?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Reducing the price of expensive medical products through centralized procurement is generally considered an effective way to save public medical resources. Against this background, this paper presents an analysis of the impact of centralized procurement in China by comparing the treatment costs and patterns for acute myocardial infarction (AMI) patients before and after the introduction of this method of purchasing, with specific reference to the use of coronary stents. We found that, after the implementation of centralized procurement for coronary stents, the total expenditure of AMI cases receiving percutaneous coronary interventions with stent implantation (PCI with stents) dropped by 23.4%. The use rate of PCI with stents decreased by 32.5%, with the most significant decrease being evident in cases in which two stents were used simultaneously (32.9%). Meanwhile, percutaneous coronary interventions with balloon implantation (PCI with balloons) increased by 31.5% and coronary artery bypass grafting (CABG) increased by 80.3%. Based on these patterns, it can be observed that the use of centralized procurement significantly reduced the profits of the relevant medical manufacturers, forcing them to decrease their marketing investments, weakening their influence on providers, and ultimately resulting in a more principled use of coronary stents. We therefore conclude that, with reference to the data cited, the centralized procurement program led not only to a reduction in procurement prices but also to decreased overuse of these expensive medical products.
Introduction
With increasing usage, high-value medical consumables continue to impose a significant and growing financial burden on healthcare systems. “Centralized procurement,” a collaborative initiative involving joint procurement by buyers, is considered to be an effective means of addressing this burden. One common understanding of the mechanism of centralized procurement is that, by consolidating demand, one can intensify competition among suppliers, leading to reductions in product prices.Citation1 The experience of some OECD countries (e.g., Greece and Italy) includes the implementation of such centralized procurement programs for medical devices and consequent savings in public health expenditure without compromising the level of health services.Citation2–4 As a result, significant numbers of low-and middle-income countries (LMICs), such as Tunisia,Citation5 Brazil,Citation6 the Philippines, Zambia, and China, have also come to implement centralized procurement programs for high-value medical consumables.
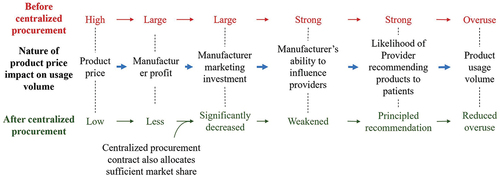
Although the literature demonstrates clear benefits stemming from centralized procurement, there are other ways in which centralized procurement impacts the market that must be borne in mind. illustrates the nature of the relationship between the price of medical products and their sales volume. In situations of information asymmetry between providers and patients, manufacturers can expand their product sales by influencing healthcare providers and incentivizing them to recommend their products to patients. There is ample evidence indicating that manufacturers are willing to make such marketing investments to influence providers.Citation7–10 As a result, providers often recommend more expensive medical consumables at a high price to their patients.Citation11–13 Undoubtedly, for manufacturers, sustaining such marketing investment requires high levels of profits.
Figure 1. The nature of the relationship between sales price and volume of medical products in the context of information asymmetry between providers and patients.
In 2014, the average price of a coronary stent in the United States was around 1,360 USD, four times the cost of the same consumable in Germany. The price in Mainland China was even higher; before the centralized procurement policy was implemented, the average price of a coronary stents was 1,964 USD, while the same devices cost 330 USD in Brazil and 1,039 USD in France.Citation8,Citation14,Citation15 Moreover, high prices do not seem to have reduced the use of high-value medical consumables. Before centralized procurement, the overall rates of use of coronary stents in China increased between 2009 and 2018, from 250,000 stents to 1.5 million.Citation16
Based on the analysis given above, if China implements centralized procurement for coronary stents, both mechanisms will come into play, potentially resulting in simultaneous decreases in both the price and use of coronary stents.
