+ for global functions out of total ODA+ increased from 23% in 2013 to 29% in 2015. In 2017, the share allocated for global functions decreased to 24% (). The remaining shares in all three years were for country-specific functions (77% in 2013, 71% in 2015, and 76% in 2017). In absolute terms, funding for global functions grew from $5.9 billion in 2013 to $7.3 billion in 2015. In 2017, funding declined to 7.0 billion ().
Spending on GPGs accounted for the largest proportion of total funding for global functions in all three years. Out of all funding for global functions, GPGs accounted for 70% ($4.1 billion) in 2013, 59.3% ($4.3 billion) in 2015, and 64% ($4.4 billion) in 2017 (). In absolute terms, funding for GPGs steadily increased. Funding for the management of cross-border externalities fluctuated substantially. In 2013, 24.1% ($1.4 billion) of all funding for global functions was allocated to cross-border externalities. In 2015, a substantially larger share (35%) of global functions funding went to this category, a total of $2.5 billion. By 2017, this share and the absolute amount had fallen to 30% ($2.1 billion). The share of funding for global health leadership remained relatively stable across the three years, accounting for about 6% of the total.
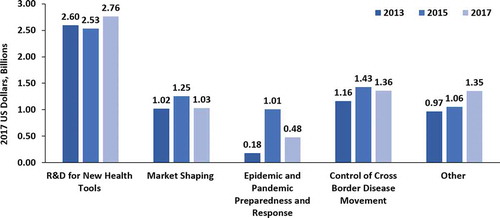
We disaggregated international funding for the three categories of global functions into 11 sub-functions (see above). Product development for PRNDs was the GPG subcategory that received the most international funding, accounting for 59–63% ($2.5–2.8 billion) of all GPG funding in 2013, 2015, and 2017 (; ). International funders also provided substantial funding for knowledge generation and distribution beyond product development. Approximately 10–14% ($431–597 million) of all GPG funding was allocated towards this sub-function across the three years assessed. Market shaping fluctuated, accounting for 25% ($1.0 billion), 29% ($1.2 billion), and 23% ($1.0 billion) in 2013, 2015, and 2017, respectively. Much of this funding came from Gavi, the Vaccine Alliance, which contributes to market shaping through bulk procurement of vaccines. Comparatively little funding was provided by international funders for development of international norms and guidelines (2%) and sharing of intellectual property (<1%).
TABLE 3. Funding for Global Functions by Sub-function, Years 2013, 2015, and 2017
Overall funding for cross-border externalities was more volatile compared to flows for GPGs and leadership. Much of the fluctuation in the total funding flows for managing cross-border externalities was due to fluctuation in funding to the sub-function “epidemic and pandemic preparedness and response.” Funding for this sub-function increased from $201.8 million (14% out of all funding for cross-border externalities) in 2013 to $1.0 billion (40%) in 2015. Most of the 2015 funding was provided by international funders responding to the 2014–2016 Ebola outbreak in West Africa. In 2017, disbursements to this sub-function fell to $477.8 million (26%). The changes in funding levels are even more pronounced when the funding for epidemic and pandemic preparedness reported as humanitarian aid is taken into account. While international funders disbursed a total of $21.9 million in 2013 to epidemic and pandemic preparedness reported under humanitarian aid, this category’s funding increased to $842.4 million in 2015, and then dropped again to $145.0 million in 2017.
Control of cross-border disease movement was the sub-function that accounted for the largest proportion of total funding for the management of cross-border externalities. Funding for this sub-function rose from $1.2 billion (81% of all funding for cross-border externalities) in 2013 to $1.4 billion in 2015 (56%) and remained at $1.4 billion (64%) in 2017. While most of these funds were for polio eradication, there was a notable increase in the number of projects with regional and global focus (88 in 2013 compared to 253 in 2017), including for malaria elimination.
Funding in response to the marketing of unhealthful products accounted for 2–3% of all funding for cross-border externalities in 2013, 2015, and 2017. Funding for projects exclusively targeted at AMR increased from $37.1 million in 2013 (3%) to $147.1 million (7%) in 2017. However, one limitation of our method, which included drug-resistant TB under AMR, is that our estimate on global functions-targeted funding only counts aid projects exclusively focused on multi-drug resistant (MDR) and extensively drug resistant (XDR) TB. Projects that only partially contributed to addressing MDR- or XDR-TB—for example, through the provision of treatment for drug-resistant TB—fell outside our main metric (The Lancet Commission on Tuberculosis faced similar limitations.Citation13) This means that we to some extent underestimate the full amount of funding in response to AMR (see Appendix A3 for more details).
