Abstract
Relatives and close friends provide life-long support as informal carers to those living with psychosis. We introduce a model for training informal carers in cognitive behaviour therapy (CBT) for psychosis, called Psychosis Recovery by Enabling Adult Carers at Home (Psychosis REACH). The model aims to address the carers’ own emotional needs and at the same time build their capabilities of promoting the recovery trajectory of the person they care for. We delivered two- and five-day workshops, underpinned by the Psychosis REACH model, to a cohort of 95 self-identified carers recruited via a charitable organisation in Canada. In a single-group before-and-after design, carers’ anxiety, depression and mental well-being significantly improved within a few days. A handful of carers who returned data for their cared-for-person after the end of training, observed either no change or a positive change in functioning. Our findings generated hypotheses that deserve further research to test whether training large groups of relatives and friends in CBT-informed care for psychosis can improve their anxiety, depression and mental well-being in the context of their caring role, as well as improve the functioning of those they care for.
PUBLIC INTEREST STATEMENT
Schizophrenia is a complex, difficult to treat, long-term mental illness. People with schizophrenia rely on their relatives and close friends for life-long support in the community; however, caring for someone with schizophrenia can take its toll on the carer’s well-being. CBT is shown to improve symptoms, quality of life and functioning in schizophrenia, but it is usually only delivered by professionals. Training relatives and friends in CBT-informed care for schizophrenia could help improve the carers’ well-being, as well as improve the recovery trajectory of those they care for. We delivered CBT-informed care workshops to 95 self-identified carers of people with schizophrenias via a charitable organisation in Canada. Questionnaires before and after the workshops indicated a positive shift in carers’ anxiety, depression and mental well-being. Future research needs to measure the effect of CBT-informed care by relatives and friends on the functioning of those cared-for with schizophrenia in the community.
Competing Interest
For the remaining authors, no conflict of interests were declared.
1. Introduction
Schizophrenia is a complex, difficult to treat, long-term mental illness. Although it is less common than depression and anxiety, it bears a greater direct cost for the individual, their family and the healthcare system, because it is associated with high co-morbidity and mortality, severe impairment of work and social functioning, significant healthcare utilisation and a need for life-long emotional and practical support for those recovering in the community. The cost of schizophrenia has been estimated at £6.7 billion per year in England (in 2004–2005), of which £2 billion are direct healthcare costs (Mangalore & Knapp, Citation2007).
Informal carers—relatives or close friends who provide substantial care without being paid—make a significant economic and moral contribution through life-long support to those with schizophrenia in the community. Due to resource constraints in public services, informal carers increasingly assume duties previously performed by professionals, for example, dealing with residual positive symptoms, negative symptoms, risk to self and others, comorbid depression, anxiety and substance misuse, medication side-effects and internalised stigma (Andrews, Knapp, & McCrone et al., Citation2012; Eassom et al., Citation2014). Carer involvement can improve outcomes with pharmacotherapy (Glick, Stekoll, & Hays, Citation2011), prevent relapse and hospitalisation (Bird et al., Citation2010) and instigate prompt help-seeking (Fridgen et al., Citation2013).
Caring for someone with psychosis can take its toll on the carer’s health. Carers of family members with psychosis have poorer health outcomes compared to the general population and to other carers (Gupta et al., Citation2015; Hayes et al., Citation2015). Existing psychosocial interventions for carers of people with psychosis include family therapy and one-to-one cognitive behaviour therapy (CBT) (see reviews by Bird et al., Citation2010; Lobban et al., Citation2013), as well as respite arrangements, NHS carer support services and carer health checks (see review by Yeandle & Wigfield, Citation2011). Other existing interventions that can reduce carer burden and distress include psychoeducation and support groups (review Yesufu-Udechuku et al., Citation2015), or self-management toolkits (e.g. Fadden, James & Pinfold, Citation2012; Lobban et al., Citation2013; Rotondi et al., Citation2010).
CBT is a well established psychological treatment for anxiety and depression and has shown to improve refractory symptoms, quality of life and social functioning in psychosis (Tai & Turkington, Citation2009). The basic premise of CBT is that we can influence our emotional state and mental well-being in two ways: first, by changing the way we perceive and respond to our day-to-day experiences—whether these experiences are psychotic symptoms, care-giving or random life events; second, by increasing our meaningful, pleasurable and challenging day-to-day activities—whether these activities are social, personal, recreational or occupational.