In 2020, the National Healthcare Security Administration of China extended the centralized procurement program to cover high-value medical consumables for the first time, including coronary stents. The process of implementing centralized procurement includes a basic rule of first conducting a consistency evaluation of similar products, with those of at least equivalent efficacy but sold at lower prices winning out for selection. Ten different varieties of coronary stents, produced by eight medical device manufacturers, won the bidding, at a price of around 106 USD (with the lowest at 67 USD and the highest at 114 USD), a striking 1/18 of the previous price (1,964 USD on average).Citation17 From 2021, in the 30 pilot cities in which centralized procurement had been introduced, winning bids for coronary stents were required to be used preferentially.
Patients with acute myocardial infarction (AMI) are a group of clear interest in relation to the use of coronary stents. In China, under the guidelines for AMI diagnosis and treatment, doctors typically determine the treatment options of AMI patients based on the degrees of blockage of the patient’s coronary artery and its branches.Citation18 If one or two branches have severe narrowing, percutaneous coronary interventions with stent implantation (PCI with stents) are usually chosen; in this situation, some doctors may prefer to choose percutaneous coronary interventions with balloon implantation (PCI with balloons). If three or more blood vessels are narrowed or blocked, or the anatomical location of the blockage is otherwise unsuitable for treatment with PCI, then coronary artery bypass grafting (CABG) will be prioritized. Regarding choices between PCI and CABG surgeries, recommendations in guidelines issued by various countries are generally similar.Citation19–21
Using data from a Chinese city, City M, which is piloting a centralized procurement policy and has a population of 20 million, this study was conducted to investigate the hypothesis that, following the introduction of the centralized procurement policy in relation to coronary stents, the utilization rate of PCI with stents in patients with AMI would decrease. It was also hypothesized that the utilization rate of PCI with multiple stents would be reduced more significantly. Turning to PCI with balloons, these constitute an alternative treatment option,Citation22 and are an example of high-value medical consumables that have not yet been included in the centralized procurement policy, although the average purchase price of balloon catheters is about 500 USD, around a quarter of the pre-centralized procurement price of coronary stents.Citation17 Following the implementation of centralized procurement in respect of coronary stents, the price of balloon catheters can be observed to be 4–5 times that of coronary stents. It was therefore expected that the utilization rate of PCI with balloons for AMI patients would increase following the implementation of the policy.
Materials and Methods
Study Design
Previous studies employ cross-sectional designs for correlation analysis or use DID methodologies or Interrupted Time Series analysis for causal inference to assess the impact of centralized procurement on medical costs. We designed this study based on the characteristics of the data we obtained.
Starting in early 2021, all hospitals in City M have been required to give priority to the use of coronary stents accessed by the centralized procurement program. As this reform covers all hospitals in City M, this study could not have been conducted by setting any hospital that did not participate in the reform as the control group; therefore, to capture the impact of the centralized procurement policy for coronary stents, we measured the trend changes before and after the implementation of the centralized procurement program for coronary stents (between 2019 and 2021), and, based on this, compared the resulting data with the natural trend before the reform (between 2018 and 2020). If the reform can be seen to result in a change from the natural trend, this may be taken as evidence that the reform has had an effect. Clearly, establishing that the natural trend before centralized procurement is stable is a requirement if this design is to capture the effects of centralized procurement.
As shown in , the years 2018 and 2020 were grouped together (Group A), representing the “natural” changes without experiencing centralized procurement, only subject to time trends; and 2019 and 2021 into another group (Group B), representing the combined changes of natural variation plus the experience of centralized procurement. The combined change of Group B minus the natural change of Group A was taken to indicate the impact of centralized procurement.
Data
We obtained the discharge data of AMI patients in City M from the city’s health security bureau. Data relating to discharged cases primarily diagnosed as having AMI were identified according to the ICD-10 code (I21), and a total of 97,776 AMI cases were extracted from 174 hospitals for the period 2018–2021. The data for each discharged case contained information relating to primary and secondary diagnoses, procedures, medical expenses and demographics.
The primary outcome variable was the type of treatment each AMI case received, with options including PCI with stents, PCI with balloons and coronary artery bypass grafting (CABG). Following the identification of this variable, measurements were carried out with respect to the number of stents implanted (one, two, three, and four or more stents, identified by code ICD-9-CM3), expenditure (adjusted by the consumer price index of City M), length of hospitalization, 30-day readmission rate, and in-hospital mortality.
