ABSTRACT
In 2013, the Government of The Gambia implemented a novel results-based financing (RBF) intervention designed to improve maternal and child nutrition and health through a combination of community, facility and individual incentives. In a mixed-methods study, we used a randomized 2 × 2 study design to measure these interventions’ impact on the uptake of priority maternal health services, hygiene and sanitation. Conditional cash transfers to individuals were bundled with facility results-based payments. Community groups received incentive payments conditional on completion of locally-designed health projects. Randomization occurred separately at health facility and community levels. Our model pools baseline, midline and endline exposure data to identify evidence of the interventions’ impact in isolation or combination. Multivariable linear regression models were estimated. A qualitative study was embedded, with data thematically analyzed. We analyzed 5,927 household surveys: 1,939 baseline, 1,951 midline, and 2,037 endline. On average, community group interventions increased skilled deliveries by 11 percentage points, while the facility interventions package increased them by seven percentage points. No impact was found, either in the community group or facility intervention package arms on early ANC. The community group intervention led to 49, 43 and 48 percentage point increases in handwashing stations, soaps at station and water at station, respectively. No impact was found on improved sanitation facilities. The qualitative data help understand factors underlying these changes. No interaction was found between the community and facility interventions. Where demand-side barriers predominate and community governance structures exist, community group RBF interventions may be more effective than facility designs.
Introduction
Results-based financing (RBF) has been used to increase coverage and quality of health services and maximize the impact of available funding. Its defining characteristic is that payments within the health system are issued only when pre-determined health-related results are achieved. Within maternal and child health (MCH), RBF is seen by some as a potentially effective tool for improving health system performance, but evidence remains mixed.Citation1–5 These inconsistent findings suggest that RBF is not monolithic.Citation6 The details of what is done to incentivize different stakeholders and how it is done are critical to shaping outcomes, as are factors relating to the health system and larger socio-political and cultural contexts in which an RBF intervention is staged.Citation7
The Government of The Gambia knew about RBF projects in other low-income settings experiencing similar challenges with regard to the health system including low uptake of services, shortages of medicines and supplies, and dilapidated infrastructure. In 2013, with support from the World Bank Health Results Innovation Trust Fund, they decided to pilot a novel RBF intervention to improve maternal and child nutrition and health. In addition to providing RBF incentives to health facilities, the program included a conditional cash transfer (CCT) disbursed to pregnant women for antenatal care (ANC) attendance and provided incentive payments to community groups for achieving relevant community-level targets, including around water, sanitation and hygiene (WASH). By incentivizing individuals, health facilities and communities, the intervention aimed to achieve more effective progress toward national MCH goals.
We carried out a mixed-methods study to assess the impact of these interventions on the uptake of targeted health services and behaviors. Our findings contribute to understanding how to design RBF interventions to inform policy to help maximize improvements in health system performance.
Materials and Methods
Study Setting
The Gambia, a small West African country, has a population of approximately 2.4 million.Citation8 When the RBF project was being designed in 2013, the country ranked 172 out of 187 countries in the Human Development Index and more than half of the population was living below the poverty line (US$1.25 /day).Citation9 Nearly 75% of the population relied on agriculture for income. Schooling was limited and literacy rates were low, particularly among women.Citation10 In comparison to many neighboring countries, The Gambia had a high fertility rate, and a young population, with 64% under the age of 24 and a life expectancy at birth of 60 years.Citation8
Although The Gambia achieved early success with a strong primary health program instituted following the 1978 Alma-Ata Conference,Citation11 the country was facing substantial health challenges. At the time of the intervention design, progress on a number of key indicators, including skilled delivery and management of childhood illnesses, had stagnated. Meanwhile, ANC uptake, neonatal tetanus inoculation, contraceptive prevalence rate, and malnutrition interventions had all declined.Citation10,Citation12 Maternal mortality was high, estimated at 291 deaths per 100,000 live births,Citation8 while institutional delivery remained low. In 2013, 63% of women gave birth at a health facility, up only seven percentage points from 2000–2005 despite targeted efforts to increase skilled birth attendance during this time.Citation10,Citation13 ANC and delivery services were free, although the costs of transportation and food at facilities remained a barrier. Women in The Gambia are generally disadvantaged in terms of income. Although many engage in small-scale income-generating activities, financial barriers continue to limit timely uptake of services.
In 2015, the intervention was introduced in three of the country’s five regions, covering approximately one-third of the country’s population and selected based on poor health indicators: the Central River, North Bank West, and Upper River Regions. The regions are sparsely populated and home to approximately 800 mostly rural communities, each with 1–3,000 inhabitants. This population is served by 22 health centers (some ‘major’ and some ‘minor’Footnotea) and two hospitals. Each health center has a non-overlapping catchment area of 20–40 communities. Complex and emergency care is generally provided by the two hospitals.
