Abstract
Pregnancy preparation, to optimize health before pregnancy, has been shown to reduce adverse maternal and neonatal outcomes. This study investigated the changes that women, and their partners, made in preparation for pregnancy. Analyses showed that less than half of women (n = 134, 49%) and only 24% of partners (n = 22) reported making any changes in preparation for pregnancy. Desire to Avoid Pregnancy (DAP) score was the only significant factor associated with pregnancy preparation; every 1-point increase in DAP reduced the odds of a woman reporting preparing for pregnancy by 78% (OR = 0.22, 95% CI = 0.15 to 0.34). This study highlights the need for interventions addressing pregnancy preparation.
Introduction
Pregnancy preparation, to optimize health before pregnancy, has been shown to reduce adverse maternal and neonatal outcomes, such as pregnancy loss, intrauterine growth restriction, and low birth weight (Maas et al., Citation2022; Stephenson et al., Citation2018). The health of both mother and father before pregnancy has also been shown to have long-term impacts on the health of future generations, including the risk of obesity, coronary heart disease, type 2 diabetes, and neurodevelopmental disorders (Fleming et al., Citation2018; Godfrey et al., Citation2017).
Currently more than 90% of women of reproductive age have at least one behavioral or medical risk factor before pregnancy (Stephenson et al., Citation2021) (where we refer to ‘women’ this should be taken to include people who do not identify as women but who have the capability to become pregnant). Almost 50% of women in the UK are either overweight (body mass index [BMI] > 25 kg/m2) or obese (BMI > 30 kg/m2) when they become pregnant (NHS, Citation2020; Stephenson et al., Citation2018), states that are associated with substantial risks for both mother and child, including sub-fertility and adverse pregnancy outcomes (Law et al., Citation2007; Marchi et al., Citation2015; Poston et al., Citation2016; Stephenson et al., Citation2018). Paternal obesity has also been linked to impaired fertility, increased risk of adverse pregnancy outcomes, and chronic disease risk in offspring (Hieronimus & Ensenauer, Citation2021; Lin et al., Citation2022; Stephenson et al., Citation2018). Micronutrient deficiencies are also a growing issue globally; studies have shown that many women of reproductive age will have dietary intakes below the recommend reference nutrient intake (RNI) for many micronutrients (Stephenson et al., Citation2018). Micronutrient deficiency during pregnancy can cause numerous adverse effects. For example, folic acid deficiency is associated with neural tube defects and other congenital abnormalities (Greenberg et al., Citation2011), while iodine and iron deficiencies can adversely affect cognitive development (Pearce, Citation2013; Zimmermann, Citation2009); studies suggest that supplementation during pregnancy does not reverse the effect (Bath et al., Citation2013; Janbek et al., Citation2019; Means, Citation2020).
Preconception care involves the identification of risk factors alongside health promotion and health intervention to minimize risks and reduce adverse pregnancy outcomes (Bortolus et al., Citation2017; Ignaszak-Kaus et al., Citation2018). For example, aiming to achieve a healthy weight, through a healthy diet, can help reduce the risks associated with being overweight/obese as well as improving some micronutrient deficiencies. However, for some micronutrients, such as folate, supplementation or food fortification are needed to achieve adequate levels. Folic acid supplementation, for at least 3months prior to pregnancy (through to 12 weeks of pregnancy), has been shown to be effective at decreasing the risk of neural tube defects by as much as 70% (De‐Regil et al., Citation2015; He et al., Citation2016; Stephenson et al., Citation2018).
The timing of the preconception period is a debated topic (Hill et al., Citation2020), but it is often defined as 3 months prior to conception. However, time to conception is different for every couple and can only be calculated retrospectively. Furthermore, numerous health issues that affect pregnancy, such as obesity and smoking, often take time and support to be tackled effectively (Stephenson et al., Citation2021). As a result, it is recommended that people start preparing for pregnancy when they start thinking about having a baby, to ensure they have adequate time to receive the full benefits of preconception care (CDC, Citation2022; Stephenson et al., Citation2018, 2021).
According to the Theory of Planned Behavior (TPB), which proposes that an individual’s decision to engage in a specific behavior is determined by their intention (Ajzen & Madden, Citation1986), everyone with a formed pregnancy intention will be undertaking actions and behaviors in line with that intention, including preparing for pregnancy. However, other more complex models, such as Bachrach and Morgan’s cognitive social model of intentions, bring together multiple factors that determine intentions and the extent to which they are enacted (Bachrach & Morgan, Citation2013). They challenge the assumption that conscious intentions precede all behaviors, instead proposing that the formation of a conscious intention draws on multiple schemas and structures relevant to that behavior. This is important in understanding why people do or do not prepare for pregnancy.