The delivery of therapeutic interventions, like CBT, can be scaled up to reach more people by training lay members of the community in techniques traditionally used only by professionals. This is known as a “task-shifting” approach, promoted in low- and middle-income countries where resources for mental healthcare are limited (Petersen, Lund, Bhana, Flisher, & Health, Citation2012). Training carers in CBT requires a new conceptual and practical model that goes beyond the task-shifting approach of lay training. This is because carers are emotionally affected by the illness of their relative or friend and may also be vulnerable themselves; therefore, a suitable model for training carers in therapeutic skills needs to prepare them emotionally and help them use these skills within the dynamics of a personal relationship while having a balance between looking after themselves and their loved ones.
This article introduces a model for training relatives and friends in CBT-informed care for psychosis, called Psychosis Recovery by Enabling Adult Carers at Home (Psychosis REACH). Psychosis REACH takes into account the carers’ own emotional needs and at the same time builds their capabilities of promoting the recovery trajectory of the person they care for. We have applied this model of training in a naturalistic setting with a cohort of self-identified carers. Our main aim was to generate hypotheses and inform the design of a future randomised controlled trial (RCT) that will test the value of training large groups of relatives and friends in CBT-informed care for psychosis with regard to improving the carers’ well-being and the functioning of those they care for.
2. Methods
2.1. Design
We invited all relatives and friends of people with psychosis who were registered with the Schizophrenia Society of Ontario (SSO)—a charitable organisation in Canada—to attend a series of CBT-informed care in psychosis training workshops. The workshops were underpinned by the Psychosis REACH model and were delivered in two formats: standard training (2 days) and enhanced training (5 days). In a single-group before-and-after (pretest-posttest) design, we collected data from the workshop participants through self-completed pen and paper questionnaires at baseline (at the start of the first day of training) and post-training (at the end of the last day of training).
2.2. The Psychosis REACH model
We developed the Psychosis REACH model because training carers in CBT is different to the task-shifting approach of teaching therapeutic skills to lay people, since carers are emotionally involved and affected by their relative’s experience of psychosis. The model has 4 levels: 1. Emotional Readiness 2. Skills Building 3. Behaviour Change and 4. Recovery (Figure ).
Figure 1. Psychosis REACH (Recovery by Enabling Adult Carers at Home): A model for training relatives and friends in CBT-informed care for psychosis.
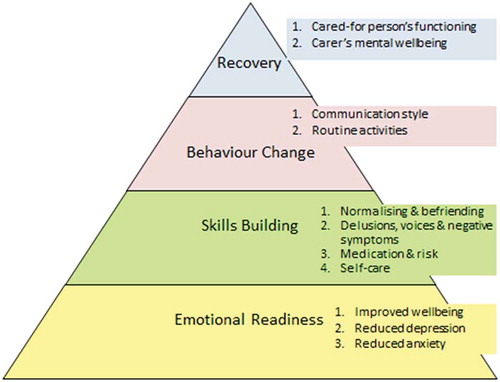
1. Emotional readiness: We aim to instil hope and optimism that carers can influence the recovery of their loved ones at home, while balancing their caring responsibilities with their own needs and wishes. We intend to help carers activate self-nurturing, reduce their own stress and challenge their perceptions of guilt and hopelessness.
2. Skills building: We teach carers how to initiate conversations, question and respond to those who may be distressed or experience psychotic symptoms, make sense and normalise the psychotic symptoms that they observe, address issues with antipsychotic medication, work with voices and strange beliefs, tackle apathy and self-neglect, prevent relapse and manage risk.
3. Behaviour change: Our aim is to influence the style of communication and daily activities at home between the carer and the cared-for-person. Maintaining emotional neutrality, avoiding over-critical or over-dependant relationships and planning meaningful activities unrelated to the illness are important behaviour changes in the context of caring for someone with psychosis.
4. Recovery: Within the remit of the Psychosis REACH model, recovery is the intended outcome of improving the functioning of people living with psychosis and of improving or maintaining the mental well-being of the relatives and friends who care for them.
2.3. Training workshops
The training used a variety of learning methods, such as expert presentations, role plays, brief DVD demonstrations, quizzes and exercises. The content of the workshops include introductory CBT techniques (normalising, befriending and formulating), more advanced CBT techniques for delusions, voices and negative symptoms, general psychiatry techniques for medication and risk, and specific CBT techniques to boost mood and deal with anxiety and stress. Table gives an indicative content outline for the workshops.