Intervention
Based on the idea that desired changes in maternal and child nutrition and health outcomes could best be achieved if provider, individual and community behaviors could be improved, complementary interventions were developed for implementation in facilities and communities. The intervention’s conceptual framework has been published previously.Citation14
Facility Intervention Package
Designed to improve the availability, accessibility and quality of care, the facility package included two distinct interventions: payments to health facilities for delivering specified maternal and child nutrition and health services, and CCTs to individual women for timely use of ANC. RBF payments were issued quarterly based on the quantity of each targeted service reportedly provided. Quarterly payments could be increased by up to 50% for compliance with quality standards, or reduced in cases of inaccurate reporting. Health facilities could use 60% of these quarterly payments to finance materials and equipment, training, consulting services, operating costs and 40% for staff bonuses.
The facility intervention package was provided at all health centers and two hospitals in the study regions. Throughout the intervention, the average quarterly RBF payments received were, $44,395 USD for a hospital, $13,325 USD for a major health center and $10,092 USD for a minor health center. This was over and above other support which included, for all facilities, provision of medicines and supplies, and, for hospitals, also a government subvention and income from user fees. Without the RBF incentive payments, health centers had no income over which they had control. The average quarterly income for health workers ranged from approximately $210 USD to $488 USD based on factors including seniority and length of service.
Health facilities also oversaw the issuance of CCTs to pregnant women, which were designed to facilitate access to health services and help toward costs associated with pregnancy and delivery. Women were eligible for two CCTs, each one of approximately $3.50 USD. The first payment was for attending early ANC, defined as an initial ANC visit in the first 12 weeks of pregnancy. Women attending early ANC could receive a second payment if they attended at least three additional ANC visits during the pregnancy. Although often considered a community intervention, because health facilities managed the CCT program, it was included in the facility intervention package; we cannot separate out the impact of the CCTs from the facility RBF payments.
Community Group Intervention
A sub-set of communities participated in the community group intervention. In each, contracts were established with local administrative structures known as Village Development Committees (VDCs) and a VDC sub-committee called the Village Support Group (VSG). The VDC is the local governance body common to communities across the country; with no regular funding, they mobilize resources to fund specific projects. VSGs are responsible for promoting health and nutrition within communities.
The community group intervention offered quarterly incentive payments to VDCs and VSGs for jointly achieving agreed benchmarks related to health-enhancing behaviors. Eighty percent of each payment was allocated to the VDC, and 20% to the VSG. VDCs were charged with engaging their constituencies to decide which community development activities should be financed with the money received. VSGs were asked to carry out social and behavioral change communication (SBCC) activities intended to increase knowledge and awareness of pregnancy, labor and delivery, and to promote institutional delivery and good hygiene practices. The VSGs’ portion of the payments was given to individual members as compensation for the time they spent on project activities. The average quarterly payment varied by community size with small communities receiving $1,031 USD, medium-sized communities receiving $1,313 USD and large communities receiving $2,225 USD.
Prerequisites for participation in the community intervention included the preexistence of an established VDC, being classified as a Primary Health Care Village, and participation in the Baby-Friendly Community Initiative (BFCI). The latter two requirements are initiatives undertaken by the country’s health agencies and ensured a minimum size (400 people) and the availability of a trained village health worker and Community Birth Companion (formerly ‘Traditional Birth Attendant’). Of approximately 800 communities in the project area, 298 were eligible at the time the program launched and 224 were randomly selected for phased-in inclusion.
Incentivized Indicators
Indicators to be incentivized were selected through review of existing data, and consultations with health facility staff and community members. Further detail on the incentivized indicators and payment calculations are in the Supplemental Material.
Intervention Implementation
Pilot and Main Study
The National Nutrition Agency and Ministry of Health and Social Welfare led implementation in collaboration with Regional Health Directorates, health facilities and communities. To test payment levels and oversight mechanisms, a one-year pilot was conducted at three health centers and ten surrounding communities between December 2013 and December 2014. Activities in the pilot areas continued after the launch of the main intervention in 2015.
This evaluation focuses on the 19 remaining health centers in the three regions and their catchment areas. For these areas, the timing of the RBF program was randomly determined through two separate processes.
Facility Randomization
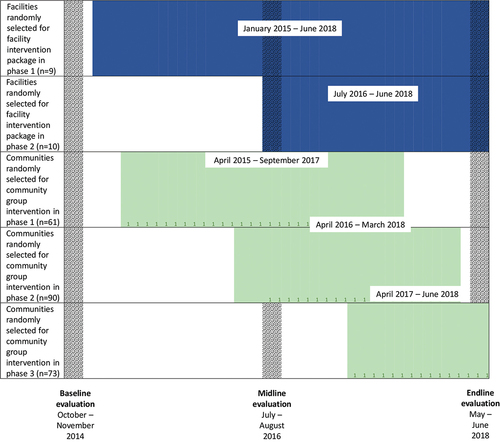
Randomization at the facility level was carried out through a national-level public selection ceremony organized in cooperation with the Ministry of Health and Social Welfare. Fifty percent of facilities in each region were randomly chosen for the RBF intervention in the first phase, launched in January 2015. The remaining facilities launched the intervention in July 2016.