Statistical Analysis
The propensity score matching (PSM) method was used to process the discharge data between 2018 and 2019 and 2020 and 2021, respectively, to ensure consistency between the intervention group and the control group regarding age, gender and the Charlson Comorbidity Index (CCI). A total of 92,944 AMI cases were included in the study.
Regression analyses were conducted to determine whether the implementation of the centralized procurement program for coronary stents was associated with outcome variables of PCI with stents, PCI with balloons and CABG occurrence rate, as well as expenditure, length of hospitalization, 30-day readmission rate, and in-hospital mortality. Local price indices were used to adjust for the effects of inflation when calculating medical expenses. Following the design as shown in , we established a regression model
in which Y is the corresponding dependent variable (logistic regression is used for the probability of PCI or CABG use, in-hospital mortality rate, and 30-day readmission rate; logarithmic linear regression is used for medical expenses and length of stay); T is the grouping variable of time, indicating which year the data pertain to (for 2018 and 2019, T = 0; for 2020 and 2021, T = 1). CP represents the trend change brought about by centralized procurement. In 2018 and 2020, CP = 0; while in 2019 and 2021, CP = 1. X is a covariable, including gender, age, comorbidities, etc. The results of continuous variables were estimated using a linear probability model, with the regression coefficient taken to reflect the changes in medical indicators. The results of dichotomous variables were assessed using a logistic model, with the OR value being taken to reflect the impact of policy implementation on procedures.
In order to measure the stability of the natural trend before centralized procurement for coronary stents, there was a need to first assess two periods of data before the pilot reform was implemented, namely the first halves of 2018/2019 and 2020 and the second halves of 2018/2019 and 2020. A stable trend test prior to the centralized procurement for coronary stents was conducted for this purpose. The design of the stable trends test is detailed in Appendix 2.
Standard errors were clustered at the hospital level to account for potential correlation within hospitals.
All data analysis in this study was performed using Stata SE 15.0.
Results
Basic Information
presents the numbers of AMI discharges between 2018 and 2021 in City M. After PSM, there were 23,962 samples in 2018 and 2019, and 22,510 samples in 2020 and 2021. In terms of gender distribution, males accounted for two-thirds of the cases. Regarding age structure, the largest group of patients was those aged 61–80 (47–48%). More than 70% of these patients had comorbidities, with 1/3 of cases having severe comorbidities (CCI ≥3).
Table 1. Descriptive statistics of the sample characteristics, costs, procedure type and outcomes, 2018–2021.
For treatment options, the proportion of cases receiving medical therapy without procedures shows a downward trend before the implementation of the centralized procurement program for coronary stents, from 54.1% in 2018 to 46.4% in 2020. After the implementation of the program, this downward trend halts, with the proportion rising to 47.6% in 2021, showing a slight rise from 2020. For cases receiving PCI treatment, the number continues to rise from 2018 to 2020, before dropping sharply in 2021, with the number of cases receiving PCI with balloons increasing even more in 2021 than in the previous two years. The trend for the probability of receiving CABG treatment is different, showing a continuous decline from 2018 to 2020 but a sudden increase in 2021.
The mean expenditure per case of AMI rises continuously from 2018 to 2020, but then falls significantly in 2021, with a marked decrease in consumables costs, from an average of 4,384.6 USD per case in 2020 to 2,257.2 USD per case in 2021. Length of hospitalization shows a downward trend, and the in-hospital mortality rate in 2020 and 2021 is lower than in 2018 and 2019. The 30-day readmission rate gradually declines over these four years.
The case mix of the raw (pre-matched) data is not significantly different from the matched data. Descriptive statistics of the raw data can be found in Appendix 1.