Table 1. Content of CBT-informed care for psychosis workshops
2.4. Data collection
We asked carers some basic information about themselves (gender, age, education, employment) and about their caring role (whether they consider themselves as “carers”, how long they have been caring for their relative/friend with psychosis and how many hours per day they spend caring). We also asked the age of the cared-for-person, their relationship with the carer and how ill the person with psychosis had been over previous 2 months (see ).
We used two standardised questionnaires to assess participating carers’ emotional readiness before and after the training: the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, Citation1983), as a measure of presence and severity of specific emotional problems (anxiety and depression), and the Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (Tennant et al., Citation2007), as a measure of general emotional well-being.
HADS is a universal clinical tool that can indicate not only the presence of common mental health problems, such as anxiety and depression, but also the need for signposting people for help based on established cut-off points. The HADS includes 14 items rated on a 0–3 scale measuring the presence of anxiety (7 items, e.g. “I feel tense or ‘wound up’”) or depression (7 items, e.g. “I feel as if I am slowed down”). Questions about depression and anxiety are scored separately, with lower scores indicating less anxiety/depression. Conventional cut-off scores are: 7 or less, no clinical anxiety/depression and 8–10 mild, 11–14 moderate and 15–21 severe anxiety/depression.
WEMWBS has 14 statements (e.g. feeling optimistic about the future, feeling useful, feeling relaxed, etc.) which the rater scores according to how often they experience that statement over the past two weeks, using a 5-point scale: 1 = None of the time, 2 = Rarely, 3 = Some of the time, 4 = Often, 5 = All of the time. The total WEMWBS score ranges from 14 to 70 with higher scores denoting better mental well-being. A cut-off score of 43.5 and below (Bianco, Citation2012) has been suggested as indicative of depressive symptoms. The WEMWBS has been shown to be responsive to changes in the mental well-being of the general population following CBT-based health promotion (Powell et al., Citation2013).
To assess the potential of Psychosis REACH to influence the functioning of the cared-for-person from the perspective of the carer, we used a carer-reported version of the Personal and Social Performance (PSP) Scale (Morosini, Magliano, Brambilla, Ugolini, & Pioli, Citation2000). The PSP assesses the presence and severity of difficulties in four domains: a. socially useful activities, including work and study; b. personal and social relationships; c. self-care; d. disturbing and aggressive behaviours. The carer scored the level of difficulty that their relative/friend had in each of these four domains, and the final score took into account additional affected domains of functioning out of a given checklist of 11 domains, including healthcare, home care, intimate and sexual relationships and financial management. The higher the final PSP score, the better the cared-for-person’s mental health and functioning.
2.5. Data analysis
We used descriptive statistics (means, standard deviations, median and range values for continuous variables and frequencies and percentages for categorical variables) to map the demographic and clinical characteristics of our sample. We checked for normality of distribution of our continuous variables (e.g. age, HADS, WEMWBS and PSP scores). We analysed the HADS and WEMWBS in two ways: first, as continuous variables, by using paired sample t-tests to explore changes in HADS and WEMWBS total scores pre-post training; second, as categorical variables, by grouping scores together according to established cut-off points (as detailed in the data collection section above). We calculated the Cohen’s d for one-sample repeated measures in each continuous variable (HADS and WEMWBS) by diving the mean difference in scores pre-post by the standard deviation of the difference in scores pre-post.
We grouped together WEMWBS scores of 43 and below as “low well-being” and scores higher than 43 as “high well-being”. We grouped HADS scores into four groups indicating no depression/anxiety (0–7) and mild (8–10), moderate (11–14) or severe (15–21) depression/anxiety. We used the McNemar and the McNemar-Bowker tests (for 2 × 2 and 4 × 4 tabulations of the WEMWNS and HADS, respectively) to determine whether there was any significant change pre-post training in the proportions of carers with low vs. high well-being on the WEMWBS and in the proportion of carers with no depression or anxiety vs. mild/moderate/severe depression or anxiety on the HADS.
