 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
From 2005 to 2019, the Mexican government financed cervical cancer treatment for individuals without social security insurance through Seguro Popular’s Fund for Protection against Catastrophic Health Expenses. To better understand the impact of this program on access to treatment, we estimated the cervical cancer treatment gap (the proportion of patients with cervical cancer in this population who did not receive treatment). To calculate the expected number of incident cervical cancer cases we used national surveys with information on insurance affiliation and incidence estimates from the Global Burden of Disease study. We used a national claims database to determine the number of cases whose treatment was financed by Seguro Popular. From 2006 to 2016, the national cervical cancer treatment gap changed from 0.61 (95% CI 0.59 to 0.62) to 0.45 (95% CI 0.43 to 0.48), with an average yearly reduction of −0.012 (95% CI −0.024 to −0.001). The gap was greater in states with higher levels of marginalization and in the youngest and oldest age groups. Although the cervical cancer treatment gap among individuals eligible for Seguro Popular decreased after the introduction of public financing for treatment, it remained high. Seguro Popular was eliminated in 2019; however, individuals without social security have continued to receive cancer care financed by the government in the same healthcare facilities. These results suggest that barriers to care persisted after the introduction of public financing for treatment. These barriers must be reduced to improve cervical cancer care in Mexico, particularly in states with high levels of marginalization.
Introduction
Cervical cancer is the second leading cause of cancer death among women in Mexico.Citation1,Citation2 As in other regions of the world, individuals living in rural and lower socioeconomic status areas experience the highest cervical cancer mortality rates.Citation3,Citation4 Cervical cancer can be prevented through vaccination or with effective screening and treatment of pre-cancerous lesions.Citation5 In Mexico, a national cervical cancer screening program was introduced in 1974.Citation6 Nevertheless, coverage remains low, with a 28.9% one-year prevalence of Pap smear among women aged 20 and older in 2018–2019.Citation7 If screening fails, timely treatment of cervical cancer can increase survival and quality of life.Citation8 However, individuals in low- and middle-income countries often face barriers to timely diagnosis and treatment. Among these are sociocultural barriers like poverty, low health literacy, and the stigmatization of cancer and sexual and reproductive health, as well as health system barriers like the accessibility and quality of available health services.Citation9,Citation10
These challenges also confront the Mexican healthcare system, which is divided into three sectors: 1) social security organizations with financing from the government, employers and employees that provide health services for the formally employed and their families (approximately 40% of the population); 2) Ministry of Health facilities, which are mainly utilized by the population without social security; and 3) private facilities, which are very often used by both the insured by social security and the uninsured paying out of pocket (only 1% of the population has private health insurance).Citation11
A voluntary insurance scheme, Seguro Popular, in place from 2004 until 2019, provided healthcare financing for a predetermined list of health interventions for people without social security. As part of this program there was a Fund for Protection against Catastrophic Health Expenses that covered high-cost treatments for selected conditions. By 2018 this fund covered treatment for 65 different medical conditions, including cervical cancer (beginning in 2005).Citation12,Citation13 Coverage for other cancers for adults including breast, testicular, non-Hodgkin lymphoma, prostate, colorectal, and ovarian was gradually rolled out until 2016. Health services were provided mainly at hospitals financed by the federal and state Ministries of Health. However, there is no research on how access to treatment for cervical cancer might have improved with the implementation of Seguro Popular financing.
A treatment gap is defined as the number of people with a condition or disease who need treatment but do not receive it.Citation14 The treatment gap is a measure of healthcare utilization that can be used to assess access. There has been one prior study of the impact of breast cancer treatment financed through Seguro Popular, but no other studies of its impact on the treatment gap for any other type of cancer, including cervical cancer.Citation15 Estimating the cervical treatment gap could help researchers and policymakers better understand whether Seguro Popular expanded access to treatment and inform ongoing efforts to reduce disparities and improve cancer outcomes in Mexico. Therefore, in the present study, we estimated the national treatment gap for cervical cancer by comparing the number of cervical cancer cases with treatment financed by Seguro Popular between 2006 and 2016 with estimates of incident cervical cancer cases among the eligible population. Additionally, we stratified treatment gap estimates by state level marginalization and by age group to assess for disparities.