Impact on Treatment Patterns
The results of the stable trend test show that the natural trend was consistent for each outcome indicator before centralized procurement (details are provided in Appendix 2). Therefore, the regression analysis we designed was considered suitable for assessing the impact of centralized procurement.
details how logistic regression was used to control for age, gender and severity of comorbidities among AMI cases, and to evaluate the impact of the centralized procurement program for coronary stents on health providers’ treatment options. It can be seen that the implementation of this program led to a 32.5% decrease in the probability of health providers choosing PCI with stents, with a decline of 23.6%, 32.9%, and 29.2% for a PCI with one stent, two stents and three stents, respectively. The probability of choosing PCI with four stents shows a numerical decrease albeit not a statistically significant one. On the other hand, after the implementation of the program, the probability of pursuing treatment using PCI with a balloon increases by 31.5%, and the probability of selecting CABG increases by 80.3%.
Table 2. Logistic regression estimates of the effects of the centralized procurement of coronary stents on procedure types for AMI patients.
Effects on Costs, Length of Hospitalization and Quality of Care
As shown in , the regression analysis indicates that the implementation of the centralized procurement program for coronary stents led to a 23.4% decrease in the average cost per AMI case, with a 43.2% decrease in the average medical consumables cost and a 13.4% decrease in the average drug cost. However, no significant change can be observed in the length of hospitalization, in-hospital mortality rate or 30-day readmission rate for AMI cases following the implementation of the centralized procurement program.
Table 3. Regression estimates of the effects of the centralized procurement of coronary stents on costs, length of hospitalization, in-hospital mortality, and 30-day readmission rate for AMI patients.
Discussion
As previously discussed, centralized procurement is considered an effective means of increasing the efficient use of public resources, and one that has attracted the attention of both developing and developed nations alike. Beginning with the phenomenon of coronary stents being widely sold at high prices in China, the focus of this study is to analyze changes in the use of coronary stents brought about by centralized procurement. This change is reflected in the treatment patterns received by AMI patients. The results show that, first, the direct effect of this program has been a reduction in the medical expenditure in cases of AMI; second, that the probability of AMI patients receiving PCI with stents has decreased, with the decrease in the use of two or three stents being more significant than that of the use of a single stent; and third, that there has been an increase in the probability of AMI patients receiving PCI with balloons or CABG.
Given the specifics of the hypothesis stated at the outset, it can be concluded that there is consistency between this hypothesis and what is witnessed in terms of the reduction in medical expenditure for AMI patients, the decrease in the probability of receiving PCI with a stent, and the rise in the likelihood of an AMI patient receiving a PCI with a balloon. It is notable also that another study conducted using data from a medium-sized city in China reports similar results.Citation23 We interpret these findings as follows. First, the centralized procurement program has directly reduced the cost of stents through lowering the purchase price; as a result, profits from the selling of coronary stents have disappeared; consequently, manufacturers been incentivized to reduce their investment in marketing; this, in turn, has led to a decrease in the influence of the manufacturer on healthcare providers, and health providers have thus become more inclined to select treatment patterns in a manner more influenced by patients’ needs. Ultimately, the decrease in the treatment cost for AMI patients is the combined result of the drop in stent prices and reductions in usage.
As previously noted, PCI with balloons is another alternative treatment option available for use with AMI patients, albeit it is not yet included in the centralized procurement program. Before the centralized procurement reform for coronary stents, the price of balloons in Mainland China was much lower than that of stents. However, following the reform, the price of balloons has become higher than that of stents, indicating a potential increase in the probability of using PCI treatments with balloons as a substitute for PCI treatments with coronary stents. A similar situation can be observed with respect to the case of the centralized procurement of drugs. In one study, researchers reviewed centralized drug procurement policies in 17 countries and regions and came to the conclusion that total drug expenditure may have failed to continue to decline due to the phenomenon of “demand redistribution” involving the offsetting of cost savings from centralized procurement policies by the increased costs of alternative drugs.Citation24 A study of 9 pilot cities and 12 non-pilot cities of centralized drug procurement policy in China found that the proportion of bid-winning drugs decreased significantly by 23.3%; in contrast, the proportion of the use of non-bid-winning drugs increased significantly, by 17.7%.Citation25
It was not expected that the centralized procurement program for coronary stents would lead to an increase in CABG. One possible explanation for this observation is that the surgical indication of CABG is multi-vessel and multi-site coronary artery lesions,Citation21,Citation26 making it necessary to use multiple stents if a PCI with a stent is selected as the treatment option. This study offers empirical support for this explanation. The regression analysis was found to indicate a 16.1% decrease in PCI with the use of four or even more stents simultaneously, albeit only to a statistically insignificant degree possibly due to the small sample size of the CABG cases.