We explored individual items of the HADS and WEMWBS to understand which ones changed pre-post training. We analysed responses to each WEMWBS item pre-post training as a categorical variable with 2 levels: “low well-being” for scores of 1, 2 and 3 (never, rarely, sometimes) and “high well-being” for scores of 4 and 5 (often, all the time). We analysed responses to each HADS item pre-post training as a categorical variable with 4 levels (none, mild, moderate, severe). We plotted carer responses to each HADS and WEMWBS item before and after the training and visually inspected the resulting histograms to identify those items that showed a pronounced shift towards the right-hand side (indicating a positive emotional change in that item).
We tabulated PSP responses to determine the level of functional impairment identified by carers for their cared-for-person during training and at follow-up (6 weeks later). We used cross-tabulations that visually represented changes in the distribution of PSP scores for different levels of functional impairment (absent, mild, manifest, marked, severe, very severe). Due to the small number of participants, we did not carry out any statistical tests on the PSP but we visually inspected the data on a case-by-case basis to observe any notable changes.
2.6. Ethical considerations
We have received ethics clearance by the Queen’s University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board (Ethics ROMEO # 6019427). We have adhered to the code of conduct of the SSO which hosted the training and is the custodian of all the data. All participating carers were given an information sheet and a consent form to sign before the training started and could opt out from completing the questionnaires or could leave any questionnaires or any items within the questionnaires blank.
3. Results
3.1. Baseline characteristics
The relatives and friends (n = 95) in our sample were in their late fifties (m = 57 yrs, sd = 12), mostly women (82%), Caucasian (80%), with higher education (90%), who lived in a household with others (92%) and were in paid employment (67%). Not all of them (87%) described themselves as “carers”. Those performing a caring role did so for over a decade (n = 80, m = 13 yrs, sd = 13 yrs). Most participants were parents (80%) of someone with psychosis and the rest had a parent (5%) or a sibling (8%) or knew someone else (e.g. in-laws or friends) (6%) with psychosis. The typical cared-for-person was in their mid-thirties (n = 80, m = 34 yrs, sd = 14) and experienced marked/moderate (53%) or severe/extreme (17%) illness over the previous two months; 30% had either no symptoms or experienced threshold/mild symptoms of psychosis. Only 11% of participants reported that they performed caring duties for most of the day; 47% cared for someone for part of the day and 42% for less than 1 h/day.
3.2. Carer’s emotional readiness
Before the training (baseline), mean scores for our participating relatives on HADS indicated mild anxiety (n = 76, HADS anxiety sub-scale m = 8.6, sd = 4) and no depression (n = 81, HADS depression sub-scale m = 6.7, sd = 4.7). When scores were grouped according to established cut-offs, 29% of carers had moderate-to-severe anxiety and 20% moderate-to-severe depression. Similarly, mean scores on the WEMWBS denoted an average high level of well-being across carers (n = 77, WEMWBS total score m = 50.97, sd = 10.4), but when using established cut-offs for different levels of well-being, 23% of carers at baseline scored in the range of “low well-being” (Tables and ).
Table 2. HADS and WEMWBS, expressed as continuous variables, at baseline and post-training
Table 3. HADS and WEMWBS, expressed as categorical variables, at baseline and post-training
After the training, paired sample t-tests (n = 64) indicated: a small but significant mean increase in carers’ well-being by 2.1 points (sd = 4.6, p = 0.001, Cohen’s d = 0.2); a medium effect in reduction of depression by 1.3 point (sd = 3.4, p = 0.004, Cohen’s d = 0.4); and a medium effect of reduction in anxiety by 1.7 point (sd = 4.4, p = 0.005, Cohen’s d = 0.4). These results are shown in Table .
There were notable reductions post-training by 19% and 15% in the proportions of carers who scored below the HADS cut-off point for clinical anxiety and depression respectively; this means 19% more carers were anxiety-free and 15% more carers were depression-free post-training. In addition, 10% of carers with moderate depression moved to mild depression and 13% of carers with moderate anxiety moved to mild anxiety. There was no real change in the proportion of carers with WEMWBS scores below the cut-off point for low well-being (from 17% to 16%) (Table )
When analysing individual questionnaire items, we identified only 2/14 HADS items which may explain improved scores post-training in anxiety (“I feel tense and wound up”) and in depression (“I have lost interest in my appearance”). We identified 5/14 WEMWBS items for which improved scores may account for the small shift towards better well-being post-training: “feeling relaxed”, “feeling optimistic about the future”, “feeling cheerful”, “feeling loved” and “feeling useful”. Surprisingly, there was no notable shift in items that reflected cognitive change as we expected, for example, in the carers’ perceived ability to problem-solveing or think clearly.