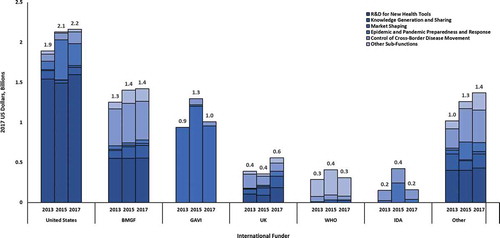
Five international funders provided 78% ($5.5 billion) of the $7.0 billion total funding for global functions in 2017. The US government was the largest international funder ($2.2 billion), followed by the Bill & Melinda Gates Foundation ($1.4 billion), Gavi ($1.0 billion), the United Kingdom ($558.8 million), and WHO ($310.6 million). WHO is included in the CRS database as an international funder of global CGH and a channel; all earmarked bilateral funding channeled through WHO is counted as funding by the bilateral donor. While the use of channels in the CRS ensures that aid from donors to multilaterals is not claimed by both funders (i.e. double-counted), examining WHO as both an international funder and a channel illuminates the important role it plays in organizing and disbursing funding from various sources to support global functions. To fully acknowledge the critical contribution of WHO in the provision of global functions, we also calculated how much funding for global functions is channeled through WHO: a total of $735.4 million in 2017.
International funders focus on different categories of global functions (; ). The Bill & Melinda Gates Foundation has a strong focus on R&D and knowledge generation. Gavi contributes through its market shaping model. The US government is major contributor to product development for PRNDs and also provides substantial support to emergencies and for epidemic and pandemic preparedness. WHO is critical for a range of functions, and is a major channel for polio eradication.
TABLE 4. Funding for Global Functions by Major International Funders and Sub-functions, Years 2013, 2015, and 2017
FIGURE 4. Funding for Global Functions by Major International Funders and Sub-functions, Years 2013, 2015, and 2017
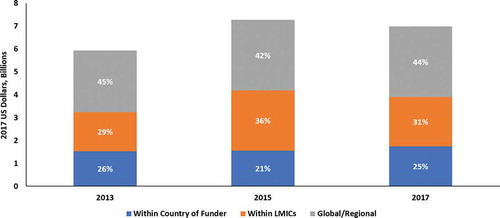
In 2017, 45% of all funding for global functions was allocated at the global and regional levels (). A quarter was spent within the home countries of international funders on R&D for PRNDs. In addition, 31% was spent within low- and middle-income countries, a lower share compared to 2015 (36%). This is also attributable to the Ebola outbreak in West Africa, which led to increased funding for the three countries that were most heavily affected, Guinea, Liberia, and Sierra Leone ().
TABLE 5. Top 10 Low- and Middle-income Country Recipients of Funding for Global Functions, Years 2013, 2015, and 2017 (in USD Millions)
Discussion
This study shows that international funding for global functions, also called global CGH, increased between 2013 and 2015 by $1.35 billion, bringing funding for global functions to a total of $7.3 billion in 2015. In that year, 29% of disbursements to health ODA+ focused on global CGH. In 2017, however, funding for global CGH decreased by $300 million to $7.0 billion, although total ODA+ grew substantially (a $3.5 billion increase) compared to 2015.
In the Global Health 2035 report published in 2013 and then again in its five-year follow-up report published last year,Citation9,Citation23 the CIH called for international funders to “meet the challenges of the next generation” by shifting their funding for health towards CGH over time. The CIH argued that the graduation of middle-income countries from health ODA provides an opportunity to redirect funding towards global CGH. The 2014–2016 Ebola outbreak shone a spotlight on the need to mobilize additional funding for global CGH such as pandemic preparedness and product development for neglected and emerging diseases. Our study suggests that international funders did initially heed the call to step up their investments in global CGH—the increase in international financing for global CGH in 2015 was mostly driven by a substantial increase in international funding for projects classified as epidemic and pandemic preparedness and response, likely in response to Ebola. However, international funders did not sustain this financing.