Community Randomization
Similar public ceremonies were used at the community level. 61 communities were randomly selected to receive the community intervention in the first phase, 90 for the second, and 73 communities for the last phase, launched in April 2015, July 2016, and April 2017, respectively. All community programs were designed to be temporary, with Phases 1 and 2 ending before the intervention end date, so as to encourage sustainability after the initial investment.
summarizes the timeline of the interventions as well as the evaluation rollout.
Research Design
We used a 2 × 2 study design to measure the impact of three intervention arms: the facility package arm (including facility RBF payments and CCTs for women), the community group arm, and the combination of facility package and community group arm.
Sample Selection and Quantitative Data Collection
The impact evaluation included all 19 health centers in the study regions and their catchment areas, excluding only the three previously participating in the pilot. This meant that there is no pure control for the facility intervention package at endline. We collected evaluation data from all facilities and a sample of households in their catchment areas at three timepoints: baseline (October–November 2014), midline (July–August 2016) and endline (May–June 2018). Experienced enumerators were trained on and then administered these surveys.
Two-stage cluster sampling was used to identify study households. For each of the 19 health centers participating in the evaluation, a full list of eligible enumeration areas and their respective population was obtained from the national statistical office. Six enumeration areas were randomly selected from each facility’s catchment area with probability proportional to size, resulting in a total of 114 study clusters. Because the Gambian health sector maps villages only to health centers, the two hospitals in the project area do not have unique catchment areas and were not considered for the community sampling. Randomization was implemented using Stata’s “samplepps” command.
Once enumeration areas were selected, a census of eligible households within them was conducted, and 20 households in each randomly selected for the survey. A household was eligible for inclusion if it had at least one woman aged 15 or older and at least one child under the age of five. In enumeration areas with fewer than 20 eligible households, all consenting households were enrolled. Within each household, questionnaires were administered to the household head and the mother of the youngest child. This process was repeated for subsequent survey rounds. With a target of 20 households across 114 enumeration areas, the expected sample size for each round was 2,280 households.
Qualitative Data Collection
Qualitative data were collected from different stakeholders to obtain further insight into the intervention’s performance. Semi-structured interviews and focus group discussions (FGDs) took place at baseline, midline and endline ().
Table 1. Qualitative research participants and sample sizes.
. Qualitative research participants and sample sizes
Study communities were purposively selected to reflect regional diversity and a mix of performance across the incentivized quantitative indicators. FGD participants included female and male community residents; female groups were purposively selected to comprise women who had given birth in the preceding six months. Data collection guides were tailored to different types of participants but explored the same core themes: perceptions of the intervention, health- and nutrition-related behaviors, and if, how and why these behaviors changed as the interventions were implemented. Instruments were field-tested and amended as necessary before data collection. Interviews were conducted in the language of each respondent’s choice, including Mandinka, Wollof and Fula.
Outcome Measures
The quantitative analysis used seven indicators to assess intervention impact. These indicators measured changes in behaviors that had been incentivized in order to achieve the desired improvements: attending early ANC; three additional ANC visits following a timely first visit; skilled delivery at a health facility; existence of improved household sanitation facilities; existence of a handwashing station; soap at handwashing station; and water at handwashing station.
Exposure Measures
The primary variables of interest were exposure to the facility package and community group RBF interventions. For maternal health outcomes, information on the date of delivery was used to assess intervention exposure during pregnancy. For delivery outcomes, exposure was assessed on the date of delivery. For ANC outcomes, exposure was assessed at the presumed start of the pregnancy, calculated as 280 days prior to the reported date of delivery.
Statistical Analysis
Multivariable linear regression models were estimated using pooled baseline, midline and endline data. Regressions included binary indicators for exposure to each of the community group and facility package interventions, survey round dummy variables for midline and endline data, and community fixed effects. The main model is explained in the Supplemental Material.
Two supplemental models were also run. Supplemental Model 1 includes a binary interaction term to assess synergies between community group and facility package interventions. Supplemental Model 2 assesses the impact of prolonged exposure to either intervention. Similar to the main model, Supplemental Model 2 includes a dummy variable indicating any exposure; it also includes a second dummy indicating exposure for at least one completed quarter (90-plus days) of exposure. This second dummy is modeled as supplementary to the first, so any effect is over and above the initial impact.