3.3. Cared-for-person’s functioning
For the small number of carers who provided data for the person they cared for (n = 20) at the end of training, the mean PSP score attributed to their cared-for-person at baseline was 53.3 (sd = 22.3). This was indicative of marked difficulties (e.g. at work, relationships or self-care). There was a general shift in the distribution of carer-reported PSP scores for their cared-for-person towards better functioning at 6 weeks follow-up. From the handful of PSP data available at follow-up (n = 6), the mean PSP score was 67.2 (sd = 22.5), indicating manifest and not marked difficulties. Out of the six carers who gave data follow-up data, three reported no change in the PSP scores and three reported a positive change (n = 1 from marked difficulties to mild, n = 1 from manifest difficulties to good functioning and n = 1 from mild difficulties to excellent functioning).
4. Discussion
The well-being of carers in our sample at baseline—measured by the WEMWBS—lies within a margin of 1 point (scores rounded to the nearest integer) (m = 51, sd = 10.4) to the general population in England (m = 52, sd = 8.7) (WEMWBS Population Norms in Health Survey for England data, Citation2011; we have no comparable data for Canada). This means that well-being is not necessarily compromised by caring for someone with psychosis.
In our sample, the average score on the HADS was below the indicated cut-off point for depression and within the “mild” range for anxiety on the corresponding HADS subscales. When we converted the HADS scores into categories (denoting no, mild, moderate, severe depression or anxiety), 47% of carers scored above the cut-off point for presence of depression and 68% for presence of anxiety, which is much higher than the point prevalence of the two conditions in the general population. This means that an intervention for depression and anxiety may be relevant for a large sub-group, but not for the whole population, of those caring for people with psychosis.
Notably, after our CBT training, 15% and 19% more carers were free of depression and anxiety respectively and there was a shift towards more mild depression and anxiety for those with moderate symptoms at baseline. Attending CBT training did not intend to replace additional or alternative help for those carers with clinical symptoms at baseline; in fact, it intended to make carers aware of their needs and encouraged them to actively seek help. In the context of CBT-informed care, improving mental health outcomes for carers with indicated depression and anxiety at baseline is the cornerstone of the Psychosis REACH model, because carers who are emotionally vulnerable need to feel better in themselves before they are ready to help those around them.
Previous skills training in CBT for carers of people with anorexia (e.g. Grover et al., Citation2011) and in motivational interviewing for carers of young adults with cannabis use (Smeerdijk et al., Citation2012, Citation2014, Citation2015) have showed promise for patient outcomes. In this study, we were only able to tentatively gauge outcomes for the cared-for-person by training carers to assess and report functioning using the PSP scale for those they cared for. We only had a handful of carers who returned data for their cared-for-person after the end of training, but the direction of this data was towards a positive shift in functioning, if at all.
4.1. Limitations
As this was a naturalistic study with no control group, we cannot draw inferences about the impact of CBT-informed care for psychosis training on carer well-being; however, our findings have generated two hypotheses that deserve to be tested in a future RCT. The first hypothesis is that a training programme underpinned by the Psychosis REACH model could improve carers’ anxiety and depression and incrementally improve their general mental well-being. The second hypothesis is that the functioning of someone with psychosis—as assessed by their carer—can improve after their relatives and friends are trained in CBT-informed care.
A future RCT is necessary so that a control group can adjusts for the confounding non-specific effects of a group intervention. This will tell us whether it is the CBT training programme itself, rather than the social interaction of attending a peer group, that accounts for changes in carers’ self-reported depression, anxiety and mental well-being. To explore the mechanisms by which carer training influences the functioning of the cared-for-person, we need to capture the impact that this training has on the carer’s communication style and daily activities in the context of their caring role. To do this, we need to select appropriate and sensitive measures that assess the carers’ behaviour at home, while supporting them to implement their newly acquired CBT knowledge and skills. We will also ask the carers to specify the type of psychosis their relative was diagnosed with and what medication their relative was receiving at the time, to allow for sub-group analyses.
Repeated measurement of carer mental health outcomes, before and after the training, took place in the space of 2–5 days. This is within the test-retest period for the outcome measures, and as such, it cannot be taken as a reliable or specific indicator of change in mental well-being due to the CBT training; the result could be spurious and attributed to the effect of measurement or of participating in the study itself rather than the effect of CBT training per se. A future RCT will include a longer follow-up to establish whether the same outcomes can be observed and sustained long after the end of training.