Despite the importance of preconception health, there appears to be, within the general public, a lack of awareness of preconception care and a lack of knowledge of the impact that poor preconception health can have (Daly et al., Citation2022; McGowan et al., Citation2020). There is limited research into whetherand how people prepare for pregnancy, specifically in the UK. This paper aims to identify the changes that women, and their partners, reportedly make in preparation for pregnancy, the reasons for not preparing, and the factors associated with pregnancy preparation.
Materials and methods
Study setting and design
As part of The Pregnancy Planning Preparation and Prevention (P3) study, women in the UK were invited to participate in an online survey about pregnancy preferences. The data collection methods for this study have been previously described in detail elsewhere (Hall et al., Citation2022a). Briefly, data were collected from non-pregnant women, aged 15 or older, living in the UK who had not been through the menopause or been sterilized. The cohort was recruited using social media as well as advertisements in a university, school, abortion clinic, and outreach sexual health service (see supplementary material for recruitment materials). Women completed a baseline survey online and were then invited to complete the survey again every 3 months for 1 year, unless they had an ongoing pregnancy at two consecutive time points. Overall, 994 women completed the baseline survey and almost 90% of eligible participants completed follow-up at 12 months; those lost to follow-up were not significantly different on key sociodemographic factors (Hall et al., Citation2022a).
Survey development
Details of the survey development have been previously described elsewhere (Hall et al., Citation2022a). Briefly, the survey included a range of questions, such as obstetric history, contraception use, reproductive autonomy, and sociodemographics. Wherever possible, existing measures or questions were used. Cognitive interviews were conducted to check women’s understanding of the whole survey. Changes were made iteratively and retested until no further changes were needed.
Who was asked?
Of the 994 women who took part in the baseline survey, 274 women were asked about pregnancy preparations; these were women who answered “Yes” to currently trying to get pregnant, “Yes” or “Maybe” to thinking about getting pregnant in the next year, or “No” to using contraception in the last 30 days because they were either “Trying to get pregnant” or “Didn’t mind if they got pregnant.” Further, 92 of the 274 women were asked about partner preparations; these were women who answered “No” to using contraception in the last 30 days because they were either “Trying to get pregnant” or “Didn’t mind if they got pregnant.”
What were they asked?
Women were asked whether they (or their partner) had done anything in preparation for pregnancy. If yes, they were asked what changes they had made, and if no, they were asked why they had not made any changes. All questions had multiple-choice answers with “other” as an option. See supplementary materials for exact survey questions and multiple-choice answer options.
The changes that women and their partners reportedly made in preparation for pregnancy, as well as the reasons given for not preparing, were investigated. Both univariate and multivariable analyses were then performed to determine factors associated with pregnancy preparation and partner preparation.
Measures
Pregnancy preparation
We created a binary variable of pregnancy preparation (yes/no) and a binary variable of partner preparation (yes/no). These outcome variables were derived from the answers to two self-reported questions in the baseline survey: “Are you doing anything to improve your health in preparation for pregnancy?” and “Is your partner doing anything in preparation for pregnancy?”
Pregnancy intention
Women were categorized into one of four pregnancy intention groups (“trying,” “thinking,” “maybe thinking,” or “not trying or thinking”) based on their answers to the “trying” (“Are you currently trying to get pregnant?”) or “thinking” (“Are you thinking about getting pregnant in the next year?”) questions. Women in the “trying,” “thinking,” or “maybe thinking” groups were asked about pregnancy preparations.
While the pregnancy preparation questions were asked to women based on their answers to the “trying” and “thinking” questions, within the statistical analysis we chose to use Desire to Avoid Pregnancy (DAP) score to measure pregnancy intention as it has been shown to be a better predictor of pregnancy (Hall et al., Citation2023).
DAP scale
The DAP scale is a psychometrically validated measure of a person’s preferences about a potential future pregnancy. The DAP scale has been validated for use within the UK and shown to be highly predictive of pregnancy (Hall et al., Citation2022a; Citation2022b). The DAP scale is a continuous measure, with scores ranging from 0 (no desire to avoid pregnancy) to 4 (high desire to avoid pregnancy) (Hall et al., Citation2022a).
Statistical analysis
To assess the determinants of pregnancy preparation, univariate ordered logistic regressions of the chosen variables were performed to investigate the relationship between the variable and pregnancy preparation. Multivariable ordered logistic regression was then used with the pregnancy preparation variable as the outcome measure. All variables, regardless of their significance in the univariate analysis, were included in the multivariable analysis. This was decided as most of the variables are correlated and therefore, while the variables may be insignificant on their own, there is potential for negative confounding, with relationships being revealed in the multivariable analysis. All variables were introduced simultaneously, and any variables found to be non-significant (p > .05) were removed using manual backward stepwise elimination, starting with the variable with the highest p value. The relationship between the variables and partner preparations was investigated using the same strategy.