The facility interventions package was not hypothesized to impact the WASH outcomes as there were no relevant incentivized indicators. Analyses of the WASH variables include a binary indicator for exposure to the community group intervention, and survey round dummy variables. As above, community fixed effects were also included to account for time-invariant regional variation in behaviors. In all models, standard errors were clustered at the facility level using Huber’s cluster robust variance estimator.Citation15
Qualitative Data Analysis
All interviews and FGDs were recorded, transcribed verbatim and translated into English, then imported into NVivo 10 for analysis. We performed thematic analyses of the data using a set of codes derived originally from the literature on RBF and the project’s theory of change, which we refined as themes emerged in the data. Example codes include: knowledge and beliefs related to ANC and delivery, demand for services, barriers to access, and community ownership of activities. Midline and endline findings are presented here, with a focus on understanding the mechanisms and dynamics underlying the quantitative findings. Select quotations illustrate main themes.
Ethical Approval
This study received ethical approval from the Gambia Government/MRC Joint Ethics Committee (R014 036), the University of Southern California’s Institutional Review Board (HS-14-00688), and Harvard School of Public Health’s Institutional Review Board (IRB14-3955). Study participation was voluntary and informed consent was obtained from all study participants prior to study commencement.
Results
We analyzed 5,927 household surveys: 1,939 conducted at baseline, 1,951 at midline, and 2,037 at endline. In all rounds, final sample sizes were slightly below the original targets due to some relatively small enumeration areas yielding fewer than 20 eligible households.
Characteristics of mothers who participated in the surveys are reported in . Findings across all rounds were consistent with these regions’ demographics.
Table 2. Balance across survey rounds.
. Balance across survey rounds
Deliveries and ANC Attendance
Our primary results for ANC and deliveries are presented in .
Table 3. Intervention impact on key maternal health variables.
: Intervention impact on key maternal health variables
Skilled Delivery
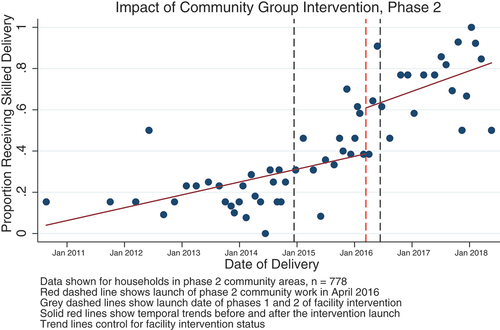
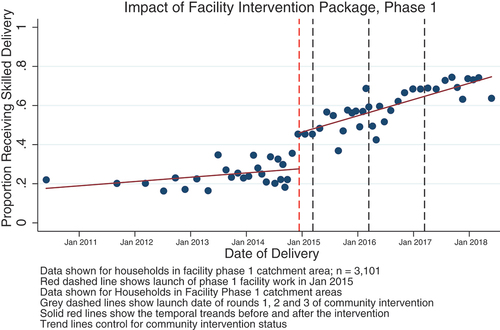
On average, community group interventions increased skilled deliveries by 11 percentage points, while the facility package increased it by 7 percentage points. Data suggest strong temporal trends, with linearly increasing rates of skilled delivery in the intervention areas, and visible shifts in uptake that coincide with the launch of intervention activities. There were no interactions in the data so we analyzed the isolated impact of each type of intervention (community group and facility package) on uptake of skilled delivery. highlights the increase in utilization immediately following the launch of the second round of community group interventions.
The figure pools data from the 778 births in the phase 2 community area to present monthly skilled delivery rates. All households in this sub-group were exposed to community group interventions beginning in April 2017 (red dashed line), and were evenly split between phases 1 and 2 of the facility intervention package (gray dashed lines). The impact of the facility interventions package is not observable in this pooled data but there is a visible jump in the rate of skilled delivery that coincides with the launch of the community group intervention.
highlights the increase in utilization immediately following the launch of the first round of the facility intervention package.
Focusing here on the households exposed to Phase 1 of the facility intervention package (3,101 births), we again observe a strong linear trend of increasing facility delivery over the study period, with a marked increase at the time that the facility intervention package launched (shown in red). This impact cannot be attributed to the community group interventions (launch dates shown in gray).
Qualitative participants perceived a sharp increase in health facility deliveries since intervention implementation, driven by understanding of the health benefits of facility delivery and that complications can be managed more effectively in health facilities than at home. Most women reported that educational efforts and a desire to protect themselves and their babies motivated them to seek facility-based skilled delivery. A male community member explained:
“If you deliver at home you may not know whether you lack water (dehydration) or whether you have low blood (anemia). But if you deliver at the health facility the nurses will know whether you lack water or not or whether you have low blood. This is why it is better and safer to deliver at the health facility. For if I leave my wife to deliver at home she may lose her life.“ Male community member
Interview participants indicated that when a woman delivers at home, it is often because she delayed calling for assistance until she was fully dilated or because she did not realize soon enough that she was in active labor. Other reported barriers related to transportation including distance from a health facility, the absence of a suitable vehicle, and poor roads. Many villages reported using community incentive payments to acquire a motorized tricycle ambulance to transfer mothers to the facility, but others are still reliant on donkey carts or private vehicles.