Materials and Methods
Treated Cervical Cancer Cases
We assumed that all individuals eligible for Seguro Popular who received cervical cancer treatment had their treatment financed by Seguro Popular. All cervical cancer cases with treatment financed by Seguro Popular were routinely documented in a nationwide claims database. Claims were submitted to Seguro Popular by the facilities providing treatment. This database has previously been used to study cervical cancer survival in Mexico.Citation16 For our study we analyzed claims for incident cervical cancer cases available from years 2006 to 2016. Patients were excluded from analysis if the age at diagnosis was less than 15 as estimates of the proportion of the population eligible for Seguro Popular were not available for this age group. Patients with recurrent, progressive, or persistent cancers were excluded as these cancers had already received treatment. Patients with pre-invasive lesions were also excluded as these are typically classified as pre-cancerous and are categorized separately from cervical cancer in the Global Burden of Disease (GBD) database from which we obtained estimates of cervical cancer incidence.Citation1
From the analytic database, we extracted the following descriptive variables for patients: year initiating treatment, age at diagnosis, state of residence and clinical stage at the initiation of treatment. The state of residence variable was not available for the years 2015 and 2016. Clinical stages were documented using the International Federation of Obstetrics and Gynecology (FIGO) 2009 guidelines and classified as follows based on categories used by the Mexican Society of Oncology: early (IA1 to IB1), locally advanced (IB2 to IIIB), and metastatic (IVA to IVB).Citation17,Citation18 Cervical cancer cases were grouped according to the degree of marginalization of their state of residence using Mexico’s National Population Council (CONAPO) classification (five levels, from very low to very high).Citation19 This index is defined periodically for each state based on geographic socioeconomic indicators including poverty, education, and access to services.
Cervical Cancer Incidence
We estimated the expected incidence of cervical cancer among individuals eligible for Seguro Popular by multiplying the estimated proportion of women eligible for Seguro Popular in strata defined by year, state and age group by cervical cancer incidence rates estimated for Mexico. As Mexico has no national cancer registry, we used incidence estimates from the Global Burden of Disease (GBD), which is the only source of information on cancer incidence for Mexico that provides estimates by year and state. For the proportion of individuals in each stratum eligible for Seguro Popular, we used estimates that were derived for a prior study.Citation15 Briefly, for this estimation process we combined data from the Mexican Census and multiple national surveys containing information on insurance coverage for individuals in Mexico. Using this combined dataset, we specified linear regression models to estimate the proportion of individuals eligible for Seguro Popular by strata defined by year, state, and age group.
Cervical Cancer Treatment Gap
The cervical cancer treatment gap was calculated by dividing the number of cervical cancer cases who received treatment financed through Seguro Popular by the number of estimated incident cases among individuals eligible for Seguro Popular and then subtracting the result from 1 (EquationEquation 1(1)
(1) ).
We estimated the yearly cervical cancer treatment gaps from 2006 to 2016 nationally and by age group and from 2006 to 2014 also by degree of marginalization at the state level. We calculated uncertainty intervals for treatment gap estimates that incorporated uncertainty in the inputs used to generate the treatment gap, i.e., uncertainty in the proportion of women eligible for Seguro Popular and uncertainty in GBD estimates of cervical cancer incidence. This was done by using randomly generated numbers from a normal distribution and variance estimates from these inputs to produce 1,000 simulated datasets which were used to estimate 1,000 sets of treatment gap estimates. We defined the uncertainty interval by taking the 2.5th and 97.5th percentiles of the distribution of treatment gap estimates created by this procedure. This method is described in detail in a prior publication.Citation15
A linear regression model with treatment gap as the outcome and year as a predictor was used to assess the average yearly reduction in the treatment gap. To estimate uncertainty intervals for this trend, we specified 1,000 linear regression models (one for each simulated dataset) and combined estimates of the standard deviation for the time coefficient using Rubin’s rules. Rubin’s rules are designed to pool parameter estimates from multiple datasets, incorporating variance present within datasets as well as variance present between datasets.Citation20 We then repeated this procedure specifying one set of models with an interaction between year and age group and another set of models with an interaction between year and state level marginalization. Statistical analyses were completed using SAS 9.4 (SAS Institute, Cary NC) and Stata 14.0 (Stata Corp, College Station, TX).