During the period covered in this study (2018–2021), the Chinese government implemented two policies related to medical consumables. In addition to the centralized procurement of coronary stents, which is the focus of this research, there was also the elimination of mark-ups on medical consumables referred to as “zero mark-up,” enacted in 2019.Citation27,Citation28 This was another initiative by the Chinese government to minimize the influence of manufacturers on the treatment decisions of healthcare providers by prohibiting healthcare providers from earning profits through the sale of medical consumables. To assess the impact of the zero mark-up policy, we conducted a stable trend test using data from 2018 and 2020 (see revised drafts in Appendix 2–3 and Appendix 2–4), in addition to the previously conducted stable trend tests for 2019 and 2020 (see Appendix 2–1 and Appendix 2–2). We found that from 2018 to 2020, the probability of myocardial infarction patients receiving PCI treatment and the associated medical costs showed a stable trend, indicating that the zero mark-up policy has not yet impacted the use of PCI treatment for patients with myocardial infarction.
In societies in which manufacturers can use financial payments to influence physicians’ clinical decisions, including in the prescription of drugs, the Chinese experience indicates that the centralized procurement program is more effective than the “zero mark-up” policy. The primary reason is that the zero mark-up policy only applies to hospitals, resulting in hospital administrators no longer encouraging doctors to prescribe more drugs or use expensive consumables. Although physicians nevertheless remain under the influence of manufacturers, centralized procurement can be seen to have significantly reduced the profit margins of consumables sold by manufacturers, forcing them to cut back on marketing investments and thereby freeing physicians (at least to some extent) from their influence.
There have been concerns that the price of coronary stents for China’s centralized procurement program may be too low and may therefore affect product quality notwithstanding that manufacturers are required to provide product quality assurance during bidding.Citation29–31 Given the potential for knock-on effects on healthcare quality more generally, the effects of centralized procurement on stent quality remains a concern. In this study, in-hospital mortality and 30-day readmission rate were used as indicators to measure the quality of care, and no increase in in-hospital mortality and 30-day readmission rate of AMI patients was found to occur due to the centralized coronary stent procurement program. Thus, in the short term, no evidence suggests that centralized procurement of coronary stents has affected the healthcare quality of AMI patients, although the question of whether centralized procurement will shorten the working time of stents or have other adverse outcomes will require long-term monitoring.
There are some limitations to this study to note. First, it captures only short-term implementation effects, with an analysis of only the first year of post-reform discharge data being presented. Second, no information is available that evaluates the quality of coronary stents, so it is impossible to judge whether centralized procurement will impact their quality.
Conclusions
In conclusion, beyond reducing purchasing prices, using centralized procurement for high-value medical consumables also affects such consumables’ sales modes. This is likely to be an especially profound phenomenon in relation to program implications, as healthcare providers will be less influenced by manufacturers and more principled in terms of what they recommend and provide in terms of treatment options. This is possible following the disruption of the cycle of high profit engendering high investment in high-value medical consumables; as a result, it is, in turn, possible for healthcare to become more efficient and affordable.
Data Sharing
The Healthcare Security Administration governing the sample area of this study does not permit data sharing.