Participants reported that Community Birth Companions now accompanied women in labor to the health facility rather than delivering the babies at home. This was due to both a policy shift that mandated that Community Birth Companions no longer carry out deliveries and the information and incentives provided by the project.
ANC Attendance
No impact on ANC attendance was found, either in the community group or facility package exposure arms.
In the qualitative data, women reported ongoing challenges to attending early ANC including distance to the health facility, women not understanding the importance of early attendance and not yet wanting other people to know about the pregnancy. The latter two were reported to particularly affect unmarried women. Women still breastfeeding their previous child were reportedly ashamed to be seen to be pregnant again while still breastfeeding.
“What factors affect the women’s decision about when to seek ANC service apart from distance? R3: Sometimes cultural barriers like hiding early pregnancy from people, until 5 months or so for fear of being bewitched … Also the young ‘primips’ (first pregnancy) they are shy for people to know that they are pregnant so they will be reluctant to come for booking early.” – FGD, women who had delivered within the previous 6 months
Participants reported a variety of reasons for women not completing four ANC visits as well as early ANC including women’s geographical distance from facilities, competing responsibilities, gender dynamics and concerns about potentially unfriendly health facility staff.
“Young women coming with their children is very difficult. The issue of male domination in this patriarchal society … in The Gambia particularly, some families cannot make a decision without the men.” – Regional Health Directorate
However, there were also some reports that attitudes about seeking early ANC had improved and husbands’ support for early ANC attendance had increased. Women who had given birth in the preceding six months reported that both the CCT and the known health benefits influenced their decisions to attend ANC during the first trimester of pregnancy. Women reported appreciating not needing to ask their husbands for money, and being able to use the money to support their and their infants’ health.
There was no indication of interaction between the facility intervention package and community group intervention for any of the skilled delivery or ANC variables (Supplementary Table 2).
Exposure Time
This study suggests that longer exposure to an RBF intervention may not result in greater impact on the targeted behaviors (Supplementary Table 3). Communities receiving the facility intervention package in the second phase and thus for a shorter period of time (22 months) on average experienced larger improvements than communities with longer exposures to the facility intervention package (40 months).
Water, Sanitation and Hygiene
The community group intervention led to 49, 43 and 48 percentage point increases in handwashing stations, soap at station, and water at stations, respectively ().
Table 4. Intervention impact on key water, sanitation and hygiene variables.
: Intervention impact on key water, sanitation and hygiene variables
No impact was found on improved sanitation facilities.
Supplementary Figures 1–4 show the availability of the different WASH facilities at baseline, midline and endline by when the community group intervention was initiated. Where community group interventions began in 2014 or 2016, an increase in availability of handwashing stations, soap and water observed soon after interventions began was not sustained, as indicated by declines in these indicators at endline.
Qualitative participants reported major improvements in handwashing practices following the intervention. Community residents noted that handwashing with soap and running water, both after using the toilet and before handling food, has become commonplace and is widely accepted to be beneficial for health. VDCs are likely to have contributed to this change as representatives reported that there had been ongoing efforts both to gather the materials for hygiene systems and to promote handwashing.
Discussion
This large mixed-methods study sought to determine the effects of a combination incentive program on key MCH indicators. Results indicate that, compared to controls, for most indicators, the community group interventions appeared to have the strongest impact, particularly on skilled delivery as well as water and hygiene, but not the sanitation indicators measured. The facility intervention package had a positive impact on skilled delivery. Compared with control areas, neither intervention impacted early ANC attendance alone or in combination with three additional ANC visits, with gender norms and societal beliefs about pregnancy likely still impeding uptake of early ANC. We had expected to find an interaction between the community group intervention and the facility intervention package based on the hypothesis that incentivizing the same behaviors in different ways would better promote change, but this was not found.