Results
The claims database contained 39,983 patients with treatment financed by Seguro Popular from 2006 to 2016 (Supplementary Figure S1). Of these, 9,713 patients were excluded because they did not have an incident cancer, including 8,473 patients with precancerous lesions and 1,240 patients with previously treated cancers. A further 15 patients were excluded due to age less than 15 and 1,676 patients were excluded because the year of initiation of treatment was before 2006. In the final sample 28,579 cases remained.
The mean age of included patients was 51.4 (SD 13.7) (). Most patients had locally advanced disease (IB2 to IIIB; 64.5%). The highest proportion of patients (23.1%) was from states with high levels of marginalization while the lowest proportion was from states with very low levels of marginalization (10.6%). A minority of patients (18.3%) received treatment outside of their state of residence. State of residence was not available for 2015 and 2016 so data on state level marginalization and out-of-state treatment was not reported for these years (20.2% of patients).
Table 1. Characteristics of women with cervical cancer treatment financed by Seguro popular between 2006 and 2016 (n = 28,567).
National treatment gap estimates are presented in and . From 2006 to 2016, the treatment gap changed from 0.61 (95% CI 0.59 to 0.62) to 0.45 (95% CI 0.43 to 0.48). There was a downward linear trend in the treatment gap across the study period. The average yearly reduction of the treatment gap was − 0.012 (95% CI − 0.024 to − 0.001). The annual number of patients with treatment financed by Seguro Popular increased from 2,162 in 2006 to 3,311 in 2016 while the number of expected cases increased from 5,500 to 6,047 during the same period.
Figure 1. National cervical cancer treatment gap between 2006 and 2016. The treatment gap demonstrated a downward trend with an average yearly change of − 0.012 (95% CI: −0.024 to − 0.001) estimated using linear regression.
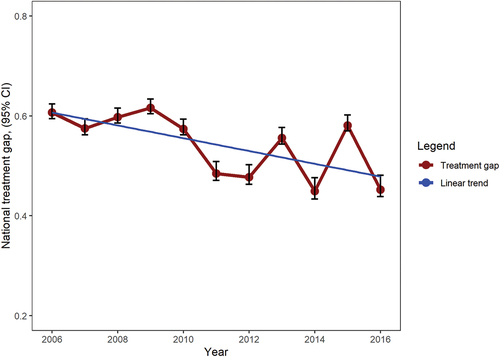
Table 2. National cervical cancer treatment gap by year from 2006 to 2016 among women in Mexico eligible for Seguro popular.
We observed higher treatment gaps and smaller reductions in the treatment gap in older and younger age groups than in intermediate age groups (Supplementary Table S1). For example, among individuals aged 55 to 59 the treatment gap decreased from 0.58 (95% CI 0.53 to 0.63) in 2006 to 0.23 (95% CI 0.12 to 0.33) in 2016 with an average yearly reduction of − 0.026 (95% CI − 0.041, −0.012). For individuals aged 20 to 24 the treatment gap decreased from 0.78 (95% CI 0.75 to 0.81) to 0.62 (95% CI 0.58 to 0.68) during this same period with an average yearly reduction of − 0.011 (95%CI: −0.024, 0.002) and for those aged 70–74 the treatment gap decreased from 0.58 (95% CI 0.53 to 0.63) to 0.35 (95% CI 0.27 to 0.43) with an average yearly reduction of − 0.018 (−0.032, −0.005). In our regression model, there was some evidence of interaction between year and age group (p = .141).