One interpretation of this finding is that international funders are willing to help contain infectious disease outbreaks. A 2015 analysis of humanitarian assistance for Ebola using the United Nations Office for the Coordination of Humanitarian Affairs financial tracking system found evidence that while “contributions to fight the epidemic were slow to take off,” international funding pledges then rose sharply.Citation24 However, the significant decline in funding for epidemic and pandemic preparedness and response between 2015 and 2017 (a fall of over $500 million, a 50% decline) also shows that international funders continue to behave reactively to events rather than investing in system strengthening that improves the preparedness and resilience of health systems. Our study provides empirical evidence that international funders are prone to “cycles of panic and neglect,” a phrase coined by the International Working Group on Financing Preparedness in its report From Panic and Neglect to Investing in Health Security.Citation25 Our analysis of trends in ODA+ is in line with the notion that there was a “panic” phase in response to the Ebola epidemic in which funding for preparedness efforts rose, followed by a decline in funding during the “neglect” phase.
Our study found an upward trend in annual funding for product development for neglected diseases by international funders reporting to the DAC, from $2.6 billion to $2.8 billion between the years 2013 and 2017. Our analysis only counts funding from international funders that reported to the DAC; if we had added funding from the private sector and low- and middle-income countries, the total annual funding for product development for PRNDs in the year 2017 would even be higher ($3.6 billion). However, although this upward trend is promising, the annual amount still falls far short of R&D funding needs. For example, a recent modeling study by Young et al. estimated that about $6 billion annually would be needed to (a) advance the current pipeline of products under development, and (b) develop key “missing” products that the current pipeline is unlikely to yield (e.g., highly effective vaccines for HIV, TB, malaria, and hepatitis C and a combined vaccine for multiple causes of diarrhea).Citation26 The need for additional funding is particularly acute for late stage (phases IIb and III) clinical trials.
One other important finding merits discussion among policy makers. Achieving the ambitious global health targets in the Sustainable Development Goals clearly requires high-quality research evidence, ideally from large and well-designed studies. In year 2017, there was substantial funding ($597 million) for research and knowledge distribution beyond R&D. At the same time, our study found a large number of research projects (1,500 projects in 2017). However, the quality of study designs and the value of the data that emerge from these studies are often unclear. We believe it would be helpful for WHO, as the overarching global health governance agency, to develop a framework to help rationalize the system of funding research via ODA, including to reduce duplication and inefficiencies likely to result from a multiplicity of small-scale and under-funded efforts.
Overall, our study suggests that international funders have not fully embraced the strategic direction promoted by the CIH. We found that in 2013, 23% of ODA+ was focused on global CGH—this result is similar to the 2015 study from Schäferhoff et al., which found that 21% of ODA+ was for global CGH.Citation1 In absolute terms, our study finds a higher amount for global CGH in 2013 (an additional $1.3 billion) because less R&D funding from G-FINDER was included in the 2015 paper. However, while the absolute amount of funding for global CGH was much higher in 2017 compared to 2013 (about $1.0 billion more), the share of total ODA+ devoted to global functions was similar in 2017 (24%). Former US Treasury Secretary Larry Summers, the chair of the CIH, has argued that “the lack of investment in this global goods agenda is an international emergency”; he has proposed that by 2030 approximately 50% of all international funding for health should be targeted at global CGH.Citation27 In 2030, of course, there will still be many low- and lower-middle-income countries that require international funding in the form of country-specific support, including to help fund a package of essential services (so-called “essential universal health coverage”.Citation22)
In another contribution to this special issue, Yamey and colleagues summarize the best available estimate of the annual price tag for critical global CGH.Citation2 In total, they write, at least an additional $9.5 billion is needed annually, and this is likely a highly conservative number (e.g., it does not include the estimated costs of malaria eradication, which will soon be presented by The Lancet Commission on Malaria Eradication). The trends identified in our study suggest that there will continue to be a large need for funding for years to come. This necessitates establishing more sustainable financing models for global CGH.
Two important questions that recur throughout this special issue on financing CGH are relevant to our study. First, is it possible to spark political interest in CGH among global health funders (principally international agencies, governments of LICs, MICs, and high-income countries, and foundations)? The answer probably depends on whether it is possible to convince funders of the rationale for and importance of investing in CGH. When it comes to global CGH, our study suggests that international funders can be motivated to support certain types of functions, in particular pandemic preparedness (as shown by the rise in funding after the 2014–2016 Ebola outbreak in West Africa) and global health R&D (funding for which rose to its highest-ever level in 2017). However, funding for both of these goods has waxed and waned. It remains unclear how best to motivate long-term and sustained political attention, and how to focus international funders attention on the “most neglected” global CGH.