Ethics Committee Approval
Ethical approval for this study was obtained from Peking University (IRB number: IRB00001052–18005). All methods were carried out in accordance with relevant guidelines and regulations in terms of the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardian(s).
supplementary material.docx
Download MS Word (90.7 KB)Acknowledgments
We thank Yuehui Wei and Ruilin Wang for their input and support with revising the manuscript.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental material for this article can be accessed online at https://doi.org/10.1080/23288604.2024.2366167
Additional information
Funding
Notes on contributors
Weiyan Jian
WJ contributed to study design, interpretation, and coordinated the finalization of the manuscript. SH and WZ conducted the data collection and analysis, and compiled the associated tables and figures. WJ, LZ and WZ produced the first draft. LZ and SH contributed to work undertaken in respect of surveying the existing literature and interpreting the data. WJ and LZ wrote and edited the final manuscript. All authors provided feedback during the design and interpretation of the study and contributed to revisions of the manuscript.
References
- Long H, Yang Y, Geng X, Mao Z, Mao Z. Changing characteristics of pharmaceutical prices in china under centralized procurement policy: a multi-intervention interrupted time series. Front Pharmacol. 2022;13:944540. doi:10.3389/fphar.2022.944540.
- Callea G, Armeni P, Marsilio M, Jommi C, Tarricone R. The impact of HTA and procurement practices on the selection and prices of medical devices. Soc Sci Med. 2017;174:89–9. doi:10.1016/j.socscimed.2016.11.038.
- Kastanioti C, Kontodimopoulos N, Stasinopoulos D, Kapetaneas N, Polyzos N. Public procurement of health technologies in Greece in an era of economic crisis. Health Policy. 2013;109(1):7–13. doi:10.1016/j.healthpol.2012.03.015.
- Ferraresi M, Gucciardi G, Rizzo L. Savings from public procurement centralization in the healthcare system. Eur J Polit Econ. 2021;66:101963. doi:10.1016/j.ejpoleco.2020.101963.
- Dubois P, Lefouili Y, Straub S. Pooled procurement of drugs in low and middle income countries. Eur Econ Rev. 2021;132:103655. doi:10.1016/j.euroecorev.2021.103655.
- Dos Santos RLB, Pepe VLE, Osorio-de-Castro CGS. Public procurement of antineoplastic agents used for treating breast cancer in Brazil between 2013 and 2019. BMC Cancer. 2022;22(1):769. doi:10.1186/s12885-022-09851-3.
- Vincent Rajkumar S. The high cost of prescription drugs: causes and solutions. Blood Cancer J. 2020;10(6):71. doi:10.1038/s41408-020-0338-x.
- Wenzl M, Mossialos E. Prices for cardiac implant devices may be up to six times higher in the US than in some European countries. Health Aff (Millwood). 2018;37(10):1570–77. doi:10.1377/hlthaff.2017.1367.
- Fu H, Lai Y, Li Y, Zhu Y, Yip W. Understanding medical corruption in China: a mixed-methods study. Health Policy Planning. 2023;38(4):496–508. doi:10.1093/heapol/czad015.
- Fierce Pharma. Pfizer faces whistleblower lawsuit from former compliance manager who says he flagged possible fraud in China. 2023 [accessed 2024 Feb 26]. https://www.fiercepharma.com/pharma/pfizer-faces-employee-lawsuit-after-whistleblower-raises-flag-possible-bribery-china.
- Fu H, Li L, Yip W. Intended and unintended impacts of price changes for drugs and medical services: evidence from China. Soc Sci Med. 2018;211:114–22. doi:10.1016/j.socscimed.2018.06.007.
- Xu J, Jian W, Zhu K, Kwon S, Fang H. Reforming public hospital financing in China: progress and challenges. BMJ. 2019;365:l4015. doi:10.1136/bmj.l4015.
- Zhang Y. The study of medical consumable’s price regulation [ dissertation]. Shanghai (China): Shanghai Jiao Tong University; 2011.
- Gao H, Hu Y. Some practical problems and solutions caused by the centralized procurement system of medical consumables from the perspectives of economics. Proceedings of the 2021 12th International Conference on E-business, Management and Economics; 2021; New York, USA. doi:10.1145/3481127.3481244.
- Fan Y. To lower medical costs, China bets big on buying in bulk. 2020 [accessed 2024 Feb 26]. https://www.sixthtone.com/news/1006411.