From 2006 to 2014 (the period for which state data were available) there was a graded association between state-level marginalization and the treatment gap, with higher treatment gaps observed for states with higher marginalization levels (). The average yearly reduction tended to be greater in states with low and moderate levels of marginalization in comparison to states with very low, high or very high levels. In states with very low levels of marginalization, the treatment gap decreased from 0.52 (95% CI 0.47, 0.57) to 0.31 (95% CI 0.25, 0.39) with an average yearly reduction of − 0.012 (95% CI − 0.029 to 0.004). In states with moderate levels of marginalization, the treatment gap decreased from 0.59 (95% CI 0.57 to 0.62) to 0.44 (95% CI 0.41 to 0.48) with an average yearly reduction of − 0.023 (95% CI − 0.038, −0.008). In states with very high levels of marginalization the treatment gap decreased from 0.68 (95% CI 0.66 to 0.71) to 0.55 (95% CI 0.52 to 0.59) with an average yearly reduction of − 0.013 (95% CI − 0.028 to 0.002). We did not find evidence of interaction between year and marginalization in our regression model (p = .370).
Table 3. Cervical cancer treatment gap by year from 2006 to 2014 among women in Mexico eligible for Seguro Popular, by state-level marginalization.
Discussion
The cervical cancer treatment gap among individuals in Mexico eligible for Seguro Popular was reduced after ten years of treatment financing through Seguro Popular but remained high by the end of the study period. The highest treatment gaps were observed in states with the highest levels of marginalization as well as in younger and older patients.
The limited reduction of the treatment gap observed for cervical cancer contrasts with the findings for breast cancer treatment, the only other type of cancer for which the treatment gap has been studied. The breast cancer treatment gap went from 0.71 (95% CI 0.69 to 0.73) in 2007 to 0.15 (95% CI 0.09 to 0.22) by 2016.Citation15 The difference between cancer sites could be related to persistent barriers to treatment impacting individuals with cervical cancer more than individuals with breast cancer. Prior studies have reported that cervical cancer disproportionately affects individuals of lower socioeconomic status in Mexico, in contrast with breast cancer, which is more likely to affect individuals of higher socioeconomic status.Citation21 After treatment financing was introduced, individuals of higher socioeconomic status may have been more able to leverage resources to overcome the persistent barriers to care that we describe in the following paragraphs than individuals with low socioeconomic status.
Seguro Popular financing for cervical cancer treatment removed the barrier of having to pay out of pocket for oncologic care, but it is likely that other access barriers to care persisted, including barriers to screening and diagnosis, financial barriers not addressed by Seguro Popular, and non-financial barriers to treatment. One possible explanation for the persistently high cervical cancer treatment gap in our study could be that many individuals with cervical cancer never received treatment because they were never diagnosed due to limited access to screening and diagnostic testing. The GBD estimates cancer incidence using mortality estimates derived from death records and reclassifies deaths with a nonspecific cause using a statistical model.Citation22 Consequently, our incidence estimates included cases which were diagnosed and treated, cases which were diagnosed and remained untreated as well as cases that were never diagnosed. It is likely that there was an important proportion of individuals with cervical cancer who remained undiagnosed and did not receive treatment, as there is limited access to screening and to diagnostic testing for cervical cancer. Despite the existence of a cervical cancer screening program in Mexico for more than 50 years, the one-year prevalence of Pap smear among women aged 20 and older continues to be low (28.9% in 2018–2019 and 21.4% in 2021) and there are concerns that the effectiveness of screening may be limited by the inconsistent quality of cytology interpretation.Citation7,Citation23,Citation24 Prior studies have identified significant barriers to participation in cervical cancer screening in Mexico including limited patient knowledge of cervical cancer and screening, negative perceptions of screening and the inaccessibility of health services.Citation25,Citation26
In addition to limited access to screening, limited access to diagnostic testing for cervical cancer may have also presented a barrier to cervical cancer treatment. A recent study of women who participated in a cervical HPV screening program in public clinics in Mexico City reported that only 57% of those with abnormal results adhered to the recommended colposcopy. Longer travel times between the primary healthcare facility where screening was performed and the colposcopy clinic reduced the likelihood of adherence.Citation27 In addition, a study of cervical cancer patients receiving treatment in Mexico City found that the median time between first contact with a physician for findings concerning for cervical cancer and diagnosis of cervical cancer was 99 days, with 28.3% of patients experiencing a delay of more than 6 months, suggesting that substantial barriers to diagnostic testing exist as well.Citation28 The most prominent barriers to cancer care identified by women participating in this study were lack of information about public health services, lack of financial resources to use services, long wait times and diagnostic errors at primary care services.