The second question is: what approaches, strategies, and mechanisms could help establish sustainable financing mechanisms for CGH? While our study focuses on the size and distribution of international funding for CGH, it is also critical to consider how these funds are used. Without well-thought-out funding approaches, the funds will not achieve the envisioned impact. International funders and countries alike should be working proactively to develop effective mechanisms to ensure that funds are effectively channeled and transformed into services and purposes that serve their designated objectives. In this special issue, Sparkes and colleagues lay out a suite of options for financing national CGH,Citation28 and Yamey and colleagues do the same for financing global CGH.Citation1 Several parallels exist between the two lists. For example, in both cases the authors describe the importance of reducing fragmented funding flows and pooling funds for CGH and of strengthening the overarching governance of CGH financing. For global CGH, three broad financing mechanisms need to be further developed:
Resource mobilization mechanisms: These include compulsory mechanisms, such as global taxation (e.g., on airline tickets or financial transactions), voluntary earmarked mechanisms (e.g., CEPI), and reallocation of ODA to global CGH after MICs graduate from direct country support).
Pooling approaches: These include pooled R&D funds and coordination platforms (e.g., the G20 Global AMR Hub).
Strategic purchasing of global CGH: Several multilateral agencies purchase global CGH (e.g., Gavi’s funding for pooled procurement/market shaping).
There are grounds for cautious optimism that multilateral agencies in particular could intensify their collaboration in financing global CGH (the “pooling approach” in the above taxonomy) to contribute to more effective and efficient use of funding. A recent policy analysis found “significant convergence” between four major multilateral health agencies—the World Bank, the Global Fund, Gavi, and WHO—in their strategic approaches to global CGH.Citation29 This convergence is particularly evident in the agencies’ support for: improving the production, quality, and use of health data; pandemic preparedness; and, development of and access to health technologies in both LICs and MICs (including MICs that have graduated from receiving direct county support).
Limitations
There are several limitations to our study. The project descriptions in the CRS can be very basic and lacking in relevant information; as a result we may have missed certain projects in our key term search. The variability in the quality of project descriptions makes it hard to assess if a project is focused on global functions. The key metric used in this paper—spending targeted at global functions—underestimates funding for global functions because it only counts projects that are primarily targeted at global functions. To account for this, we included a “global functions-inclusive funding” category, which captures projects that support a mix of global and country-specific functions (Appendix A3). Third, although we have added the G-FINDER data in an effort to capture investments beyond the CRS, there are likely other investments in support of global functions that are not captured by either database. This includes, for instance, non-ODA financing from public research institutions on AMR, epidemic and pandemic preparedness, and NCDs. Future analyses should attempt to capture these investments.
Conclusions
To the best of our knowledge, this study is the first to have estimated financing for global functions—global CGH in the terminology used in this special issue—over time. We found that in absolute terms the overall amount of funding for global CGH rose from 2013 to 2017.
In 2013, the CIH argued that global health funders have been under-investing in global CGH. Six years later, many critical CGH remain underfunded.Citation2 Unless international funders further ramp up their support for global health—and establish sustainable financing to ensure ongoing, timely and appropriate levels of funding—existing health ODA should be reallocated towards global CGH. This reallocation can be achieved over time by redirecting country-specific funding from countries that become able to provide their own resources. Additionally, funding within countries can be redirected from routine disease control or health system strengthening to areas like pandemic preparedness and AMR control that have benefits extending beyond individual countries’ borders.
We recognize, of course, that many LICs—particularly fragile and post-conflict nations—will need country-specific health ODA for years to come. Nevertheless, as Richard Horton, editor of The Lancet, recently noted, “Two-thirds of the poor live in middle-income countries.” New aid approaches are needed to tackle the problem of poverty-related ill health in MICs.Citation30 Other researchers have proposed alternate approaches to allocating ODA to health. For example, Dieleman and colleagues suggest that to tackle the problem of poverty-related morbidity and mortality in MICs, ODA for health could be allocated based on the absolute size of populations living in poverty.Citation31 This approach would mean an increase in country-specific support to large MICs such as Brazil, China, and India. We argue for a different approach to improving the health of poor people in MICs: greater support for global CGH, such as market shaping and pooled procurement that would bring down the prices of medicines and vaccines, and R&D to develop and deliver new health tools.