Finally, the group of carers in our sample is not representative of all carers within and across different countries. Educated, white, middle-aged mothers dominated our Canadian sample. Also, carers who put themselves forward to attend training may be a self-selected group with higher well-being who have the motivation and time to attend the training. We could expect that carers in developed counties like Canada have a greater level of well-being than in countries with less resources and education around mental health.
5. Conclusions
Our application of the Psychosis REACH model to a training programme in a naturalistic setting with a cohort of carers recruited via a charitable organisation has led to two questions for a future RCT. First, can CBT-informed care for psychosis training improve anxiety, depression and mental well-being for carers, as well as improve the functioning of those they care for? Second, are these improved outcomes mediated by a change in the carers’ communication style and daily activities following their training? Although training carers can be seen as a task-shifting initiative that allows lay people to deliver therapeutic interventions usually restricted to professionals, the Psychosis REACH model does not aim to turn relatives and friends into therapists; instead, it aims to help cares be more effective in looking after their loved ones while maintaining their own mental well-being.
Additional information
Funding
Notes on contributors
Douglas Turkington
Professor Douglas Turkington has 30 years experience of cognitive behavioural therapy (CBT) for people with schizophrenia. He has led on numerous randomised controlled trials of CBT as compared to befriending, cognitive remediation and treatment as usual in schizophrenia. He was the chief investigator of the largest pragmatic trial of CBT delivered by psychiatric nurses. Currently he is working on the linguistics of thought disorder and voice hearing and on the application of perceptual control theory within method of levels therapy for psychosis. He has been training psychiatrists, psychologists, nurses, support workers and carers around the world in CBT techniques to help the recovery of people with schizophrenia both in hospitals and in the community. In 2015, he received jointly with Prof. David Kingdon the Aaron Beck Award for Excellence in Cognitive Therapy.
References
- Andrews, A., Knapp, M., McCrone, P., Parsonage M, Trachtenberg M. (2012). Effective interventions in schizophrenia: The economic case. A report prepared for the Schizophrenia Commission. London: Rethink Mental Illness.
- Bianco, D. (2012) Performance of the Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) as a screening tool for depression in UK and Italy. Retrieved from http://www2.warwick.ac.uk/fac/med/research/platform/wemwbs/development/papers/donatella_bianco-thesis.pdf
- Bird, V, Premkumar, P, Kendall, T, Whittington, C, Mitchell, J, & Kuipers, E. (2010). Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. British Journal of Psychiatry, 197(5), 350-6. doi: 10.1192/bjp.bp.109.074526
- Eassom, E, Giacco, D, Dirik, A, & Priebe, S. (2014). Implementing family involvement in the treatment of patients with psychosis: a systematic review of facilitating and hindering factors. Bmj Open, 4(10), e006108. doi: 10.1136/bmjopen-2014-006108
- Fadden, G, James, C, & Pinfold, V. (2012). Caring for yourself – self-help for families and friends supporting people with mental health problems. In Rethink mental illness and meriden family programme. Birmingham: White Halo Design.
- Fridgen, G. J., Aston, J., Gschwandtner, U., Pflueger, M., Zimmermann, R., Studerus, E., … Riecher-Rössler, A. (2013). Help-seeking and pathways to care in the early stages of psychosis. Soc Psychiatry Psychiatr Epidemiol, 48, 1033–1043. doi:10.1007/s00127-012-0628-0
- Glick, I. D., Stekoll, A. H., & Hays, S. (2011). The role of the family and improvement in treatment maintenance, adherence, and outcome for schizophrenia. Journal of Clinical Psychopharmacology, 31, 82–85. doi:10.1097/JCP.0b013e31820597fa
- Grover, M., Naumann, U., Mohammad-Dar, L., Glennon, D., Ringwood, S., Eisler, I., … Schmidt, U. (2011). A randomized controlled trial of an internet-based cognitive behavioural skills package for carers of people with anorexia nervosa. Psychological Medicine, 41, 2581–2591. doi:10.1017/S0033291711000766
- Gupta, S, Isherwood, G, Jones, K.J, & Impe, K.V. (2015). Assessing health status in informal schizophrenia caregivers compared with health status in non-caregivers and caregivers of other conditions. Bmc Psychiatry. doi:10.1186/s12888-015-0547-1
- Hayes, L, Hawthorne, G, & Farhall, J, et al. 2015. Quality of life and social isolation among caregivers of adults with schizophrenia: policy and outcomes. Community Mental Health Journal. doi: 10.1007/s10597-015-9848-6
- Lobban, F., Postlethwaite, A., Glentworth, D., Pinfold, V., Wainwright, L., Dunn, G., … Haddock, G. (2013). A systematic review of randomised controlled trials of interventions reporting outcomes for relatives of people with psychosis. Clinical Psychology Review, 33, 372–382. doi:10.1016/j.cpr.2012.12.004
- Mangalore, R., & Knapp, M. (2007). Cost of schizophrenia in England. The Journal of Mental Health Policy and Economics, 10, 23–41.