Limited access to cervical cancer screening and diagnostic testing may also influence the treatment gap by increasing the number of cancer cases diagnosed at locally advanced or metastatic stages. One study focusing on the two largest cancer treatment centers serving Seguro Popular patients in Mexico City found that between 2016 and 2017, 17.4% of patients had metastatic disease when they initiated treatment, a figure more than twice as large as what we observed in our study.Citation28 Individuals with metastatic cancer may have decided to forego treatment after being told that treatment would likely not be curative. Such individuals may have been more prevalent in our study as our sample included rural areas and states with higher levels of marginalization. In such settings, the financial and time burdens associated with treatment of metastatic disease may have seemed less worthwhile to many patients. Furthermore, whereas early-stage cervical cancer can be treated with surgery alone at local facilities, cervical cancer diagnosed at locally advanced or metastatic stages may require radiation therapy and concomitant chemotherapy only available in tertiary care hospitals that are concentrated in urban areas.Citation29 This could further explain the low proportion of metastatic cases observed in our study, if patients in rural and highly marginalized areas with metastatic disease were unable to travel to treatment centers.
Another possible explanation for the high cervical cancer treatment gap we observed could be persistent financial barriers to treatment not addressed by Seguro Popular financing. Seguro Popular reimbursed hospitals for the cost of the treatment they provided; however, patients may still incur substantial expenses associated with treatment. Cervical cancer mortality rates have been shown to be disproportionately higher in low socioeconomic status and rural areas both in Mexico and globally.Citation3,Citation16,Citation21 Patients who live in rural areas far from cancer centers travel long distances at personal expense to seek specialized treatment in large cities. Time away from home can lead to additional financial difficulties as patients are unable to fulfill family and work responsibilities.Citation30
Finally, non-financial barriers may also have prevented individuals with cervical cancer from receiving treatment. Globally, limited health literacy, cancer stigma, gender related cultural norms, like the expectation that women should prioritize taking care of their family above their own health, have been described as important non-financial barriers to cancer treatment.Citation10 Additional research is needed to assess the influence of these barriers on access to cervical cancer treatment in Mexico.
Limitations
We note several limitations to our study. Our results depend on accurate estimates of cervical cancer incidence, but the GBD and the Global Cancer Observatory (GLOBOCAN), the two most authoritative estimates of cancer incidence globally, provide discrepant estimates of cervical cancer incidence in Mexico. It is generally accepted that the most reliable estimates of cancer incidence are produced using cancer registries, but as there is no national cancer registry in Mexico, both GLOBOCAN and the GBD use vital statistics to estimate cancer incidence in Mexico. However, differences in the specific methodologies each project uses lead to different results.
For our study, we chose to use GBD estimates as the GBD is the only source of cancer data that provides historical and state-level estimates of cancer incidence across Mexico. GLOBOCAN reports a cervical cancer age standardized incidence rate of 12.6 for Mexico in 2020 (the only year for which data is available) which is 31% lower than the age standardized incidence rate of 18.3 (95% CI 14.6, 24.8) estimated by the GBD for 2019 (the closest available year).Citation1,Citation2 If we were to reduce our incidence estimate for 2016 by 31% to reflect this, the treatment gap for 2016 would be 0.21, which still represents a substantial proportion of untreated cases but is about half as much as the treatment gap of 0.45 that we estimated using the GBD. Furthermore, estimates from both sources differ from estimates provided by the state level registry in Mérida, Yucatán, which is the only population-based cancer registry in Mexico. From 2015 to 2018, the age standardized incidence rate for cervical cancer estimated using a state level registry in Mérida, Yucatán was 17.5 while the rate estimated by the GBD for Yucatán in 2018 was 22.4 (95% CI 18.7, 27.0).Citation1,Citation31
A second limitation is our assumption that the Seguro Popular database accurately represented the number of women eligible for Seguro Popular who received treatment. It is possible that a small number of individuals eligible for Seguro Popular may have received treatment in the private system and were not included in the database. This would have inflated our treatment gap estimates. On the other hand, some women who were technically ineligible for Seguro Popular because they had social security may have enrolled in Seguro Popular and been included in the database. This would have led to underestimation of the treatment gap.