Results
Participant characteristics
The 274 women asked about pregnancy preparations ranged in age from 16 to 47 years (median = 32, interquartile range [IQR] = 29 to 35, mean = 32), 87% were white and 86% were educated to at least undergraduate level. The majority described themselves as heterosexual (87%); most were married (71%) or in a relationship (25%); and most had a male partner (91.2%). Seventy-two percent of women had been pregnant at least once before. The sociodemographic characteristics of all women, as well as a breakdown by pregnancy intention, are shown in .
Table 1. Characteristics of all women and the women within each pregnancy intention group (“trying,” “thinking,” and “maybe thinking”).
The average DAP score for each pregnancy intention group is shown in .
Table 2. The average Desire to Avoid Pregnancy (DAP) score for the pregnancy intention groups.
Pregnancy preparations
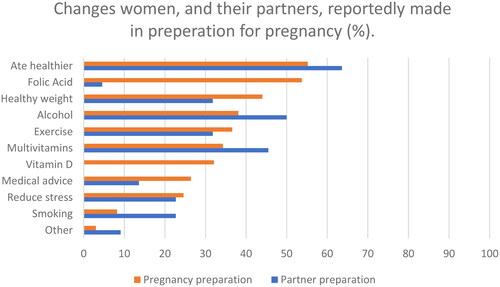
Of the 274 women asked about pregnancy preparations, less than half (n = 134, 49%) reported making any changes in preparation for pregnancy. Women who were preparing for pregnancy reported making between one and nine changes, with four being the average number of changes reported by women. The most common changes reported by women were “eating healthier” (n = 74; 55%) and “taking folic acid” (n = 72; 54%). All the changes reported are shown in .
Partner preparations
Ninety-two women were asked questions about partner preparations; only 22 women reported their partner making any changes in preparation for pregnancy (24%), 67 women reported no changes (73%), and 3 women did not have a partner (3%) (these women were subsequently dropped from analysis). Partners reportedly made between one and seven changes in preparation for pregnancy, with three being the average number of changes. The most common change reported was “eating healthily” (n = 14, 64%) followed by “stopping or cutting down alcohol” (n = 11, 50%). The other changes reportedly made by partners in preparation for pregnancy are shown in .
Reasons for not preparing
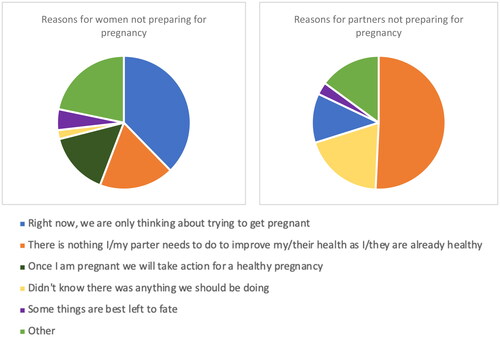
One hundred forty women reported making no changes in preparation for pregnancy; the reasons given for not preparing are shown in . The most common reason given for not preparing was “right now, I’m only thinking about trying to get pregnant” (n = 52, 38%), with other reasons including “there is nothing I need to do to improve my health in preparation for pregnancy because I am already healthy” (n = 25, 18%) and “once I am pregnant, I will take some action for a healthy pregnancy” (n = 21, 15%). The reasons given for why partners were not preparing are also show in ; the main reasons were “there is nothing my partner needs to do to improve their health in preparation for pregnancy because they are already healthy” (n = 34, 51%) and “we did not know there was anything my partner should be doing before pregnancy” (n = 13, 19%).
Pregnancy preparation analysis
Univariate analysis showed that relationship status and DAP score were both significantly associated with pregnancy preparation. Married women were more than five times more likely to report preparing for pregnancy than women not in a relationship (OR = 5.6, 95% CI = 1.2 to 26.25). All other variables—age, education, previous pregnancy, ethnicity, religion, and first language—were not significant ().
Table 3. Univariate and multivariable linear regressions of characteristics associated with pregnancy preparation.
Following multivariable analysis, DAP score was the only variable found to be significantly associated with pregnancy preparation (), with each increasing DAP point (range: 0–4) resulting in a 78% decrease in the odds of a woman reporting preparing for pregnancy (OR = 0.22, 95% CI = 0.15 to 0.34); that is, as a women’s desire to avoid pregnancy increases, the chances of her preparing for pregnancy significantly decreases. Relationship status became insignificant, suggesting that its association is likely mediated by DAP score. Previous work has shown that a women’s DAP score is associated with relationship status (Hall et al., Citation2022a).