Prior to study design, two preliminary assessments, commissioned by the Government of The Gambia and the World Bank, identified the potential for demand-side barriers to limit the impact of a traditional supply-side RBF intervention focused only on incentive payments within health facilities. This led to the inclusion of community group interventions—a particularly innovative feature for an RBF intervention. The community group interventions were designed to foster demand for ANC and skilled delivery through community channels, including a SBCC campaign carried out by community actors. The design of the intervention took into account the potential for existing local governance and health-promoting bodies to effectively foster greater demand for some health services and behaviors, including through purchase of vehicles to help overcome access barriers. The Gambia’s VDCs and VSGs exist throughout the country, are well-established mechanisms for delivering public services and are viewed by their constituents as credible institutions. As such, they were a highly effective platform for implementation of the community group RBF intervention, which showed most successful outcomes. In other settings with less robust community groups, the same approach might not be advisable. Although none of the interventions included community group incentives, a recent review found that incorporating demand-side RBF tools was a critical success factor for institutionalizing RBF.Citation16 However, as has been noted for previous health facility RBF interventions,Citation17 our community group intervention provided an influx of funding to local committees who usually operate without a budget: we cannot ascertain whether it was the performance targets or simply the cash injection that created the changes recorded.
Implementation required diverse health system and community actors to adopt and integrate complex administrative and service delivery-related procedures into existing activities. Health facilities and community partners faced implementation challenges including the ongoing administrative burden imposed by reporting and verification mechanisms. Coordinating partners also found their roles to be labor-intensive. During the first 18 months of project implementation, an administrative error led to the wrong pricing being applied, causing health facilities to receive, on average, 13% less income than anticipated from the intervention. Data suggest that there were many challenges for the implementation of the CCT program, which required both tracking of women and targeted disbursements. The capacity for verification and incentive disbursement as well as the financial autonomy of health facilities has been noted as a key foundation for RBF activities.Citation18,Citation19
RBF interventions around the world have had mixed results: some have improved both utilization and quality of MCH services, others have improved quality but not utilization, and others still have been found to be largely ineffective.Citation1–5 Overall, our program impact varied largely across indicators, likely because they were all incentivized through different combinations of community, facility and individual incentives and because some behaviors are more sensitive to change based on financial incentives than others,Citation20 with, for example, social and cultural beliefs about behaviors such as adolescent sexuality and family planning often a barrier.
Community norms about not revealing a pregnancy during the first trimester and shyness among young mothers seem particularly entrenched in The Gambia. Increased uptake of early ANC has been achieved using facility RBF in ArgentinaCitation21 and by providing incentives to community health workers in Rwanda,Citation22 but community norms surrounding pregnancy may be markedly different in these settings. Within The Gambia, barriers to the uptake of delivery services appear to have been easier to tackle, partly with the change in role of the Community Birth Companions but also with the introduction of better transportation to health facilities through the use of the community incentives. Logistical barriers may, in some cases, be easier to overcome than cultural barriers.
With the exception of improved sanitation, there were pronounced increases in availability of WASH facilities during the period immediately following the community groups intervention but these were not sustained. The greater cost of materials and labor required for improved sanitation facilities may explain why less improvement was seen in this indicator. Community group incentives for improving WASH indicators are innovative. Previous studies have looked primarily at service delivery being contracted out to a third party which receives a subsidy to complement or replace the user contribution, CCTs at household level and voucher payments, all of which operate very differently than the community group incentives. While some of these approaches have been found to be effective, their efficiency and sustainability is less clear.Citation23
That longer exposure to the interventions did not necessarily result in greater impact suggests that the quality of the intervention may matter more than the duration of exposure. Implementation at both the facility- and community-level may have improved over time as actors became more familiar with the project, resulting in better outcomes in later phases.
Limitations
This study has a number of limitations. Although we included all health facilities in the study regions, this provided a sample size of 19, meaning that relatively large changes were needed to identify statistically significant changes in the outcomes of interest. For some outcomes, strong positive trends were also seen over time, further limiting the ability to see intervention impacts. We could not separate out the impact of health facility incentive payments and the CCTs provided to individual women. Subgroup analyses by wealth quintile were not possible because differences in the income levels of household survey participants were small. Finally, our findings are based on self-reported data, which can be subject to bias.
Potential Future Analyses
The need remains to better understand the impact of duration of exposure and the importance of long-term evaluation. This is a particularly important issue for RBF because of the complexity of implementing both a facility intervention package and a community group intervention that are sufficiently far-reaching to drive large-scale improvements in health outcomes.
Given the emphasis of this RBF intervention on providing combinations of incentives, a key research question is whether more heavily incentivized behaviors underwent more pronounced changes. The meta-analysis mentioned above found no statistically significant differences in impact between single interventions and interventions that sought to address both supply and demand side barriers.Citation24 This reflects our study findings (Supplemental Table 1). Our data are suggestive that there was no effect on the most incentivized behavior (ANC attendance), which is surprising but could be at least partially explained by the implementation challenges of the CCTs noted above.
Conclusions
The intervention studied was innovative in bringing together a community group RBF intervention and a facility RBF intervention package to improve maternal and child nutrition and health. Although no interaction was found between these two interventions, this study highlights the importance of understanding the nature of barriers to uptake of MCH services before designing RBF interventions. Where demand-side barriers predominate and where community governance structures exist, community-based interventions may be more effective than the facility-only RBF designs that have been widely adopted.