A third possible cause of bias in our treatment gap estimates is our assumption that cervical cancer incidence was the same in individuals with and without social security. If cervical cancer incidence among individuals without social security (the population eligible for Seguro Popular) was higher or lower than in the general population, this could influence treatment gap estimates.
A fourth limitation is that preinvasive cases could have been classified as invasive because the reimbursement amount was higher for invasive cases. This would have led to an underestimation of the treatment gap. However, monitoring performed by Seguro Popular administrators may have limited this possibility.Citation13
An additional limitation of our study is that there is no available information about the treatment gap prior to the implementation of Seguro Popular financing for treatment or after the elimination of Seguro Popular. It is imaginable that the treatment gap estimates observed in our study in fact represent a reduction from an even higher baseline prior to 2006, and we are unable to determine if the trend observed in our study continued after 2016. Finally, although with our study design it is not possible to assess specific domains of access such as the approachability, acceptability, availability, affordability and appropriateness of health services for the patients to get treated, our treatment gap estimate provides a measure of access to cervical cancer treatment.Citation32
Implications
These results have important implications for efforts to improve cervical cancer outcomes in Mexico. Although Seguro Popular was eliminated in 2019, individuals without social security continue to receive cancer care in the same healthcare facilities and the government has continued to finance cancer treatment for patients without social security through a similar funding mechanism.Citation11 Providing financing for the direct costs of cervical cancer treatment remains an essential priority, however, the health system needs to do more than this to ensure access to cervical cancer treatment in Mexico, particularly in states with high levels of marginalization. Interventions are needed to address persistent financial barriers to care such as costs associated with transportation to the cancer center and lodging while receiving treatment.Citation29 Addressing non-financial barriers to treatment such as cancer stigmatization or low health literacy may also be necessary. Finally, while supporting treatment of cervical cancer patients is necessary, the focus of interventions for cervical cancer control should be on prevention, early detection and timely treatment: increasing HPV vaccine coverage and improving timely access and quality of screening tests and diagnostics.
Conclusions
Although the cervical cancer treatment gap was reduced among the population without social security after ten years of treatment financing through Seguro Popular, it remained quite high, especially in states with high levels of marginalization. These findings are likely due to persistent barriers to treatment, including limited access to screening and diagnostic testing, costs of treatment not addressed by Seguro Popular financing, and non-financial barriers to treatment. To increase access to cervical cancer treatment in Mexico, future interventions will be needed to address these persistent barriers to care.
Ethical Approval
The study protocol was approved the Institutional Review Board of Mexico’s National Cancer Institute.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Data Availability Statement
The data that support the findings of this study are available from the CNPSS (Comisión Nacional de Protección Social en Salud). These data were used under license for the study. Therefore, restrictions apply to the availability of the data. Data are available from the authors with the permission of the CNPSS.
Additional information
Funding
References
- Global Burden of Disease Collaborative Network. Global burden of disease study 2019 (GBD 2019) results. IHME; 2019 [accessed 2022 Aug 16]. https://vizhub.healthdata.org/gbd-results/.
- Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global cancer observatory: cancer today. 2020 [accessed 2022 Jan 8]. https://gco.iarc.fr/today.
- Singh GK, Azuine RE, Siahpush M. Global inequalities in cervical cancer incidence and mortality are linked to deprivation, low socioeconomic status, and human development. Int J MCH AIDS. 2012;1(1):17–9. doi:10.21106/ijma.12.
- Palacio-Mejía LS, Rangel-Gómez G, Hernández-Avila M, Lazcano-Ponce E. Cervical cancer, a disease of poverty: mortality differences between urban and rural areas in Mexico. Salud Publica Mex. 2003;45(Suppl 3):S315–25. doi:10.1590/s0036-36342003000900005.
- Gultekin M, Ramirez PT, Broutet N, Hutubessy R. World Health Organization call for action to eliminate cervical cancer globally. Int J Gynecol Cancer. 2020 Apr;30(4):426–27. doi:10.1136/ijgc-2020-001285.