Partner preparation analysis
DAP score was shown to be the only factor significantly associated with partner preparation following both univariate and multivariable analysis (); for every one-point increase in DAP score, the odds of a woman reporting her partner preparing for pregnancy decreased by 87% (OR = 0.13, 95% CI = 0.03 to 0.46).
Table 4. Univariate and multivariable linear regressions of characteristics associated with partner preparation.
Discussion
Overall, there appears, within the UK, to be a lack of awareness among the general population of the importance of preconception health. This not only is shown by the inadequate number of people preparing for pregnancy—less than half of women, and less than a quarter of partners, reported making any changes—but is also exposed in the reasons given for not preparing. When women were asked why they were not preparing for pregnancy, the most common reasons given were “right now, I’m only thinking about trying to get pregnant” and “once I am pregnant, I will take some action for a healthy pregnancy.” This highlights a lack of knowledge of the time that preparing for pregnancy can take and the impact that it can have, not only on pregnancy outcomes and the future health of offspring but also on the chances of getting pregnant (de Angelis et al., Citation2020; Godfrey et al., Citation2017; Poston et al., Citation2016; Sharma et al., Citation2013; Stephenson et al., Citation2018). Furthermore, research has shown that intervening during pregnancy is often too late and therefore preconception preparations are vital (Dodd et al., Citation2019; Janbek et al., Citation2019). Another common reason given for not preparing was “there is nothing I need to do to prepare for pregnancy as I am already healthy.” While this may be true (although previous research has shown people often overestimate their own health status (Maas et al., Citation2022)), every woman, regardless of their health, should be taking (at least) 400 mg of folic acid for at least 3 months prior to pregnancy to reduce the risk of neural tube defects (De-Regil et al., Citation2015; Mastroiacovo & Leoncini, Citation2011). Despite this recommendation, almost 50% of women who said they were preparing for pregnancy were not taking folic acid, indicating a lack of understanding of the importance of preconception folic acid. Within the UK, it is estimated that 85% of women take folic acid during pregnancy (NHS, Citation2021); however, as the critical period for folic acid supplementation is 3 months before and after conception (Stephenson et al., Citation2018), women who only start taking folic acid once they find out they are pregnant are likely to miss out on many of the benefits, highlighting the importance of preconception folic acid supplementation.
One of the main reasons given for why partners were not preparing was “we didn’t know that they should be doing anything,” suggesting that people are unaware of the impact that preconception partner health can have (Fleming et al., Citation2018; Hieronimus & Ensenauer, Citation2021; Lin et al., Citation2022).
DAP score was shown to be the only factor significantly associated with pregnancy preparations; as a woman’s desire to avoid pregnancy increased, the odds of her reporting preparing for pregnancy decreased. This is in line with previous research showing that pregnancy intention is linked to maternal health behaviors (Chatterjee & Sennott, Citation2020; Chuang et al., Citation2011). The DAP scale has been shown to provide nuance that is often missed by a single question (Hall, et al., Citation2023). For example, women who categorized themselves as only thinking about pregnancy within the next year had an average DAP score of 1.4 (indicating a relatively low desire to avoid pregnancy); previous work on the predictive ability of the DAP suggests that around 43% of these women would become pregnant within 12 months (Hall, et al., Citation2022b). Furthermore, almost 30% of the women in the “thinking” group were not using any contraception, in line with previous findings from similar studies (Chivers et al., Citation2020). Therefore, while they may only be thinking about getting pregnant, they still have a relatively high chance of pregnancy in the near future. In addition, it is recommended that women, and their partners, start to prepare for pregnancy before actively trying to conceive (so within the thinking period) to ensure that they receive the full benefits of preconception care (CDC, Citation2022; Stephenson et al., Citation2018, Citation2021). Consequently, women who are thinking about pregnancy make up a critical group, and it will be vital to increase the number of women within this group preparing for pregnancy in order to improve pregnancy outcomes.
Our work shows a relationship between pregnancy intention and pregnancy preparations. This finding is in line with the TPB (Ajzen & Madden, Citation1986). However, the TPB would predict no, or minimal, discrepancies between a formed intention for pregnancy and pregnancy preparation (Ajzen & Madden, Citation1986), and while those who were trying to get pregnant were more likely to report that they were preparing for pregnancy than those who were not, there were still many women with a formed pregnancy intention who were not preparing. This indicates that while there is clearly a relationship between pregnancy intention and pregnancy preparation, it may not be as simple as the one proposed by the TPB. Therefore, Bachrach and Morgan’s cognitive social model of intentions (Bachrach & Morgan, Citation2013) may be helpful in exploring this discrepancy. For example, the lack of schemas and structures relevant to pregnancy planning—the concept of planning for pregnancy, the action of taking folic acid when preparing for pregnancy, and the structure of the availability of preconception care services—are all likely to play a part in the observed gap between intention and action (Bachrach & Morgan, Citation2013).