- Morosini, P. L., Magliano, L., Brambilla, L., Ugolini, S., & Pioli, R. (2000). Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatrica Scandinavica, 101, 323–329.
- Petersen, I., Lund, C., Bhana, A., Flisher, A. J., & Health, M.; Poverty Research Programme Consortiu. (2012). A task shifting approach to primary mental health care for adults in South Africa: Human resource requirements and costs for rural settings. Health Policy and Planning, 27(1), 42–51. doi:10.1093/heapol/czr012
- Powell, J, Hamborg, T, Stallard, N, Burls, A, McSorley, J, Bennett, K, & Christensen, H. (2013). Effectiveness of a web-based cognitive-behavioral tool to improve mental well-being in the general population: randomized controlled trial. Journal of Medical Internet Research, 15(1), e2. doi: 10.2196/jmir.2240
- Rotondi, AJ, Anderson, CM, Haas, GL, Eack, SM, Spring, MB, Ganguli, R, Newhill, C, & Rosenstock, J. (2010). Web-based psychoeducational intervention for persons with schizophrenia and their supporters: one-year outcomes. Psychiatric Services, 61, 1099–1105.
- Smeerdijk, M., Keet, R., De Haan, L., Barrowclough, C., Linszen, D., & Schippers, G. (2014). Feasibility of teaching motivational interviewing to parents of young adults with recent-onset schizophrenia and co-occurring cannabis use. Journal of Substance Abuse Treatment, 46(3), 340–345. doi:10.1016/j.jsat.2013.09.006
- Smeerdijk, M., Keet, R., Dekker, N., Van Raaij, B., Krikke, M., Koeter, M., … Linszen, D. (2012). Motivational interviewing and interaction skills training for parents to change cannabis use in young adults with recent-onset schizophrenia: A randomized controlled trial. Psychological Medicine, 42(8), 1627–1636. doi:10.1017/S0033291711002832
- Smeerdijk, M., Keet, R., Van Raaij, B., Koeter, M., Linszen, D., De Haan, L., & Schippers, G. (2015). Motivational interviewing and interaction skills training for parents of young adults with recent-onset schizophrenia and co-occurring cannabis use: 15-Month follow-up. Psychological Medicine, 45(13), 2839–2848. doi:10.1017/S0033291715000793
- Tai, S, & Turkington, D. (2009). The evolution of cognitive behavior therapy for schizophrenia: current practice and recent developments. Schizophr Bull, 35(5), 865-73. doi: 10.1093/schbul/sbp080
- Tennant, R., Hiller, L., Fishwick, R., Platt, P., Joseph, S., Weich, S., … Stewart-Brown, S. (2007). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health and Quality of Life Outcomes, 5, 63. doi:10.1186/1477-7252-5-63
- WEMWBS Population Norms in Health Survey for England data. (2011). Retrieved from http://www2.warwick.ac.uk/fac/med/research/platform/wemwbs/researchers/interpretations/wemwbs_population_norms_in_health_survey_for_england_data_2011.pdf
- Yeandle, S, Wigfield A (eds). (2011) New approaches to supporting carers’ health and well-being: Evidence from the National Carers’ strategy demonstrator sites programme. CIRCLE, University of Leeds, Leeds.
- Yesufu-Udechuku, A, Harrison, B, Mayo-Wilson, E, Young, N, Woodhams, P, Shiers, D, Kuipers, E, & Kendall, T. (2015). Interventions to improve the experience of caring for people with severe mental illness: systematic review and meta-analysis. British Journal of Psychiatry, 206(4), 268-74. doi: 10.1192/bjp.bp.114.147561
- Zigmond, AS, & Snaith, RP. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361-70.