- Lazcano-Ponce EC, Rascón-Pacheco RA, Lozano-Ascencio R, Velasco-Mondragón HE. Mortality from cervical carcinoma in Mexico: impact of screening, 1980-1990. Acta Cytol. 1996 May-Jun;40(3):506–12. doi:10.1159/000333907.
- Encuesta Nacional de Salud y Nutricion 2018-2019: Resultados nacionales. Instituto Nacional de Salud Publica; 2020. https://ensanut.insp.mx/encuestas/ensanut2018/doctos/informes/ensanut_2018_informe_final.pdf.
- Diagnosis and treatment of invasive cervical cancer. The World Health Organization; 2014 [accessed 2022 Jul 30]. https://www.ncbi.nlm.nih.gov/books/NBK269603/.
- Paz-Soldán VA, Bayer AM, Nussbaum L, Cabrera L. Structural barriers to screening for and treatment of cervical cancer in Peru. Reprod Health Matters. 2012 Dec;20(40):49–58. doi:10.1016/S0968-8080(12)40680-2.
- Nnaji CA, Ezenwankwo EF, Kuodi P, Walter FM, Moodley J. Timeliness of diagnosis of breast and cervical cancers and associated factors in low-income and middle-income countries: a scoping review. BMJ Open. 2022 Feb 4;12(2):e057685. doi:10.1136/bmjopen-2021-057685.
- Gonzalez-Block MA, Reyes-Morales H, Hurtado LC, Balandrán A, Méndez E. Mexico: health system review. Health Syst Transit. 2020 Apr;22(2):1–222. https://www.ncbi.nlm.nih.gov/pubmed/33527902.
- Aracena-Genao B, González-Robledo MC, González-Robledo LM, Palacio-Mejía LS, Nigenda-López G. El Fondo de Protección contra Gastos Catastróficos: tendencia, evolución y operación. Salud pública Méx. 2011 [accessed 2022 Jul 30];53:407–15. https://www.scielosp.org/article/spm/2011.v53suppl4/407-415/es/.
- Chemor Ruiz A, Ratsch AEO, Alamilla Martínez GA. Mexico’s Seguro Popular: achievements and challenges. Health Syst Reform. 2018 Jul 3;4(3):194–202. doi:10.1080/23288604.2018.1488505.
- Kale R. Global campaign against epilepsy: the treatment gap. Epilepsia. 2002;43(Suppl 6):31–33. doi:10.1046/j.1528-1157.43.s.6.13.x.
- Unger-Saldaña K, Contreras-Manzano A, Lamadrid-Figueroa H, Mohar A, Suazo-Zepeda E, Espinosa-Tamez P, Lajous M, Reich MR. Reduction in the treatment gap for breast cancer in Mexico under Seguro Popular, 2007 to 2016. Health Syst Reform. 2022 Jan 1;8(1):e2064794. doi:10.1080/23288604.2022.2064794.
- Torreglosa-Hernández S, Grisales-Romero H, Morales-Carmona E, Hernández-Ávila JE, Huerta-Gutiérrez R, Barquet-Muñoz SA, Palacio-Mejía, LS. Supervivencia y factores asociados en pacientes con cáncer cervicouterino atendidas por el Seguro Popular en México. Salud Publica Mex. 2022 Feb 25;64(1):76–86. doi:10.21149/13119.
- Cetina-Pérez L, Ochoa-Carrillo F. Cáncer cervicouterino, aún el reto por vencer. Gaceta Mexicana de Oncología. 2014 Oct;13. https://www.gamo-smeo.com/temp/SUPLE%204%20CANCER%20CERVICOUTERINO.PDF.
- Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009 May;105(2):103–04. doi:10.1016/j.ijgo.2009.02.012.
- Consejo Nacional de Población. Índice de marginación por entidad federativa y municipio 2010; 2012. https://www.gob.mx/cms/uploads/attachment/file/671846/1_IMEyM2010_PAG_1_64.pdf.
- Rubin DB. Multiple imputation for nonresponse in surveys. New York (NY): John Wiley & Sons; 2004. p. 258.