Moving forward, it is also critical that international funders proactively invest in country preparedness, rather than only providing funding reactively after outbreaks occurred. The international funding community should break the vicious cycle of panic followed by neglect. It appears that we are now—again—in a phase of neglect, leaving the world highly vulnerable to massive loss of life and economic shocks from natural or human-made epidemics and pandemics. Finally, we recommend including our model for tracking into WHO’s national health accounts (NHAs) system. As our analysis produces policy-relevant data, institutionalizing the tracking of funding for CGH through an NHA subaccount would be an important step going forward.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Supplemental Material
Download MS Word (85.1 KB)Supplemental data
Supplemental data for this article can be accessed on the publisher’s website. All appendices mentioned in the text are available in the supplemental data.
Additional information
Funding
References
- Schäferhoff M, Fewer S, Kraus J, Richter E, Summers LH, Sunderwall J, Yamey G, Jamison DT. How much donor financing for health is channeled to global versus country-specific functions? Lancet. 2015;386:2436–41. PMID: 26178405. doi:10.1016/S0140-6736(15)61161-8.
- Yamey G, Jamison DT, Hanssen O, Soucat A. Financing global common goods for health: when the world is a country. Health Syst Reform. 2019;5(4):334–349.
- Bassett H. CEPI: a new approach to epidemic preparedness. Washington (DC): Sabin Vaccine Institute; 2017 Jun16 [accessed 2019 Jul 5]. https://www.sabin.org/updates/blog/cepi-new-approach-epidemic-preparedness.
- German Federal Ministry of Education and Research. Global AMR R&D hub. Berlin (Germany): Federal Ministry of Education and Research; [accessed 2019 Jul 5]. https://www.gesundheitsforschung-bmbf.de/en/GlobalAMRHub.php.
- World Health Organization. Global action plan for healthy lives and well-being for all. Geneva (Switzerland): World Health Organization; 2019 [accessed 2019 Jul 5]. https://www.who.int/sdg/global-action-plan.
- World Health Organization. Thirteenth general programme of work 2019−2023. Geneva (Switzerland): World Health Organization; 2018 May16 [accessed 2019 Jul 5]. https://www.who.int/about/what-we-do/thirteenth-general-programme-of-work-2019-2023.
- Organisation for Economic Co-operation and Development. Creditor reporting system (CRS). Paris (France): Organisation for Economic Co-operation and Development; 2019 Apr9 [accessed 2019 Jul 5]. https://stats.oecd.org/Index.aspx?DataSetCode=crs1.
- Policy Cures Research. G-FINDER public search tool. Sydney (Australia): Policy Cures Research; 2017 [accessed 2019 Jul 5]. https://gfinder.policycuresresearch.org/PublicSearchTool/.
- Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, Bustreo F, Evans D, Feachem RG, Frenk J, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382(9908):1898–955. PMID: 24309475. doi:10.1016/S0140-6736(13)62105-4.
- Jamison DT, Frenk J, Knaul F. International collective action in health: objectives, functions, and rationale. Lancet. 1998;351:514–17. PMID: 9482466. doi:10.1016/S0140-6736(97)11451-9.
- World Health Organization, World Intellectual Property Organization, World Trade Organization. Chapter 3—medical technologies: the innovation dimension. In: WHO, WIPO, WTO, editors. Promoting access to medical technologies and innovation: intersections between public health, intellectual property and trade. Geneva (Switzerland): WHO, WIPO, WTO; 2012. p. 100–41.
- Moon S, Røttingen J-A, Frenk J. Global public goods for health: weaknesses and opportunities in the global health system. Health Econ Policy Law. 2017;12:195–205. doi:10.1017/S1744133116000451.
- Reid M, Arinaminpathy N, Bloom A, Bloom B, Boehme C, Chaisson R, Chin D, Churchyard G, Cox H, Ditio L, et al. Building a tuberculosis-free world: the Lancet commission on tuberculosis. Lancet. 2019 Mar 20. PMID: 30904263. doi:10.1016/S0140-6736(19)30024-8.
- Yen C, Hyde T, Costa A, Fernandez K, Tam J, Hugonnet S, Huvos A, Duclos P, Dietz V, Burkholder B. The development of global vaccine stockpiles. Lancet Inf Dis. 2015;15:340–47. PMID: 25661473. doi:10.1016/S1473-3099(14)70999-5.
- African Academy of Sciences. Coalition for African research and innovation (CARI). Nairobi (Kenya): Alliance for Accelerating Excellence of Science in Africa; 2017 [accessed 2019 Jul 5]. https://aesa.ac.ke/cari/coalition-for-african-research-and-innovation/.