The lack of awareness and low uptake of pregnancy preparations reported in this study fit with the findings of published literature (Daly et al., Citation2022; Maas et al., Citation2022; McDougall et al., Citation2021; McGowan et al., Citation2020), highlighting the need for strategies aimed at improving preconception knowledge. Previous studies have identified patients’ lack of knowledge of preconception care (Ojukwu et al., Citation2016) and other psychosocial factors (such as self-efficacy or perceived control, which have been shown to impact preventative health behaviors) as barriers to the provision of preconception care (Goossens et al., Citation2018; Smith et al., Citation1995). There are also barriers at the health service level including confusion over professional responsibility (i.e., who should be providing preconception care) (Poels et al., Citation2017; Stephenson et al., Citation2014) and health professionals only having access to patients after conception (Heyes et al., Citation2004). As a result, it would be important to ensure that any strategy aimed at improving uptake of preconception care took all these barriers into account.
These findings stress the need for normalizing conversations around pregnancy intention and pregnancy preparations, suggesting that clinicians should routinely ask people of reproductive age questions about pregnancy intentions (Hall, et al., Citation2023; Stephenson et al., Citation2021). Although the DAP scale has been shown to provide more nuance than other measures, it is made up of 14 questions, which limits its clinical use. Therefore, until there is further research into the clinical applications of the DAP, for example, as a digital tool or using a single DAP question or combination of DAP questions (Hall, et al., Citation2023), clinicians should routinely ask people of reproductive age questions such as “Are you thinking about pregnancy in the next year?” (Hammarberg et al., Citation2020; Stephenson et al., Citation2021) or “Can I help you with any reproductive health services today?” (Jones et al., Citation2020; Manze et al., Citation2020). Based on the response, clinicians should discuss preconception health with individuals who are thinking about pregnancy or contraception with those who wish to avoid pregnancy. Finally, this study also highlights the importance of including partners in these conversations to ensure that people know how impactful partner health can be.
Strengths and limitations
This analysis used data from a large, broadly representative dataset, suggesting generalizability of our findings. However, the women in the sample were relatively highly educated, possibly due to recruitment methods, which may limit the external validity of the findings. Furthermore, evidence shows that people often overreport health behaviors, particularly those that are “socially desirable.” Therefore, the results of this study likely show an overestimation of the level of pregnancy preparation in the UK, meaning that our findings are a “best-case scenario.”
Importantly, this study involved participants who were not pregnant, meaning that the data are prospective; this is novel, with most preconception studies being conducted in pregnant women retrospectively. This study also included data on partner preparations, which is an understudied area; however, partner preparations were reported by women and therefore could be at risk of bias. Furthermore, we were unable to analyze partner preparation by sex of partner, as the numbers of female partners were too small.
Within the P3 Study questionnaire, the questions on pregnancy preparation were about changes made in preparation for pregnancy. As a result, the data collected give us a guide to the relative likelihood of the changes women and their partners make in preparation for pregnancy but do not give us the absolute prevalence of those changes within the UK.
Conclusion
Overall, the results of this study suggest a lack of pregnancy preparation among women and their partners, potentially due to a lack of knowledge of the importance of preconception care and the impact that poor preconception health can have on pregnancy outcomes and the future health of offspring. This highlights the need for strategies aimed at increasing awareness of the importance of health before pregnancy within the UK to incorporate these behaviors within the schema of preparing for pregnancy. These strategies should be focused on people who are thinking about getting pregnant (not just those who are actively trying) to ensure that they have enough time to properly prepare for pregnancy, enabling them to receive the full benefits of better preconception health.
Supplemental Material
Download MS Word (6 MB)Acknowledgements
We would like to thank all the women who took part in the P3 study.
Disclosure Statement
The authors report there are no competing interests to declare.
Data Availability
The data that support the findings of this study are openly available in UCL Research Data Repository, DOI: 10.5522/04/23390072.
Additional information
Funding
Notes on contributors
Catherine Stewart
Catherine Stewart is a Research Assistant within the Sexual and Reproductive Health Research Team at UCL Institute for Women’s Health. She holds a BSc in Reproductive Biology from the University of Edinburgh and an MSc in Reproductive Science and Women’s Health from UCL. She has experience of both quantitative and qualitative research, with areas of interest including pregnancy preparation, pregnancy intentions and the utilization of maternal healthcare.
Jennifer Hall
Jennifer Hall is a Clinical Associate Professor and NIHR Advanced Fellow at the UCL Institute for Women’s Health. She is an Honorary Consultant in Public Health Medicine at UCLH and OHID. She is a mixed-methods researcher with skills and expertise in quantitative, qualitative, and psychometric methodologies and holds a PhD in Maternal Health and Epidemiology. She has national and international experience of working with clinical, public health, and academic colleagues, particularly around the measurement of pregnancy intention, preconception care, and the detection and management of unplanned pregnancies, bringing a life course approach to reproductive health services and research.