- Palacio-Mejía LS, Lazcano-Ponce E, Allen-Leigh B, Hernández-Ávila M. Diferencias regionales en la mortalidad por cáncer de mama y cérvix en México entre 1979 y 2006. Salud pública Méx. 2009;51:s208–s19. http://www.scielo.org.mx/scielo.php?pid=S0036-36342009000800011&script=sci_abstract&tlng=pt.
- Global Burden of Disease 2019 Cancer Collaboration.Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the global burden of disease study 2019. JAMA Oncol. 2021 Dec 30. doi: 10.1001/jamaoncol.2021.6987.
- Encuesta Nacional de Salud y Nutrición 2021 sobre Covid-19: Resultados nacionales. Instituto Nacional de Salud Publica; 2022. https://ensanut.insp.mx/encuestas/ensanutcontinua2021/doctos/informes/220804_Ensa21_digital_4ago.pdf.
- Lazcano-Ponce E, Palacio-Mejia LS, Allen-Leigh B, Yunes-Diaz E, Alonso P, Schiavon R, Hernandez-Avila M. Decreasing cervical cancer mortality in Mexico: effect of Papanicolaou coverage, birthrate, and the importance of diagnostic validity of cytology. Cancer Epidemiol Biomarkers Prev. 2008 Oct;17(10):2808–17. doi:10.1158/1055-9965.EPI-07-2659.
- Lazcano-Ponce EC, Castro R, Allen B, Nájera P, Alonso de Ruíz PA, Hernández-Avila M. Barriers to early detection of cervical-uterine cancer in Mexico. J Womens Health. 1999 Apr;8(3):399–408. doi:10.1089/jwh.1999.8.399.
- Allen-Leigh B, Uribe-Zúñiga P, León-Maldonado L, Brown BJ, Lörincz A, Salmeron J, Lazcano-Ponce, E. Barriers to HPV self-sampling and cytology among low-income indigenous women in rural areas of a middle-income setting: a qualitative study. BMC Cancer. 2017 Nov 9;17(1):734. doi:10.1186/s12885-017-3723-5.
- León-Maldonado L, Hernández-Ramírez RU, Torres-Ibarra L, Spiegelman D, Sheth SS, Lazcano E, Cadena-Fiscal JD, Salmerón J. Factors associated with receiving results and attending colposcopy in patients with positive HPV screens in Mexico City. Prev Med Rep. 2023 Jul 24;102347:102347. https://www.sciencedirect.com/science/article/pii/S2211335523002383.
- Unger-Saldaña K, Arroyo-Valerio A, Turrubiates GS, Gómez-Navarro JA, Bargalló-Rocha E, Quintero-Beuló G, Isla-Ortiz D, Jiménez-Ríos MÁ, García HAM, Salgado IRL, et al. Time intervals to care and health service use experiences of uninsured cancer patients treated under public financing in Mexico city. Cancer Epidemiol. 2023 Apr 20;84:102366. doi:10.1016/j.canep.2023.102366.
- Maldonado Magos F, Lozano Ruíz FJ, Álvarez SI P, Garay Villar O, Cárdenas Pérez C, Bautista Hernández MY, Núñez Guardado G. Radiation oncology in Mexico: current status according to Mexico’s radiation oncology certification board. Rep Pract Oncol Radiother. 2020 Sep;25(5):840–45. doi:10.1016/j.rpor.2020.06.002.
- Wu ES, Jeronimo J, Feldman S. Barriers and challenges to treatment alternatives for early-stage cervical cancer in lower-resource settings. J Glob Oncol. 2017 Oct;3(5):572–82. doi:10.1200/JGO.2016.007369.
- Leal YA, Torres J, Gamboa R, Mantilla-Morales A, Piña-Sanchez P, Arrieta O, Bonifaz L, Meneses A, Duque C, Piñeros M, et al. Cancer incidence in Merida, Mexico 2015-2018: first report from the population-based cancer registry. Arch Med Res. 2022 Dec;53(8):859–66. doi:10.1016/j.arcmed.2022.11.015.
- Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013 Mar 11;12(1):18. doi:10.1186/1475-9276-12-18.