Contributorship Statement
We would like to acknowledge the time and expertise of the many experts who contributed to the development of this article.
Overall Development, Coordination And Oversight
Laura Ferguson, Principal Investigator
Rifat Hasan, co-Principal Investigator of the impact evaluation
Quantitative Data Team
Yaya Jallow – University of The Gambia
Günther Fink – Swiss TPH and University of Basel
Chantelle Boudreaux – Harvard University
Gambia Bureau of Statistics:
Project Manager: Nyakassi M B Sanyang
Field Manager: Lamin L Dibba
Coordinators: Catherine Gibba Omo, Famara Fatty, Lamin Kanteh, Samba Barrow
Supervisors: Abdou Sanyang, Abie Jabang, Amie Bojang, David Mendy, Ebrima Jammeh, Ebrima Tunkara, Fatou S Jabang, Ndye Binta Bojang, Saikou Jawara, Sainey Sanneh, Sandiki Colley
Household interviewers: Abou Fofana, Aja T.M.Kinteh, Alimameh Badjie, Amie Gigo, Amie Sallah, Aminata Badjie, Babucarr Danso, Babucarr Jasseh, Bai Matarr Jaiteh, Bintou Badjie, Charles Demba, Dembo Fofana, Dobally Jobe, Ebrima Jallow, Edrisa Njie, Fabakary Jawneh, Famara Nyabally, Fatou Manneh, Fatoumatta Ceesay, Fatou Suwareh, Indira Henry Jammeh, Isatou A Badjie, Isatou Bah, Isatou Jallow, Ismaila Dibba, Josephine Sylva, Madi Mangan, Mam Fatou Gaye, Mamanding Colley, Mansour Dibba, Mansour B Joof, Mariama Dibba, Modou S Nyassi, Momodou Sarr, Muhammed Bah, Muhammed Sanneh, Mustapha Saho, Mustapha Sanyang, Nafisatou Jatta, Olimatou Sissoho, Omar Njie, Ousman Cham, Pa Ousman Ceesay, Tabara Gibba, Tida Gassama
Health facility interviewers: Adama Humma, Alieu Faal, Hassan Njie, Lamin B. Fatty, Lamin Saidykhan, Mass Joof, Mustapha Sanneh, Omar Mbackeh
Anthropometrists: Balla Cham, Basiru Sanyang, Fatou Cham, Imran Jabang, Lamin Darboe, Muhammed Joof, Ousman L. Kanyi
Real-Time Analytics: Le Dang Trung and his team
Qualitative Data Team
Mariama Dibba, Sira Bah, Momodou Conteh, Sering Fye, Kristin Dessie Zaccharias, Bita Minaravesh
Peer Review
Project Implementation Committee: Modou Cheyassin Phall, Abdou Aziz Ceesay, Ousman Ceesay, Dr. Momodou L. Waggeh, Mamady Cham, Famata Colley, Modou Lamin Darboe, Malang N. Fofana, Catherine Gibba, Bakary Jallow, Musa Loum, Elizabeth Mago, Lamin Njie, Matty Njie, Alhagie Sankareh. World Bank Task Team: Rifat Hasan, Menno Mulder-Sibanda and Ronald Mutasa, The World Bank GroupImpact Evaluation Advisory Panel: Christopher Belford UTG, Alfusaney Jabbi MOF, Bakary Jallow NaNA, Dr Momodou Jasseh MRC, Sainey Sanneh MOHSW, Sheriffo Sonko NMCP
Data Availability
The data used for this evaluation are publicly available through the World Bank Microdata Repository (Reference: GMB_2014_HRBFIE-BL_v01_M).
Supplemental Material
Download EPS Image (22.1 KB)Supplemental Material
Download EPS Image (21.9 KB)Supplemental Material
Download EPS Image (22.3 KB)Supplemental Material
Download EPS Image (22.3 KB)Supplemental Material
Download MS Word (26.5 KB)Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplementary Material
Supplemental material for this article can be accessed online at https://doi.org/10.1080/23288604.2022.2117320
Additional information
Funding
Notes
[a]. Minor health facilities provide only primary health care while major health facilities have a larger, better trained workforce as well as a functional blood bank, operating theater and electricity.
References
- Bonfrer I, Van de Poel E, Van Doorslaer E. The effects of performance incentives on the utilization and quality of maternal and child care in Burundi. Soc Sci Med. 2014;123:96–12. doi:10.1016/j.socscimed.2014.11.004.
- Huillery E, Seban J. Performance-based financing, motivation and final output in the health sector: experimental evidence from the Democratic Republic of Congo. Sciences Po Economics Discussion Papers 2014-12. Paris, France: Sciences Po Department of Economics.; 2014.