References
- Ajzen, I., & Madden, T. J. (1986). Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology, 22(5), 453–474. https://doi.org/10.1016/0022-1031(86)90045-4
- Bachrach, C. A., & Morgan, S. P. (2013). A cognitive-social model of fertility intentions. Population and Development Review, 39(3), 459–485. https://doi.org/10.1111/j.1728-4457.2013.00612.x
- Bath, S. C., Steer, C. D., Golding, J., Emmett, P., & Rayman, M. P. (2013). Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet (London, England), 382(9889), 331–337. https://doi.org/10.1016/s0140-6736(13)60436-5
- Bortolus, R., Oprandi, N. C., Rech Morassutti, F., Marchetto, L., Filippini, F., Agricola, E., Tozzi, A. E., Castellani, C., Lalatta, F., Rusticali, B., & Mastroiacovo, P. (2017). Why women do not ask for information on preconception health? A qualitative study. BMC Pregnancy and Childbirth, 17(1), 5. https://doi.org/10.1186/s12884-016-1198-z
- CDC. (2022). Planning for pregnancy. Retrieved December 5, 2022, from https://www.cdc.gov/preconception/planning.html
- Chatterjee, E., & Sennott, C. (2020). Fertility intentions and maternal health behaviour during and after pregnancy. Population Studies, 74(1), 55–74. https://doi.org/10.1080/00324728.2019.1672881
- Chivers, B. R., Boyle, J. A., Lang, A. Y., Teede, H. J., Moran, L. J., & Harrison, C. L. (2020). Preconception health and lifestyle behaviours of women planning a pregnancy: A cross-sectional study. Journal of Clinical Medicine, 9(6), 1701. https://doi.org/10.3390/jcm9061701
- Chuang, C. H., Hillemeier, M. M., Dyer, A. M., & Weisman, C. S. (2011). The relationship between pregnancy intention and preconception health behaviors. Preventive Medicine, 53(1–2), 85–88. https://doi.org/10.1016/j.ypmed.2011.04.009
- Daly, M. P., White, J., Sanders, J., & Kipping, R. R. (2022). Women’s knowledge, attitudes and views of preconception health and intervention delivery methods: A cross-sectional survey. BMC Pregnancy and Childbirth, 22(1), 729. https://doi.org/10.1186/s12884-022-05058-3
- de Angelis, C., Nardone, A., Garifalos, F., Pivonello, C., Sansone, A., Conforti, A., Di Dato, C., Sirico, F., Alviggi, C., Isidori, A., Colao, A., & Pivonello, R. (2020). Smoke, alcohol and drug addiction and female fertility. Reproductive Biology and Endocrinology, 18(1), 21. https://doi.org/10.1186/s12958-020-0567-7
- De-Regil, L. M., Peña-Rosas, J. P., Fernández-Gaxiola, A. C., & Rayco-Solon, P. (2015). Effects and safety of periconceptional oral folate supplementation for preventing birth defects. The Cochrane Database of Systematic Reviews, 2015(12), Cd007950. https://doi.org/10.1002/14651858.CD007950.pub3
- Dodd, J. M., Louise, J., Deussen, A. R., Grivell, R. M., Dekker, G., McPhee, A. J., & Hague, W. (2019). Effect of metformin in addition to dietary and lifestyle advice for pregnant women who are overweight or obese: The GRoW randomised, double-blind, placebo-controlled trial. The Lancet. Diabetes & Endocrinology, 7(1), 15–24. https://doi.org/10.1016/S2213-8587(18)30310-3
- Fleming, T. P., Watkins, A. J., Velazquez, M. A., Mathers, J. C., Prentice, A. M., Stephenson, J., Barker, M., Saffery, R., Yajnik, C. S., Eckert, J. J., Hanson, M. A., Forrester, T., Gluckman, P. D., & Godfrey, K. M. (2018). Origins of lifetime health around the time of conception: Causes and consequences. Lancet (London, England), 391(10132), 1842–1852. https://doi.org/10.1016/s0140-6736(18)30312-x
- Godfrey, K. M., Reynolds, R. M., Prescott, S. L., Nyirenda, M., Jaddoe, V. W., Eriksson, J. G., & Broekman, B. F. (2017). Influence of maternal obesity on the long-term health of offspring. The Lancet. Diabetes & Endocrinology, 5(1), 53–64. https://doi.org/10.1016/s2213-8587(16)30107-3
- Goossens, J., De Roose, M., Van Hecke, A., Goemaes, R., Verhaeghe, S., & Beeckman, D. (2018). Barriers and facilitators to the provision of preconception care by healthcare providers: A systematic review. International Journal of Nursing Studies, 87, 113–130. https://doi.org/10.1016/j.ijnurstu.2018.06.009
- Greenberg, J., Bell, S., Guan, Y., & Yu, Y. (2011). Folic Acid supplementation and pregnancy: More than just neural tube defect prevention. Reviews in Obstetrics and Gynecology, 4(2), 52–59.