- Organisation for Economic Co-operation and Development. DAC data submitters. Paris (France): Organisation for Economic Co-operation and Development; 2019 [accessed 2019 Jul 5]. http://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/dacdatasubmitters.htm.
- Organisation for Economic Co-operation and Development. Technical guide to terms and data in the creditor reporting system (CRS) aid activities database. Paris (France): Organisation for Economic Co-operation and Development; 2019 [accessed 2019 Jul 5]. http://www.oecd.org/development/financing-sustainable-development/development-finance-standards/crsguide.htm.
- Organisation for Economic Co-operation and Development. DAC list of ODA recipients. Paris (France): Organisation for Economic Co-operation and Development; 2019 [accessed 2019 Jul 5]. http://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/DAC_List_ODA_Recipients2018to2020_flows_En.pdf.
- Li Z, Li M, Patton GC, Lu C. Global development assistance for adolescent health from 2003 to 2015. JAMA Network Open. 2018;1(4):e181072. PMID: 30646101. doi:10.1001/jamanetworkopen.2018.1072.
- Pitt C, Lawn JE, Ranganathan M, Mills A, Hanson K. Donor funding for newborn survival: an analysis of donor reported data, 2002–2010. PLoS Med. 2012;9(10):e1001332. PMID: 23118619. doi:10.1371/journal.pmed.1001332.
- Dieleman JL, Schneider MT, Haakenstad A, Singh L, Sadat N, Birger M, Reynolds A, Templin T, Hamavid H, Chapin S, et al. Development assistance for health: past trends, associations, and the future of international financial flows for health. Lancet. 2016;387(10037):2536–44. PMID: 27086170. doi:10.1016/S0140-6736(16)30168-4.
- Schäferhoff M, Martinez S, Ogbuoji O, Sabin ML, Yamey G. Trends in global health financing. BMJ. 2019;365:I2185. PMID: 31109918. doi:10.1136/bmj.l2185.
- Watkins D, Yamey G, Schäferhoff M, Adeyi O, Alleyne G, Alawan A, Berkley S, Feachem R, Frenk J, Ghosh G, et al. Alma-Ata at 40 years: reflections from the Lancet commission on investing in health. Lancet. 2018;392:1434–60. PMID: 30343859. doi:10.1016/S0140-6736(18)32389-4.
- Grépin K. International donations to the Ebola virus outbreak: too little, too late? BMJ. 2015;350:h376. PMID: 25649057. doi:10.1136/bmj.h376.
- International working group on financing preparedness. From panic and neglect to investing in health security. Washington (DC): World Bank; 2017 Dec [accessed 2019 Jul 5]. pubdocs.worldbank.org/en/890291523304595565/FINAL-IWG-Report-3-5-18.pdf.
- Young R, Bekele T, Gunn A, Chapman N, Chowdhary V, Corrigan K, Dahora L, Martinez S, Permar S, Persson J, et al. Developing new health technologies for neglected diseases: a pipeline portfolio review and cost model. Gates Open Res. 2018;2:23. PMID: 30234193. doi:10.12688/gatesopenres.12817.1.
- Summers L. The future of aid for health. Presented at: the World Innovation Summit for Health; 2016 Nov 30; Doha, Qatar [accessed 2019 Jul 5]. http://larrysummers.com/wp-content/uploads/2016/11/Doha-LHS-Speech.pdf.
- Sparkes S, Kutzin J, Earle A. Financing common goods for health: a country agenda. Health Syst Reform. 2019;5(4):322–333.
- Yamey G, Kennedy K, Kaus J, Petitjean H, Schrade C, Fewer S, Beyeler N, Schwalbe N. Intensified multilateral cooperation on global public goods for health: three opportunities for collective action. Durham (NC): Center for Policy Impact in Global Health; 2018 Nov [accessed 2019 Jul 5]. http://centerforpolicyimpact.org/wp-content/uploads/sites/18/2018/11/Multilaterals-and-GPGs_LONG_Final.pdf.
- Horton R. Offline: global health’s indifference to poverty must end. Lancet. 2019;394(10195):286. doi:10.1016/S0140-6736(19)31710-6.
- Dieleman JL, Cowling K, Agyepong IA, Alkenbrack S, Bollyky TJ, Bump JB, Chen CS, Grépin KA, Haakenstad A, Harle AC, et al. The G20 and development assistance for health: historical trends and crucial questions to inform a new era. Lancet. 2019;394:173–83. doi:10.1016/S0140-6736(19)31333-9.