- Engineer CY, Dale E, Agarwal A, Agarwal A, Alonge O, Edward A, Gupta S, Schuh HB, Burnham G, Peters DH, et al. Effectiveness of a pay-for-performance intervention to improve maternal and child health services in Afghanistan: a cluster-randomized trial. International Journal of Epidemiology. 2016;45(2):451–59. doi:10.1093/ije/dyv362.
- De Brauw A, Peterman A. Can conditional cash transfers improve maternal health and birth outcomes?. Washington D. C: International Food Policy Research Institute (IFPRI); 2011.
- Shapira G, Kalisa I, Condo J, Humuza J, Mugeni C, Nkunda D, Walldorf J. Going beyond incentivizing formal health providers: evidence from the Rwanda community performance-based financing program. Health Economics. 2018;27(12):2087–106. doi:10.1002/hec.3822.
- Bertone MP, Falisse JB, Russo G, Witter S. Context matters (but how and why?) A hypothesis-led literature review of performance based financing in fragile and conflict-affected health systems. PLoS One. 2018;13(4):e0195301. doi:10.1371/journal.pone.0195301.
- Binyaruka P, Lohmann J, De Allegri M. Evaluating performance-based financing in low-income and middle-income countries: the need to look beyond average effect. BMJ Glob Health. 2020;5(8):e003136. doi:10.1136/bmjgh-2020-003136.
- World Development Indicator database. 2013. https://databank.worldbank.org/views/reports/reportwidget.aspx?Report_Name=CountryProfile&Id=b450fd57&tbar=y&dd=y&inf=n&zm=n&country=GMB
- UNDP. Human Development Report 2014. Sustaining human progress: reducing vulnerabilities and building resilience. New York: UNDP; 2014.
- The Gambia Bureau of Statistics G, and I. C. F. International. The Gambia demographic and health survey 2013. Banjul (The Gambia): GBOS and ICF International; 2014.
- Sundby J. A rollercoaster of policy shifts: global trends and reproductive health policy in The Gambia. Glob Public Health. 2014;9(8):894–909. doi:10.1080/17441692.2014.940991.
- Ministry of Health and Social Welfare. 2012 services statistics report: final draft: government of The Gambia; 2012.
- Cole-Ceesay R, Cherian M, Sonko A, Shivute N, Cham M, Davis M, Fatty F, Wieteska S, Baro M, Watson D, et al. Strengthening the emergency healthcare system for mothers and children in The Gambia. Reproductive Health. 2010;7(1):21–21. doi:10.1186/1742-4755-7-21.
- World Bank. Using results-based financing to achieve maternal & child health: progress report. Washington (DC, USA): World Bank; 2013.
- Huber PJ The behavior of maximum likelihood estimates under nonstandard conditions. presented at: Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Vol. 1: Statistics; 1967; Berkeley, Calif.
- James N, Lawson K, Acharya Y. Evidence on result-based financing in maternal and child health in low-and middle-income countries: a systematic. Global Health Research and Policy. 2020;5(1). doi:10.1186/s41256-020-00158-z.
- Diaconu K, Falconer J, Verbel A, Fretheim A, Witter S. Paying for performance to improve the delivery of health interventions in low‐ and middle‐income countries. Cochrane Database of Systematic Reviews. 2021;2021(5). doi:10.1002/14651858.CD014669.
- McIsaac M, Kutzin J, Dale E, Soucat A. Results-based financing in health: from evidence to implementation. Bull World Health Organ. 2018;96(11):730–730a. doi:10.2471/BLT.18.222968.
- Coulibaly A, Gautier L, Zitti T, Ridde V. Implementing performance-based financing in peripheral health centres in Mali: what can we learn from it? Health Res Policy Syst. 2020;18(1):54. doi:10.1186/s12961-020-00566-0.
- Gneezy U, Meier S, Rey-Biel P. When and why incentives (Don’t) work to modify behavior. J Econ Perspect. 2011;25(4):191–210. doi:10.1257/jep.25.4.191.
- Gertler P GP, Martinez S. Rewarding provider performance to enable a healthy start to life: evidence from Argentina’s plan Nacer. Policy Res Work Pap. Washington, D.C: World Bank; 2014.
- Shapira G KI, Condo J, Humuza J, Mugeni C, Nkunda D, Walldorf J. Effects of performance incentives for community health worker cooperatives in Rwanda. Washington, D.C: World Bank; 2017.
- Castalia Strategic Advisors. Review of results-based financing schemes in WASH (The Hague, The Netherlands: IRC Wash) 2015.
- Neelsen S, de Walque D, Friedman J, Wagstaff A. Financial incentives to increase utilization of reproductive, maternal and child health services in low- and middle-income countries: a systematic review and meta-analysis. Washington, D.C: World Bank; 2021.