- Hall, J., Barrett, G., & Rocca, C. (2022a). Evaluation of the Desire to Avoid Pregnancy Scale in the UK: A psychometric analysis including predicitive validity. BMJ Open, 12(7), e060287. https://doi.org/10.1136/bmjopen-2021-060287
- Hall, J., Barrett, G., Stephenson, J., Rocca, C., & Edelman, N. (2022b). Predictive ability of the desire to avoid pregnancy scale. Reproductive Health, 20(1), 1–7. https://doi.org/10.1101/2022.10.17.22281028
- Hall, J., Barrett, G., Stephenson, J., Edelman, N., & Rocca, C. (2023). The Desire to Avoid Pregnancy Scale: Clinical considerations and comparison with other questions about pregnancy preferences. BMJ Sexual & Reproductive Health, 49(3), 167–175. https://doi.org/10.1136/bmjsrh-2022-201750
- Hammarberg, K., Hassard, J., de Silva, R., & Johnson, L. (2020). Acceptability of screening for pregnancy intention in general practice: A population survey of people of reproductive age. BMC Family Practice, 21(1), 40. https://doi.org/10.1186/s12875-020-01110-3
- He, Y., Pan, A., Hu, F. B., & Ma, X. (2016). Folic acid supplementation, birth defects, and adverse pregnancy outcomes in Chinese women: A population-based mega-cohort study. The Lancet, 388, S91. https://doi.org/10.1016/S0140-6736(16)32018-9
- Heyes, T., Long, S., & Mathers, N. (2004). Preconception care: Practice and beliefs of primary care workers. Family Practice, 21(1), 22–27. https://doi.org/10.1093/fampra/cmh106
- Hieronimus, B., & Ensenauer, R. (2021). Influence of maternal and paternal pre-conception overweight/obesity on offspring outcomes and strategies for prevention. European Journal of Clinical Nutrition, 75(12)volume, 1735–1744. https://doi.org/10.1038/s41430-021-00920-7
- Hill, B., Hall, J., Skouteris, H., & Currie, S. (2020). Defining preconception: Exploring the concept of a preconception population. BMC Pregnancy and Childbirth, 20(1), 280. https://doi.org/10.1186/s12884-020-02973-1
- Ignaszak-Kaus, N., Ozegowska, K., Piekarski, P., Pawelczyk, L., & Jędrzejczak, P. (2018). Planning and preparation for pregnancy among women with and without a history of infertility. Ginekologia Polska, 89(2), 74–79. https://doi.org/10.5603/GP.a2018.0013
- Janbek, J., Sarki, M., Specht, I. O., & Heitmann, B. L. (2019). A systematic literature review of the relation between iron status/anemia in pregnancy and offspring neurodevelopment. European Journal of Clinical Nutrition, 73(12), 1561–1578. https://doi.org/10.1038/s41430-019-0400-6
- Jones, H. E., Calixte, C., Manze, M., Perlman, M., Rubin, S., Roberts, L., & Romero, D. (2020). Primary care patients’ preferences for reproductive health service needs assessment and service availability in New York Federally Qualified Health Centers. Contraception, 101(4), 226–230. https://doi.org/10.1016/j.contraception.2019.12.003
- Law, D. C. G., Maclehose, R. F., & Longnecker, M. P. (2007). Obesity and time to pregnancy. Human Reproduction (Oxford, England), 22(2), 414–420. https://doi.org/10.1093/humrep/del400
- Lin, J., Gu, W., & Huang, H. (2022). Effects of paternal obesity on fetal development and pregnancy complications: A prospective clinical cohort study. Frontiers in Endocrinology, 13, 826665. https://doi.org/10.3389/fendo.2022.826665
- Maas, V. Y. F., Poels, M., Kievit, M. H. D., Hartog, A. P., Franx, A., & Koster, M. P. H. (2022). Planning is not equivalent to preparing, how Dutch women perceive their pregnancy planning in relation to preconceptional lifestyle behaviour change-a cross-sectional study. BMC Pregnancy and Childbirth, 22(1), 577. https://doi.org/10.1186/s12884-022-04843-4
- Manze, M. G., Romero, D. R., Sumberg, A., Gagnon, M., Roberts, L., & Jones, H. (2020). Women’s perspectives on reproductive health services in primary care. Family Medicine, 52(2), 112–119. https://doi.org/10.22454/FamMed.2020.492002
- Marchi, J., Berg, M., Dencker, A., Olander, E. K., & Begley, C. (2015). Risks associated with obesity in pregnancy, for the mother and baby: A systematic review of reviews. Obesity Reviews : An Official Journal of the International Association for the Study of Obesity, 16(8), 621–638. https://doi.org/10.1111/obr.12288