- Editorial Department of the Journal of Cardiopulmonary Vascular Diseases. Annual report on cardiovascular health and diseases in China 2019. J Cardiovasc Pulm Dis. 2020;39(9):1145–56. doi:10.3969/j.issn.1007-5062.2020.09.028.
- China Daily. Stent prices to fall at least 90 percent. 2020 [accessed 2024 Feb 26]. https://www.chinadaily.com.cn/a/202011/09/WS5fa89445a31024ad0ba83dbc.html.
- Chinese Society of Cardiology of Chinese Medical Association; Editorial Board of Chinese Journal of Cardiology. 2019 Chinese Society of Cardiology (CSC) guidelines for the diagnosis and management of patients with ST⁃segment elevation myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(10):766–83. doi:10.3760/cma.j.issn.0253-3758.2019.10.003.
- Patel MR, Calhoon JH, Dehmer GJ, Grantham JA, Maddox TM, Maron DJ, Smith PK, Wolk MJ, Patel MR, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Thorac Cardiovasc Surg. 2019;157(3):e131–61. doi:10.1016/j.jtcvs.2018.11.027.
- National Institute for Health and Care Excellence (NICE). Acute coronary syndromes. 2020. https://www.ncbi.nlm.nih.gov/books/NBK565352/.
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. doi:10.1093/eurheartj/ehy394.
- Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, Shin E-S, Alfonso F, Latib A, Ong PJ, Rissanen TT. Drug-coated balloons for coronary artery disease: third report of the international DCB consensus group. JACC Cardiovasc Interv. 2020;13(12):1391–402. doi:10.1016/j.jcin.2020.02.043.
- Jian W, Zhou W, Zhang L. The impact of centralized coronary stent procurement program on acute myocardial infarction treatments: evidence from China. Front Public Health. 2023;11:1285558. doi:10.3389/fpubh.2023.1285558.
- Maniadakis N, Holtorf A-P, Otávio Corrêa J, Gialama F, Wijaya K. Shaping pharmaceutical tenders for effectiveness and sustainability in countries with expanding healthcare coverage. Appl Health Econ Health Policy. 2018;16(5):591–607. doi:10.1007/s40258-018-0405-7.
- Lu J, Yang Y, Long H, Wang J, Shen Y, Cui D, Mao Z, Li J. Impact of volume-based drug procurement policy on drug use structure of Chinese public medical institutions: a difference-in-difference analysis of nine pilot cities and twelve non-pilot provinces. PREPRINT (Version 1) available at Research Square. 2021; doi:10.21203/rs.3.rs-888080/v1.
- Mohr FW, Morice M-C, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Morel M-A, Van Dyck N, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. The Lancet. 2013;381(9867):629–38. doi:10.1016/S0140-6736(13)60141-5.
- China Daily. Public hospitals told to end drug markups. 2017 [accessed 2024 Feb 26]. http://english.www.gov.cn/news/top_news/2017/04/13/content_281475625276156.htm.
- China Daily. New regulation to help drive down costs of expensive medical devices. 2019 [accessed 2024 Feb 26]. http://english.www.gov.cn/news/pressbriefings/201908/02/content_WS5d43747cc6d0c6695ff7e146.html.
- Tang M, He J, Chen M, Cong L, Xu Y, Yang Y, Hou Z, Song P, Jin C. “4+7” city drug volume-based purchasing and using pilot program in China and its impact. Drug Discov Ther. 2019;13(6):365–69. doi:10.5582/ddt.2019.01093.
- Zhou J, Tan Z. Implementation and suggestions of centralized volume-based procurement of coronary stent by national organization. Health Econ Res. 2021;38(11):3–5. doi:10.14055/j.cnki.33-1056/f.2021.11.001.
- Zheng Y, Ding J, Li J, Wu Q. Research on the main obstacles and countermeasures of centralized quantity purchase of high value medical consumables. Health Econ Res. 2021;38(4):35–38. doi:10.14055/j.cnki.33-1056/f.2021.04.009.