- Mastroiacovo, P., & Leoncini, E. (2011). More folic acid, the five questions: Why, who, when, how much, and how. BioFactors (Oxford, England), 37(4), 272–279. https://doi.org/10.1002/biof.172
- McDougall, B., Kavanagh, K., Stephenson, J., Poston, L., Flynn, A. C., & White, S. L. (2021). Health behaviours in 131,182 UK women planning pregnancy. BMC Pregnancy and Childbirth, 21(1), 530–541. https://doi.org/10.1186/s12884-021-04007-w
- McGowan, L., Lennon-Caughey, E., Chun, C., McKinley, M. C., & Woodside, J. V. (2020). Exploring preconception health beliefs amongst adults of childbearing age in the UK: A qualitative analysis. BMC Pregnancy and Childbirth, 20(1), 41. https://doi.org/10.1186/s12884-020-2733-5
- Means, R. T. (2020). Iron deficiency and iron deficiency anemia: Implications and impact in pregnancy, fetal development, and early childhood parameters. Nutrients, 12(2), 447. https://doi.org/10.3390/nu12020447
- NHS. (2020). Statistics on obesity, physical activity and diet. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020/part-3-adult-obesity-copy
- NHS. (2021). NHS Maternity Statistics, England - 2020-21. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2020-21
- Ojukwu, O., Patel, D., Stephenson, J., Howden, B., & Shawe, J. (2016). General practitioners’ knowledge, attitudes and views of providing preconception care: A qualitative investigation. Upsala Journal of Medical Sciences, 121(4), 256–263. https://doi.org/10.1080/03009734.2016.1215853
- Pearce, E. N. (2013). Monitoring and effects of iodine deficiency in pregnancy: Still an unsolved problem? European Journal of Clinical Nutrition, 67(5), 481–484. https://doi.org/10.1038/ejcn.2012.215
- Poels, M., Koster, M. P., Franx, A., & van Stel, H. F. (2017). Healthcare providers’ views on the delivery of preconception care in a local community setting in the Netherlands. BMC Health Services Research, 17(1), 92. https://doi.org/10.1186/s12913-017-2051-4
- Poston, L., Caleyachetty, R., Cnattingius, S., Corvalán, C., Uauy, R., Herring, S., & Gillman, M. W. (2016). Preconceptional and maternal obesity: Epidemiology and health consequences. The Lancet. Diabetes & Endocrinology, 4(12), 1025–1036. https://doi.org/10.1016/S2213-8587(16)30217-0
- Sharma, R., Biedenharn, K. R., Fedor, J. M., & Agarwal, A. (2013). Lifestyle factors and reproductive health: Taking control of your fertility. Reproductive Biology and Endocrinology, 11(1), 66. https://doi.org/10.1186/1477-7827-11-66
- Smith, M. S., Wallston, K. A., & Smith, C. A. (1995). The development and validation of the Perceived Health Competence Scale. Health Education Research, 10(1), 51–64. https://doi.org/10.1093/her/10.1.51
- Stephenson, J., Patel, D., Barrett, G., Howden, B., Copas, A., Ojukwu, O., Pandya, P., & Shawe, J. (2014). How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PloS One, 9(7), e103085. https://doi.org/10.1371/journal.pone.0103085
- Stephenson, J., Heslehurst, N., Hall, J., Schoenaker, D. A. J. M., Hutchinson, J., Cade, J. E., Poston, L., Barrett, G., Crozier, S. R., Barker, M., Kumaran, K., Yajnik, C. S., Baird, J., & Mishra, G. D. (2018). Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet (London, England), 391(10132), 1830–1841. https://doi.org/10.1016/S0140-6736(18)30311-8
- Stephenson, J., Schoenaker, D. A., Hinton, W., Poston, L., Barker, M., Alwan, N. A., Godfrey, K., Hanson, M., & de Lusignan, S. (2021). A wake-up call for preconception health: A clinical review. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 71(706), 233–236. https://doi.org/10.3399/bjgp21X715733
- Zimmermann, M. B. (2009). Iodine deficiency in pregnancy and the effects of maternal iodine supplementation on the offspring: A review. The American Journal of Clinical Nutrition, 89(2), 668s–672s. https://doi.org/10.3945/ajcn.2008.26811C